|
December 2021

Get ready for Availity: Find out which web browser to use
 To prepare for moving to the Availity® provider portal in the coming months, you should take a look at the internet browser you’re currently using. To prepare for moving to the Availity® provider portal in the coming months, you should take a look at the internet browser you’re currently using.
Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services.
We shared technical requirements with you in the February 2021 issue of The Record. But since that time, there has been a change: Availity no longer supports Internet Explorer 11.
If you’re using Internet Explorer now, you’ll need to switch to a new browser. Otherwise, your experience on Availity will be affected.
The preferred browser for Availity is Google Chrome, but Microsoft Edge (version 79 or higher) and Firefox® are also acceptable. You can download Google Chrome for free.**
For more information on Availity technical requirements, go to the Availity website.** Scroll down, and click on the Requirements tab.
Questions?
If you have questions about the move to Availity, check our Frequently asked questions document first. If your question isn’t already answered there, submit your question to ProviderPortalQuestions@bcbsm.com so we can consider adding it to the FAQ document.
Previous articles about Availity
We’re providing a series of articles focusing on our move to Availity for our provider portal. Here are the articles we’ve already published in case you missed them:
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Blue Cross updates continuity of care requirements to align with law
In 2020, the president signed the Consolidated Appropriations Act of 2021, or CAA, into law. That legislation had several health care-related provisions. Part of the legislation addresses continuity of care requirements.
Blue Cross Blue Shield of Michigan and Blue Care Network already allow for continuity of care for our members in Michigan as required by state law and the Affordable Care Act, and we are updating our policies to align with the requirements of the CAA.
What is continuity of care?
Sometimes, a contract between a health care provider and a health plan is modified (for example through departicipation, termination, etc.) and results in a loss or reduction of benefits for an individual. Through continuity of care, the individual is still able to see their health care provider under certain circumstances because their health situation requires it. In addition, the care would be provided as if there were no change to the contract.
What does the CAA say about continuity of care?
According to the legislation, effective Jan. 1, 2022, if a health care provider changes network status, patients with complex care needs have the option of up to 90 days of continued coverage at in-network cost sharing to allow for a transition of care to an in-network health care provider.
Complex care circumstances where you can continue treatment
The circumstances below are similar to our existing continuity of care situations with some changes outlined in the CAA legislation. You can still see your patient if he or she is:
- Undergoing a course of treatment for a “serious and complex condition,” defined as:
- An acute illness — A condition that is serious enough to require specialized medical treatment to avoid the reasonable possibility of death or permanent harm; or
- A chronic illness or condition — A condition that is:
- Life-threatening, degenerative, potentially disabling or congenital; and
- Requires specialized medical care over a prolonged period of time
- Getting inpatient care.
- Scheduled to undergo nonelective surgery, including receipt of postoperative care for that surgery
- Pregnant and undergoing a course of treatment for the pregnancy
- Determined to be terminally ill (defined as “a medical prognosis that the individual’s life expectancy is six months or less”) and is receiving treatment for their illness.
Requirements to provide services under continuity of care
If you choose to treat your patient for a continuity of care period of time, you’re required to:
- Accept payment from Blue Cross as payment in full (less any required copays or deductibles).
- Adhere to Blue Cross’ standards for maintaining quality health care and provide Blue Cross with necessary medical information related to your patient’s care.
- Adhere to Blue Cross’ policies and procedures, including, but not limited to, those concerning utilization review, referrals, pre-authorizations and treatment plans.
For more information about continuity of care, see our online provider manuals on web-DENIS.
Overview of care management and utilization management programs now available
Blue Cross Blue Shield of Michigan and Blue Care Network have implemented many care management programs for members and utilization management programs for providers.
- Care management programs provide patient support by identifying patients with health risks and working with them to improve or maintain their health.
- Utilization management programs focus on ensuring that patients get the right care at the right time in the right location through the authorization process.
These programs vary based on member coverage and may be administered by Blue Cross or BCN staff or by contracted vendors.
We recently published the Care management and utilization management programs: Overview for providers document to help you navigate these programs. This information may help you to identify services that could be useful to your patients or to learn more about programs in which your patients are participating.
In the overview document, we’ve:
- Categorized the programs and the services for which we have care management and utilization management programs.
- Listed who provides services within each category (Blue Cross or BCN staff, contracted vendors or both).
- Indicated whether services are available to Blue Cross commercial, Medicare Plus Blue℠, BCN commercial or BCN Advantage℠ members
To see more details about the programs, click a category heading. A document will open that provides:
- A summary of available services
- The groups and individual members to which services are available
- Resources for finding more information
You can access the overview document by going to ereferrals.bcbsm.com, clicking on the Quick Guides link (under Additional Resources) and then clicking on the Care management and utilization management programs: Overview for providers link.
We appreciate your efforts in helping us achieve high Medicare Star Ratings
As we reported in a web-DENIS message in October and a November-December Hospital and Physician Update article, the Centers for Medicare & Medicaid Services gave Blue Cross Blue Shield of Michigan and Blue Care Network high Medicare Star Ratings for 2022. Here are highlights:
- Our BCN Advantage℠ HMO plan received a 5-Star rating — the highest rating possible and the first 5-Star rating Blue Cross Blue Shield of Michigan has ever achieved.
- Our Medicare Plus Blue℠ PPO plan received a 4.5-Star rating, an increase of one full star over last year.
These ratings reflect improvements made in several key areas, including adherence to HEDIS® measures and CAHPS® survey results.** We appreciate all you’ve done over the last few years to help ensure that practitioners adhere to HEDIS measures and that members are satisfied with the care provided by you — the physicians and practice staff who care for our members directly.
For more details, see the article in the November-December issue of Hospital and Physician Update. We’ll also provide additional details on our 2022 Star Ratings performance in future issues of our provider publications. If you haven’t already done so, we encourage you to subscribe to Hospital and Physician Update or other provider newsletters at bcbsm.com/providers/newsletters/subscribe.html.
**HEDIS®, which stands for Healthcare Effectiveness Data and Information Set, is a registered trademark of the National Committee for Quality Assurance. CAHPS®, which stands for Consumer Assessment of Healthcare Providers and Systems, is a registered trademark of the Agency for Healthcare Quality and Research.
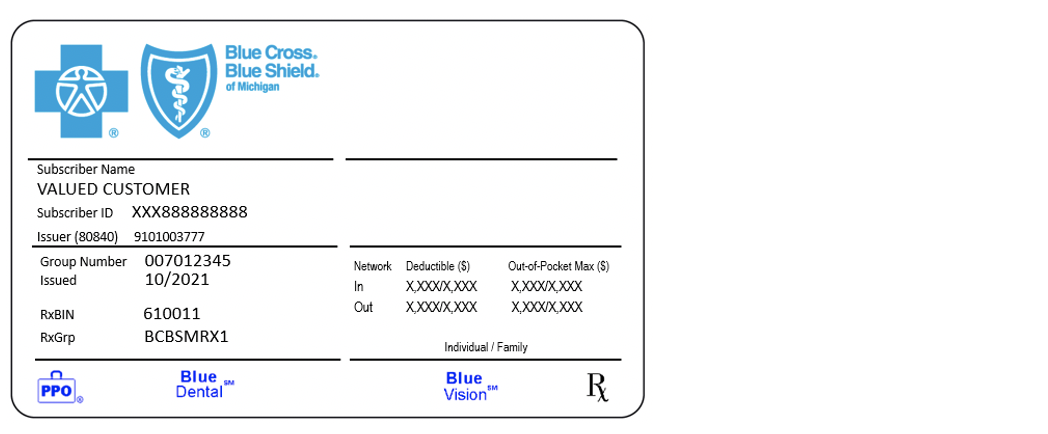
Benefit changes coming Jan. 1 for UAW Retiree Medical Benefits Trust members
There are several benefit changes that the UAW Retiree Medical Benefits Trust requested Blue Cross Blue Shield of Michigan make for its members starting Jan. 1, 2022. These include:
- Lower in-network deductible and out-of-pocket maximums for Enhanced Care Plan, or ECP, and Traditional Care Network, or TCN, members.
- For ECP members:
- In-network primary care office visit copay will be $10.
- Copays for in-network specialist visits will be $20.
- For TCN members, acupuncture (for lower back pain only) will be an allowable service secondary to Medicare and subject to the appropriate cost share.
- For both ECP and TCN members:
- In-network allergy testing and ear wax removal are covered services, subject to the appropriate cost share.
- In-network chiropractic manipulations for subluxation of the spine are covered with a $20 copay (24 visit maximum).
There have also been changes for Medicare Plus Blue℠ members:
- Lower in-network deductible and out-of-pocket maximums.
- In-network primary care office visit copays will be $10.
- Copays for in-network specialist visits will be $20.
- Copay for in-network acupuncture will be $20 (20 visit limit).
- In-network outpatient rehabilitation services, outpatient mental health and substance use disorder, compression stockings and diabetic eye exams are covered at 100%.
- Skilled nursing facility is covered at 100% for days 1 through 50 and a $20 copay per day for days 51 through 100 in-network.
- Diabetic shoes have an enhanced benefit of two pairs per year.
- Wigs are covered at 100% up to a $250 annual maximum.
This benefit information will be updated on web-DENIS, so be sure to check there for member benefit and eligibility information.
Third-quarter 2021 HCPCS update: New and updated codes
The Centers for Medicare & Medicaid Services has added several new codes as part of its quarterly Health Care Procedure Coding System updates. The codes, effective dates and Blue Cross Blue Shield of Michigan’s coverage decisions are below.
Injections
| Code |
Change |
Coverage comments |
Effective date |
| C9065 |
Deleted |
Deleted Sept. 30, 2021 |
|
| C9075 |
Deleted |
Deleted Sept. 30, 2021 |
|
| C9076 |
Deleted |
Deleted Sept. 30, 2021 |
|
| C9077 |
Deleted |
Deleted Sept. 30, 2021 |
|
| C9078 |
Deleted |
Deleted Sept. 30, 2021 |
|
| C9079 |
Deleted |
Deleted Sept. 30, 2021 |
|
| C9080 |
Deleted |
Deleted Sept. 30, 2021 |
|
| C9081 |
Added |
Requires manual review |
Oct. 1, 2021 |
| C9082 |
Added |
Covered for facility only |
Oct. 1, 2021 |
| C9083 |
Added |
Covered for facility only |
Oct. 1, 2021 |
| C9084 |
Added |
Requires manual review |
Oct. 1, 2021 |
| J0693 |
Deleted |
Deleted Sept. 30, 2021 |
|
| J0699 |
Added |
Covered |
Oct. 1, 2021 |
| J0741 |
Added |
Covered |
Oct. 1, 2021 |
| J1305 |
Added |
Requires manual review |
Oct. 1, 2021 |
| J1426 |
Added |
Not covered |
Oct. 1, 2021 |
| J1445 |
Added |
Covered |
Oct. 1, 2021 |
| J1448 |
Added |
Requires manual review |
Oct. 1, 2021 |
| J2406 |
Added |
Covered |
Oct. 1, 2021 |
| J9247 |
Added |
Covered |
Oct. 1, 2021 |
| J9315 |
Deleted |
Deleted Sept. 30, 2021 |
|
| J9318 |
Added |
Covered |
Oct. 1, 2021 |
| J9319 |
Added |
Covered |
Oct. 1, 2021 |
| Q2054 |
Added |
Requires manual review |
Oct. 1, 2021 |
Skin Substitutes
| Code |
Change |
Coverage comments |
Effective date |
| Q4228 |
Deleted |
Deleted Sept. 30, 2021 |
|
| Q4236 |
Deleted |
Deleted Sept. 30, 2021 |
|
| Q4251 |
Added |
Covered |
Oct. 1, 2021 |
| Q4252 |
Added |
Covered |
Oct. 1, 2021 |
| Q4253 |
Added |
Covered |
Oct. 1, 2021 |
DME/P&O/Medical Supplies
| Code |
Change |
Coverage comments |
Effective date |
| A4453 |
Added |
Not covered |
Oct. 1, 2021 |
| K1021 |
Added |
Not covered |
Oct. 1, 2021 |
| K1022 |
Added |
Covered by groups with prosthetic and orthotic benefits. |
Oct. 1, 2021 |
| K1023 |
Added |
Not covered |
Oct. 1, 2021 |
| K1024 |
Added |
Not covered |
Oct. 1, 2021 |
| K1025 |
Added |
Not covered |
Oct. 1, 2021 |
| K1026 |
Added |
Not covered |
Oct. 1, 2021 |
| K1027 |
Added |
Covered by groups with DME benefits. |
Oct. 1, 2021 |
Transfusion Medicine/Miscellaneous Blood Products
| Code |
Change |
Coverage comments |
Effective date |
| P9025 |
Added |
Covered |
Oct. 1, 2021 |
| P9026 |
Added |
Covered |
Oct. 1, 2021 |
Medicine Supplementary/Contraception/Devices and Supplies
| Code |
Change |
Coverage comments |
Effective date |
| J7294 |
Added |
Covered |
Oct. 1, 2021 |
| J7295 |
Added |
Covered |
Oct. 1, 2021 |
| J7303 |
Deleted |
Deleted Sept. 30, 2021 |
|
Medicine Supplementary/Special Foods and Formulas
| Code |
Change |
Coverage comments |
Effective date |
| S9432 |
Added |
Not covered |
Oct. 1, 2021 |
Surgery
| Code |
Change |
Coverage comments |
Effective date |
| C1831 |
Added |
Not covered |
Oct. 1, 2021 |
| C9779 |
Added |
Not covered |
Oct. 1, 2021 |
| C9780 |
Added |
Not covered |
Oct. 1, 2021 |
Temporary Q Code/Unclassified
| Code |
Change |
Coverage comments |
Effective date |
| Q9004 |
Added |
Not covered |
Oct. 1, 2021 |
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
HCPCS replacement codes, effective Oct. 1, 2021, established
J1305 replaces J3490, J3590 and C9079 when billing for Evkeeza (evinacumab-dgnb)
Effective Oct. 1, 2021, the Centers for Medicare and Medicaid Services has established a permanent procedure code for specialty medical drug Evkeeza™ (evinacumab-dgnb).
Services can continue to be reported with J3490, J3590 and C9079 through Sept. 30, 2021. All services performed on and after Oct. 1, 2021, must be reported with J1305.
Prior authorization is required by the Medical Benefit Drug Prior Authorization program for Evkeeza (evinacumab-dgnb), procedure code J1305, for all groups unless they opted out of the prior authorization program.
For groups that have opted out of the prior authorization program, this procedure requires manual review.
J1448 replaces J3490, J3590 and C9078 when billing for Cosela (trilaciclib)
Effective Oct. 1, 2021, CMS has established a permanent procedure code for specialty medical drug Cosela™ (trilaciclib dihydrochloride).
Services can continue to be reported with J3490, J3590 and C9078 through Sept. 30, 2021. All services performed on and after Oct. 1, 2021, must be reported with J1448.
Prior authorization is required by the Medical Benefit Drug Prior Authorization program for Cosela (trilaciclib dihydrochloride), procedure code J1448, for all groups unless they opted out of the prior authorization program.
For groups that have opted out of the prior authorization program, this procedure requires manual review.
J9247 replaces J3490, J3590 and C9080 when billing for Pepaxto (melphalan flufenamide)
Effective Oct. 1, 2021, CMS has established a permanent procedure code for specialty medical drug Pepaxto® (melphalan flufenamide).
Services can continue to be reported with J3490, J3590 and C9080 through Sept. 30, 2021. All services performed on and after Oct. 1, 2021, must be reported with J9247.
Prior authorization is required through the AIM Oncology Management Authorization program for Pepaxto (melphalan flufenamide), procedure code J9247, for all groups unless are opted out of the prior authorization program.
Pepaxto (melphalan flufenamide) is covered for all groups not included in the AIM Oncology Management Authorization program as a chemotherapy benefit for malignant conditions.
J9318 replaces J3490, J3590 and C9065 when billing for romidepsin, non-lyophilized
Effective Oct. 1, 2021, CMS has established a permanent procedure code for specialty medical drug romidepsin, non-lyophilized.
Services can continue to be reported with J3490, J3590 and C9065 through September 30, 2021. All services performed on and after Oct. 1, 2021, must be reported with J9318.
Prior authorization is required through the AIM Oncology Management Authorization program for romidepsin, non-lyophilized, procedure code J9318, for all groups unless they opted out of the prior authorization program.
Romidepsin, non-lyophilized is covered for all groups not included in the AIM Oncology Management Authorization program as a chemotherapy benefit for malignant conditions.
Q2054 replaces J3490, J3590, J9999 and C9076 when billing for Breyanzi (lisocabtagene maraleucel)
Effective Oct. 1, 2021, CMS has established a permanent procedure code for specialty medical drug Breyanzi® (lisocabtagene maraleucel).
Services can continue to be reported with J3490, J3590, J9999 and C9076 through Sept. 30, 2021. All services performed on and after Oct. 1, 2021, must be reported with Q2054.
Prior authorization is still required by the Medical Benefit Drug Prior Authorization program for Breyanzi (lisocabtagene maraleucel), procedure code Q2054, for all groups unless they opted out of the prior authorization program.
For groups that have opted out of the prior authorization program, this procedure requires manual review.
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Billing chart: Blue Cross highlights medical, benefit policy changes
You’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart.
This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures.
You will also see that descriptions for the codes are no longer included. This is a result of recent negotiations with the AMA on use of the codes.
We will publish information about new BCBS groups or changes to group benefits under the Group Benefit Changes heading.
For more detailed descriptions of the BCBSM policies for these procedures, please check under the Medical/Payment Policy tab in Explainer on web-DENIS. To access this online information:
- Log in to web-DENIS.
- Click on BCBSM Provider Publications & Resources.
- Click on Benefit Policy for a Code.
- Click on Topic.
- Under Topic Criteria, click on the drop-down arrow next to Choose Identifier Type and then click on HCPCS Code.
- Enter the procedure code.
- Click on Finish.
- Click on Search.
| Code* |
BCBSM changes to:
Basic Benefit and Medical Policy, Group
Variations Payment Policy, Guidelines
|
| NEW PAYABLE PROCEDURES |
0404T
Other codes:
58674, 58578,** 58999**
**Represent non-covered services |
Basic benefit and medical policy
Myolysis of uterine fibroids – Sonata® added
Laparoscopic or transcervical ultrasound-guided radiofrequency ablation (e.g., Acessa™ or Sonata® System™) for the treatment of uterine fibroids is established. It may be considered a useful therapeutic option when indicated.
Laparoscopic and percutaneous techniques of myolysis as a treatment of uterine fibroids other than laparoscopic ultrasound-guided radiofrequency ablation (e.g., Acessa™) and transcervical ultrasound-guided radiofrequency ablation (e.g., Sonata® System) are considered experimental, including Nd: YAG lasers, bipolar electrodes and cryomyolysis. There is insufficient published evidence to assess the safety and impact on health outcomes in the treatment of uterine fibroids.
This policy update is effective Sept. 1, 2021.
Inclusions:
Laparoscopic or transcervical ultrasound-guided radiofrequency ablation (e.g., Acessa™ or Sonata® System™)
Laparoscopic or transcervical ultrasound-guided radiofrequency ablation for the treatment of uterine fibroids may be indicated as an alternative to hysterectomy or myomectomy when the member has one or more of the following:
- Evidence of uterine fibroids via ultrasound that are less than 10 cm in diameter for Acessa™ or 7 cm for Sonata™
- Pre-menopausal state with symptomatic fibroids in members who want to avoid a hysterectomy
- Members who have contraindications to general anesthesia
- Members who have experienced any of the following symptoms that are the direct result of the fibroids:
- Severe menorrhagia causing anemia
- Bulk-related symptoms (e.g., pelvic pain, pressure or discomfort, urinary symptoms related to compression of the ureter or
bladder, or dyspareunia)
Exclusions:
Laparoscopic or transcervical ultrasound-guided radiofrequency ablation (e.g., Acessa™ or Sonata® System™) for all situations other than those specified above, and not limited to the conditions below:
- When there has been a diagnosis of cancer (or pre-cancerous lesions) anywhere in the pelvis
- In members who are diagnoses with or at risk for leiomyosarcoma
- In members with acute pelvic inflammatory disease
- In members with abnormal pap smear test results
- In members who are in a post-menopausal state
- Pedunculated fibroid type 0 or type 7 for the Sonata® System™
|
81541,** 81542,** 81479, 81551, 81599
**Payable effective Sept. 1, 2021 |
Basic benefit and medical policy
Gene expression profile analysis for prostate cancer
The safety and effectiveness of gene expression analysis to guide management of prostate cancer have been established. It may be considered a useful option when indicated.
Payment policy:
Payable providers are as follows:
- M.D. and D.O. – all specialties
- Physician assistant
- Freestanding radiology center/diagnostic imaging
- Independent laboratory
- Retail health center
- Urgent care center
- Nurse
- Multiple physician practice, groups, clinics, undetermined partnership
Inclusions for Decipher:
- Men with NCCN very low-risk, low-risk and favorable intermediate-risk prostate cancer who have a greater than 10-year life expectancy who haven’t received treatment for prostate cancer and are candidates for active surveillance or definitive therapy
- Men with intermediate-risk prostate cancer when deciding whether to add androgen-deprivation therapy to radiation
- Men with an undetectable PSA after prostatectomy for prostate cancer, to determine adjuvant versus salvage radiation therapy or to determine whether to initiate systemic therapies
Inclusions for Oncotype DX Prostate, Prolaris, ProMark:
- Men with NCCN very low-risk, low-risk and favorable intermediate-risk prostate cancer who have a greater than 10-year life expectancy who haven’t received treatment for prostate cancer and are candidates for active surveillance or definitive therapy
- Men with intermediate-risk prostate cancer when deciding whether to add androgen-deprivation therapy to radiation
Inclusions for AR-V7 testing:
Testing can be considered to help guide selection of therapy in the post abiraterone/enzalutamide metastatic castration-resistant prostate cancer, or CRPC, setting.
Exclusions:
- The use of more than one type of test to assess risk of prostate cancer progression (Oncotype DX Prostate, Decipher, Prolaris or ProMark) is considered experimental.
- ConfirmMDx testing
|
15833, 15836, 15878, 15879, 38589,**
38999**
**Unlisted codes used to report primary surgical procedure
Not covered procedures:
49329, 49999 |
Basic benefit and medical policy
Surgical treatments for lymphedema
Lymphovenous bypass and vascularized lymph node transplant for lymphedema may be considered established as a therapeutic option when indicated.
Surgical treatment of massive localized lymphedema and late-stage lymphedema by liposuction or excision is considered established.
The policy effective date is March 1, 2021.
Inclusions:
Lymphovenous bypass and vascularized lymph node transplant may be considered as surgical options when the following criteria are met:
- Signs and symptoms consistent with lymphedema as determined by a certified lymphedema therapist, and
- A diagnosis of stage ≥ I lymphedema by the International Society of Lymphology, or ISL, standards, and
- For lymphovenous bypass for unilateral disease, at least one of the following positive quantitative measurements:
- MR lymphangiogram demonstrating residual lymphatic channels
- Lymphoscintigraphy findings showing a minimum of a one-hour delayed transit time to first-level lymph nodes, axillary lymph nodes (upper extremity lymphedema) or inguinal lymph nodes (lower extremity lymphedema), or a dermal back flow pattern
- Volumetry differential (circumferential measurements and/or perometry differential) >10% (if affected extremity dominant extremity) or >7% (affected extremity is non-dominant extremity),
- Bioimpedance abnormality differential consistent with lymphedema
- Patients with bilateral disease should meet A, B, and C-1 or C-2, above.
- For vascularized lymph node transfer, at least one of the following:
- MR lymphangiogram showing absence of lymphatic channels
- Lymphoscintigraphy findings showing a minimum of a one-hour delayed transit time to first-level lymph nodes, axillary lymph nodes (upper extremity lymphedema) or inguinal lymph nodes (lower extremity lymphedema), or a dermal back flow pattern
- Volumetry differential (circumferential measurements and/or perometry differential >10% (if affected extremity dominant extremity) or >7% (affected extremity is non-dominant extremity),
- Bioimpedance abnormality differential consistent with lymphedema.
- Patient also meets all the following eligibility criteria:
- Patient has body mass index ≤ 35-40kg/m2
- Patient has undergone a course of conservative treatment under the supervision of a lymphedema therapist
- Patient has demonstrated the ability to tolerate post-surgical compression therapy and physical therapy sessions per treating lymphedema provider.
- None of the following are present:
- Chronic venous disease (e.g., chronic venous insufficiency, superior vena cava syndrome)
- Congestive heart failure
- Medication-induced swelling
- Liver disease including, but not limited to, cirrhosis, hypoproteinemia v. nephropathy including end-stage renal disease
- Active infection of the affected extremity (cellulitis/erysipelas)
- History of dye anaphylaxis
- Microsurgery for lymphedema is performed by surgeons with specialized training in lymphedema surgery and lymphology.
Exclusions:
- Lymph node transplant or lymphovenous bypass is considered experimental if the above criteria aren’t met.
- Debulking of a limb not impacted by lymphedema or lipedema is considered experimental if the above criteria aren’t met.
- Greater omental lymph node flap is considered experimental.
- Lymphatic microsurgical preventing healing approach (Lympha) is considered experimental.
Note: Refer to Table 1 for staging of lymphedema.
Table 1. Recommendations for staging lymphedema
Stage |
Description |
Stage 0 (subclinical) |
Swelling isn’t evident and most patients are asymptomatic despite impaired lymphatic transport |
Stage I (mild) |
Accumulation of fluid that subsides (usually within 24 hours) with limb elevation; soft edema that may pit, without evidence of dermal fibrosis |
Stage II (moderate) |
Doesn’t resolve with limb elevation alone; limb may no longer pit on examination |
Stage III (severe) |
Lymphostatic elephantiasis; pitting can be absent; skin has trophic changes |
|
| POLICY CLARIFICATIONS |
0358T, 76499**
**Unlisted code used to report not otherwise classified procedure |
Basic benefit and medical policy
Dual energy X-ray absorptiometry and bioelectrical impedance analysis to determine body composition
The DXA body composition system is considered experimental. While it may be safe, its utility in the medical management of the patient, compared to standard currently available measurement methods, hasn’t been scientifically determined.
Bioelectrical impedance for body composition analysis is considered experimental. It hasn’t been scientifically demonstrated to be an accurate and useful diagnostic tool.
This policy has been updated effective Nov. 1, 2021. |
15271-15278, 15777, Q4100-Q4108,
Q4110, Q4114, Q4116-Q4118, Q4121, Q4122, Q4124, Q4127, Q4128, Q4130, Q4135, Q4136, Q4147, Q4149, Q4158, Q4161, Q4164-Q4166, Q4182, Q4195, Q4196, Q4203, A6010, A6011, A6021-A6023, C9356, C9358, C9360, C9363, C9364
Experimental:
Q4111-Q4113, Q4115, Q4123, Q4125,
Q4126, Q4134, Q4141-Q4143, Q4146,
Q4152, Q4167, Q4175-Q4180, Q4193,
Q4197, Q4200, Q4202, Q4220, Q4222,
Q4226, Q4238 |
Basic benefit and medical policy
Skin and tissue substitutes
The safety and effectiveness of skin and tissue substitutes approved by the U.S. FDA and the Centers for Medicare & Medicaid Services have been established for patients meeting specified selection criteria. They may be useful therapeutic options when indicated.
Human tissue products are subject to the rules and regulations of banked human tissue by the American Association of Tissue Banks, or AATB, and have been established for patients meeting specified selection criteria. They may be useful therapeutic options when indicated.
This policy has been updated, effective Nov. 1, 2021.
Inclusions:
The following skin and tissue substitutes are considered established as they have been approved by the FDA. This list may not be all-inclusive:
- Apligraft®
- Atlas Wound Matrix
- Biobrane®
- Bio-conneKt® Wound Care Matrix
- Cytal® Burn Matrix
- Cytal® MicroMatrix™
- Cytal™ Wound Matrix (formerly MatriStem)
- Cytal® Wound Sheet
- Derma-Gide (aka Geistlich Derma-Gide™)
- Dermagraft®
- Endoform Dermal Template™
- Epicel® has FDA humanitarian device spproval
- E-Z Derm™
- Helicoll™
- Hyalomatrix®
- Integra® Bilayer Matrix
- Integra® Dermal Regeneration Template
- Integra® Flowable Wound Matrix
- Intregra® Matrix Wound Dressing (formerly known as Avagen)
- Keratec Wound Dressings (Kermatrix®):
- Keratec Keragel
- Keraderm
- Kerafoam
- Kerecis™ Omega3 Wound (formerly known as MeriGen)
- MediSkin®
- MicroMatrix®
- Oasis® Burn Matrix
- Oasis® Ultra Tri-Layer Wound Matrix
- Oasis® Wound Matrix
- Ologen™ Collagen Matrix
- OrCel®
- Permacol™ (Covidien)
- PriMatrix™
- Puracol® and Puracol® Plus Collagen Wound Dressings
- PuraPly Wound Matrix (PuraPly)
- PuraPly Antimicrobial Wound Matrix (PuraPly AM)
- Strattice™
- Suprathel®
- SurgiMend®
- Talymed™
- TenoGlide™
- TheraSkin®
- TransCyte®
Breast reconstructive surgery using allogeneic acellular dermal matrix products (including each of the following: AlloDerm®, AlloMend®, Cortiva®, [AlloMax™], DermACELL™, DermaMatrix™, FlexHD®, FlexHD® Pliable™, Graftjacket®) are considered established when one of the following is met:
- There’s insufficient tissue expander or implant coverage by the pectoralis major muscle and additional coverage is required.
- There’s viable but compromised or thin postmastectomy skin flaps that are at risk of dehiscence or necrosis.
- The inframammary fold and lateral mammary folds have been undermined during mastectomy and reestablishment of these landmarks is needed.
Note: Various acellular dermal matrix products used in breast reconstruction have similar efficacy. The products listed are those that have been identified for use in breast reconstruction. Additional acellular dermal matrix products may become available for this indication.
Treatment of chronic, noninfected, full-thickness diabetic lower extremity ulcers is established when using the following tissue engineered skin substitutes:
- AlloPatch®a
- Apligraft®b
- Dermagraft®b
- GraftJacket® Regenerative Tissue Matrix-Ulcer Repair
- Integra®, OmnigraftTM Dermal Regeneration Matrix (also known as Omnigraft™) and Integra Flowable Wound Matrix
- Theraskin®
Treatment of chronic, noninfected, partial- or full-thickness lower-extremity skin ulcers due to venous insufficiency, which have not adequately responded following a one-month period of conventional user therapy is established when using the following tissue-engineered skin substitutes:
- Aplifraf®b
- OasisTM Wound Matrixc
- Theraskin®
OrCel™ is considered established when all of the following criteria are met:
- Used for the treatment of dystrophic epidermolysis bullosa
- Used for the treatment of mitten-hand deformity
- Standard would therapy has failed
- Provided in accordance with the humanitarian device exemption, or HDE, specifications of the FDA
The following skin and tissue products and substitutes are considered established for use in the treatment of second- and third-degree burns:
- Alloderm
- Epicel® (for the treatment of deep dermal or full-thickness burns comprising a total body surface area ≥30% when provided in accordance with the HDE specifications of the FDA)d
- Integra® Dermal Regeneration Templateb
aBanked human tissue
bFDA premarket approval
cFDA 510(k) clearance
dFDA-approved under an HDE
Exclusions:
All other uses of bioengineered skin and soft tissue substitutes listed above unless they meet the following criteria:
- FDA approval and provided in accordance with the FDA guidelines
- Covered by Centers for Medicare & Medicaid Services
All other skin and soft tissue substitutes, including but not limited to:
- ACell® UBM Hydrated/Lyophilized Wound Dressing
- AlloSkin™
- AlloSkin™ RT
- Aongen™ Collagen Matrix
- Architect® ECM, PX, FX
- ArthroFlex™ (Flex Graft)
- AxoGuard® Nerve Protector (AxoGen)
- BellaCell HD or SureDerm®
- CollaCare®
- CollaCare® Dental
- Collagen Wound Dressing (Oasis Research)
- CollaGUARD®
- CollaMend™
- CollaWound™
- Coll-e-Derm
- Collexa®
- Collieva®
- Conexa™
- Coreleader Colla-Pad
- CorMatrix®
- Cymetra™ (Micronized AlloDerm™)
- Dermadapt™ Wound Dressing
- DermaPure™
- DermaSpan™
- DressSkin
- Durepair Regeneration Matrix®
- ENDURAGen™
- Excellagen
- ExpressGraft™
- FlexiGraft®
- FlowerDerm®
- GammaGraft
- Graftjacket® Xpress, injectable
- hMatrix®
- InteguPly®
- Keramatrix®
- Keroxx™
- MatriDerm®
- Matrix HD™
- MemoDerm™
- Microderm® biologic wound matrix
- Miroderm®
- MyOwn Skin™
- NeoForm™
- Progenamatrix™
- Puros® Dermis
- RegenePro™
- Repliform®
- Repriza™
- Restrata
- SkinTE™
- StrataGraft®
- TenSIX™ Acellular Dermal Matrix
- TissueMend
- TheraForm™ Standard/Sheet
- TruSkin™
- Veritas® Collagen Matrix
- XCM Biologic® Tissue Matrix
- XenMatrix™ AB
|
33340 |
Basic benefit and medical policy
Percutaneous left atrial appendage closure devices
The medical policy statement, and inclusionary and exclusionary criteria have been updated, effective Nov. 1, 2021.
Medical policy statement:
The safety and effectiveness of an FDA-approved percutaneous left atrial appendage closure device (e.g., Watchman™ Left Atrial Appendage Closure or Watchman FLX) for the prevention of stroke in patients with atrial fibrillation have been established. It may be considered a therapeutic option when indicated
Inclusions (both of the following):
- There is an increased risk of stroke and systemic embolism based on CHADS2 or CHA2DS2-VASc score and systemic anticoagulation therapy is recommended.
- The long-term risks of systemic anticoagulation outweigh the risks of the device implantation.
Exclusions:
The use of a device with FDA approval for percutaneous left atrial appendage closure (e.g., the Watchman™ or the Watchman FLX) for stroke prevention in patients who don’t meet the above criteria is considered experimental.
The use of devices not approved by the FDA for percutaneous left atrial appendage closure (including but not limited to the Lariat and Amplatzer devices) for stroke prevention in patients with atrial fibrillation is considered experimental. |
47133, 47135, 47140, 47141, 47142, 47143, 47144, 47145, 47146, 47147, 47399
|
Basic benefit and medical policy
Liver transplant
The safety and effectiveness of liver transplantation and retransplantation have been established. It may be considered a useful therapeutic procedure in carefully selected patients with end-stage liver failure due to irreversibly damaged livers.
Exclusionary criteria have been updated, effective Nov. 1, 2021.
Inclusionary and exclusionary guidelines:
Inclusions for liver transplant:
- Patients with end-stage liver disease. Etiologies of end-stage liver disease include, but are not limited to, the following:
- Hepatocellular diseases
- Alcoholic liver disease
- Viral hepatitis (either A, B, C, or non-A, non-B)
- Autoimmune hepatitis
- Alpha-1 antitrypsin deficiency
- Hemochromatosis
- Non-alcoholic steatohepatitis
- Protoporphyria
- Wilson's disease
- Cholestatic liver diseases
- Primary biliary cirrhosis
- Primary sclerosing cholangitis with development of secondary biliary cirrhosis
- Biliary atresia
- Vascular disease
- Neuroendocrine tumors metastatic to the liver*** (see NET criteria below)
- Primary hepatocellular carcinoma
- Inborn errors of metabolism
- Trauma and toxic reactions
- Miscellaneous indications
- Familial amyloid polyneuropathy
- Patients with polycystic disease of the liver who have massive hepatomegaly causing obstruction or functional impairment.
- Pediatric patients with nonmetastatic hepatoblastoma
- Patients with unresectable hilar cholangiocarcinoma if additional inclusionary criteria are met (see below)**
**Cholangiocarcinoma (Available online at:
https://optn.transplant.hrsa.gov/)
According to the OPTN policy on liver allocation, candidates with cholangiocarcinoma, or CCA, meeting the following criteria will be eligible for a MELD/PELD exception with a 10% mortality equivalent increase every three months:
- Centers must submit a written protocol for patient care to the OPTN/UNOS Liver and Intestinal Organ Transplantation Committee before requesting a MELD score exception for a candidate with CCA. This protocol should include selection criteria, administration of neoadjuvant therapy before transplantation, and operative staging to exclude patients with regional hepatic lymph node metastases, intrahepatic metastases, or extrahepatic disease. The protocol should include data collection as deemed necessary by the OPTN/UNOS Liver and Intestinal Organ Transplantation Committee.
- Candidates must satisfy diagnostic criteria for hilar CCA:** malignant-appearing stricture on cholangiography and one of the following: carbohydrate antigen 19-9 100 U/mL, or a biopsy or cytology results demonstrating malignancy, or aneuploidy. The tumor should be considered unresectable on the basis of technical considerations or underlying liver disease (e.g., primary sclerosing cholangitis).
- If cross-sectional imaging studies (CT scan, ultrasound, MRI) demonstrate a mass, the mass should be 3 cm or less.
- Intra- and extrahepatic metastases should be excluded by cross-sectional imaging studies of the chest and abdomen at the time of initial exception and every three months before score increases.
- Regional hepatic lymph node involvement and peritoneal metastases should be assessed by operative staging after completion of neoadjuvant therapy and before liver transplantation. Endoscopic ultrasound-guided aspiration of regional hepatic lymph nodes may be advisable to exclude patients with obvious metastases before neoadjuvant therapy is initiated.
- Transperitoneal aspiration or biopsy of the primary tumor (either by endoscopic ultrasound, operative or percutaneous approaches) should be avoided because of the high risk of tumor seeding associated with these procedures.
***Criteria for liver transplant patient selection for neuroendocrine tumors, or NET, metastatic to the liver (MELD exception applications for patients with NET):
- Recipient age <60 years
- Resection of primary malignancy and extra-hepatic disease without any evidence of recurrence at least six months prior to MELD exception request.
- Liver-limited neuroendocrine liver metastasis, or NLM, bi-lobar, not amenable to resection. Tumors in the liver should meet the following radiographic characteristics:
- CT scan: Triple phase contrast:
- Lesions may be seen on only one of the three phases
- Arterial phase: may demonstrate a strong enhancement
- Large lesions can become necrotic/calcified
- MRI appearance:
- Liver metastasis are hypodense on T1 and hypervascular in T2 wave images
- Diffusion restriction
- Majority of lesions are hypervascular on arterial phase with wash – out during portal venous phase IV. Hepatobiliary phase post Gadoxetate Disodium (Eovist): Hypointense lesions are characteristics of NET
- Consider for exception only those with a NET of Gastro-entero-pancreatic, or GEP, origin tumors with portal system drainage. Note: Neuroendocrine tumors with the primary located in the lower rectum, esophagus, lung, adrenal gland or thyroid aren’t candidates for automatic MELD exception.
- Lower-intermediate grade following the WHO classification. Only well differentiated (low grade, G1) and moderately differentiated (intermediate grade G2). Mitotic rate <20 per 10 HPF with less than 20% ki-67 positive markers
- Tumor metastatic replacement shouldn’t exceed 50% of the total liver volume
- Negative metastatic workup should include one of the following:
- No evidence for extra-hepatic tumor recurrence based on metastatic radiologic workup at least three months prior to MELD exception request (submit date)
- Recheck metastatic workup every three months for MELD exception increase consideration by the Regional Review Board. Occurrence of extra-hepatic progression – for instance lymph-nodal Ga68 positive locations – should indicate de-listing. Patients may come back to the list if any extra-hepatic disease is zeroed and remained so for at least six months.
- Presence of extra-hepatic solid organ metastases (e.g., lungs, bones) should be a permanent exclusion criteria.
Exclusions for liver transplant:
- Patients with intrahepatic cholangiocarcinoma
- Patients with hepatocellular carcinoma that has extended beyond the liver
- Patients with ongoing alcohol or drug abuse. (Evidence for abstinence may vary among liver transplant programs, but generally, a minimum of three months is required.)
- Patients with conditions not included in the inclusions section:
- Severe cardiac or pulmonary disease
- AIDS
- Uncontrolled sepsis
- Anatomic abnormality that precludes liver transplantation Intrahepatic cholangiocarcinoma
- Extrahepatic malignancy
- Hemangiosarcoma
- Persistent noncompliance
Inclusions for liver retransplant:
Liver retransplant is established for patients with:
- Primary graft non-function
- Hepatic artery thrombosis
- Chronic rejection
- Ischemic type biliary lesions after donation after cardiac death
- Recurrent non-neoplastic disease-causing late graft failure
Exclusions for liver retransplant:
Patients not meeting above inclusionary criteria for retransplant.
Potential contraindications for transplant or retransplant:
Note: Final patient eligibility for transplant is subject to the judgment and discretion of the requesting transplant center.
Potential contraindications represent situations where proceeding with transplant isn’t advisable in the context of limited organ availability. Contraindications may evolve over time as transplant experience grows in the medical community. Clinical documentation supplied to the health plan should demonstrate that attending staff at the transplant center have considered all contraindications as part of their overall evaluation of potential organ transplant recipients and have decided to proceed.
- Known current malignancy or history of recent malignancy
- Untreated systemic infection making immunosuppression unsafe, including chronic infection
- Other irreversible end-stage disease not attributed to liver disease
- Systemic disease that could be exacerbated by immunosuppression
- Psychosocial conditions or chemical dependency affecting ability to adhere to therapy as defined by the transplant program
|
69710, 69711, 69714, 69715, 69717,
69718, L8625, L8690, L8691, L8692,
L8693, L8694 |
Basic benefit and medical policy
Implantable bone conduction or anchored hearing devices
The safety and effectiveness of FDA-approved unilateral or bilateral fully or partially implanted bone-conduction (bone-anchored) hearing aids have been established. They may be considered a useful therapeutic option when indicated.
The use of a Baha® Softband may be considered established in children ages 5 and younger meeting criteria for BAHA treatment, but who are determined to have inadequate skeletal maturity to sustain osteointegration of the BAHA device.
The inclusionary criteria have been updated, effective Nov. 1, 2021.
Inclusions:
FDA-approved devices when used according to approved indications and guidelines.
Conductive hearing loss:
FDA-approved unilateral or bilateral fully or partially implantable bone-conduction (bone-anchored) hearing aids may be necessary as an alternative to an air-conduction hearing aid in patients with conductive or mixed hearing loss ages 5 and older (Baha 4, Baha 5, Baha 5 SuperPower, Baha Cordele II, Ponto™ Bone Anchored Hearing System, Ponto 4 and Otomag® Bone Conduction [OBC] devices) or ages 12 and older (Cochlear OSIA and Cochlear OSIA 2 system) who also meet one of the following criteria:
- Congenital or surgically induced malformations (e.g., atresia) of the external ear canal or middle ear
- Chronic external otitis or otitis media
- Tumors of the external canal or tympanic cavity
- Chronic dermatitis of the external canal prohibiting the usage of an air conduction hearing aid
and meet the following audiologic criteria:
- A pure-tone average bone-conduction threshold measured at 0.5, 1, 2, and 3 kHz or better than or equal to one of the following:
- 45 dB (OBC and BP100, Baha 4 and Baha 5, Ponto, Ponto 3, Ponto Pro, Ponto Plus, and Ponto 4 devices)
- 55 dB (Intenso, Cochlear OSIA and Cochlear OSIA 2, Ponto 3 power, Ponto Pro Power and Ponto Plus Power devices)
- 65 dB (Cordele II, Baha 5 SuperPower, Ponto 3 SuperPower devices)
For bilateral implantation, patients should meet the above audiologic criteria in both ears and have symmetrically conductive or mixed hearing loss as defined by a difference between left and right side bone-conduction threshold of less than 10 dB on average measured at 0.5, 1, 2 and 3 kHz (4 kHz for OBC, Ponto Bone Anchored Hearing System, Ponto 3, Ponto 3 Power, Ponto 3 SuperPower, Ponto 4 and Ponto Pro devices) or less than 15 dB at individual frequencies.
Sensorineural hearing loss:
A unilateral implantable bone-conduction (bone-anchored) hearing aid may be considered medically necessary as an alternative to an air-conduction contralateral routing of signal hearing aid in patients ages 5 and older (Baha 4, Baha 5, Baha 5 SuperPower, Baha Cordele II, OBC, Ponto 3, Ponto 3 Power and Ponto 3 SuperPower and Ponto Bone Anchored Hearing devices) or ages 12 and older (Cochlear OSIA and Cochlear OSIA 2 system) with single-sided sensorineural deafness and normal hearing in the other ear. The pure-tone average air-conduction threshold of the normal ear should be better than 20 dB measured at 0.5, 1, 2 and 3 kHz.
Note: The Audiant® bone conductor is a bone-conduction hearing device. While this product is no longer actively marketed, patients with existing Audiant devices may require replacement, removal or repair.
In patients being considered for implantable bone-conduction (bone-anchored) hearing aids, skull bone quality and thickness should be assessed for adequacy to ensure implant stability. Additionally, patients (or caregivers) must be able to perform proper hygiene to prevent infection and ensure the stability of the implants and percutaneous abutments.
Exclusions:
- Other uses of implantable bone-conduction (bone-anchored) hearing aids, including use in patients with bilateral sensorineural hearing loss, are considered experimental
- Non-FDA-approved devices or indications
|
Established:
81201, 81202, 81203, 81210, 81288, 81292, 81293, 81294, 81295, 81296, 81297, 81298, 81299, 81300, 81301, 81307, 81308, 81317, 81318, 81319, 81401, 81403, 81406, 81435, 81436, 81445, 81450
Experimental:
81327, 81455, 81479, 81437, 81438, 0037U, 0048U, 0238U, 0244U |
Basic benefit and medical policy
Genetic cancer susceptibility panels
The medical policy statement, and inclusionary and exclusionary criteria have been updated, effective Nov. 1, 2021.
Medical policy statement:
Limited genetic cancer susceptibility panels that include only gene variants for which the member meets criteria in other policies may be considered established (see related policies for the Inclusionary and Exclusionary Guidelines).
Genetic cancer susceptibility panel testing is considered experimental in all other situations.
Reference the following policies for specific coverage criteria:
- Genetic Testing for Hereditary Breast/Ovarian Cancer Syndrome (BRCA1 or BRCA2)
- Genetic Testing for Lynch Syndrome and Other Inherited Colon Cancer Syndromes
- Genetic Testing (Single Nucleotide Variants) To Predict Risk of Nonfamilial Breast Cancer
- Gene Expression Profiling for Cutaneous Melanoma
- Gene Variants Associated with Breast Cancer in Individuals at High Breast Cancer Risk
- Moderate Penetrance Variants Associated with Breast Cancer in Individuals at High Breast Cancer Risk
- Circulating Tumor DNA Management of Non-Small-Cell Lung Cancer (Liquid Biopsy)
- Genetic Testing for PTEN Hamartoma Tumor Syndrome
- Genetic Testing-NGS Testing of Multiple Genes (Panel) to Identify Targeted Cancer Therapy
|
Established:
81243, 81244
Experimental:
81171, 81172 |
Basic benefit and medical policy
Genetic testing for FMR1 and FMR2
The testing strategy that required procedure code *81243 to be performed with positive test results is no longer required, effective Sept. 1, 2021. |
81401, 81405, 81408, 81410, 81411,
81479**
**Used to describe not otherwise classified procedure |
Basic benefit and medical policy
Genetic testing for connective tissue disorders and thoracic aortic aneurysms
The safety and effectiveness of genetic testing for Marfan syndrome, Ehlers-Danlos syndrome type IV (vascular type), other syndromes associated with thoracic aortic aneurysms and dissections, and related disorders have been established. It may be considered a useful diagnostic option when indicated.
The inclusionary criteria and policy title have been updated, effective Nov. 1, 2021.
Inclusions:
Individual genetic testing for the diagnosis of Marfan syndrome, Ehlers-Danlos syndrome type IV (vascular type), other syndromes associated with thoracic aortic aneurysms and dissections, and related disorders when:
- Focused genetic testing of the following genes: FBN1, COL3A1, MYH11, ACTA2, SLC2A10, SMAD3, MYLK, TGFBR1 and TGFBR2 or
- A panel of at least nine genes that must include FBN1, COL3A1, MYH11, ACTA2, SLC2A10, SMAD3, MYLK, TGFBR1 and TGFBR2 when one of the following is met:
- Signs and symptoms of a connective tissue disorder are present, but a definitive diagnosis can’t be made using established clinical diagnostic criteria (i.e., Ghent criteria)
- Assessing future risk of disease in an asymptomatic individual when there is a known pathogenic variant in the family.
Exclusions:
- Genetic testing panels for Marfan syndrome, Ehlers-Danlos syndrome type IV (vascular type), other syndromes associated with thoracic aortic aneurysms and dissections, and related disorders that don’t include genes listed under inclusions
- For the prenatal or pre-implantation genetic diagnosis of Marfan syndrome in the offspring of patients with known disease-causing variants
|
84145 |
Basic benefit and medical policy
Actemra procalcitonin testing
The safety and effectiveness of procalcitonin, or PCT, testing, for detection and monitoring of bacterial infections and sepsis in specified patient populations have been established. PCT testing is a useful diagnostic option for patients meeting selection criteria in the inpatient or outpatient setting when used as part of the physician’s total treatment armamentarium.
This policy update is effective Nov. 1, 2021.
Inclusions:
For use in the inpatient or outpatient (emergency department, observation care, etc.) setting for the following conditions:
- Hospitalized patients who are initiating and/or discontinuing antibiotic therapy
- Risk assessment for critically ill patients as a guidance for continuation of therapy
Exclusions:
The use of procalcitonin testing with serial testing of the following conditions is considered experimental for the following indications because of insufficient evidence of its effectiveness. Note: This isn’t an all-inclusive list. These indications include the diagnoses of:
- Surgical infections (including monitoring of the infection
- Appendicitis
- Chronic renal insufficiency
- Infective endocarditis
- Non-alcoholic fatty liver disease
- Parapneumonic pleural effusions
- Spontaneous bacterial peritonitis
It’s also considered experimental for:
- Measuring the differentiation of infection from other inflammatory complications following stem cell transplantation
- The evaluation of fever of uncertain source in infants
- Predicting outcomes in people with acute coronary syndrome
- Prediction of neurological deficits following carotid endarterectomy
|
Covered services:
Online codes:
98970-98972, 99421-99423
Telephone codes:
99441-99443, 98966 98968
Any code that is appropriate for both the encounter and provider scope, (including behavioral health not related to autism) and is delivered synchronously (in real time)
Asynchronous care:
99446, 99447, 99448, 99449, 99451, 99452
Any code that is appropriate for both the encounter and provider scope and is delivered asynchronously
Behavioral health services: There are multiple billing codes for behavioral health services; behavioral health services aren’t appropriate for asynchronous care. |
Basic benefit and medical policy
Telemedicine services
Medical
The safety and effectiveness of telemedicine (synchronous and asynchronous care) for medical care have been established. It may be considered a useful diagnostic and therapeutic option when indicated.
Behavioral health
The safety and effectiveness of telemedicine synchronous care for behavioral health have been established, with the exception of specific autism services.**
Telemedicine asynchronous care isn’t appropriate for behavioral health services.
**Refer to the policy “Autism Spectrum Disorder Services.”
The exclusionary criteria have been updated, effective Nov. 1, 2021.
Payment policy:
Behavioral health services may require prior authorization. Procedure codes *96130 and *96156 aren’t eligible telemedicine services.
Inclusions:
Synchronous/real-time encounter:
- The provider must be licensed, registered or otherwise authorized to perform service in their health care profession in the state where the patient is located. Services must fall within their scope of practice.
- Telemedicine delivered services are available to all clinicians; however, this may not be the preferred method of delivery in certain clinical scenarios, for example chronic suicidal ideation or unstable angina. A hosted visit** or a face-to-face visit may be necessary due to the complexity of the clinical situation. The telemedicine provider may provide the face-to-face encounter.
- Telemedicine delivered services for ongoing treatment of a condition that is chronic or is expected to take more than five sessions before the condition resolves or stabilizes may require a hosted visit** or a face-to-face visit. The telemedicine provider may provide the face-to-face encounter.
- The service must be conducted over a secured channel.
- The delivery of the service can be either audio only (telephone) or audio/video (a secured computer-based system).
Online visit:
- An audiovisual online communication
- The patient initiates the medical or behavioral health encounter
- The provider must be licensed, registered or otherwise authorized to perform service in their health care profession in the state where the patient is located.
- A low complexity, straight forward decision-making encounter that addresses urgent but not emergent clinical conditions
- A single encounter where a follow-up encounter isn’t anticipated
- Services must fall within the provider’s scope of practice.
Asynchronous/store and forward encounter:
- The provider must be licensed, registered or otherwise authorized to perform service in their health care profession in the state where the patient is located. Services must fall within their scope of practice.
- The patient data (pre-recorded videos, digital images such as X-rays or photos, test results or any other information necessary for the evaluation) must be transmitted over a secured channel.
Exclusions:
Synchronous and asynchronous:
- Request for medication refills
- Reporting of normal test results
- Provision of educational materials
- Scheduling of appointments and other health care related issues
- Registration or updating billing information
- Reminders for health care related issues
- Referrals to other providers
- An online or telemedicine visit resulting in an office visit, urgent care or emergency care encounter on the same day for the same condition
- An online visit for the same condition of an online visit within the previous seven days
- An online or telemedicine visit occurring during the post-operative period
Behavioral health care:
Behavioral health care services may be delivered via synchronous telemedicine, including intensive outpatient program, or IOP, and partial hospital program, or PHP, services.
Behavioral health-specific synchronous care exclusions:
Autism services are allowed via telemedicine synchronous care, but with limitations and exceptions. Refer to the policy “Autism Spectrum Disorder Services.”
Behavioral health-specific asynchronous care exclusions:
Behavioral health services aren’t appropriate via telemedicine asynchronous care.
Note: See policy guidelines and billing guidance sections of the medical policy for more information. |
J3262 |
Basic benefit and medical policy
Actemra (tocilizumab)
Actemra (tocilizumab) is payable for the
following updated FDA-approved indications:
Systemic sclerosis-associated interstitial lung disease, or SSc-ILD
- Slowing the rate of decline in pulmonary function in adult patients with systemic sclerosis-associated interstitial lung disease
Dosage information:
Recommended adult subcutaneous dosage: The recommended dose of Actemra for adult patients with SSc-ILD is 162 mg given once every week as a subcutaneous injection. |
| GROUP BENEFIT CHANGES |
Faurecia USA Holdings, Inc. |
Faurecia USA Holdings, Inc., group number 000071830, is adding the following plans, effective Jan. 1, 2022.
Group number: 000071830
Alpha prefixes:
M5G: Anthem MO Blue Access Choice
K4C: BCBS Kansas City Preferred Care Blue
T6T: BCBS Tennessee Network S
A4F: Non-Select Network PPO Plans
Platform: NASCO
Plans offered:
PPO medical/surgical
CDH – HSA
Prescription drug
Hearing |
None of the information included in this billing chart is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.

Starting Jan. 1, 2022, bill Medicare Advantage plans for administration of COVID‑19 vaccines and monoclonal antibody treatments
Beginning Jan. 1, 2022, the Centers for Medicare & Medicaid services will require Medicare Advantage plans to cover the cost to administer COVID-19 vaccines (including approved booster doses) and monoclonal antibody products to treat COVID-19, with no out-of-pocket costs for members.
For dates of service on or after Jan. 1, 2022, submit claims for the administration of vaccines and monoclonal antibody treatments to Blue Cross Blue Shield of Michigan or Blue Care Network for members with Medicare Plus Blue℠ or BCN Advantage℠ plans.
Note: If your patient scheduled an office visit on or after Jan. 1, 2022, for any other reason than getting the vaccine or monoclonal antibody treatments, bill the usual office visit charge.
More information
For more information on the COVID-19 vaccine, refer to CMS’ COVID-19 toolkit** for health care providers.
For more information on monoclonal antibody treatment, see the Monoclonal Antibody COVID-19 Infusion webpage** of CMS’ COVID-19 toolkit for health care providers.
Reminder
For dates of service on or after Oct. 1, 2021, cost share applies for any treatment related to COVID-19, other than monoclonal antibody treatment, for Medicare Plus Blue and BCN Advantage members.
None of the information in this article is intended to be legal advice and, as such, it remains the providers’ responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Intensive outpatient program and partial hospital program services now payable on an ongoing basis when delivered through telemedicine
As previously communicated, Blue Cross Blue Shield of Michigan and Blue Care Network began allowing behavioral health intensive outpatient and partial hospital program services to be payable when provided by contracted facilities through telemedicine as a temporary measure during the COVID-19 pandemic.
Effective Nov. 1, 2021, we’re updating our Telemedicine Services medical policy to allow these services to be payable when delivered by contracted facility providers through synchronous (real-time) telemedicine on an ongoing basis, rather than as a temporary measure. We’re doing this to make it easier for members to receive these services beyond the COVID-19 pandemic.
For more information, including information about billing for these services, see the Telehealth for behavioral health providers document on our public website at bcbsm.com/coronavirus or within Provider Secured Services.
Reminders
- Facilities can provide behavioral health IOP and PHP services to BCN commercial and BCN Advantage℠ members only when their contracts specifically include IOP and PHP services.
- For Blue Cross commercial members, most plans don’t cover IOP services for mental health or PHP services for substance use disorders. IOP services for substance use disorders must be delivered by a substance abuse treatment facility. Be sure to check member eligibility and benefits through web-DENIS or by contacting Provider Inquiry before performing services.
- For Medicare Plus Blue℠ members, follow Centers for Medicare & Medicaid Services guidance.
Updated documents
We’ve updated the following documents to reflect this change:
- Telehealth for behavioral health providers
- Temporary changes due to the COVID-19 pandemic
You can find these documents on our public website at bcbsm.com/coronavirus or within Provider Secured Services.
You can view the updated Telemedicine Services medical policy through our Medical Policy & Pre-Cert/Pre-Auth Router on bcbsm.com.
Additional autism interventions delivered through telemedicine now payable
As previously communicated, Blue Cross Blue Shield of Michigan and Blue Care Network began allowing some services for autism spectrum disorder to be payable when delivered through telemedicine as a temporary measure during the COVID-19 pandemic.
Effective Nov. 1, 2021, we’re updating our Autism Spectrum Disorder Services medical policy to allow those telemedicine services to be payable on an ongoing basis. We’re also removing restrictions on protocol modification *97155.
These changes apply to members whose coverage includes an autism benefit.
To determine which procedures can be performed through telemedicine for Medicare Plus Blue℠ members who have an autism benefit, see the Medicare-covered telehealth services for the COVID-19 PHE document.
Telemedicine services payable on an ongoing basis, effective Nov. 1
Per the updated medical policy, we’ll allow the following autism services to be delivered through synchronous (real time) telemedicine on an ongoing (no longer temporary) basis:
- Assessment, *97151
- Applied behavior analysis, or ABA, *97153
This service is allowed for children who meet appropriateness criteria. The Guidelines for autism interventions delivered through telemedicine document offers guidance in determining which members can benefit from direct-line ABA interventions delivered through telemedicine.
- Skills training, *97154
- Intensive skills training, *97158
Restrictions lifted on protocol modification
Per the updated medical policy, protocol modification *97155, will be allowed through real-time telemedicine visits 100% of the time. (Previously, this service was allowed to be delivered through telemedicine only 50% of the time.)
During the COVID-19 pandemic, for dates of service from April 14, 2020, through Oct. 31, 2021, we allowed licensed behavior analysts, or LBAs, to troubleshoot treatment protocols directly with the parent or caregiver functioning as the behavioral technician. With the Nov. 1, 2021, update to the Autism Spectrum Disorder medical policy, this temporary measure is no longer payable.
Reminder
The following services continue to be payable when delivered through real-time telemedicine: caregiver training (*97156), multi-family caregiver training (*97157), supervision (S5108) and caregiver training (S5111).
S5108 and S5111 are payable only to Michigan providers who deliver services to out-of-state members and can’t use the American Medical Association category 1 codes.
Updated documents
We’ve updated the following documents to reflect this change:
- Telehealth for behavioral health providers
- Temporary changes due to the COVID-19 pandemic
You can find these documents on our public website at bcbsm.com/coronavirus or within Provider Secured Services.
You can view the updated Telemedicine Services medical policy through our Medical Policy & Pre-Cert/Pre-Auth Router on bcbsm.com.
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Behavioral health services delivered through synchronous telemedicine
With the Nov. 1, 2021, updates to the following medical policies, additional behavioral health and autism spectrum disorder, or ASD, services are now payable when delivered through telemedicine:
- Telemedicine Services
- Autism Spectrum Disorder Services
Behavioral health and ASD services must be delivered synchronously (in real time), with the exception of *96130 and *96156, which can be delivered asynchronously.
Telemedicine asynchronous (store and forward) care generally isn’t payable for behavioral health services.
This applies to Blue Cross Blue Shield of Michigan commercial, Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members.
For more information about providing behavioral health and ASD services through telemedicine, see the Telehealth for behavioral health providers document, which is available on our public website at bcbsm.com/coronavirus or within Provider Secured Services.
You can view the updated medical policies through our Medical Policy &
Pre-Cert/Pre-Auth Router at bcbsm.com.
Acupuncturists invited to apply to be part of Blue Cross’ provider networks
What you need to know
Enrollment forms and practitioner agreements will be available at bcbsm.com/providers, starting Dec. 1, 2021, for acupuncturists who want to join a Blue Cross network. Once approved, acupuncturists can begin participating in a Blue Cross network, starting March 1, 2022.
Acupuncturists have the opportunity to participate in Blue Cross Blue Shield of Michigan’s Traditional and TRUST PPO networks, Medicare Plus Blue℠, BCN commercial and BCN Advantage℠, effective March 1, 2022.
How to join a Blue Cross network
Acupuncturists can find enrollment forms and practitioner agreements at bcbsm.com/providers, starting Dec. 1, 2021. To find enrollment information, click on Enroll to become a network provider. Specific qualification requirements are identified within each agreement.
All applicants must pass a credentialing review before participation. We’ll notify applicants in writing of their approval status.
Billing for services
Participating acupuncturists can bill their professional services using codes *97810, *97811, *97813 and *97814. They can receive direct reimbursement for covered services within the scope of their licensure at 85% of the applicable fee schedule, minus any member deductibles and copayments.
This change, effective for outpatient services provided on or after March. 1, applies to Blue Cross and BCN benefit plans that cover services these providers are licensed to provide. To find out if a member has coverage, check web-DENIS for member benefits and eligibility or call Provider Inquiry at 1-800-344-8525.
Prior authorization and referrals
Prior authorization isn’t required for acupuncture services for any member. For BCN commercial members who have a primary care provider who is part of a medical care group based in the East or Southeast region, their primary care provider must submit a referral for a specialist office visit. Referrals aren’t required for other members.
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Services related to complementary and alternative therapies aren’t covered benefits
The use of complementary or alternative therapies, practices, medicine or supplements that aren’t supported by valid scientific studies is considered experimental. When there’s insufficient evidence in the current medical literature to show that these approaches are safe or as beneficial as the current standard of care, Blue Cross Blue Shield of Michigan doesn’t cover them.
Ancillary services, such as visits, imaging and testing, that are performed primarily to facilitate the delivery of an unproven or experimental service are also considered experimental in nature and aren’t a covered benefit. The effective date for this policy is Nov. 1, 2021.
“Alternative medicine” is a term that describes a broad range of treatments and practices that are used in place of traditional therapies. “Complementary medicine” is a term that describes treatments and practices that are used in conjunction with traditional therapies.
Other terms used to describe such practices include functional, integrative, herbalism, homeopathy, holistic, unconventional, nonconventional, nontraditional, new age and natural. “Traditional medicine” refers to the standard of practice that’s widely used by the medical community and has been proven safe and efficient.
Types of complementary and alternative medicine that lack evidence-based, clinical-decision support
| Type of complementary or alternative medicine |
Description |
| Active release technique |
Relief of tissue tension using a soft tissue method (manipulation and movement) to remove fibrosis or adhesions |
| Acupressure |
Using fingers to apply steady force on specific pressure points to mobilize chi or life force energy to aid in healing |
| Applied kinesiology |
Belief that various muscles are linked to internal organs and glands. Evaluates structural, chemical and mental aspects of health using manual muscle testing. |
| Aromatherapy |
Uses natural plant extracts topically or through inhalation to promote health and well-being |
| Art therapy (color, light, music) |
Clinical use of expressive art forms to promote optimal functioning of physical and emotional health |
| Ayurveda |
Prevention and maintenance of health through balance of thinking, diet, lifestyle and the use of herbs |
Biofield therapeutics
- Healing touch
- Pranic healing
- Reiki or Qigong
- Biofield tuning
- Regenetics method
|
Noninvasive therapy that stimulates healing by the practitioner interacting with a client’s field of energy
- Energy therapy where practitioners use their hands in a heart-centered way to support and facilitate physical, emotional, mental and spiritual health
- No-touch energy healing that focuses on the 11 major chakras in the body and uses the body’s inborn ability to heal itself
- Palm/hands-on healing is used to transfer a universal energy through the palms of the hands of the practitioner to the individual to promote emotional or physical healing.
- Use of a tuning fork to scan for resistance and turbulence in an individual’s energy field. The body’s organization energy uses the coherent vibrational frequency of the tuning fork to “tune” itself.
- Utilizes intention and vowel sounds at specific frequencies to activate a systematic “biofield cleanse,” clearing out distortions within one's biofield that may be negatively impacting physical, emotional and mental health
|
| Coffee enema |
Detoxes the liver by absorbing the coffee enema through the venous system in the lower part of the colon. The liver is stimulated to produce more bile and in turn flushes out toxins |
| Combined electrochemical therapy |
High-frequency electrical stimulation and peripheral nerve block purported to treat peripheral neuropathy by first injecting the peripheral nerve with a local anesthetic, then ”nutraceuticals” (mostly vitamins), followed by a high-frequency electrical stimulation. The techniques are purported to treat peripheral neuropathy. |
| Crystal healing |
Proponents of this technique believe that crystals act as conduits for healing. Positive, healing energy flows into the body as negative, disease-causing energy flows out. |
| Cupping |
Special cups are placed on the skin to create suction for the purpose of helping with pain, inflammation, blood flow, relaxation, well-being and as a type of deep tissue massage. |
| Dry hydrotherapy |
Treatment that uses heated water in a self-contained device, such as a table or chair. The water circulates around the individual in a massaging or pulsing manner (for example, aqua massage). |
| DUTCH testing |
Dried urine test for comprehensive hormones, or DUTCH, involves the collection of a small amount of urine on filtered paper one to four times a day. Mapping of hormone metabolites (cortisol, cortisone, estradiol, estrone, estriol, progesterone, testosterone, DHEA and melatonin) of the adrenal glands, sex hormones and melatonin is used to treat a multitude of aliments.
The ailments include sleep issues, fertility problems, stress, fatigue, decreased muscle mass or bone density, aching joints, loss of libido, lowered immunity, endometriosis, PMS, painful periods and fibrous breasts. And DUTCH is used in an attempt to lower the risk of estrogen-dominant cancers, such as breast, cervical and uterine. |
| Ear candling |
Ear candles are hollow cone candles made of wax-covered fabric. The pointed end is placed in the ear while the other end is lit. The warm “suction” is believed to remove earwax, improve hearing and treat conditions such as sinus infections and colds. |
| Full body hyperthermia |
Systemically targets abnormal cells and pathogens by raising the temperature of the entire body. The patient’s body temperature is raised to 102° - 104°F. |
| Functional intracellular analysis |
Evaluates and leverages an individual’s interaction between nutrients and their genes, pathophysiology and biochemistry to optimize function |
| Gc-MAF |
Gc protein (known as vitamin D(3)-binding protein) is the precursor for the principle macrophage-activating factor, or MAF, and is used on the theory that it has various functions as an immune modulator. Gc-MAF is injected into the body to encourage macrophage activation, anti-angiogenic activity and anti-tumor activity. |
| Guided imagery |
Mental images are used to stimulate or re-create the sensory perception of sights, sounds, tastes, smells, movements and images associated with touch. |
| Hair analysis |
Used to identify or monitor trace minerals or toxins in the body |
| High-dose vitamin C |
May decrease cell proliferation in a variety of cancer cell lines, such as prostate, pancreatic, hepatocellular, colon, mesothelioma and neuroblastoma |
| Homeopathy |
Whole-body approach where products come from plants, minerals or animals |
| Hydrogen peroxide therapy |
Intravenously used to treat ailments such as cold, flu and sinus infections |
| Hypnosis |
Uses the power of suggestion to promote recovery of suppressed memories or to encourage behavior modification |
| Immunoimagery |
Consists of guided imagery, deep relaxation exercises, visualization videos or audio stimulation to promote healing from within using the mind-body connection to stimulate the immune system |
Intravenous therapies
- Antioxidant
- Micronutrient
- Phospholipids
|
- Ingredients thought to counteract the effects of free radicals. Free radicals are substances that cause oxidative stress, which may contribute to aging and certain diseases.
- Minerals, trace elements, amino acids, vitamins and fatty acids used to improve the physical and mental performance into old age. Also a popular approach to treat fibromyalgia.
- Series of infusions containing phospholipids, glutathione (an intracellular antioxidant) folic acid and vitamin B12, usually given weekly.
|
| Inversion therapy |
Suspends the individual upside down to stretch the spine and relieve back pain |
| Laetrile |
Drug that contains purified amygdalin — a compound found in the seeds or kernels of many fruits, raw nuts, beans and other plant foods. It’s converted by the body into hydrogen cyanide, which is believed to be a source of anticancer effects. |
| Magnet therapy |
Uses static magnets to alleviate pain and other health concerns |
| Meridian therapy |
Includes specialized tools, which stroke the skin in the direction of the flow of blood and lymph. This aims to improve circulation, remove toxins, lift sagging facial contours, minimize fine lines and wrinkles, and improve radiance. |
| Myotherapy |
Assess, treats and manages pain associated with soft tissue injury and restricted joint mobility caused by muscle or myofascia dysfunction. It uses therapies that include muscle stretching, transcutaneous electrical nerve stimulation, passive stretching, dry needling, cupping, acupressure and muscle energy techniques. |
| Naprapathic medicine |
Naprapathic manipulation, use of heat, cold, light, water, radiant energy electricity, sound, air or other adjunctive therapies, focusing on the soft tissues (muscle, fascia) to treat connective tissue disorders |
| Naturopathy |
System that rejects the use of medications and is based on the theory that diseases can be successfully treated or prevented through diet, exercise and massage |
| Near infrared lamp therapy |
Uses light wavelengths to aid in detoxification, deep tissue healing and pain or inflammation relief. Indicated to destabilize cancer cells and aid in the process of cancer cell destruction. |
| Over-the-counter biologics |
Products that are produced from living organisms or contain components of living organisms (for example: glucosamide, coenzyme Q10, fish oil) |
| Ozone therapy |
Process of administering ozone gas into your body to treat a disease or wound. Used to treat medical conditions by stimulating the immune system or to disinfect and treat disease |
| Reflexology |
Based on theory that areas of the feet, hands and ears are connected to certain body parts and systems. Applying pressure to specific areas is believed to offer a range of health benefits. |
| Rolfing |
Technique that involves the manipulation of the fascia and soft tissue to create better alignment and balance in the body |
| Traumeel |
Used for temporary relief of minor muscle and joint aches caused by strains, sprains and bruising by reducing inflammation. Traumeel is a nonstandardized compounded substance that is available topically, orally and by injection. |
| Ultraviolet blood transfusion |
Exposure of the blood to light to heighten the body’s immune response and to kill infections |
| Visceral massage |
Gentle manual therapy technique that assesses the relationship between the body’s organs (for example, the bladder, bowel or uterus) and other structures, such as muscles, fascia, ligaments and joints |
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Coming soon: We’re changing how we issue value‑based reimbursements for PDCM outcomes
Effective Jan. 1, 2022, Blue Cross Blue Shield of Michigan will change the way it issues value-based reimbursements for outcomes related to Provider-Delivered Care Management.
No action is required from provider organizations or health care providers at this time. We simply want to make them aware of the process.
Eligibility for value-based reimbursements for PDCM outcomes has already been determined, and changes in the process started Sept. 1, 2021.
Through Dec. 31, 2021, value-based reimbursements for PDCM outcomes will continue to be paid as they are today. Starting January 2022, and for each month thereafter, Blue Cross will produce a claim on behalf of eligible providers for each attributed member. The attribution will include:
- Members who have Blue Cross Blue Shield of Michigan coverage and live in Michigan
- Members who have coverage through another Blue plan
This value-based reimbursement claim for PDCM outcomes will be represented by one procedure code and not spread across multiple codes (as with the percentage VBR).
Keep the following in mind:
- Each month, Blue Cross will produce a claim on behalf of the eligible physician. The claim will include procedure code S0281, diagnosis code Z0289 and modifier 3P.
- The value-based reimbursement amount is dependent on the VBR percentage the provider earned as of Sept. 1.
- The dollar amount varies from $0.40 to $1.60 per attributed member per month, based on the chart below.
- This change only affects value-based reimbursements for PDCM outcomes. All other value-based reimbursements will remain unchanged.
See the below charts for additional details:
Adults
| Measure |
Performance
threshold |
Potential rate |
Improvement percent |
Value-based reimbursement amount |
| Emergency department encounters (per 1,000 members per year) |
175 |
55 |
10% |
$0.40 per attributed member per month |
| Inpatient encounters (per 1,000 members per year) |
45 |
15 |
8% |
$0.40 per attributed member per month |
| Comprehensive diabetes control: HbA1c < 8% |
0.70 |
0.98 |
10% |
$0.40 per attributed member per month |
| High blood pressure
(<140/90 mm Hg for all adults ages 18-64 with hypertension)
|
0.70 |
0.98 |
10% |
$0.40 per attributed member per month |
Pediatric
| Measure |
Composite measure |
Performance threshold |
Potential rate |
Improvement percent |
Value-based reimbursement amount |
| Emergency department encounters (per 1,000 members per year) |
N/A |
164 |
55 |
10% |
$0.40 per attributed member per month |
| Inpatient encounters (per 1,000 members per year) |
N/A |
13.5 |
1 |
9% |
$0.40 per attributed member per month |
| Follow-up after emergency department visit for mental illness |
PEDCOMP1 |
56% |
N/A |
N/A |
$0.80 per attributed member per month |
| Follow-up care for children prescribed ADHD medication — continuation and maintenance phase
|
PEDCOMP1 |
47% |
N/A |
N/A |
| Asthma medication ratio — 5 to 11 ratio > 50%
|
PEDCOMP1 |
44% |
N/A |
N/A |
| Asthma medication ratio — 12 to 17 ratio > 50%
|
PEDCOMP1 |
65% |
N/A |
N/A |
If you have any questions, send an email to ValuePartnerships@bcbsm.com.
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
2022 member ID cards to display deductible, out‑of‑pocket maximum
Effective Jan. 1, 2022, ID cards issued to Blue Cross Blue Shield of Michigan and Blue Care Network commercial members will display their deductible and out-of-pocket maximum. This change applies to both the physical and electronic ID cards. The Consolidated Appropriations Act of 2021 requires us to provide this information on the ID cards issued to participants, beneficiaries or enrollees.
The new CAA mandate requires that issued ID cards contain the following:
- In-network and out-of-network individual and family deductibles
- Out-of-pocket maximums
The following is a sample card image:
Providers should continue to use webDENIS and PARS for benefit information.
In some cases, where member deductibles or out-of-pocket maximums aren’t available on the card, the card will show “See Benefits.” Members will be directed to access their benefits on bcbsm.com or the BCBSM mobile app.
In addition, for commercial members with prescription drug coverage, their ID cards will also show a new RxBIN to reflect our pharmacy benefit manager change from Express Scripts to OptumRx. This was announced in an article in the September 2021 Record and on Page 26 of the September-October 2021 BCN Provider News.
Remote Clinical Documentation Improvement program helps keep medical records accurate
Advantasure® employs the Remote Clinical Documentation Improvement program to help providers accurately capture their patients’ severity of illness in their medical records.
The Centers for Medicare & Medicaid Services requires providers to document certain chronic conditions in the patient’s medical record at least once every calendar year.
The incentive-based Remote CDI program uses the Clinical Documentation Improvement Alert, a single-page guide to help providers perform CMS-compliant medical record documentation during face-to-face, audio and audiovisual telehealth visits. Advantasure will distribute CDI Alerts to providers up to three times a year that are based on:
- Actual diagnoses submitted on claims within the prior two calendar years
- Potential new diagnoses based on findings in the medical record or prior pharmacy and lab claims
- Star Ratings or quality measure gaps identified through claims data that may require tests or services to be ordered for your patient
How to earn the Remote CDI incentive
- Address all identified confirmation of diagnosisand clinical documentation improvement opportunities on your patients’ CDI Alerts by Dec. 31 each calendar year.
- Submit a completed CDI Alert with the office visit notes from the same date of service. (Healthy Blue portal closures do not qualify for the Remote CDI incentive.)
- Submit the alerts to Advantasure within 14 days of the patient visit.
Providers who close out 100% of the identified risk gaps listed on the CDI Alert are eligible to earn a $100 incentive for each attributed member.
For more information about the program or to request a brochure, contact:
- Tom Rybarczyk, clinical consultant, at 313-378-8259
- Denise McMillan, senior analyst, at 313-407-7529
Blue Cross has partnered with Advantasure on the Remote Clinical Documentation Improvement program. This program supports providers in accurately addressing conditions for their Medicare Advantage patients.
Our new, updated enrollment flyers assist providers joining our network
We’ve updated some of our enrollment flyers to help providers joining Blue Cross Blue Shield of Michigan or Blue Care Network. The Enrollment documents helpful hints flyers are step-by-step guides that walk providers through each section of their enrollment application. Depending on the classification type, providers may see different form fields on their application. Here are the three available flyers, with information on recent changes:
Blue Cross enhances tools for electronically prescribing medications and submitting prior authorizations
Blue Cross Blue Shield of Michigan is committed to enhancing its electronic processes across the health care spectrum, including the processes used by prescribers.
As part of our transition to OptumRx as our new pharmacy benefit manager, we’re making some improvements to our provider-facing tools to assist with prescribing and submitting prior authorizations electronically. These enhancements will primarily take place behind the scenes and won’t have a major effect on how providers prescribe and submit prior authorizations or check on patients’ benefits.
As you read in a September Record article, the move from Express Scripts, Inc. to OptumRx will take place Jan. 1, 2022, for commercial individual and group members, and Jan. 1, 2023, for Medicare Advantage individual and group members.
Continue to use your current electronic medical record system or CoverMyMeds® to submit electronic prior authorizations for Blue Cross and Blue Care Network members. Keep in mind that the BIN number changes to 610011, effective Jan. 1, 2022, for all Blue Cross and BCN commercial members.
Electronic prior authorization, or ePA, replaces faxing and phone calls so you can focus less on administrative tasks and more on patient care. For more information on ePA and CoverMyMeds, see our ePA flyer. Once we launch Availity, our new secure provider portal, we’ll also provide a link to Prompt PA, another resource that can be used to submit electronic prior authorization requests for pharmacy benefit drugs.
Also, continue to use electronic medical records for electronic prescribing and real-time prescription benefit checks. Note: You may have heard of a tool called PreCheck MyScript. This is a product name that OptumRx uses for its real-time benefit check connectivity and programing with electronic medical record systems. From a provider perspective, the interface will look and feel much the same as what providers currently use with Express Scripts.
By using these tools, physicians get patient-specific pharmacy information up front. And the better physicians and patients understand the medication options and costs at the point of prescribing, the more likely patients are to fill prescriptions and adhere to their medication regimen.
The Pharmacy team is communicating about these enhancements at various provider-facing forums, including regional medical director meetings, BCN business administrator meetings and network performance improvement meetings.
If you have any questions, call the Pharmacy Help Desk at 1-800-437-3803.
Reminder: TurningPoint to review sites of care for total hip and knee surgeries for some members
For dates of service on or after Jan. 3, 2022, TurningPoint Healthcare Solutions, LLC will review the site of care for total hip and knee surgeries as part of each authorization determination. Based on medical necessity review, TurningPoint may approve authorization requests for select total hip and knee cases only when scheduled in an outpatient setting.
This applies to members with the following coverage:
- Medicare Plus Blue℠
- BCN commercial
- BCN Advantage℠
If TurningPoint approves an authorization for a hip or knee surgery in an outpatient setting and the member experiences a change in condition that requires an inpatient admission, you’ll need to submit an authorization request for the inpatient admission (procedure code *99222) through the e‑referral system; see the “Submit an inpatient authorization” section of the e-referral User Guide for more information. Blue Cross Blue Shield of Michigan or Blue Care Network will review the request, using InterQual® criteria.
Performing total hip and knee surgeries in outpatient settings is supported by both evidence-based guidelines and the Centers for Medicare & Medicaid Services.
For more information about the TurningPoint musculoskeletal surgical quality and safety management program, see these pages on the ereferrals.bcbsm.com website:
TurningPoint Healthcare Solutions, LLC is an independent company that handles authorizations for musculoskeletal surgical and other related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Reminder: Prior authorization requirements expanding for Medicare Advantage and BCN commercial on Jan. 1
We’re expanding our prior authorization requirements for Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members. For the procedure codes listed below, you’ll need to complete questionnaires in the e-referral system when you submit prior authorization requests for dates of service on or after Jan. 1, 2022.
We’ll update related documents to reflect this change before Jan. 1.
For Medicare Plus Blue members
Most of the procedure codes below already require prior authorization for BCN commercial and BCN Advantage members. But this requirement is new for Medicare Plus Blue members for requests submitted for dates of service on or after Jan. 1.
| Category |
Procedure codes |
| Blepharoplasty and repair of brow ptosis |
*15822, *15823, *67900, *67901, *67902, *67903, *67904, *67906, *67908 |
| Cosmetic or reconstructive surgery |
*20912, *21210, *30465, *67909, *67911 |
| Rhinoplasty |
*30460, *30462 |
For BCN commercial and BCN Advantage members
The procedure codes below require prior authorization for BCN commercial and BCN Advantage, but aren’t associated with a questionnaire in the e-referral system. For dates of service on or after Jan. 1, you’ll need to complete a questionnaire when you request prior authorization for these codes.
| Category |
Procedure codes |
| Cosmetic or reconstructive surgery |
**20912, *30465 |
For Medicare Plus Blue, BCN commercial and BCN Advantage members
For requests submitted for dates of service on or after Jan. 1, these procedure codes will require prior authorization for Medicare Plus Blue, BCN commercial and BCN Advantage members.
| Category |
Procedure codes |
| Blepharoplasty of the lower lid |
*15820,a *15821a |
| Cardiac devices |
*33285, *33340 |
| Cardiac ablation |
*93653, *93654, *93656 |
| Thyroid surgeries |
*60210, *60212, *60220, *60225, *60240, *60252, *60254, *60260, *60270, *60271 |
| Vein ablation and related services |
*36473, *36474, *36482, *36483 |
| Septoplasty |
*30520 |
aThis procedure code currently requires prior authorization for BCN commercial and BCN Advantage members. For dates of service on or after Jan. 1, 2022, this code will be associated with the new Blepharoplasty of the lower lid questionnaire. (For dates of service prior to Jan. 1, 2022, this code is associated with the Cosmetic or reconstructive surgery questionnaire.)
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Additional drugs require prior authorization for URMBT members with Blue Cross non‑Medicare plans
For dates of service on or after Jan. 27, 2022, we’re adding prior authorization requirements for the following drugs covered under the medical benefit for UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans:
- Blenrep™ (belantamab mafodotin-blmf), HCPCS code J9037
- Jemperli™ (dostarlimab-gxly), HCPCS codes J3490, J3590, J9999, C9082
- Monjuvi® (tafasitamab-cxix), HCPCS code J9349
- Zynlonta® (loncastuximab tesirine-lpyl), HCPCS codes J3490, J3590, J9999, C9084
Submit prior authorization requests through AIM Specialty Health®, an independent company that contracts with Blue Cross Blue Shield of Michigan to provide benefit management services.
Prior authorization requirements apply when these drugs are administered in an outpatient setting.
This requirement doesn’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714).
How to submit authorization requests
Submit prior authorization requests to AIM using one of the following methods:
Additional information
Authorization isn’t a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members.
For additional information on requirements related to drugs covered under the medical benefit for UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans, see:
We’ll update the appropriate drug lists to reflect the information in this message prior to the effective date.
Accredo manages prior authorization requests for additional medical benefit drugs. Accredo is an independent company that works with the URMBT on specialty pharmacy services.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Blue Cross will provide physical therapy benefits for GM hourly employees under group number 83200
Effective Jan. 1, 2022, Blue Cross Blue Shield of Michigan will administer outpatient physical therapy benefits to GM hourly populations under group number 83200. TheraMatrix will no longer be the outpatient physical therapy provider for this group.
Members will receive new ID cards in the mail with updated phone numbers so they can contact Customer Service if they have questions. Benefits and coverage will remain the same. Outpatient physical therapy and benefits don’t require a prior authorization. Nonparticipating providers aren’t covered.
On and after Jan. 1, 2022, contact Blue Cross if you have benefit and claims questions. You can also log in to Provider Secured Services to review benefits and submit claims. If you have questions, call Provider Relations and Servicing at the number on the back of the card or one of the following phone numbers:
- Physicians and other professional providers: 1-800-344-8525
- Hospital and facility providers: 1-800-249-5103
For processing or if you have questions about claims dated Dec. 31, 2021, and older, contact TheraMatrix at 1-888-638-8786 or theramatrix.com.** Theramatrix is an independent company that Blue Cross had contracted with to provide physical therapy services.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Get ready for welcome to Medicare and annual wellness visits for Medicare Plus Blue patients
The new year will bring new and existing Medicare Plus Blue℠ members to your medical practice for their annual wellness visits. These visits are at no cost to members and play an important role in helping maintain or improve their health.
Welcome to Medicare visit
New Medicare Plus Blue members should be scheduling their welcome to Medicare preventive visit, which is their Initial Preventive Physical Examination. This is a one-time appointment for new Medicare patients to be scheduled within their first 12 months of enrollment. Medicare pays for one welcome to Medicare visit per member, per lifetime.
This visit is a great way to get up-to-date information on health screenings, shot records, family medical history and other preventive care services. For more information on the components of a welcome to Medicare visit, see the Medicare Learning Network Educational Tool.**
The following is the billing code for the welcome to Medicare visit, also known as the Initial Preventive Physical Examination, or IPPE:
Annual wellness visits
Existing Medicare Plus Blue℠ members should be scheduling their annual wellness visits. Medicare will cover an annual wellness visit every 12 months for patients who’ve been enrolled in Medicare for longer than 12 months.
The annual wellness visit is a chance for you to develop or update your patient’s personalized prevention plan based on his or her current health situation and risk factors. A health risk assessment is part of the annual wellness visit. It includes self-reported information from your patient to be completed before or during the visit. For more information on the components of an annual wellness visit, see the Medicare Learning Network Educational Tool.**
The following are billing codes for annual wellness visits, which include a personalized prevention plan of service:
- G0438 — First visit AWV; can only be billed one time, 12 months after a G0402 (IPPE)
- G0439 — Annual wellness visit (subsequent)
Note: G0438 or G0439 must not be billed within 12 months or previous billing of a G0402 (IPPE).
You can also offer to conduct virtual visits depending on your office’s capabilities.
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Helping to limit disability with osteoporosis management
Musculoskeletal conditions are the second largest contributor to disability, according to the World Health Organization.
The HEDIS® measure** (also one of our Star measures) called Osteoporosis Management in Women who had a Fracture, or OMW, assesses women ages 67 through 85 who suffered a fracture and had either a bone mineral density test or received a prescription to treat osteoporosis within six months of the fracture.
Read the Osteoporosis Management in Women who had a Fracture tip sheet to learn more about this measure, including:
- Information to include in medical records
- ICD-10 codes to include on patient claims
**HEDIS®, which stands for Healthcare Effectiveness Data Information Set, is a registered trademark of the National Committee for Quality Assurance.
Register for Transitions of Care Medicare Star measure webinar
Action item
Watch a short video introducing a new Medicare Star measure, and register for a webinar.
The four components of the HEDIS® Transitions of Care measure will be added to the list of Medicare Star measures starting in 2022. Watch this short video about Blue Cross Blue Shield of Michigan and Blue Care Network’s training efforts to help you avoid gaps in care for this measure.
Register and attend a webinar
Learn more about Transitions of Care, including requirements and coding tips. To register, click on a sign-up link below.
Sign up for final live coding webinar of 2021; recent sessions now on‑demand
We’re offering additional webinars that provide updated information on risk adjustment documentation and coding of common challenging diagnoses.
All sessions start at 12:15 p.m. Eastern time and run for 15 to 30 minutes. They also provide physicians and coders with an opportunity to ask questions.
Click on a link below to sign up for a live webinar:
| Session date |
Topic |
Led by |
Sign-up link |
| Thursday, Dec. 9 |
Evaluation and management coding tips |
Coder |
Register here |
You can watch previously hosted sessions on our new provider training site:
| Session date |
On-demand webinar |
| April 20 |
Acute conditions reported in the outpatient setting |
| May 19 |
Morbid (severe) obesity |
| June 17 |
Major depression |
| July 20 |
Diabetes with complication |
| Aug. 18 |
Renal disease |
| Sept. 23 |
Malignant neoplasm |
| Oct. 12 |
Updates for ICD-10 CM |
| Nov. 17 |
Coding scenarios for primary care and specialty |
Access to the training site differs slightly for new and existing users:
Once logged in, users can access the modules in two ways:
- Look in the course catalog under Quality management.
- Enter “lunch and learn” in the search box at the top of the screen.
More information
Provider Experience delivers new on-demand training resources
Action item
Visit our provider training site to find helpful resources. Details on accessing the site can be found below.
Our online, on-demand, provider training courses are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network.
The newest resources include:
- Claims Attachment Process video. This updated video guides you through the process of identifying services that need documentation, locating the Medical Record Routing Form and using it to correctly submit medical records or documentation.
- E-referral tutorials. We’ve made updates to several modules within the series. Tutorials review how to perform major tasks in the e-referral tool to manage referrals and authorizations. This series has moved from ereferrals.bcbsm.com to our new provider training site.
- 2021 lunch and learn webinar recordings. The newest topic added to the series, Updates for 2022 ICD-10 CM codes, reviews key changes for the ICD-10 CM codes and guidelines.
To request access to our training site, follow these steps:
- Open the registration page.
- Complete the registration. We recommend using the same email you use to communicate with Blue Cross and BCN for provider-related needs. This will become your login ID.
- Follow the link to log in.
If you need assistance creating your login ID or navigating the site, contact ProviderTraining@bcbsm.com.
Help managing acute low back pain in adults
This is part of an ongoing series of articles focusing on the tools and resources available to help FEP® members manage their health.
The Centers for Disease Control and Prevention estimates that 2.5 million Americans visit an outpatient clinical setting each year for the treatment of low back pain. To help doctors treat patients with this pain, the Michigan Quality Improvement Consortium developed a Management of Acute Low Back Pain in Adults** guideline.
The MQIC guideline focuses on assessment and conservative treatments for patients with no red flags of a more serious pathology. Diagnostic tests or imaging such as X-ray, CT scan or MRI are usually not required to treat low back pain in the first six weeks of onset. By avoiding imaging, exposure to radiation and health care costs are reduced.
To help patients recover from low back pain and for long-term protection, the American Academy of Orthopedic Surgeons developed a Spine Conditioning Program.** The program, developed in 2017, features a wide range of exercises designed to strengthen and support the spine.
Blue Cross and Blue Shield Federal Employee Program® members can also access WebMD® Interactive Resources with a MyBlue® account. There, members can find information on the management and prevention of acute low back pain.
If you or members have questions about the online interactive resources and benefit information, call Customer Service at 1-800-482-3600.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.

Update: We’re aligning local rules for acute inpatient medical admissions
What you need to know
We’ve updated the article on this topic that ran in previous issues of The Record and BCN Provider News. Key changes:
- We’ve clarified that authorization requests for inpatient admissions for certain acute medical conditions should be submitted only after the member has spent 48 hours in the hospital.
- We’ve revised the effective date for this change for BCN commercial members from Jan. 3, 2022, to Feb. 1, 2022.
You’ll want to use the following revised article as your reference on this topic.
For certain conditions, authorization requests for acute medical admissions should be submitted only after the member has spent 48 hours in the hospital. Once the 48 hours has elapsed, the facility can submit the request to authorize an inpatient admission. You must provide clinical documentation that demonstrates that the InterQual® criteria have been met at the time you submit the request.
Exception: When a member is receiving intensive care services that require an ICU setting, you can submit the request prior to completion of the 48-hour period, along with all clinical documentation supporting the critical level of care.
We’re aligning our local rules for all lines of business to reflect this change.
Effective dates for this change
This update to local rules will go into effect as follows:
- For Medicare Plus Blue℠ and BCN Advantage℠ members: This change is effective for members admitted on or after Jan. 3, 2022.
- For Blue Care Network commercial members: This change is effective for members admitted on or after Feb. 1, 2022.
- For Blue Cross Blue Shield of Michigan commercial: This change is effective for members admitted on or after March 1, 2022.
Conditions this applies to
This applies to members with the following conditions:
|
- Deep vein thrombosis
- Diabetic ketoacidosis
|
- Nausea / vomiting
- Nephrolithiasis
|
|
|
|
|
|
|
|
|
- Skin and soft tissue infection
|
|
|
|
|
- Intractable low back pain
|
- Transient ischemic attack
|
|
|
|
How determinations will be made
Once the request has been received, Blue Cross and BCN will conduct a medical necessity review based on the clinical documentation you submitted. InterQual criteria will be applied based on the member’s condition at the time the clinical documentation is received:
- If InterQual criteria are met, the authorization request will be approved.
- If InterQual criteria aren’t met, the authorization request will be sent to the plan medical director for review.
- If the member hasn’t been in the hospital for 48 hours and isn’t in the ICU, Blue Cross and BCN will request that the facility wait until the member has been in the hospital for 48 hours to send additional information about the member’s condition. We’ll make the request through the Case Communication field in the e-referral system or by calling the facility, or both.
On the third day, Blue Cross and BCN will do the following:
- If the facility sent additional clinical information and it meets criteria, we’ll approve the request.
- If the facility hasn’t sent additional clinical information or has sent additional clinical information but it doesn’t meet criteria, we’ll refer the request to the medical director for review.
For requests that are nonapproved, Blue Cross and BCN will reimburse as observation. The hospital will need to submit a claim for observation reimbursement.
Reason for change
We expect that this change will:
- Reduce the number of communications that typically accompany these types of authorization requests.
- Decrease denials for lack of clinical information, because all clinical documentation in support of the admission would be received after 48 hours of hospital care.
Additional information
For most members, facilities can request peer-to-peer reviews, if desired. Refer to the document How to request a peer-to-peer review with a Blue Cross or BCN medical director.
In addition, facilities can appeal denial decisions as usual. Refer to the pertinent provider manual for information about how to submit an appeal.
Here’s what you need to know about DRG readmission processing and how to provide input
Blue Cross Blue Shield of Michigan is proposing an enhancement to DRG readmission processing. This improvement is scheduled for implementation on March 1, 2022, for Blue Cross commercial members. The program update will identify inpatient readmission claims prior to payment.
| Current DRG readmissions process |
Proposed DRG readmissions process |
- Inpatient claims are received by Blue Cross Blue Shield of Michigan and are paid.
- Readmission claims are identified by Blue Cross’ clinical editing program and are audited post-payment.
- If the audit indicates a readmission occurred, then the claim is denied post-payment and reimbursement is requested.
- This process allows for up-front payment of claims that are non-reimbursable and requires additional administrative burden on the providers to provide medical records.
- A claim can take up to six months to finalize, depending on which appeals are filed.
|
- Inpatient claims received will review against member claim history for a prior related admission.
- Inpatient claims with no prior related admission will be paid through existing processes.
- Inpatient claims with prior related admission that meet the readmission criteria listed below will deny without payment:
- The voucher will indicate that the claim is a readmission.
- The facility should rebill the original paid claim, combining the readmission services as noted in the online provider manual.
- Providers may send an appeal through normal processes if they believe, and can support, that the rejected claim should have been billed and reimbursed separately.
- Providers have the opportunity to acknowledge the readmission before payment is required.
|
Currently, readmissions are identified by our clinical editing program and result in post-pay audits. This new process will eliminate the need for post-pay readmission audits.
What this means to hospitals
If a facility recognizes a readmission claim prior to billing Blue Cross for the second admission, it can rebill the first admission, including the services provided in the second admission, as noted in the online provider manual. This would eliminate the need for Blue Cross to deny the second admission.
If a claim qualifies as a readmission, based on the criteria outlined below, it will be denied, with further instructions. The provider will have the opportunity to resubmit all services from the original inpatient claim, along with services from the second claim.
If the facility disputes the determination that the readmission criteria was met, a level one appeal can be submitted. The appeal must include medical documentation that supports the rationale for payment of the denied claim. It’s the facility’s responsibility to rebill the original paid claim, combining the readmission services as outlined in the online provider manual.
When a patient is readmitted within 14 days, the following criteria will be used to determine if the first and second admissions match:
- Provider PIN
- Member ID
- Patient date of birth
- The same or similar DRG
The following services will be excluded from the first and second claims when a patient is readmitted within 14 days, based on guidelines from the Centers for Medicare & Medicaid Services:
- Chemo/immunotherapy procedure codes
- Discharge reason codes where patient left against medical advice
- Admissions to inpatient psychiatric, substance abuse, inpatient/outpatient rehabilitation and skilled nursing facilities
For more details, see our Blue Cross Commercial Provider Manual, which you can access through web-DENIS.
How to provide input
According to the Contract Administration Process — part of the Participating Hospital Agreement that went into effect July 1, 2021 — we will allow non-binding input from participating hospitals about this proposal.
Input from facilities is requested by Dec. 31, 2021. Send any input you may have to Liz Bowman at ebowman@bcbsm.com.
After input is received, Blue Cross has 30 calendar days to respond.
Update: CADC, CAADC credentials not required for facilities that treat substance use disorders
What you need to know
Blue Cross Blue Shield of Michigan has reversed a decision requiring that staff treating substance use disorders be certified with specific credentials.
Staff who work at facilities contracted with Blue Cross Blue Shield of Michigan and Blue Care Network for the treatment of substance use disorders aren’t required to have a Certified Alcohol and Drug Counselor, or CADC, or Certified Advanced Alcohol and Drug Counselor, or CAADC, credential.
This reverses our earlier communications on this topic, including an article in the August 2021 issue of The Record, an article in the September-October 2021 issue of BCN Provider News, a web-DENIS message posted July 1, 2021, and a news item posted in July on ereferrals.bcbsm.com.
Reason for the change
After we published the earlier communications, we had additional discussions with our contracted facilities and determined that requiring the CADC or CAADC credential creates hardships for facilities that are trying to recruit staff during the pandemic.
As a result, Blue Cross and BCN are dropping the CADC and CAADC requirement and will defer to the agencies that accredit our contracted facilities, such as the Commission on Accreditation of Rehabilitation Facilities, The Joint Commission and similar agencies, to ensure that standards related to the education and credentialing of facility staff are met.
It’s our hope that this will provide some relief as the pandemic continues and our contracted facilities continue to face challenges in recruiting clinical staff.
This change applies to facilities that treat members who have coverage through these plans:
- Blue Cross commercial
- Medicare Plus Blue℠
- BCN commercial
- BCN Advantage℠
This applies to facilities that provide and bill for one or more of the following types of treatment for substance use disorders:
- Subacute detoxification
- Residential treatment
- Partial hospital program
- Intensive outpatient program
- Individual treatment
Starting Jan. 1, 2022, bill Medicare Advantage plans for administration of COVID‑19 vaccines and monoclonal antibody treatments
Beginning Jan. 1, 2022, the Centers for Medicare & Medicaid services will require Medicare Advantage plans to cover the cost to administer COVID-19 vaccines (including approved booster doses) and monoclonal antibody products to treat COVID-19, with no out-of-pocket costs for members.
For dates of service on or after Jan. 1, 2022, submit claims for the administration of vaccines and monoclonal antibody treatments to Blue Cross Blue Shield of Michigan or Blue Care Network for members with Medicare Plus Blue℠ or BCN Advantage℠ plans.
Note: If your patient scheduled an office visit on or after Jan. 1, 2022, for any other reason than getting the vaccine or monoclonal antibody treatments, bill the usual office visit charge.
More information
For more information on the COVID-19 vaccine, refer to CMS’ COVID-19 toolkit** for health care providers.
For more information on monoclonal antibody treatment, see the Monoclonal Antibody COVID-19 Infusion webpage** of CMS’ COVID-19 toolkit for health care providers.
Reminder
For dates of service on or after Oct. 1, 2021, cost share applies for any treatment related to COVID-19, other than monoclonal antibody treatment, for Medicare Plus Blue and BCN Advantage members.
None of the information in this article is intended to be legal advice and, as such, it remains the providers’ responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Intensive outpatient program and partial hospital program services now payable on an ongoing basis when delivered through telemedicine
As previously communicated, Blue Cross Blue Shield of Michigan and Blue Care Network began allowing behavioral health intensive outpatient and partial hospital program services to be payable when provided by contracted facilities through telemedicine as a temporary measure during the COVID-19 pandemic.
Effective Nov. 1, 2021, we’re updating our Telemedicine Services medical policy to allow these services to be payable when delivered by contracted facility providers through synchronous (real-time) telemedicine on an ongoing basis, rather than as a temporary measure. We’re doing this to make it easier for members to receive these services beyond the COVID-19 pandemic.
For more information, including information about billing for these services, see the Telehealth for behavioral health providers document on our public website at bcbsm.com/coronavirus or within Provider Secured Services.
Reminders
- Facilities can provide behavioral health IOP and PHP services to BCN commercial and BCN Advantage℠ members only when their contracts specifically include IOP and PHP services.
- For Blue Cross commercial members, most plans don’t cover IOP services for mental health or PHP services for substance use disorders. IOP services for substance use disorders must be delivered by a substance abuse treatment facility. Be sure to check member eligibility and benefits through web-DENIS or by contacting Provider Inquiry before performing services.
- For Medicare Plus Blue℠ members, follow Centers for Medicare & Medicaid Services guidance.
Updated documents
We’ve updated the following documents to reflect this change:
- Telehealth for behavioral health providers
- Temporary changes due to the COVID-19 pandemic
You can find these documents on our public website at bcbsm.com/coronavirus or within Provider Secured Services.
You can view the updated Telemedicine Services medical policy through our Medical Policy & Pre-Cert/Pre-Auth Router on bcbsm.com.
Additional autism interventions delivered through telemedicine now payable
As previously communicated, Blue Cross Blue Shield of Michigan and Blue Care Network began allowing some services for autism spectrum disorder to be payable when delivered through telemedicine as a temporary measure during the COVID-19 pandemic.
Effective Nov. 1, 2021, we’re updating our Autism Spectrum Disorder Services medical policy to allow those telemedicine services to be payable on an ongoing basis. We’re also removing restrictions on protocol modification *97155.
These changes apply to members whose coverage includes an autism benefit.
To determine which procedures can be performed through telemedicine for Medicare Plus Blue℠ members who have an autism benefit, see the Medicare-covered telehealth services for the COVID-19 PHE document.
Telemedicine services payable on an ongoing basis, effective Nov. 1
Per the updated medical policy, we’ll allow the following autism services to be delivered through synchronous (real time) telemedicine on an ongoing (no longer temporary) basis:
- Assessment, *97151
- Applied behavior analysis, or ABA, *97153
This service is allowed for children who meet appropriateness criteria. The Guidelines for autism interventions delivered through telemedicine document offers guidance in determining which members can benefit from direct-line ABA interventions delivered through telemedicine.
- Skills training, *97154
- Intensive skills training, *97158
Restrictions lifted on protocol modification
Per the updated medical policy, protocol modification *97155, will be allowed through real-time telemedicine visits 100% of the time. (Previously, this service was allowed to be delivered through telemedicine only 50% of the time.)
During the COVID-19 pandemic, for dates of service from April 14, 2020, through Oct. 31, 2021, we allowed licensed behavior analysts, or LBAs, to troubleshoot treatment protocols directly with the parent or caregiver functioning as the behavioral technician. With the Nov. 1, 2021, update to the Autism Spectrum Disorder medical policy, this temporary measure is no longer payable.
Reminder
The following services continue to be payable when delivered through real-time telemedicine: caregiver training (*97156), multi-family caregiver training (*97157), supervision (S5108) and caregiver training (S5111).
S5108 and S5111 are payable only to Michigan providers who deliver services to out-of-state members and can’t use the American Medical Association category 1 codes.
Updated documents
We’ve updated the following documents to reflect this change:
- Telehealth for behavioral health providers
- Temporary changes due to the COVID-19 pandemic
You can find these documents on our public website at bcbsm.com/coronavirus or within Provider Secured Services.
You can view the updated Telemedicine Services medical policy through our Medical Policy & Pre-Cert/Pre-Auth Router on bcbsm.com.
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Behavioral health services delivered through synchronous telemedicine
With the Nov. 1, 2021, updates to the following medical policies, additional behavioral health and autism spectrum disorder, or ASD, services are now payable when delivered through telemedicine:
- Telemedicine Services
- Autism Spectrum Disorder Services
Behavioral health and ASD services must be delivered synchronously (in real time), with the exception of *96130 and *96156, which can be delivered asynchronously.
Telemedicine asynchronous (store and forward) care generally isn’t payable for behavioral health services.
This applies to Blue Cross Blue Shield of Michigan commercial, Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members.
For more information about providing behavioral health and ASD services through telemedicine, see the Telehealth for behavioral health providers document, which is available on our public website at bcbsm.com/coronavirus or within Provider Secured Services.
You can view the updated medical policies through our Medical Policy &
Pre-Cert/Pre-Auth Router at bcbsm.com.
2022 member ID cards to display deductible, out‑of‑pocket maximum
Effective Jan. 1, 2022, ID cards issued to Blue Cross Blue Shield of Michigan and Blue Care Network commercial members will display their deductible and out-of-pocket maximum. This change applies to both the physical and electronic ID cards. The Consolidated Appropriations Act of 2021 requires us to provide this information on the ID cards issued to participants, beneficiaries or enrollees.
The new CAA mandate requires that issued ID cards contain the following:
- In-network and out-of-network individual and family deductibles
- Out-of-pocket maximums
The following is a sample card image:
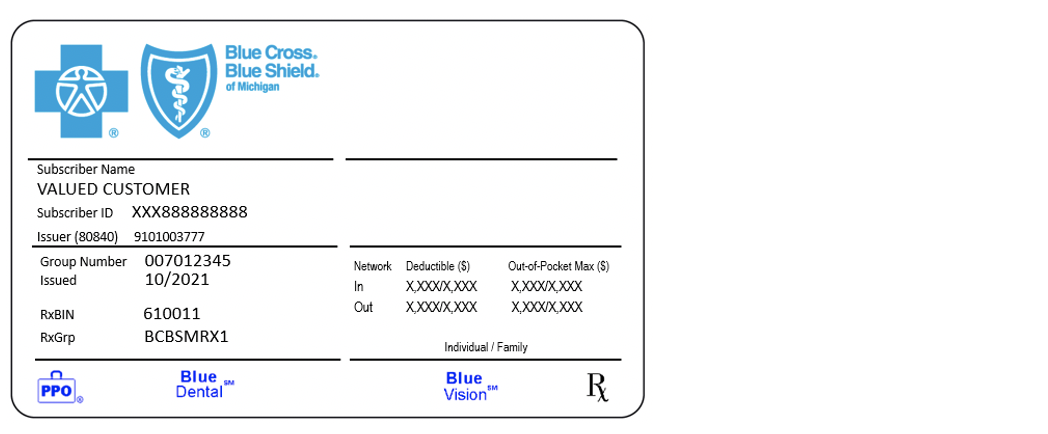
Providers should continue to use webDENIS and PARS for benefit information.
In some cases, where member deductibles or out-of-pocket maximums aren’t available on the card, the card will show “See Benefits.” Members will be directed to access their benefits on bcbsm.com or the BCBSM mobile app.
In addition, for commercial members with prescription drug coverage, their ID cards will also show a new RxBIN to reflect our pharmacy benefit manager change from Express Scripts to OptumRx. This was announced in an article in the September 2021 Record and on Page 26 of the September-October 2021 BCN Provider News.
Our new, updated enrollment flyers assist providers joining our network
We’ve updated some of our enrollment flyers to help providers joining Blue Cross Blue Shield of Michigan or Blue Care Network. The Enrollment documents helpful hints flyers are step-by-step guides that walk providers through each section of their enrollment application. Depending on the classification type, providers may see different form fields on their application. Here are the three available flyers, with information on recent changes:
Reminder: TurningPoint to review sites of care for total hip and knee surgeries for some members
For dates of service on or after Jan. 3, 2022, TurningPoint Healthcare Solutions, LLC will review the site of care for total hip and knee surgeries as part of each authorization determination. Based on medical necessity review, TurningPoint may approve authorization requests for select total hip and knee cases only when scheduled in an outpatient setting.
This applies to members with the following coverage:
- Medicare Plus Blue℠
- BCN commercial
- BCN Advantage℠
If TurningPoint approves an authorization for a hip or knee surgery in an outpatient setting and the member experiences a change in condition that requires an inpatient admission, you’ll need to submit an authorization request for the inpatient admission (procedure code *99222) through the e‑referral system; see the “Submit an inpatient authorization” section of the e-referral User Guide for more information. Blue Cross Blue Shield of Michigan or Blue Care Network will review the request, using InterQual® criteria.
Performing total hip and knee surgeries in outpatient settings is supported by both evidence-based guidelines and the Centers for Medicare & Medicaid Services.
For more information about the TurningPoint musculoskeletal surgical quality and safety management program, see these pages on the ereferrals.bcbsm.com website:
TurningPoint Healthcare Solutions, LLC is an independent company that handles authorizations for musculoskeletal surgical and other related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Additional drugs require prior authorization for URMBT members with Blue Cross non‑Medicare plans
For dates of service on or after Jan. 27, 2022, we’re adding prior authorization requirements for the following drugs covered under the medical benefit for UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans:
- Blenrep™ (belantamab mafodotin-blmf), HCPCS code J9037
- Jemperli™ (dostarlimab-gxly), HCPCS codes J3490, J3590, J9999, C9082
- Monjuvi® (tafasitamab-cxix), HCPCS code J9349
- Zynlonta® (loncastuximab tesirine-lpyl), HCPCS codes J3490, J3590, J9999, C9084
Submit prior authorization requests through AIM Specialty Health®, an independent company that contracts with Blue Cross Blue Shield of Michigan to provide benefit management services.
Prior authorization requirements apply when these drugs are administered in an outpatient setting.
This requirement doesn’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714).
How to submit authorization requests
Submit prior authorization requests to AIM using one of the following methods:
Additional information
Authorization isn’t a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members.
For additional information on requirements related to drugs covered under the medical benefit for UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans, see:
We’ll update the appropriate drug lists to reflect the information in this message prior to the effective date.
Accredo manages prior authorization requests for additional medical benefit drugs. Accredo is an independent company that works with the URMBT on specialty pharmacy services.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Blue Cross will provide physical therapy benefits for GM hourly employees under group number 83200
Effective Jan. 1, 2022, Blue Cross Blue Shield of Michigan will administer outpatient physical therapy benefits to GM hourly populations under group number 83200. TheraMatrix will no longer be the outpatient physical therapy provider for this group.
Members will receive new ID cards in the mail with updated phone numbers so they can contact Customer Service if they have questions. Benefits and coverage will remain the same. Outpatient physical therapy and benefits don’t require a prior authorization. Nonparticipating providers aren’t covered.
On and after Jan. 1, 2022, contact Blue Cross if you have benefit and claims questions. You can also log in to Provider Secured Services to review benefits and submit claims. If you have questions, call Provider Relations and Servicing at the number on the back of the card or one of the following phone numbers:
- Physicians and other professional providers: 1-800-344-8525
- Hospital and facility providers: 1-800-249-5103
For processing or if you have questions about claims dated Dec. 31, 2021, and older, contact TheraMatrix at 1-888-638-8786 or theramatrix.com.** Theramatrix is an independent company that Blue Cross had contracted with to provide physical therapy services.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Register for Transitions of Care Medicare Star measure webinar
Action item
Watch a short video introducing a new Medicare Star measure, and register for a webinar.
The four components of the HEDIS® Transitions of Care measure will be added to the list of Medicare Star measures starting in 2022. Watch this short video about Blue Cross Blue Shield of Michigan and Blue Care Network’s training efforts to help you avoid gaps in care for this measure.
Register and attend a webinar
Learn more about Transitions of Care, including requirements and coding tips. To register, click on a sign-up link below.
Sign up for final live coding webinar of 2021; recent sessions now on‑demand
We’re offering additional webinars that provide updated information on risk adjustment documentation and coding of common challenging diagnoses.
All sessions start at 12:15 p.m. Eastern time and run for 15 to 30 minutes. They also provide physicians and coders with an opportunity to ask questions.
Click on a link below to sign up for a live webinar:
| Session date |
Topic |
Led by |
Sign-up link |
| Thursday, Dec. 9 |
Evaluation and management coding tips |
Coder |
Register here |
You can watch previously hosted sessions on our new provider training site:
| Session date |
On-demand webinar |
| April 20 |
Acute conditions reported in the outpatient setting |
| May 19 |
Morbid (severe) obesity |
| June 17 |
Major depression |
| July 20 |
Diabetes with complication |
| Aug. 18 |
Renal disease |
| Sept. 23 |
Malignant neoplasm |
| Oct. 12 |
Updates for ICD-10 CM |
| Nov. 17 |
Coding scenarios for primary care and specialty |
Access to the training site differs slightly for new and existing users:
Once logged in, users can access the modules in two ways:
- Look in the course catalog under Quality management.
- Enter “lunch and learn” in the search box at the top of the screen.
More information
Provider Experience delivers new on-demand training resources
Action item
Visit our provider training site to find helpful resources. Details on accessing the site can be found below.
Our online, on-demand, provider training courses are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network.
The newest resources include:
- Claims Attachment Process video. This updated video guides you through the process of identifying services that need documentation, locating the Medical Record Routing Form and using it to correctly submit medical records or documentation.
- E-referral tutorials. We’ve made updates to several modules within the series. Tutorials review how to perform major tasks in the e-referral tool to manage referrals and authorizations. This series has moved from ereferrals.bcbsm.com to our new provider training site.
- 2021 lunch and learn webinar recordings. The newest topic added to the series, Updates for 2022 ICD-10 CM codes, reviews key changes for the ICD-10 CM codes and guidelines.
To request access to our training site, follow these steps:
- Open the registration page.
- Complete the registration. We recommend using the same email you use to communicate with Blue Cross and BCN for provider-related needs. This will become your login ID.
- Follow the link to log in.
If you need assistance creating your login ID or navigating the site, contact ProviderTraining@bcbsm.com.

Starting Jan. 1, 2022, bill Medicare Advantage plans for administration of COVID‑19 vaccines and monoclonal antibody treatments
Beginning Jan. 1, 2022, the Centers for Medicare & Medicaid services will require Medicare Advantage plans to cover the cost to administer COVID-19 vaccines (including approved booster doses) and monoclonal antibody products to treat COVID-19, with no out-of-pocket costs for members.
For dates of service on or after Jan. 1, 2022, submit claims for the administration of vaccines and monoclonal antibody treatments to Blue Cross Blue Shield of Michigan or Blue Care Network for members with Medicare Plus Blue℠ or BCN Advantage℠ plans.
Note: If your patient scheduled an office visit on or after Jan. 1, 2022, for any other reason than getting the vaccine or monoclonal antibody treatments, bill the usual office visit charge.
More information
For more information on the COVID-19 vaccine, refer to CMS’ COVID-19 toolkit** for health care providers.
For more information on monoclonal antibody treatment, see the Monoclonal Antibody COVID-19 Infusion webpage** of CMS’ COVID-19 toolkit for health care providers.
Reminder
For dates of service on or after Oct. 1, 2021, cost share applies for any treatment related to COVID-19, other than monoclonal antibody treatment, for Medicare Plus Blue and BCN Advantage members.
None of the information in this article is intended to be legal advice and, as such, it remains the providers’ responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Blue Cross enhances tools for electronically prescribing medications and submitting prior authorizations
Blue Cross Blue Shield of Michigan is committed to enhancing its electronic processes across the health care spectrum, including the processes used by prescribers.
As part of our transition to OptumRx as our new pharmacy benefit manager, we’re making some improvements to our provider-facing tools to assist with prescribing and submitting prior authorizations electronically. These enhancements will primarily take place behind the scenes and won’t have a major effect on how providers prescribe and submit prior authorizations or check on patients’ benefits.
As you read in a September Record article, the move from Express Scripts, Inc. to OptumRx will take place Jan. 1, 2022, for commercial individual and group members, and Jan. 1, 2023, for Medicare Advantage individual and group members.
Continue to use your current electronic medical record system or CoverMyMeds® to submit electronic prior authorizations for Blue Cross and Blue Care Network members. Keep in mind that the BIN number changes to 610011, effective Jan. 1, 2022, for all Blue Cross and BCN commercial members.
Electronic prior authorization, or ePA, replaces faxing and phone calls so you can focus less on administrative tasks and more on patient care. For more information on ePA and CoverMyMeds, see our ePA flyer. Once we launch Availity, our new secure provider portal, we’ll also provide a link to Prompt PA, another resource that can be used to submit electronic prior authorization requests for pharmacy benefit drugs.
Also, continue to use electronic medical records for electronic prescribing and real-time prescription benefit checks. Note: You may have heard of a tool called PreCheck MyScript. This is a product name that OptumRx uses for its real-time benefit check connectivity and programing with electronic medical record systems. From a provider perspective, the interface will look and feel much the same as what providers currently use with Express Scripts.
By using these tools, physicians get patient-specific pharmacy information up front. And the better physicians and patients understand the medication options and costs at the point of prescribing, the more likely patients are to fill prescriptions and adhere to their medication regimen.
The Pharmacy team is communicating about these enhancements at various provider-facing forums, including regional medical director meetings, BCN business administrator meetings and network performance improvement meetings.
If you have any questions, call the Pharmacy Help Desk at 1-800-437-3803.
Additional drugs require prior authorization for URMBT members with Blue Cross non‑Medicare plans
For dates of service on or after Jan. 27, 2022, we’re adding prior authorization requirements for the following drugs covered under the medical benefit for UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans:
- Blenrep™ (belantamab mafodotin-blmf), HCPCS code J9037
- Jemperli™ (dostarlimab-gxly), HCPCS codes J3490, J3590, J9999, C9082
- Monjuvi® (tafasitamab-cxix), HCPCS code J9349
- Zynlonta® (loncastuximab tesirine-lpyl), HCPCS codes J3490, J3590, J9999, C9084
Submit prior authorization requests through AIM Specialty Health®, an independent company that contracts with Blue Cross Blue Shield of Michigan to provide benefit management services.
Prior authorization requirements apply when these drugs are administered in an outpatient setting.
This requirement doesn’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714).
How to submit authorization requests
Submit prior authorization requests to AIM using one of the following methods:
Additional information
Authorization isn’t a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members.
For additional information on requirements related to drugs covered under the medical benefit for UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans, see:
We’ll update the appropriate drug lists to reflect the information in this message prior to the effective date.
Accredo manages prior authorization requests for additional medical benefit drugs. Accredo is an independent company that works with the URMBT on specialty pharmacy services.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
|

 To prepare for moving to the Availity® provider portal in the coming months, you should take a look at the internet browser you’re currently using.
To prepare for moving to the Availity® provider portal in the coming months, you should take a look at the internet browser you’re currently using.