
Subscribe | The Record Archive | Contacts | bcbsm.com
|
April 2025
Health e-Blue update: New requirement to submit quality data for HEDIS measuresWhat you need to know Starting Jan. 1, 2026, there will be changes to the way primary care providers and group administrators submit quality data to Blue Cross Blue Shield of Michigan and Blue Care Network. Primary source verification will be needed for three HEDIS® measures if entered into Health e-Blue℠ in 2026 and for all measures in 2027. Also starting in 2026, all measures manually entered into Health e-Blue must be entered by year-end of the measurement year. We’ll provide more information in future editions of The Record. As part of our ongoing efforts to align with updated federal and accreditation standards, Blue Cross Blue Shield of Michigan and Blue Care Network are announcing important changes about quality data submissions. Effective Jan. 1, 2026, quality data submitted through Health e-Blue℠ for incentive or contract performance must include primary source verification in the form of a medical record for these HEDIS® measures:
In addition, beginning in 2026, Health e-Blue entries for all measures must be completed by Dec. 31 of the measurement year. We’ll no longer accept entries into the following year. Starting on Jan. 1, 2027, Blue Cross and BCN will no longer accept Health e-Blue entries for any measure without primary source verification in the form of a medical record. Later this year, we’ll share more details about this important change, including how to submit the medical record. This change is in direct response to the Centers for Medicare & Medicaid Services and the National Committee for Quality Assurance making significant updates to their quality measurement frameworks. CMS and NCQA are placing increased emphasis on the use of standardized data to ensure consistency, accuracy and comparability across health care organizations. Failure to comply will result in the removal of a closed gap in Health e-Blue, incentives and contracts. Action steps To ensure a smooth transition and compliance with these changes:
We recognize these changes may present challenges, and we’re committed to supporting you through this transition. We’ll provide additional information about this important change in future 2025 editions of The Record. In the meantime, if you have questions or concerns about these new requirements, contact your physician organization or medical care group administrator. They can reach out as needed to their Blue Cross quality improvement performance consultant. Thank you for your partnership and for your continued commitment to delivering high-quality care to our members. HEDIS is also known as the Healthcare Effectiveness Data and Information Set. HEDIS® is a registered trademark of the National Committee for Quality Assurance.
Use our new online tool to enhance your provider directory listingBlue Cross Blue Shield of Michigan now offers Enhanced Provider Data, an online tool available on our provider portal designed to help you strengthen your Blue Cross and Blue Care Network provider directory listing. If you are an independent provider not affiliated with a large health system, you can use Enhanced Provider Data to include additional, personalized information to help patients seeking care better understand you and your practice, including:
How to access To access the Enhanced Provider Data online tool, follow these steps:
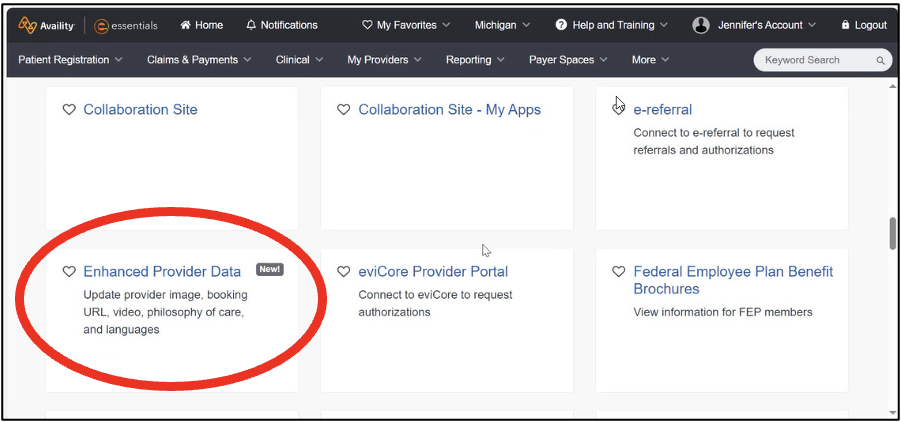
For complete information on how to use the tool, as well as a list of Frequently Asked Questions, click Enhanced Provider Data Guide (PDF). 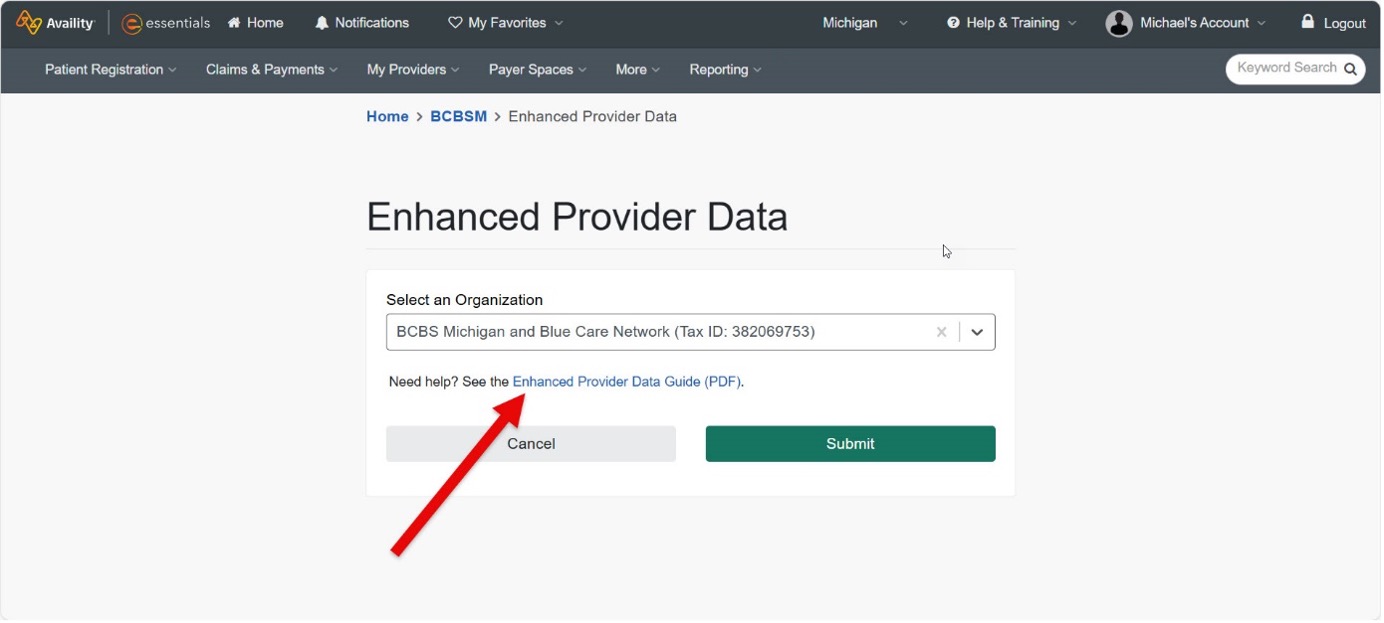 Only independent providers can access Enhanced Provider Data If you’re affiliated with a large health system, your provider directory data may already include these enhanced data points, and you won’t be able to modify or add information using the Enhanced Provider Data tool. Health systems providing enhanced data on behalf of their physicians participating include:
If your health system isn’t listed and you’re not sure whether it participates, send an inquiry to providersearch@bcbsm.com. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Use new telemedicine codes, starting July 1, 2025Blue Cross Blue Shield of Michigan and Blue Care Network commerical will require claims for virtual evaluation and management, or E/M, services to be submitted using new telemedicine procedure codes *98000 through *98015, effective July 1, 2025. Continue to use the telemedicine place of service codes 02 or 10. The telemedicine modifiers aren’t required for the new telemedicine E/M procedure codes. If rendering a virtual E/M service that’s audio-only or audio-video, don’t submit claims for these services using E/M procedure codes *99202 through *99205 or *99212 through *99215 with the telemedicine place of service codes or modifiers. The claims processing systems will be updated to deny these E/M codes when billed with any telemedicine place of service or modifiers as provider liable. The reimbursement amounts for the telemedicine E/M procedure codes *98000 through *98015 and the other outpatient visit E/M procedure codes *99202 through *99205 and *99212 through *99215 are available in the provider portal. Telemedicine synchronous audio-video codes
Telemedicine synchronous audio-only codes
Frequently asked questions Question: Will claims be denied if non-virtual E/M codes are billed using telemedicine place of service codes and modifiers? Q: Will Blue Cross limit virtual services to the use of the new telemedicine E/M procedure codes only? Q: What about the other procedure codes that are billed for telemedicine services that aren’t for an E/M procedure code? Q: Have prior provider communications for these new codes been released? Q: What is the difference in the reimbursement of the current E/M procedure codes and the new telemedicine E/M procedure codes for the Centers for Medicare & Medicaid Services? Q: Will Blue Cross reimburse both the new telemedicine E/M procedure codes and the office and outpatient E/M procedure codes? Q: Will the new telemedicine E/M codes requirement align with current Blue Cross and BCN Telemedicine Services Medical Policy? Q. What is the HMO authorization requirement for telemedicine services for BCN? Q: Does Blue Cross and BCN cover procedure code *98016? None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Reminder: Attest to provider data as requiredWhat you need to know To remain listed in our provider directories, including Find a Doctor, professional practitioners, facilities and organizational (or allied) providers must attest to their information as required. Professional practitioners, facilities and organizational (or allied) health care providers must attest to their information as required to:
Facilities and organizational (allied) providers Every 90 days, facilities and organizational (allied) providers with Type 2 national provider identifiers must update and attest to the following basic provider information in the Provider Data Management tool in our provider portal, Availity Essentials™: name, specialty, address, phone number and digital contact information. Attestation is required even if no changes are needed. This is a requirement of the Consolidated Appropriations Act. To learn more, see the document Update and attest to facility and organizational provider information in the Provider Data Management tool within Availity Essentials. Professional practitioners All professional practitioners, including those who practice at an office location or practice exclusively in an inpatient hospital setting, need to attest to their data. Attestation must be completed in the CAQH Provider Data Portal, formerly known as CAQH ProView®, every 90 and 120 days. Here’s what professional practitioners need to do:
If professional practitioners don’t attest in CAQH as required, they won’t be included in the Blue Cross and BCN provider directories, including our Find a Doctor search tool. If you’re practicing exclusively in an inpatient hospital setting, you must indicate that on your CAQH credentialing application. This information is used to determine whether full credentialing is required. CAQH is a nonprofit alliance of health plans and trade associations focused on simplifying health care administration. Blue Cross and BCN use CAQH to gather and coordinate our professional practitioner credentialing information. All health care practitioners, including hospital-based providers, must be registered with CAQH. If you have questions about CAQH, call the CAQH Solutions Center at 1-888-599-1771, or go to CAQH.org.** For more information on attestation, go to our Provider Data Attestations page. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Pharmacy news roundupWhat you need to know To view all — including the most recent — pharmacy-related provider alerts:
Here are links to pharmacy-related provider alerts from February:
Tip: You can also subscribe to Provider Alerts Weekly to receive a weekly email with links to the previous week’s provider alerts. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Here’s how medical residents can join our networkMedical residents interested in joining our network can submit their Blue Cross Blue Shield of Michigan or Blue Care Network provider enrollment application up to 60 days before they complete their training. It’s important to apply within the required time frame. If medical residents apply more than 60 days before the completion of residency training, we’ll deny the application and residents will have to reapply. The CAQH Provider Data Portal** (known as CAQH ProView) application must be completed to begin the credentialing process with Blue Cross and BCN. To keep CAQH information current, complete the re-attestation every 120 days and update the Authorize section. Visit the CAQH Provider Data Portal** for more information on application requirements. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Do you know about our BlueCard processes?At Blue Cross Blue Shield of Michigan, we want to ensure that health care providers have the information they need about BlueCard®. This national program enables members of one Blue plan to obtain health care services while traveling or living in another Blue plan's service area. About BlueCard The program links participating health care providers with independent Blue plans across the United States and in more than 200 countries and territories worldwide through a single electronic network for claims processing and reimbursement. The BlueCard program lets you conveniently submit claims for members from other Blue plans, including international Blue plans, directly to Blue Cross Blue Shield of Michigan. Blue Cross is your single point of contact for all your claims-related questions. Verifying coverage and eligibility When a member from an out-of-state Blue plan (the home plan) requests care and presents a current Blue plan's identification card, before providing services, you (as the service provider for the host plan), should:
Members with coverage from a Blue plan may also present a debit card, which may be Blue-branded, to cover cost-sharing payments. BlueCard Eligibility Call Center Call the BlueCard Eligibility Call Center at 1-800-676-2583. State the three-character alpha-numeric prefix on the patient's ID card, and you’ll be connected with the patient's home plan to verify eligibility and benefits for health care coverage. Prior authorization You have the following options for determining prior authorization requirements:
Timely filing All original facility claims must be reported to Blue Cross within 12 months from the date of service, and all original professional claims must be reported to Blue Cross within 180 days of the date of service. All claim adjustment requests for both professional and facility claims must be billed to Blue Cross within 24 months of the date of service. For more details, including information on how to submit claims for various services, see the “BlueCard Program” chapter of the Blue Cross Commercial Provider Manual. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
2025 CPT 1st-quarter update: New, deleted codesThe American Medical Association has added 21 new 2025 proprietary laboratory analyses codes as part of its CPT update. The codes, effective dates and Blue Cross Blue Shield of Michigan’s coverage decisions are below. Laboratory and pathology/proprietary laboratory analyses
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Billing chart: Blue Cross highlights medical, benefit policy changesYou’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the “Billing chart.” The billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures. We’ll publish information about new Blue Cross groups or changes to group benefits under the Group Benefit Changes heading. For more detailed descriptions of Blue Cross’ policies for these procedures, check under the Commercial Policy tab in Benefit Explainer on Availity Essentials™. To access this online information:
To view the “April 2025 Billing chart,” click here. **Blue Cross Blue Shield of Michigan doesn’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
PGIP, Blueprint allocations to change July 1What you need to know PGIP and Blueprint for Affordability allocations are changing starting July 1. Starting July 1, 2025, the Physician Group Incentive Program and Blueprint for Affordability allocations will change to further our support of value-based opportunities for professional health care providers The Blueprint allocation will be reduced from 1.5% to 1%. PGIP allocation will increase from 6% to 6.5%. The total allocation percentage will remain the same. This will be applied to all provider specialties associated with medical doctors, doctors of osteopathy, chiropractors, podiatrists and fully licensed psychologists. Providers contractually agree in their participation agreements to allocate a portion of their reimbursement to PGIP. As a reminder, all funds allocated are distributed to eligible organizations that participate in PGIP to support physician practice and system transformation. Blue Cross Blue Shield of Michigan doesn’t retain any money for administrative costs. Visit our Value Partnerships webpage to learn more about PGIP. Note: Claims for Blue Cross and Blue Shield Federal Employee Program® members are excluded from the PGIP allocation.
Blue Cross’ updates to practitioner fees will take effect July 1Blue Cross Blue Shield of Michigan will change practitioner fees for services provided on or after July 1, 2025. This change applies to services provided to our Traditional, TRUST and Blue Preferred Plus℠ members, regardless of the customer group. Blue Cross will use the 2025 Medicare resource-based relative value scale for most relative value unit priced procedures for dates of service on and after July 1. Most fees are currently priced using the 2024 values. The Blue Cross overall fee update includes base fee adjustments and value-based reimbursement. Due to significant changes in relative value unit valuations, it’s best to review the fee schedule to view the effect on an individual code or group of codes. Fee schedules effective July 1 will be available on the Provider Resources site through our provider portal on Availity Essentials™. To find the fee schedules:
Only claims submitted with dates of service on or after July 1 will be reimbursed at the new fees. **Blue Cross Blue Shield of Michigan doesn’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services.
Clinical editing updates: Modifiers, inappropriate diagnosis combinationsIn support of correct coding and payment accuracy, we are providing the information below to keep you informed about forthcoming payment policy updates, new policies and coding reminders. Blue Cross Blue Shield of Michigan commercial Reminder: Anatomical modifiers are required when billing for surgical procedures Anatomical modifiers identify the specific area of the body where a procedure is performed. Surgical procedures requiring anatomical modifiers include CPT codes in the range *10000 through *69999 that have a Medicare Physician Fee Schedule bilateral indicator “1,” denoting that the surgical code is eligible to be billed on both sides of the body. Claims may be denied when anatomical modifiers (50, LT, RT, E1, E2, E3, E4, F1, F2, F3, F4, F5, F6, F7, F8, F9, FA, T1, T2, T3, T4, T5, T6, T7, T8, T9, TA, LC, LD, RC, LM, RI) are appropriate, but haven’t been appended to the claim line. This applies to professional claims. Anatomical modifiers required for PCI procedures Percutaneous coronary intervention, or PCI, is a procedure used to open blocked arteries. PCI codes should be reported with one of the five anatomical PCI modifiers to specify which vessel is being treated. Claims submitted for PCI procedures without one of the coronary vessel modifiers LC, LD, LM, RC or RI may be denied. Medicare Plus Blue℠ PPO Surgical procedure anatomical modifiers on facility claims Anatomical modifiers will be required when surgical procedures are billed on outpatient facility claims. When an anatomical modifier is missing or incorrect, the claim may be denied. The editing has been in place for professional claims since November 2021. The facility version of this edit was implemented in March 2025. Reminder: Inappropriate modifier to diagnosis combination When an ICD-10-CM diagnosis code has a specified anatomical laterality within the code description, the anatomical modifier that is appended to the CPT or HCPCS code must correspond to the laterality within the ICD-10-CM description. Claim lines may be denied that have a laterality diagnosis submitted with a CPT or HCPCS modifier that doesn’t correspond to the diagnosis code. This applies to professional claims. Reminder: Inappropriate diagnosis combinations The current ICD-10-CM official guidelines state, “An Excludes 1 note indicates that the code excluded should never be used at the same time as the code above the Excludes 1 note. An Excludes 1 is used when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition. These conditions are mutually exclusive code combinations.” Claim lines reported with mutually exclusive code combinations may be denied. This applies to both professional and facility claims. Blue Care Network commercial and BCN Advantage℠ HMO E/M services with modifier 25 denied in error Evaluation and management services with modifier 25 reported with codes *94010 through *94781 are receiving a g33 denial in error. BCN has evaluated the code pair update that took effect in the third quarter of 2024 by the Centers for Medicare & Medicaid Services and has decided to allow modifier 25 to be recognized. Claims denied in error can be resubmitted after March 23, 2025, for reprocessing of payment. Please don’t submit appeals. BCN Advantage Modifier JW and JZ Drug codes that were appropriately reported with modifier JW and JZ that were denied QPL before Feb. 1, 2025, will be reprocessed for payment. The inappropriate denial was updated in our claims system at the end of January. None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
How to find out which procedure codes require prior authorization by TurningPointWe’ve retired the Musculoskeletal procedure codes that require authorization by TurningPoint document. To determine which procedure codes require prior authorization, open Procedure codes for which providers must request prior authorization. Here’s what you need to know:
This applies to the following lines of business:
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Here’s detailed information about our Multiple Therapy Procedure Reduction policyIn the October 2024 Record, we let you know that we were planning to implement the Multiple Therapy Procedure Reduction, or MTPR, policy in 2025. The policy will apply to claims with dates of service on and after April 1, 2025. Health care providers are responsible for submitting accurate claims. This policy is designed to ensure reimbursement aligns with correct coding and industry standards. The Blue Cross Blue Shield of Michigan reimbursement policies incorporate guidelines from the Current Procedural Terminology, or CPT®, the Centers for Medicare & Medicaid Services and other relevant coding frameworks. This policy applies to claims billed on CMS-1500 and UB-04 forms. It reflects CMS methodology, regulatory requirements, contract terms, benefit design and medical policies. Blue Cross reserves the right to modify this policy at any time by publishing updates on its website. Overview Certain physical medicine and rehabilitation therapy procedures frequently reported together on the same date of service include overlapping practice expense components, such as:
To align with CMS guidelines, Blue Cross applies a multiple therapy procedure reduction to the practice expense portion of secondary and subsequent therapy procedures provided on the same date by the same physician, facility or other qualified health care professional. Reimbursement guidelines Ranking and reduction of procedures Blue Cross follows CMS guidelines for determining which procedures are subject to the reduction and how they are ranked:
This reduction applies when one or both of the following happens:
The reduction doesn’t apply to therapy services for behavioral health conditions (ICD-10 codes beginning with an F). Procedure ranking methodology The CMS non-facility PE RVU is used to determine the primary procedure:
Example calculation
Frequently asked questions Question: How is the PE portion of a service determined? Answer: The practice expense portion is calculated by taking the PE RVU/total RVU ratio and applying it to the allowed amount. Q: If multiple therapy specialists (physical, occupational, speech-language pathology) provide services on the same day, will the reduction apply? A: Yes, if all services are billed under the same physician or other qualified health care professional, reductions will apply according to CMS guidelines. Q: How are codes ranked if they share the same PE RVU? A: If two or more codes have identical PE RVUs, the total RVU is used to rank them. Documentation requirements Providers must submit accurate and complete claims following industry coding standards, including:
Claims are subject to coding audits, benefit coverage reviews and medical policy assessments.
Medicare Advantage prior authorization requests submitted through NovoLogix must be submitted through different application, starting July 1Starting July 1, 2025, health care providers will need to submit prior authorization requests for medical benefit drugs that are currently submitted using the NovoLogix® online tool through a different application. This applies to Medicare Plus Blue℠ and BCN Advantage℠ members. The new application is called the Medical and Pharmacy Drug PA Portal. Providers will be able to access it through our provider portal, Availity Essentials™. Blue Cross Blue Shield of Michigan and Blue Care Network will continue to manage the prior authorization requirements for these drugs. Continue to submit these prior authorization requests through NovoLogix through June 30, 2025. Watch for additional communications about training opportunities and resources for the application. Note: We previously announced a similar change for commercial members. See the Jan. 3, 2025, provider alert for details. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. NovoLogix is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network.
Announcing changes to management of oncology medical benefit drugsWe’re adding more oncology medical benefit drugs to our Oncology Value Management program administered by OncoHealth. Starting June 1, health care providers should submit prior authorization requests to OncoHealth for the drugs mentioned below. Notes:
Requirements for new drugs — for commercial and Medicare Advantage members For dates of service on or after June 1, the drugs listed below will have requirements for Blue Cross Blue Shield of Michigan commercial, Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members. Note: Site-of-care requirements apply only to commercial members.
Changes to requirements For dates of service on or after June 1, providers will need to submit prior authorization requests through OncoHealth for the drugs listed below. The drugs will be managed under the Oncology Value Management program. Currently, providers submit prior authorization requests for these drugs through the NovoLogix® online tool, unless otherwise noted. For commercial and Medicare Advantage members Starting June 1, prior authorization requests for the following drugs will be managed by OncoHealth for both commercial and Medicare Advantage members.
For commercial members only Starting June 1, prior authorizations for the following drugs will be managed by OncoHealth for commercial members. (Currently, providers submit prior authorization requests for these drugs through the NovoLogix online tool.) Note: For Medicare Advantage members, these drugs are already managed by OncoHealth.
Courses of treatment that start before June 1 and continue beyond June 1 Commercial members who have authorizations that were approved before June 1 for the drugs discussed above can continue to receive therapy until their authorizations expire. Prior authorization is required through OncoHealth only if there’s a change to the treatment plan on or after June 1, or if treatment with the drug extends beyond the authorization end date. Removal of prior authorization requirement — for commercial members only For dates of service on or after June 1, Avzivi® (bevacizumab-tnjn) won’t require prior authorization for Blue Cross commercial or BCN commercial members. Note: To determine the requirement for Avzivi for Medicare Advantage members, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members. Additional information For more information about the Oncology Value Management program, including information about the members who have requirements under the program and how to submit requests to OncoHealth, see the Oncology Value Management program through OncoHealth: FAQs for providers document and the following pages on ereferrals.bcbsm.com: **For commercial members, drugs may be covered only when administered at the following sites of care: doctor’s or other health care provider’s office; the member's home, administered by a home infusion therapy provider; or an ambulatory infusion center. Site-of-care requirements don’t apply to Medicare Advantage members. NovoLogix is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network. OncoHealth is an independent company supporting Blue Cross Blue Shield of Michigan and Blue Care Network by providing cancer support services.
Changes to Oncology Value Management program will start April 1As we previously announced, starting April 1, 2025, oncology pharmacy benefit drugs will be managed through our Oncology Value Management program. Starting April 1, health care providers can submit prior authorization requests for these drugs to OncoHealth, which administers the Oncology Value Management program. Currently, only oncology medical benefit drugs are managed through the Oncology Value Management program. Adding oncology pharmacy benefit drugs to the program will:
When requesting prior authorization, OncoHealth requires that providers submit the entire drug regimen to determine medical necessity. This means providers must include all drugs in the request — those that require prior authorization and those that don’t. In addition, while reviewing clinical documentation, OncoHealth may add to the request any drugs that weren’t requested, to capture the entire regimen. Check member benefits With the April 1 expansion of the Oncology Value Management program, prior authorization requirements are changing for some commercial members. This is because some members whose employer groups didn’t participate in the Oncology Value Management program prior to April 1 will have requirements under the program for dates of service on or after April 1. As always, be sure to check benefits for all members before providing services. Drug lists By April 1, we’ll update the following drug lists to specify the oncology pharmacy benefit drugs that require prior authorization through OncoHealth.
Where to find the authorization number to include on claims When submitting claims, include the nine-digit OncoHealth authorization reference number, which is included on all OncoHealth approval letters. To locate the reference number in OncoHealth’s OneUM™ portal:
How to determine billable units for a drug OncoHealth approves drug regimens based on dose, frequency and duration of the authorization. While billable units aren’t displayed in the OneUM portal, providers can see the approved number of cycles and frequency within the case summary. To find this information in OncoHealth’s OneUM portal:
Availability of providers in OncoHealth’s OneUM portal If provider offices are unable to submit a prior authorization request through the OncoHealth OneUM portal because the ordering provider isn’t listed in the portal, email the OncoHealth Client Support Team at clientsupport@oncohealth.us. The team will add the provider. Courses of treatment that start before April 1 and continue beyond April 1 Members who start receiving oncology pharmacy benefit drugs before April 1 can continue to receive those drugs under their approved authorization until it expires. Prior authorization is required through OncoHealth only if there’s a change to the treatment plan on or after April 1, or if treatment with the drug extends beyond the authorization end date. Recorded training Providers who didn’t attend an OncoHealth provider training session or would like a refresher on the submission process can watch the recorded OncoHealth presentation on our Provider Training site. To access the recorded training:
If you need help with accessing or navigating the site, email ProviderTraining@bcbsm.com. Additional information By April 1, we’ll update the Oncology Value Management program through OncoHealth: FAQs for providers document to reflect the information in this alert. If you have issues while working in OncoHealth’s OneUM portal, email the OncoHealth Client Support Team at clientsupport@oncohealth.us. As a reminder, prior authorization requests for oncology pharmacy benefit drugs are currently submitted through an electronic prior authorization tool, such as CoverMyMeds®, and are managed by the Blue Cross and BCN pharmacy departments. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. OncoHealth is an independent company supporting Blue Cross Blue Shield of Michigan and Blue Care Network by providing cancer support services.
We’ll use updated ABA supplemental policy, starting April 22For dates of service on or after April 22, 2025, Blue Cross Behavioral Health℠ will use the updated Applied Behavioral Analysis (ABA) Supplemental Policy when making determinations on prior authorization requests. We made the following changes in the updated policy:
Blue Cross Behavioral Health manages prior authorizations for behavioral health services for:
To view the updated policy, see the Behavioral Health Services section on either of the following webpages on bcbsm.com:
We’re changing how we communicate medical policy changes for medical benefit drugs that require prior authorization for commercial membersCurrently, we publish provider alerts to announce medical policy changes for medical benefit drugs that require prior authorization for Blue Cross Blue Shield of Michigan and Blue Care Network commercial members. Effective immediately, we’ll publish these changes in a new document titled Changes to medical necessity criteria for prior authorizations for medical benefit drugs. When there are medical policy changes that affect prior authorization requirements, we’ll update the document to include:
Check the document regularly for the latest information about these changes.
Ahzantive, Enzeevu, Epysqli, Pavblu to require prior authorization for Medicare Advantage members, starting May 1For dates of service on or after May 1, 2025, the following drugs will require prior authorization for Medicare Plus Blue℠ and BCN Advantage℠ members:
Submit prior authorization requests through the NovoLogix® online tool when these drugs will be billed as a medical benefit. When prior authorization is required These drugs will require prior authorization when they are administered by a health care provider in sites of care such as outpatient facilities or physician offices and are billed in one of the following ways:
How to access NovoLogix To access NovoLogix, log in to our provider portal at availity.com,** click on Payer Spaces in the menu bar, then click on the BCBSM and BCN logo. You’ll find links to the NovoLogix tools on the Applications tab. Note: If you need to request access to our provider portal, follow the instructions on the For Providers: Register for Web Tools page at bcbsm.com/providers. List of requirements For a list of requirements related to drugs covered under the medical benefit, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members. We’ll update this list before the effective date. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. NovoLogix is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network.
Alyglo, Amtagvi, Loqtorzi to have requirements for Blue Cross commercial URMBT members, starting June 1For dates of service on or after June 1, 2025, the drugs listed below will have requirements for UAW Retiree Medical Benefits Trust members with Blue Cross Blue Shield of Michigan non‑Medicare plans. Submit requests using the online tools indicated below.
These requirements apply only when these drugs are administered in an outpatient setting. Submit prior authorization requests through the NovoLogix® online tool or the Carelon Medical Benefits Management provider portal when these drugs will be billed as a medical benefit. Note: The requirements don’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714). How to submit authorization requests To submit requests, log in to our provider portal at availity.com,*** click on Payer Spaces in the menu bar, and then click on the BCBSM and BCN logo. On the Applications tab, click the tile to open the appropriate tool. If you need to request access to our provider portal, see the Register for Web Tools webpage on bcbsm.com. For drugs that have a site-of-care requirement, you’ll be prompted to select a site of care when you submit prior authorization requests. If the request meets clinical criteria for the drug and is for one of the following sites of care, it will be approved automatically:
More about requirements for medical benefit drugs For additional information on requirements related to drugs covered under the medical benefit for UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans, see:
We’ll update the pertinent drug lists to reflect the information in this message before the effective date. As a reminder, prior authorization isn’t a guarantee of payment. Health care providers need to verify eligibility and benefits for members. **As communicated in a Jan. 3, 2025, provider alert, health care providers will need to submit prior authorization requests for medical benefit drugs that are currently submitted through the NovoLogix® online tool through a different application. This applies to dates of service on or after April 1, 2025. ***Blue Cross Blue Shield of Michigan doesn’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services. For more information, go to our ereferrals.bcbsm.com website. NovoLogix® is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network.
Trazimera to be preferred trastuzumab product for Medicare Advantage members, starting May 12Preferred and nonpreferred trastuzumab products are changing for Medicare Plus Blue℠ and BCN Advantage℠ members for dates of service on or after May 12, 2025. The preferred trastuzumab product will be Trazimera® (trastuzumab-qyyp), HCPCS code Q5116. Health care providers will have to show that our Medicare Advantage members have tried and failed Trazimera when requesting prior authorization for the following nonpreferred drugs:
Trazimera will continue to require prior authorization. Submit prior authorization requests to OncoHealth when these drugs will be billed as a medical benefit. When prior authorization is required These drugs require prior authorization, as applicable, when they are administered by a health care provider in sites of care such as outpatient facilities or physician offices and are billed in one of the following ways:
How to submit prior authorization requests Submit prior authorization requests to OncoHealth using one of the following methods:
List of requirements For a list of requirements related to drugs covered under medical benefits, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members. We’ll update this list prior to the effective date. ***Blue Cross Blue Shield of Michigan doesn’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. OncoHealth is an independent company supporting Blue Cross Blue Shield of Michigan and Blue Care Network by providing cancer support services.
Webinars for physicians, coders focus on documentation, codingAction item Register for our 2025 monthly Lunch & Learn webinars focusing on coding and documentation. In 2025, we’ll continue to offer webinars about documentation and coding of common challenging diagnoses. These live, lunchtime educational sessions will also include an opportunity to ask questions. Below is our schedule and topics for the sessions. All sessions start at noon Eastern time and should last for 30 minutes. Register for the sessions on the provider training website.
Provider training website access If you have an Availity Essentials™ account you can access the provider training website by:
Existing users who used the same email address as their provider portal profile email will be directed to the training site. If you used a different email address, contact ProviderTraining@bcbsm.com to update your profile. You can also directly access the training website if you don’t have a provider portal account. After logging in to the provider training website, look in Event Calendar to sign up for your desired session. You can also quickly search for all the sessions with the keyword “lunchtime” and then look under the results for Events. You can listen to the previously recorded sessions, too. Check out the following:
Questions?
**Blue Cross Blue Shield of Michigan doesn’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Register now for 2025 virtual provider symposium sessionsThis year’s virtual health care provider symposiums start in May. They’ll focus on quality measures and review of evaluation and management guidelines. Registration is now open on the provider training website. Physicians, physician assistants, nurse practitioners, nurses and coders can receive continuing education credits for attending. Once logged in to the provider training site, open the event calendar to sign up for any of the sessions listed below. All times are Eastern time. All Star Performance-HEDIS®/Star Rating Measure Overview: The Golden Star Awards For physicians and office staff responsible for closing gaps in care related to quality measures for adults
Conducting an Internal Chart Audit: Livestreaming with April For physicians, coders, billers and administrative staff
How to register on the provider training website Provider portal users with an Availity Essentials™ account can access the provider training website:
You can also directly access the training website if you don’t have a provider portal account. Questions?
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. HEDIS® is a registered trademark of the National Committee for Quality Assurance. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. Accreditation statement: This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of the Minnesota Medical Association and Blue Cross Blue Shield of Michigan. The Minnesota Medical Association (MMA) is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. CME statement: The Minnesota Medical Association designates this internet live activity for a maximum of 2 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Questionnaire changes in e-referralWe made changes to questionnaires in the e-referral system Feb. 23, 2025, as indicated in the tables below. We also updated the document Preview questionnaires and medical necessity criteria (previously titled Authorization criteria and preview questionnaires) on the ereferrals.bcbsm.com website to reflect these changes. As a reminder, we use the pertinent medical necessity criteria and your answers to the questionnaires in the e-referral system when making utilization management determinations on your prior authorization requests. Questionnaire updates We’ve updated the following questionnaires in the e-referral system.
Questionnaires removed The following questionnaires were removed from the e-referral system.
Preview questionnaires and medical necessity criteria In the document titled Preview questionnaires and medical necessity criteria, you’ll find the following:
Talk to Medicare Advantage members about how to maintain independence, confidenceTo help our Medicare Plus Blue℠ and BCN Advantage℠ members remain independent and feel confident as they age, we’re asking them to talk to their health care providers about the following issues:
We want our Medicare Advantage members to feel comfortable and confident sharing their concerns with you. We’re suggesting they write them down and read from the list or hand it to you so you can start the conversation. We also encourage you to discuss these issues with patients even if they don’t initiate the conversation. Many patients don’t ask questions about these topics because they forget, don’t know what to ask, are embarrassed or assume they have to “live with it.” When you bring up these topics, it opens the door to a conversation that may not otherwise happen. It helps your patients know these are common issues and what types of questions they should ask going forward. We appreciate your efforts to make members as comfortable as possible when discussing these sensitive issues.
Access resources for closing early prenatal care, childhood immunizations gaps in careThis is part of an ongoing series of articles focusing on the tools and resources available to help FEP® members manage their health. Here are some resources to help close gaps in care for the Healthcare Effectiveness Data and Information Set, or HEDIS®, measures Prenatal & Postpartum Care (PPC) and Childhood Immunization Status (CIS). Prenatal care To help providers close gaps in care for the prenatal care portion of the PPC measure, Blue Cross Blue Shield of Michigan developed a Prenatal Care (PPC) tip sheet. The tip sheet has information on measure compliance, helpful HEDIS hints and tips for coding. To help members prepare for a healthy and safe pregnancy, the Blue Cross and Blue Shield Federal Employee Program® developed a Your Pregnancy To-Do List flyer for pregnant patients to use during their pregnancies. Childhood immunizations Blue Cross Blue Shield of Michigan also developed a CIS tip sheet to help providers close gaps in care for childhood immunizations. This tip sheet includes information on exclusions, compliance and helpful HEDIS hints. The Centers for Disease Control and Prevention 2025 Recommended Immunizations** chart is now available. This chart can help parents stay on track with their children’s immunizations. If health care providers and members have questions about FEP benefits, they can call Customer Service at 1-800-482-3600 for Federal Employee Health Benefits or 1-877-760-8574 for Postal Service Health Benefits, or go online to fepblue.org. **Blue Cross Blue Shield of Michigan doesn’t own or control this website. HEDIS®, which stands for Healthcare Effectiveness Data and Information Set, is a registered trademark of the National Committee for Quality Assurance, or NCQA.
How to appeal Cotiviti’s DRG cross-claim clinical reviewsCotiviti, an independent company that provides claim reviews for Blue Cross Blue Shield of Michigan and Blue Care Network, is conducting diagnosis-related group cross-claim clinical reviews, or CCCRs, for Medicare Plus Blue℠ and BCN Advantage℠ inpatient claims. The reviews will focus on the member's episode of care as explained in a March 2024 article in The Record. Initial review and notification Cotiviti selects claims to review without medical records. If Cotiviti identifies an adjustment opportunity, it will notify health care providers by mail. If you disagree with Cotiviti's decision, you have 50 calendar days to submit a written appeal request. Appeals process Submit written appeal requests through Cotiviti's Provider Connection Portal or refer to your audit finding letter for the mail or fax addresses.
If you have questions, contact Cotiviti Provider Relations at 770-379-2009 from 8 a.m. to 5 p.m. Eastern time, Monday through Friday.
Clinical editing updates: Modifiers, inappropriate diagnosis combinationsIn support of correct coding and payment accuracy, we are providing the information below to keep you informed about forthcoming payment policy updates, new policies and coding reminders. Blue Cross Blue Shield of Michigan commercial Reminder: Anatomical modifiers are required when billing for surgical procedures Anatomical modifiers identify the specific area of the body where a procedure is performed. Surgical procedures requiring anatomical modifiers include CPT codes in the range *10000 through *69999 that have a Medicare Physician Fee Schedule bilateral indicator “1,” denoting that the surgical code is eligible to be billed on both sides of the body. Claims may be denied when anatomical modifiers (50, LT, RT, E1, E2, E3, E4, F1, F2, F3, F4, F5, F6, F7, F8, F9, FA, T1, T2, T3, T4, T5, T6, T7, T8, T9, TA, LC, LD, RC, LM, RI) are appropriate, but haven’t been appended to the claim line. This applies to professional claims. Anatomical modifiers required for PCI procedures Percutaneous coronary intervention, or PCI, is a procedure used to open blocked arteries. PCI codes should be reported with one of the five anatomical PCI modifiers to specify which vessel is being treated. Claims submitted for PCI procedures without one of the coronary vessel modifiers LC, LD, LM, RC or RI may be denied. Medicare Plus Blue℠ PPO Surgical procedure anatomical modifiers on facility claims Anatomical modifiers will be required when surgical procedures are billed on outpatient facility claims. When an anatomical modifier is missing or incorrect, the claim may be denied. The editing has been in place for professional claims since November 2021. The facility version of this edit was implemented in March 2025. Reminder: Inappropriate modifier to diagnosis combination When an ICD-10-CM diagnosis code has a specified anatomical laterality within the code description, the anatomical modifier that is appended to the CPT or HCPCS code must correspond to the laterality within the ICD-10-CM description. Claim lines may be denied that have a laterality diagnosis submitted with a CPT or HCPCS modifier that doesn’t correspond to the diagnosis code. This applies to professional claims. Reminder: Inappropriate diagnosis combinations The current ICD-10-CM official guidelines state, “An Excludes 1 note indicates that the code excluded should never be used at the same time as the code above the Excludes 1 note. An Excludes 1 is used when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition. These conditions are mutually exclusive code combinations.” Claim lines reported with mutually exclusive code combinations may be denied. This applies to both professional and facility claims. Blue Care Network commercial and BCN Advantage℠ HMO E/M services with modifier 25 denied in error Evaluation and management services with modifier 25 reported with codes *94010 through *94781 are receiving a g33 denial in error. BCN has evaluated the code pair update that took effect in the third quarter of 2024 by the Centers for Medicare & Medicaid Services and has decided to allow modifier 25 to be recognized. Claims denied in error can be resubmitted after March 23, 2025, for reprocessing of payment. Please don’t submit appeals. BCN Advantage Modifier JW and JZ Drug codes that were appropriately reported with modifier JW and JZ that were denied QPL before Feb. 1, 2025, will be reprocessed for payment. The inappropriate denial was updated in our claims system at the end of January. None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
How to find out which procedure codes require prior authorization by TurningPointWe’ve retired the Musculoskeletal procedure codes that require authorization by TurningPoint document. To determine which procedure codes require prior authorization, open Procedure codes for which providers must request prior authorization. Here’s what you need to know:
This applies to the following lines of business:
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Here’s detailed information about our Multiple Therapy Procedure Reduction policyIn the October 2024 Record, we let you know that we were planning to implement the Multiple Therapy Procedure Reduction, or MTPR, policy in 2025. The policy will apply to claims with dates of service on and after April 1, 2025. Health care providers are responsible for submitting accurate claims. This policy is designed to ensure reimbursement aligns with correct coding and industry standards. The Blue Cross Blue Shield of Michigan reimbursement policies incorporate guidelines from the Current Procedural Terminology, or CPT®, the Centers for Medicare & Medicaid Services and other relevant coding frameworks. This policy applies to claims billed on CMS-1500 and UB-04 forms. It reflects CMS methodology, regulatory requirements, contract terms, benefit design and medical policies. Blue Cross reserves the right to modify this policy at any time by publishing updates on its website. Overview Certain physical medicine and rehabilitation therapy procedures frequently reported together on the same date of service include overlapping practice expense components, such as:
To align with CMS guidelines, Blue Cross applies a multiple therapy procedure reduction to the practice expense portion of secondary and subsequent therapy procedures provided on the same date by the same physician, facility or other qualified health care professional. Reimbursement guidelines Ranking and reduction of procedures Blue Cross follows CMS guidelines for determining which procedures are subject to the reduction and how they are ranked:
This reduction applies when one or both of the following happens:
The reduction doesn’t apply to therapy services for behavioral health conditions (ICD-10 codes beginning with an F). Procedure ranking methodology The CMS non-facility PE RVU is used to determine the primary procedure:
Example calculation
Frequently asked questions Question: How is the PE portion of a service determined? Answer: The practice expense portion is calculated by taking the PE RVU/total RVU ratio and applying it to the allowed amount. Q: If multiple therapy specialists (physical, occupational, speech-language pathology) provide services on the same day, will the reduction apply? A: Yes, if all services are billed under the same physician or other qualified health care professional, reductions will apply according to CMS guidelines. Q: How are codes ranked if they share the same PE RVU? A: If two or more codes have identical PE RVUs, the total RVU is used to rank them. Documentation requirements Providers must submit accurate and complete claims following industry coding standards, including:
Claims are subject to coding audits, benefit coverage reviews and medical policy assessments.
Clarification: Blue Cross, BCN will no longer separately pay providers for services performed by bedside nurses, starting March 1We originally communicated about this in a January 2025 Record article, but we are providing additional information within the first paragraph for clarification purposes. Please keep this version for your records. Effective March 1, 2025, Blue Cross Blue Shield of Michigan and Blue Care Network will no longer separately pay health care providers on inpatient facility claims for services performed by a bedside nurse. This policy currently only applies to inpatient facility claims that are eligible for a catastrophic cost outlier payment and where Blue Cross or BCN reviews the medical record and itemized bill. Our updated payment policy isn’t intended to affect decision-making for patient care, and health care providers are expected to apply independent medical judgment when caring for all members. This policy applies to inpatient facility claims that meet the above criteria submitted for Blue Cross and BCN commercial members. Background Nursing services are prescribed by a physician or non-physician practitioner for the assessment, treatment and monitoring of patients. This policy pertains to all services performed by a bedside nurse in all prescribed settings (for example, emergency room, regular room and board, intensive care unit or operating room). Policy The following list provides examples of nursing services that aren’t separately payable on inpatient facility claims when performed by a bedside nurse, as they are inclusive to the room and board, treatment area or lab. This list is not an all-inclusive list.
Clarification: Blue Cross, BCN will no longer separately pay providers for services performed by respiratory therapists, starting March 1We originally communicated about this in a January 2025 Record article, but we are providing additional information within the first paragraph for clarification purposes. Please keep this version for your records. Effective March 1, 2025, Blue Cross Blue Shield of Michigan and Blue Care Network will no longer separately pay health care providers for services performed by respiratory therapists on inpatient facility claims. This policy currently only applies to inpatient facility claims that are eligible for a catastrophic cost outlier payment and where Blue Cross or BCN reviews the medical record and itemized bill. This payment policy isn’t intended to affect decision-making for care of the patient, and health care providers are expected to apply independent medical judgment when caring for all members. This policy applies to inpatient facility claims that meet the above criteria submitted for Blue Cross and BCN commercial members. Background Respiratory therapy services are services prescribed by a physician or a non-physician practitioner for the assessment and diagnostic evaluation, treatment, management and monitoring of patients with deficiencies and abnormalities of cardiopulmonary function. This policy pertains to services performed by a respiratory therapist in all prescribed settings (for example, an emergency room, regular room and board, intensive care unit or operating room). All respiratory services performed by a nurse are considered part of the room and board or treatment area. Policy The following list provides examples of respiratory therapy services that aren’t separately payable on the inpatient facility claim, as they are inclusive to the respiratory modality, room and board, treatment area or laboratory. This list is not an all-inclusive list.
Medicare Advantage prior authorization requests submitted through NovoLogix must be submitted through different application, starting July 1Starting July 1, 2025, health care providers will need to submit prior authorization requests for medical benefit drugs that are currently submitted using the NovoLogix® online tool through a different application. This applies to Medicare Plus Blue℠ and BCN Advantage℠ members. The new application is called the Medical and Pharmacy Drug PA Portal. Providers will be able to access it through our provider portal, Availity Essentials™. Blue Cross Blue Shield of Michigan and Blue Care Network will continue to manage the prior authorization requirements for these drugs. Continue to submit these prior authorization requests through NovoLogix through June 30, 2025. Watch for additional communications about training opportunities and resources for the application. Note: We previously announced a similar change for commercial members. See the Jan. 3, 2025, provider alert for details. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. NovoLogix is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network.
Announcing changes to management of oncology medical benefit drugsWe’re adding more oncology medical benefit drugs to our Oncology Value Management program administered by OncoHealth. Starting June 1, health care providers should submit prior authorization requests to OncoHealth for the drugs mentioned below. Notes:
Requirements for new drugs — for commercial and Medicare Advantage members For dates of service on or after June 1, the drugs listed below will have requirements for Blue Cross Blue Shield of Michigan commercial, Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members. Note: Site-of-care requirements apply only to commercial members.
Changes to requirements For dates of service on or after June 1, providers will need to submit prior authorization requests through OncoHealth for the drugs listed below. The drugs will be managed under the Oncology Value Management program. Currently, providers submit prior authorization requests for these drugs through the NovoLogix® online tool, unless otherwise noted. For commercial and Medicare Advantage members Starting June 1, prior authorization requests for the following drugs will be managed by OncoHealth for both commercial and Medicare Advantage members.
For commercial members only Starting June 1, prior authorizations for the following drugs will be managed by OncoHealth for commercial members. (Currently, providers submit prior authorization requests for these drugs through the NovoLogix online tool.) Note: For Medicare Advantage members, these drugs are already managed by OncoHealth.
Courses of treatment that start before June 1 and continue beyond June 1 Commercial members who have authorizations that were approved before June 1 for the drugs discussed above can continue to receive therapy until their authorizations expire. Prior authorization is required through OncoHealth only if there’s a change to the treatment plan on or after June 1, or if treatment with the drug extends beyond the authorization end date. Removal of prior authorization requirement — for commercial members only For dates of service on or after June 1, Avzivi® (bevacizumab-tnjn) won’t require prior authorization for Blue Cross commercial or BCN commercial members. Note: To determine the requirement for Avzivi for Medicare Advantage members, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members. Additional information For more information about the Oncology Value Management program, including information about the members who have requirements under the program and how to submit requests to OncoHealth, see the Oncology Value Management program through OncoHealth: FAQs for providers document and the following pages on ereferrals.bcbsm.com: **For commercial members, drugs may be covered only when administered at the following sites of care: doctor’s or other health care provider’s office; the member's home, administered by a home infusion therapy provider; or an ambulatory infusion center. Site-of-care requirements don’t apply to Medicare Advantage members. NovoLogix is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network. OncoHealth is an independent company supporting Blue Cross Blue Shield of Michigan and Blue Care Network by providing cancer support services.
Changes to Oncology Value Management program will start April 1As we previously announced, starting April 1, 2025, oncology pharmacy benefit drugs will be managed through our Oncology Value Management program. Starting April 1, health care providers can submit prior authorization requests for these drugs to OncoHealth, which administers the Oncology Value Management program. Currently, only oncology medical benefit drugs are managed through the Oncology Value Management program. Adding oncology pharmacy benefit drugs to the program will:
When requesting prior authorization, OncoHealth requires that providers submit the entire drug regimen to determine medical necessity. This means providers must include all drugs in the request — those that require prior authorization and those that don’t. In addition, while reviewing clinical documentation, OncoHealth may add to the request any drugs that weren’t requested, to capture the entire regimen. Check member benefits With the April 1 expansion of the Oncology Value Management program, prior authorization requirements are changing for some commercial members. This is because some members whose employer groups didn’t participate in the Oncology Value Management program prior to April 1 will have requirements under the program for dates of service on or after April 1. As always, be sure to check benefits for all members before providing services. Drug lists By April 1, we’ll update the following drug lists to specify the oncology pharmacy benefit drugs that require prior authorization through OncoHealth.
Where to find the authorization number to include on claims When submitting claims, include the nine-digit OncoHealth authorization reference number, which is included on all OncoHealth approval letters. To locate the reference number in OncoHealth’s OneUM™ portal:
How to determine billable units for a drug OncoHealth approves drug regimens based on dose, frequency and duration of the authorization. While billable units aren’t displayed in the OneUM portal, providers can see the approved number of cycles and frequency within the case summary. To find this information in OncoHealth’s OneUM portal:
Availability of providers in OncoHealth’s OneUM portal If provider offices are unable to submit a prior authorization request through the OncoHealth OneUM portal because the ordering provider isn’t listed in the portal, email the OncoHealth Client Support Team at clientsupport@oncohealth.us. The team will add the provider. Courses of treatment that start before April 1 and continue beyond April 1 Members who start receiving oncology pharmacy benefit drugs before April 1 can continue to receive those drugs under their approved authorization until it expires. Prior authorization is required through OncoHealth only if there’s a change to the treatment plan on or after April 1, or if treatment with the drug extends beyond the authorization end date. Recorded training Providers who didn’t attend an OncoHealth provider training session or would like a refresher on the submission process can watch the recorded OncoHealth presentation on our Provider Training site. To access the recorded training:
If you need help with accessing or navigating the site, email ProviderTraining@bcbsm.com. Additional information By April 1, we’ll update the Oncology Value Management program through OncoHealth: FAQs for providers document to reflect the information in this alert. If you have issues while working in OncoHealth’s OneUM portal, email the OncoHealth Client Support Team at clientsupport@oncohealth.us. As a reminder, prior authorization requests for oncology pharmacy benefit drugs are currently submitted through an electronic prior authorization tool, such as CoverMyMeds®, and are managed by the Blue Cross and BCN pharmacy departments. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. OncoHealth is an independent company supporting Blue Cross Blue Shield of Michigan and Blue Care Network by providing cancer support services.
We’re changing how we communicate medical policy changes for medical benefit drugs that require prior authorization for commercial membersCurrently, we publish provider alerts to announce medical policy changes for medical benefit drugs that require prior authorization for Blue Cross Blue Shield of Michigan and Blue Care Network commercial members. Effective immediately, we’ll publish these changes in a new document titled Changes to medical necessity criteria for prior authorizations for medical benefit drugs. When there are medical policy changes that affect prior authorization requirements, we’ll update the document to include:
Check the document regularly for the latest information about these changes.
Ahzantive, Enzeevu, Epysqli, Pavblu to require prior authorization for Medicare Advantage members, starting May 1For dates of service on or after May 1, 2025, the following drugs will require prior authorization for Medicare Plus Blue℠ and BCN Advantage℠ members:
Submit prior authorization requests through the NovoLogix® online tool when these drugs will be billed as a medical benefit. When prior authorization is required These drugs will require prior authorization when they are administered by a health care provider in sites of care such as outpatient facilities or physician offices and are billed in one of the following ways:
How to access NovoLogix To access NovoLogix, log in to our provider portal at availity.com,** click on Payer Spaces in the menu bar, then click on the BCBSM and BCN logo. You’ll find links to the NovoLogix tools on the Applications tab. Note: If you need to request access to our provider portal, follow the instructions on the For Providers: Register for Web Tools page at bcbsm.com/providers. List of requirements For a list of requirements related to drugs covered under the medical benefit, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members. We’ll update this list before the effective date. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. NovoLogix is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network.
Alyglo, Amtagvi, Loqtorzi to have requirements for Blue Cross commercial URMBT members, starting June 1For dates of service on or after June 1, 2025, the drugs listed below will have requirements for UAW Retiree Medical Benefits Trust members with Blue Cross Blue Shield of Michigan non‑Medicare plans. Submit requests using the online tools indicated below.
These requirements apply only when these drugs are administered in an outpatient setting. Submit prior authorization requests through the NovoLogix® online tool or the Carelon Medical Benefits Management provider portal when these drugs will be billed as a medical benefit. Note: The requirements don’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714). How to submit authorization requests To submit requests, log in to our provider portal at availity.com,*** click on Payer Spaces in the menu bar, and then click on the BCBSM and BCN logo. On the Applications tab, click the tile to open the appropriate tool. If you need to request access to our provider portal, see the Register for Web Tools webpage on bcbsm.com. For drugs that have a site-of-care requirement, you’ll be prompted to select a site of care when you submit prior authorization requests. If the request meets clinical criteria for the drug and is for one of the following sites of care, it will be approved automatically:
More about requirements for medical benefit drugs For additional information on requirements related to drugs covered under the medical benefit for UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans, see:
We’ll update the pertinent drug lists to reflect the information in this message before the effective date. As a reminder, prior authorization isn’t a guarantee of payment. Health care providers need to verify eligibility and benefits for members. **As communicated in a Jan. 3, 2025, provider alert, health care providers will need to submit prior authorization requests for medical benefit drugs that are currently submitted through the NovoLogix® online tool through a different application. This applies to dates of service on or after April 1, 2025. ***Blue Cross Blue Shield of Michigan doesn’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services. For more information, go to our ereferrals.bcbsm.com website. NovoLogix® is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network.
Trazimera to be preferred trastuzumab product for Medicare Advantage members, starting May 12Preferred and nonpreferred trastuzumab products are changing for Medicare Plus Blue℠ and BCN Advantage℠ members for dates of service on or after May 12, 2025. The preferred trastuzumab product will be Trazimera® (trastuzumab-qyyp), HCPCS code Q5116. Health care providers will have to show that our Medicare Advantage members have tried and failed Trazimera when requesting prior authorization for the following nonpreferred drugs:
Trazimera will continue to require prior authorization. Submit prior authorization requests to OncoHealth when these drugs will be billed as a medical benefit. When prior authorization is required These drugs require prior authorization, as applicable, when they are administered by a health care provider in sites of care such as outpatient facilities or physician offices and are billed in one of the following ways:
How to submit prior authorization requests Submit prior authorization requests to OncoHealth using one of the following methods:
List of requirements For a list of requirements related to drugs covered under medical benefits, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members. We’ll update this list prior to the effective date. ***Blue Cross Blue Shield of Michigan doesn’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. OncoHealth is an independent company supporting Blue Cross Blue Shield of Michigan and Blue Care Network by providing cancer support services.
Questionnaire changes in e-referralWe made changes to questionnaires in the e-referral system Feb. 23, 2025, as indicated in the tables below. We also updated the document Preview questionnaires and medical necessity criteria (previously titled Authorization criteria and preview questionnaires) on the ereferrals.bcbsm.com website to reflect these changes. As a reminder, we use the pertinent medical necessity criteria and your answers to the questionnaires in the e-referral system when making utilization management determinations on your prior authorization requests. Questionnaire updates We’ve updated the following questionnaires in the e-referral system.
Questionnaires removed The following questionnaires were removed from the e-referral system.
Preview questionnaires and medical necessity criteria In the document titled Preview questionnaires and medical necessity criteria, you’ll find the following:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||