Subscribe | The Record Archive | Contacts | bcbsm.com
|
March 2021
Blue Cross and BCN educate members about the COVID‑19 vaccineBlue Cross Blue Shield of Michigan and Blue Care Network are encouraging members to obtain the COVID‑19 vaccine when they have the opportunity to do so. Here’s how we’re communicating with our members about the vaccine:
These communications are designed to allay concerns about obtaining the vaccine and answer questions about cost and access. We encourage you to connect with your patients who are eligible to receive the vaccine to answer any questions they may have. We told you in our February issue that Blue Cross and BCN members have no out‑of‑pocket costs for obtaining the COVID‑19 vaccine. We also have information on vaccines for providers on our Coronavirus (COVID‑19) information updates for providers webpages within our secure provider website, as well as on our public website at bcbsm.com/coronavirus. Quick billing information can be found in our COVID‑19 vaccine billing information at a glance document.
We’re migrating to a new platform for electronic transmissionsBlue Cross Blue Shield of Michigan is moving to a new SFTP file transfer platform, Edifecs, for your electronic transmissions (such as 837 claims, 277CA transactions and reports, 835 ERA, 999 acknowledgements and capitation reports). We plan to retire the current SFTP file transfer platform, EDDI, this year. To ensure there are no interruptions to your claim submissions, we ask that you follow the migration schedule provided to you.
We’re attaching a Technical Info Sheet and FAQ document to the email so you’ll know what actions you’ll need to take. If you have any questions about this move, email EDIMigration@bcbsm.com. Note: If any of your information has changed (email, vendors, contact information, etc.), email us at EDIMigration@bcbsm.com so we can update it as soon as possible. Include your submitter ID with your inquiry.
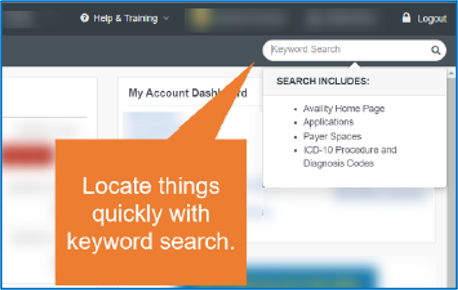
Get ready for Availity: How to use new search feature
Availity has a keyword search field in the upper right corner of the page. Here are some of the items you can find using the search feature:
Note: You can find them by code or a portion of the code name. The search feature isn’t case sensitive, but you’ll need to spell the word correctly for the system to find what you’re searching for. So, if you remember seeing a resource or an announcement, but don’t remember where it was, type in a keyword and Availity will help you find it.
Questions? If you need immediate assistance or have a question specific to a certain member or situation, use our website resources or contact Provider Inquiry. Web resources:
Provider Inquiry numbers are available at bcbsm.com/providers. Click on Contact Us. Then click on the type of provider you are, and click on Provider Inquiry. Call the Blue Cross Web Support Help Desk at 1‑877‑258‑3932 if you have problems with the current Blue Cross provider portal. Previous articles about Availity
Blue Cross and BCN to collaborate with OptumRx for pharmacy benefit management servicesBlue Cross Blue Shield of Michigan, Blue Care Network and OptumRx will be working together to give members, health care providers and employers prescription drug benefit services that are expected to improve the pharmacy experience, drive better health outcomes and lower costs. The collaboration will take effect Jan. 1, 2022, for commercial individual and group members, and Jan. 1, 2023, for Medicare Advantage individual and group members. As a leading pharmacy care services provider, OptumRx will augment Blue Cross’ existing programs, bringing new tools and digital technology designed to better manage the overall drug spend and increase member engagement in pharmaceutical treatment. The OptumRx integrated health and wellness service platform complements Blue Cross’ integrated benefit solutions. Through this collaboration, OptumRx will support administration of pharmacy claims, manage rebate contracting with pharmaceutical manufacturers, provide mail-order dispensing and manage Blue Cross’ pharmacy networks. “Holding the line on steadily increasing pharmacy costs and ensuring members have access to the prescriptions they need are top priorities for Blue Cross,” said Blue Cross President and CEO Daniel J. Loepp. “We’re confident our collaboration with OptumRx will help us move closer to reaching those goals through affordable, innovative solutions that improve care within our communities.” The collaboration advances Blue Cross’ commitment to providing members with convenient and affordable access to prescription medications, with no disruption to current members, through a comprehensive retail and home delivery pharmacy network. Leveraging OptumRx’s expertise, negotiated contracts and network of more than 68,000 pharmacies, this collaboration will expand access and significantly improve prescription drug pricing and rebates, offering members and group customers more value and cost savings. OptumRx will provide enhanced customer service technology integrated with member communications to ensure a smooth exchange of information. An updated website and new mobile app will also place individualized coverage details at each member’s fingertips for quick and convenient access to cost and benefit information. Blue Cross will continue to work closely with its current pharmacy benefit provider, Express Scripts Inc., to ensure a successful and seamless transition. We’ll provide more details later in the year as we get closer to the transition date.
New members to be issued alphanumeric subscriber IDs starting Feb. 27We’ll issue alphanumeric subscriber IDs to all new Blue Cross Blue Shield of Michigan and Blue Care Network members, starting Feb. 27, 2021. The start date was communicated in a web‑DENIS message posted Feb. 24. We announced in the June Record that we’d be transitioning to alphanumeric IDs this year, but the start date wasn’t available at that time. We’ll use the letter M after the prefix to begin the alphanumeric ID, followed by eight numbers. For example, a new subscriber ID could look like this: XYZM91234567. When you see one of these ID cards and check benefits and eligibility on web‑DENIS, you’ll enter the last nine characters of the subscriber ID. These de‑identified IDs are being used to avoid duplication with subscribers’ Social Security numbers, align with other health plans and automate manual processes previously used when correcting duplicate numbers. There are currently no plans to change subscriber IDs for existing members.
Check for messages in e‑referral to finalize your pending requestsYou can help us complete the processing of your requests for authorization — and improve turnaround time — by checking the e-referral system for messages and responding quickly. We may reach out to you using the Case Communication feature in e-referral for additional information, including clinical documentation, that we need to process your requests. Refer to the e‑referral User Guide sections about case communication for instructions.
CPT and HCPCS updateThere’s been a change in the coverage decision and benefit category for HCPCS code C9770 and a change in coverage for CPT code *55880 since we communicated about the codes in the February Record. Following is updated information:
HCPCS replacement codes establishedJ1823 replaces J3490 and J3590 when billing for Uplizna (inebilizumab‑cdon) The Centers for Medicare & Medicaid Services has established a permanent procedure code for specialty medical drug Uplizna® (inebilizumab‑cdon). All services through Dec. 31, 2020, will continue to be reported with codes J3490 and J3590. All services performed on and after Jan. 1, 2021, must be reported with J1823. Prior authorization is required for all groups unless they are opted out of the prior authorization program. For groups that have opted out of the prior authorization program, this code is covered for the FDA‑approved indications. J7352 replaces J3490 and J3590 when billing for Scenesse (afamelanotide injectable implant) The Centers for Medicare & Medicaid Services has established a permanent procedure code for specialty medical drug Scenesse (afamelanotide injectable implant). All services through Dec. 31, 2020, will continue to be reported with codes J3490 and J3590. All services performed on and after Jan. 1, 2021, must be reported with J7352. Prior authorization is required for all groups unless they are opted out of the prior authorization program. For groups that have opted out of the prior authorization program, this code is covered for the FDA‑approved indications. J9144 replaces J3490, J3590 and C9062 when billing for Darzalex FasPro (daratumumab and hyaluronidase-fihj) The Centers for Medicare & Medicaid Services has established a permanent procedure code for specialty medical drug Darzalex FasPro™ (daratumumab and hyaluronidase‑fihj). All services through Dec, 31, 2020, will continue to be reported with codes J3490 and J3590. Facilities can continue to report C9062 through Dec. 31, 2020. All services performed on and after Jan. 1, 2021, must be reported with J9144. J9223 replaces J3490 and when billing for Zepzelca (lurbinectedin) The Centers for Medicare & Medicaid Services has established a permanent procedure code for specialty medical drug Zepzelca (lurbinectedin). All services through Dec. 31, 2020, will continue to be reported with code J3490. All services performed on and after Jan. 1, 2021, must be reported with J9223. J9281 replaces J9999 and C9064 when billing for Jelmyto (mitomycin) The Centers for Medicare & Medicaid Services has established a permanent procedure code for specialty medical drug Jelmyto™ (mitomycin). All services through Dec. 31, 2020, will continue to be reported with code J9999 and facilities can continue to report C9064 through Dec. 31, 2020. All services performed on and after Jan. 1, 2021, must be reported with J9281. J9316 replaces J3590 when billing for Phesgo (pertuzumab, trastuzumab and hyaluronidase‑zzxf) The Centers for Medicare & Medicaid Services has established a permanent procedure code for specialty medical drug Phesgo (pertuzumab, trastuzumab and hyaluronidase‑zzxf). All services through Dec. 31, 2020, will continue to be reported with code J3590. All services performed on and after Jan. 1, 2021 must be reported with J9316. J9317 replaces J3590 and C9066 for Trodelvy (sacituzumab govitecan‑hziy) The Centers for Medicare & Medicaid Services has established a permanent procedure code for specialty medical drug Trodelvy™ (sacituzumab govitecan‑hziy). All services through Dec. 31, 2020, will continue to be reported with code J3590. Facilities can continue to report C9066 through Dec. 31, 2020. All services performed on and after Jan. 1, 2021, must be reported with J9317. S0013 replaces J3490 and J3590 when billing for Spravato (esketamine) The Centers for Medicare & Medicaid Services has established a permanent procedure code for specialty medical drug Spravato® (esketamine). All services through Dec. 31, 2020, will continue to be reported with codes J3490 and J3590. All services performed on and after Jan. 1, 2021, must be reported with S0013. Prior authorization is required for all groups unless they are opted out of the prior authorization program. For groups that have opted out of the prior authorization program, this code is covered for the FDA‑approved indications. Billing chart: Blues highlight medical, benefit policy changesYou’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart. This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures. You will also see that descriptions for the codes are no longer included. This is a result of recent negotiations with the AMA on use of the codes. We will publish information about new BCBS groups or changes to group benefits under the Group Benefit Changes heading. For more detailed descriptions of the BCBSM policies for these procedures, please check under the Medical/Payment Policy tab in Explainer on web-DENIS. To access this online information:
What’s included in The Record’s Pharmacy categoryWe recently received some questions about Record articles included in the newsletter’s Pharmacy category. The Pharmacy category is used for articles pertaining to both pharmacy drugs and medical benefit drugs. Our Pharmacy Services department manages both the pharmacy drug benefit and the medical drug benefit for members. However, as you know, medical drugs are billed as medical claims because they’re administered by health professionals. Drugs purchased by our members at a pharmacy are billed by the pharmacy that dispenses the drug. Drug‑related articles also may appear in other categories to reflect where they’re being billed and administered. For example, they may be included in the Professional category or the Facility category or both, depending on whether they’re billed by doctor’s offices, hospitals or both. That’s because we want to be sure that billers know of any changes related to these drugs and how we cover them. Our Record newsletter is organized by category, including Professional, Facility, Pharmacy, DME and All Providers. The All Providers category is used for articles that are likely to be of interest to all our providers. Each issue of the newsletter doesn’t necessarily include articles in every category. If you’re not already subscribed, you can subscribe to The Record or other provider newsletters by clicking here. By subscribing, the newsletter will arrive in your email on the last business day of each month.
We made changes to our Telehealth procedure codes for COVID‑19 chartWe removed certain Current Procedural Terminology codes from the commercial section of our Telehealth procedure codes for COVID‑19 document to better reflect the more general language in our policy on telemedicine. We also removed CPT codes from the Medicare Advantage sections of the document, and are referring providers to the Centers for Medicare & Medicaid Services’ Covered Telehealth Services for PHE for the COVID‑19 pandemic list** for the billable services allowed for our Medicare Advantage members. To save you the time of having to download the ZIP file from the CMS link above, we provide a PDF of the Medicare‑covered telehealth services list on our website. We review this list monthly and will provide any updates from CMS as necessary. For the most recent Medicare‑covered telehealth services, refer to the list on CMS’ website. You’ll find the PDF and the following informative documents in the Telehealth section of our COVID‑19 webpages on our public website at bcbsm.com/coronavirus and through Provider Secured Services:
Medicare Advantage cost‑sharing reminder **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
We’ve resolved attribution issue related to COVID‑19 testingLast year, Blue Cross Blue Shield of Michigan released billing guidelines for COVID‑19 testing in a web‑DENIS alert titled “Billing recommendations for COVID‑19 testing, including drive through.” In these guidelines, we instructed primary care providers to bill the evaluation and management code *99211 plus the diagnosis code Z20.828 for observing a self-administered specimen collection for COVID‑19 testing in new or established patients. When *99211 was billed by a primary care physician in an office setting, the event was included in the Blue Cross “attribution algorithm,” which assigns members to a primary care physician. When using this code as part of the algorithm, it was possible for a member to be attributed to a primary care physician when the physician was only testing for COVID‑19. This issue was brought to our attention, and we subsequently updated our attribution algorithm to exclude any claims that have both the CPT code *99211 and diagnosis code Z20.828. The update was made before the October membership freeze. All year‑end reporting, including Blueprint for Affordability and value-based reimbursement analytics, will use the corrected attribution algorithm. January 2021 reporting includes the updated attribution. Previous attribution lists won’t be restated. Physician organization administrators can submit questions about this issue to the PGIP Collaboration Site, which can be accessed in the provider area of bcbsm.com.
Medical benefit specialty drug prior authorization list changing in April for most membersStarting in April 2021, we’re adding prior authorization requirements for some drugs covered under the medical benefit. Providers must request prior authorization through AIM Specialty Health®. For dates of service on or after April 15, 2021, the following drug will require prior authorization for UAW Retiree Medical Benefits Trust PPO non-Medicare members:
For dates of service on or after April 22, 2021, the following drugs will require prior authorization for Blue Cross Blue Shield of Michigan commercial fully insured members and for Blue Care Network commercial, Medicare Plus Blue℠ and BCN Advantage℠ members:
These requirements don’t apply to members of the Blue Cross and Blue Shield Federal Employee Program® and MESSA. Submit authorization requests to AIM through the AIM provider portal** or by calling the AIM Contact Center at 1‑844‑377‑1278. For information about registering for and accessing the AIM ProviderPortal, see the Frequently Asked Questions page** on the AIM website. More about the authorization requirements Authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. For more information on requirements related to drugs covered under the medical benefit, see:
We’ll update these lists to reflect these changes prior to the effective dates. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Procedure codes *71271 and *33208 don’t require authorization for most membersServices associated with radiology CPT code *71271 and cardiology CPT code *33208 don’t require authorization for these members:
We’ve removed these procedure codes from the document, Procedures that require prior authorization by AIM Specialty Health®: Cardiology, radiology (high technology) and sleep studies (in lab).
We’re planning to update our clinical edits for Medicare Advantage PPO claimsBlue Cross Blue Shield of Michigan Medicare Advantage PPO will update clinical edits applied to claims starting in June or shortly thereafter. We’re enhancing the edits as part of our efforts to promote correct coding for claims. These improvements will help ensure that our claim payment policies align with nationally recognized sources of information and are easy to understand. They’ll also help us better meet the needs of a changing health care industry while maintaining alignment with national coding guidelines. MA PPO medical and payment policies will continue to comply with:
Some of the enhancements include, but are not limited to:
As with the application of all our clinical edits, the guidelines and regulations of these sources should be followed:
As the enhancements draw closer, we’ll provide updates. The appeal process won’t change with the expanded edits, but new edit codes will be published in the coming months. Continue to submit appeals on the Clinical Editing Appeal Form with the necessary supporting documentation. And remember to continue to fax one appeal at a time to avoid processing delays.
eviCore will no longer mail Practice Profile summaries and category information for outpatient physical therapy services starting in JulyBeginning with July 2021 data, eviCore will no longer mail paper copies of the Practice Profile Summary, which includes information about your assigned category, to health care providers. Instead, eviCore will post category updates on the first business day of February and August each year beginning in August 2021. Follow these steps to access your Practice Profile Summary and obtain your category:
If you believe there are circumstances adversely affecting your utilization data, you may still request reconsideration within 15 days of eviCore’s notification. Initiate your reconsideration request within the UM Category window. Additional information is available on the evicore.com** website as follows:
You can also contact Provider and Client Services at 1‑800‑646‑0418 for more information. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Optum to handle credit recovery efforts for Blue Cross and BCNEffective Jan. 1, 2021, Optum® has been assigned to identify and recover credit balance overpayments on behalf of Blue Cross Blue Shield of Michigan and Blue Care Network claims. Previously, these reviews may have been conducted by Conduent, formerly known as CDR Associates. Any review initiated by Conduent that is in progress will be completed by Conduent with an estimated completion date of February 2021. Optum conducts periodic claim reviews at provider locations. They’re a professional health care consulting firm that has focused on assisting both providers and payers by identifying and processing credit balances. Reviews only involve patient accounting records, not medical records. Claim recoveries will be handled through claims offset, not check refunds. Additionally, claims data will be available through a web-based tool for providers who choose to submit credit balance recoveries through Optum’s overpayment management tool. Note: For Medicare Plus Blue℠ overpayments, providers may continue to submit a Request for offset of a Medicare Advantage overpayment form directly to Blue Cross using the existing process. This involves identifying the reason for the overpayment of a medical claim paid through IKA. The claim is then adjusted in IKA, resulting in an offset of future claim payments.
Blue Cross and BCN Pharmacy to cover additional childhood vaccines, starting March 1To increase access to childhood vaccines and decrease the risk of vaccine‑preventable disease outbreaks among children, Blue Cross Blue Shield of Michigan and Blue Care Network Pharmacy Services is adding the following vaccines to its list of covered vaccines, starting March 1, 2021:
The following lists all the vaccines currently covered under eligible members’ prescription drug plans. Most Blue Cross commercial, non‑Medicare members with prescription drug coverage are eligible. If a member meets the coverage criteria, we cover the vaccine with no cost share.
If a member doesn’t meet the age requirement for a vaccine, Blue Cross won’t cover the vaccine under the prescription drug plan and the claim will reject. Certified, trained, qualified registered pharmacists must administer vaccines.
We’ve added site‑of‑care requirements for Uplizna for Blue Cross commercial membersEffective Jan. 1, 2021, Blue Cross Blue Shield of Michigan has added site‑of‑care requirements for Uplizna® (inebilizumab‑cdon), HCPCS code J1823. This drug is covered under the medical benefit for our commercial members. Encourage your patients who have Blue Cross commercial coverage to select one of the following infusion locations instead of using a hospital outpatient facility:
If members currently receive infusions for these drugs at a hospital outpatient facility, providers must:
Override for infusions received from Jan. 1 through Feb. 18 However, you can receive an override for these dates of service so the claim will pay. To inquire about an override, call the Pharmacy Clinical Help Desk at 1‑800‑437‑3803. For dates of service on or after Feb. 19, all members must receive infusions at a covered infusion location, unless the provider obtains prior authorization for receiving the infusion at a hospital outpatient facility location. More about authorization requirements Note: Uplizna already has site‑of‑care requirements for Blue Care Network commercial members for dates of service on or after Aug. 1, 2020. Authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. List of requirements
Additional information
Virtual provider symposiums to focus on patient experience, HEDIS, documentation and codingWe’ve tentatively scheduled this year’s provider symposiums virtually throughout May and June for physicians, office staff and coders. Save the dates below and keep in mind that you’ll be able to register for more than one session. We’ll publish the registration links in the April Record. These sessions are for physicians and office staff responsible for closing gaps in care related to quality measures and creating a positive patient experience:
These sessions are for physicians and office staff responsible for closing gaps in care related to quality measures and creating a positive patient experience:
Nurses and coders can receive continuing education credits for attending the sessions. HEDIS® is a registered trademark of the National Committee for Quality Assurance.
Lunch and learn webinars for physicians and coders focus on risk adjustment, codingSign up now for live, monthly, lunchtime webinars focusing on risk adjustment and coding. Starting in April, these educational sessions will update you on documentation and coding of common challenging diagnoses. You’ll also have an opportunity to ask questions. April through September’s webinars are led by physicians. The last three sessions of the year focus on coding guideline updates and are led by coders. While the session topics could change, our current schedule and tentative topics follow. All sessions start at 12:15 p.m. Eastern time and generally run for 15 to 30 minutes. Click on a Register here link below to sign up for a session.
If you have any questions about the sessions, contact April Boyce at aboyce@bcbsm.com. If you have questions regarding registration, email Patricia Scarlett at pscarlett@bcbsm.com.
Reminder: Sign up for additional training webinarsProvider Experience is continuing its series of training webinars for health care providers and staff. The webinars are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network. Here’s information on the upcoming training webinars:
The Blue Cross 201 webinar series provides an in‑depth learning opportunity and builds on information shared in our Blue Cross 101: Understanding the Basics webinar. This session reviews the processes and tools available when submitting professional claims. Recordings of previous webinars are available on web‑DENIS through the Blue Cross Provider Publications and Resources or BCN Provider Publications and Resources pages as follows: Blue Cross Provider Publications and Resources
You can also get more information about online training, presentations and videos by clicking on the E‑Learning icon at the top of the page. BCN Provider Publications and Resources
As additional training webinars become available, we’ll provide notices through web‑DENIS, The Record and BCN Provider News.
Reminder: Refer Blue Cross FEP members to Blue Cross Blue Shield of Michigan network providersWhen Blue Cross and Blue Shield Federal Employee Program® members are referred to out‑of‑network providers, they’re at risk of having to pay higher costs. Be sure to follow the directions in your Blue Cross Blue Shield of Michigan provider agreement and Blue Cross provider manual, instructing you to refer your Blue Cross patients to network providers. Our goal is to:
To verify if a provider is in the Blue Cross network for your patient, visit bcbsm.com or click here.
Follow‑up care key after ER visit for mental health issues, substance use disorderAccording to the National Committee for Quality Assurance, when a patient is discharged from an emergency room for mental health issues** or substance use disorder,** follow‑up visits with a doctor help to:
Follow‑up care can be in the doctor’s office, online or by phone. To assist members in their recovery, the Blue Cross and Blue Shield Federal Employee Program® offers additional services to support members:
New Directions is an independent company contracted by Blue Cross Blue Shield of Michigan to perform mental health and substance us disorder case management services for FEP Service Benefit Plan members. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
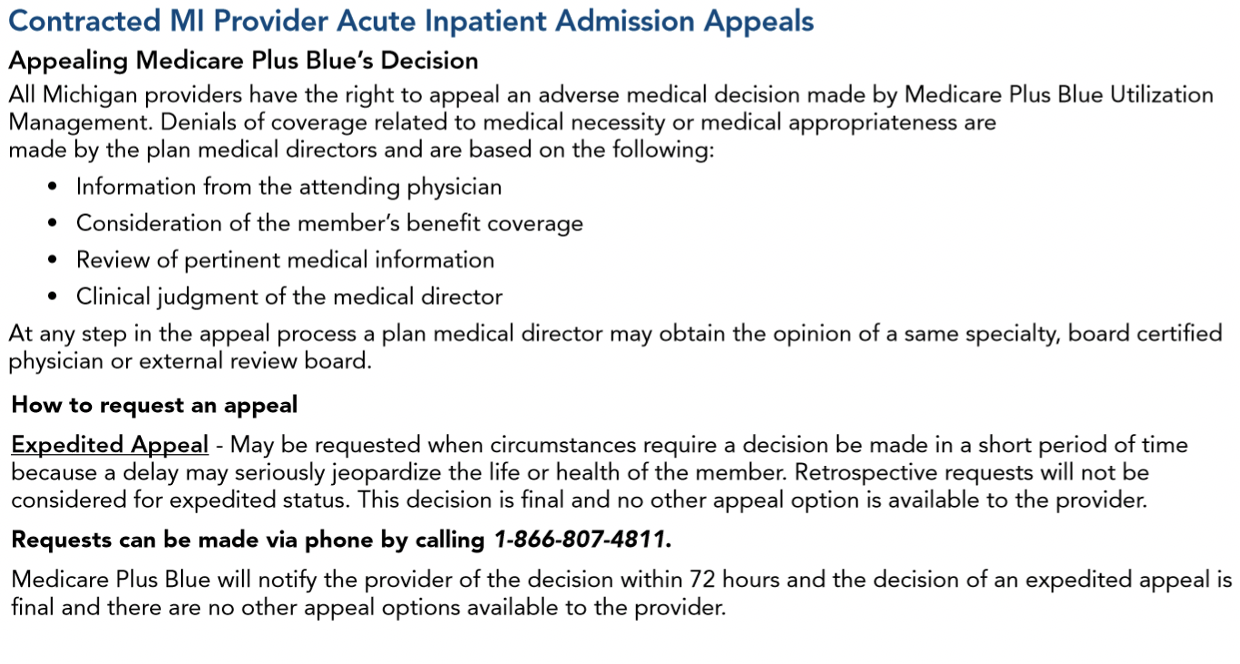
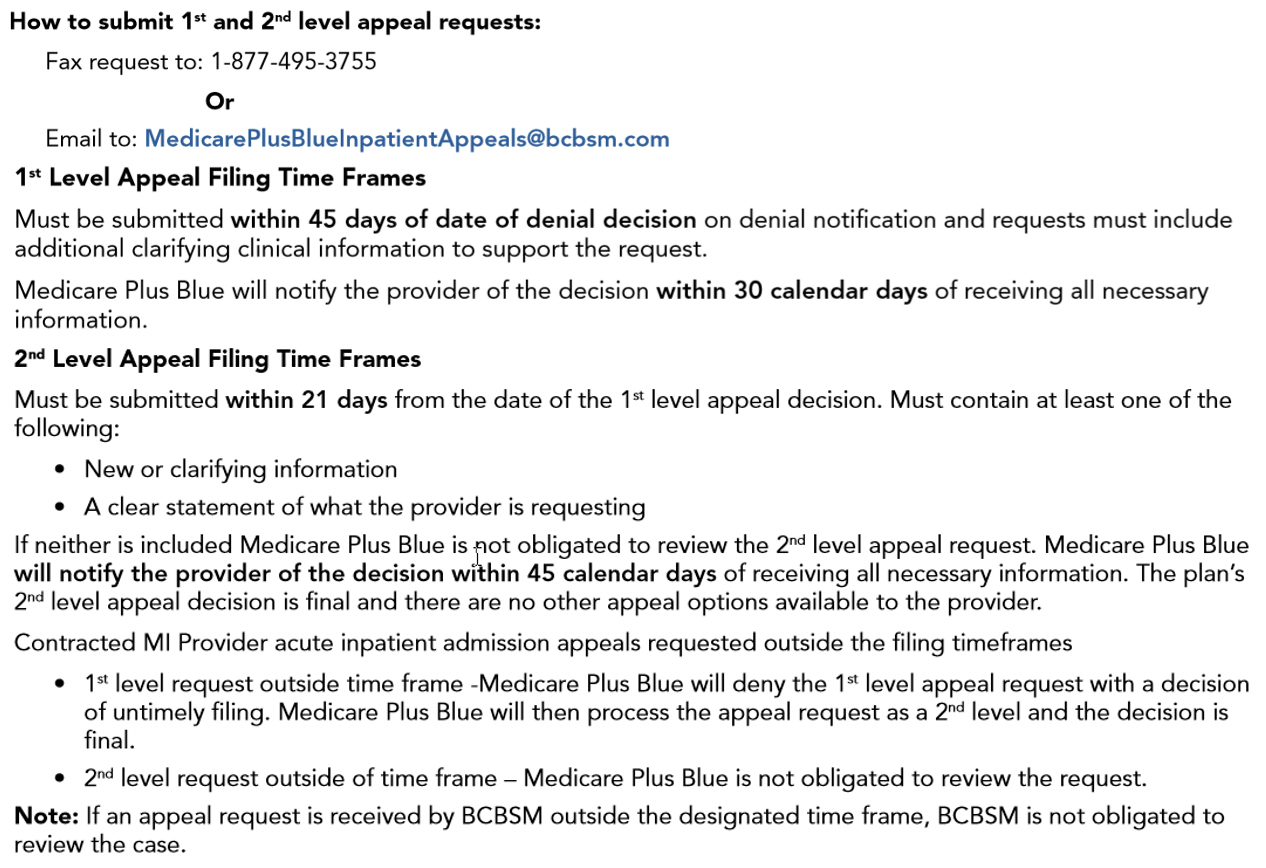
How to submit appeals of Medicare Advantage inpatient acute care admissionsProviders who need to submit appeals for denied authorization requests for Medicare Plus Blue℠ and BCN Advantage℠ inpatient acute care admissions (non‑behavioral health) should follow the process described in the provider manuals. Instructions can also be found in the denial letters Blue Cross Blue Shield of Michigan or Blue Care Network send providers. Medicare Plus Blue For Medicare Plus Blue members, providers can find the process in the “Contracted MI Provider Acute Inpatient Admission Appeals” section of the Medicare Plus Blue℠ PPO Provider Manual. Here’s a screenshot:
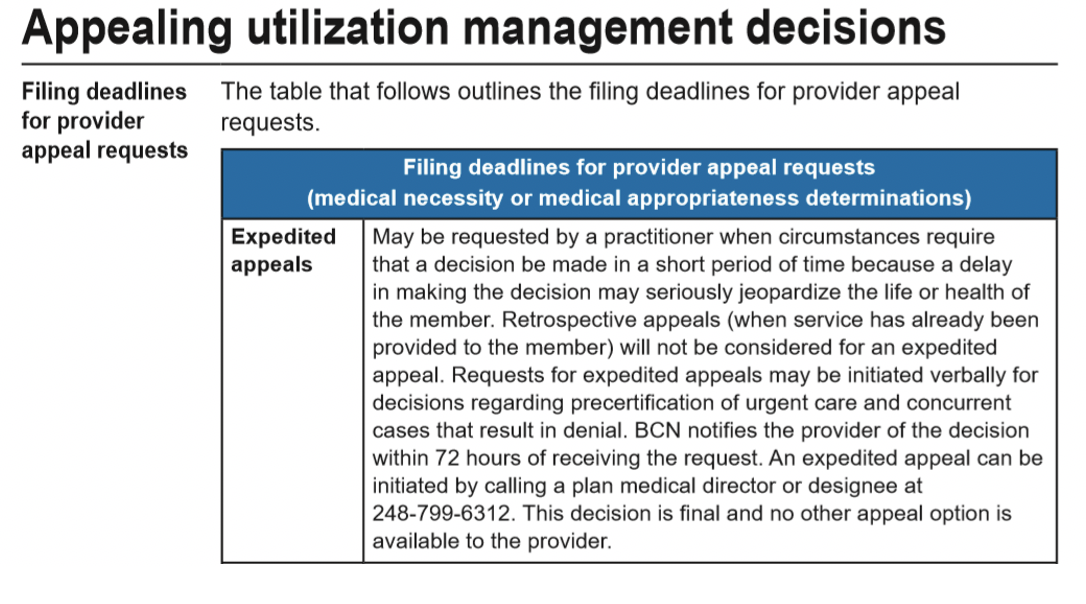
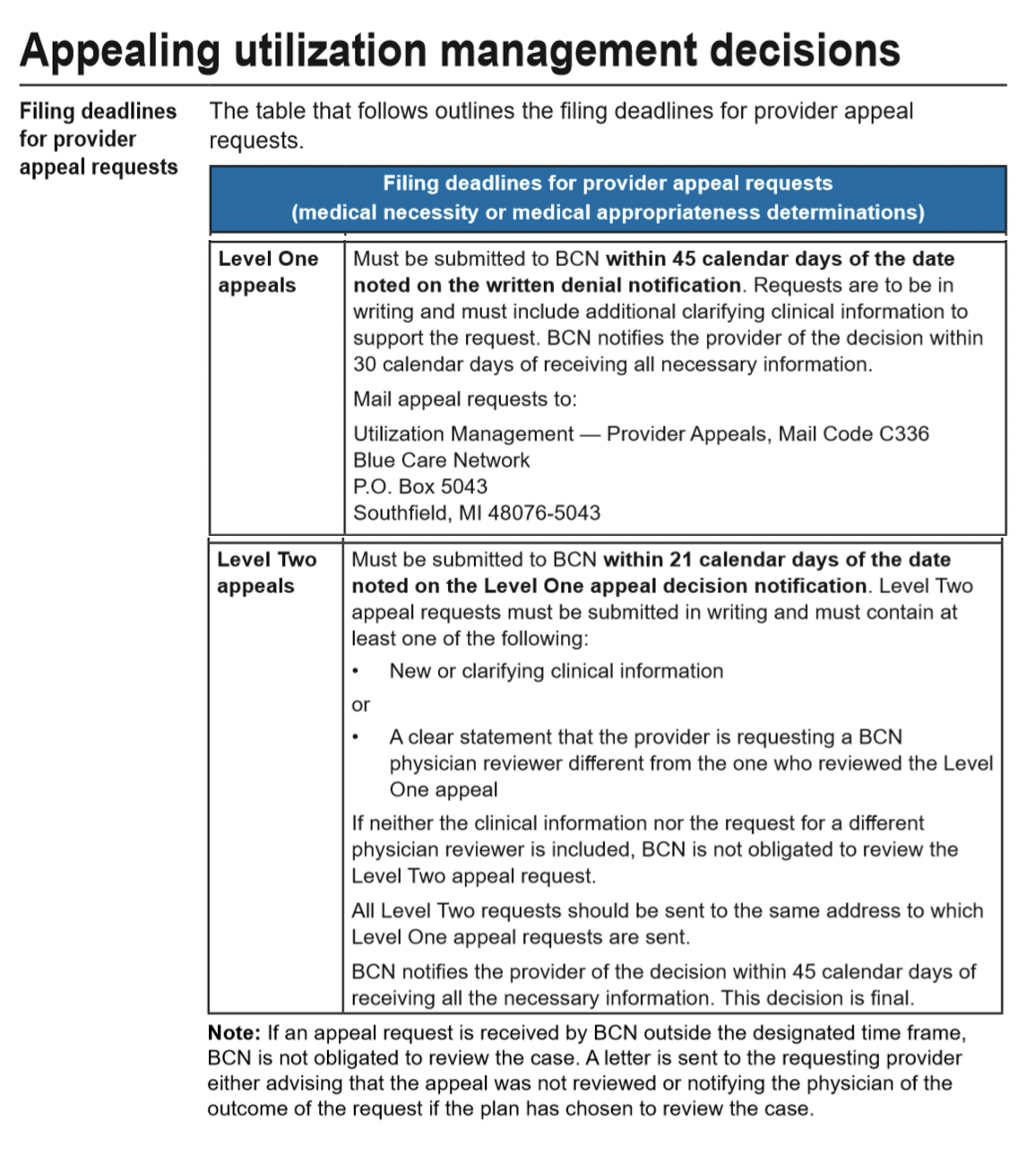
BCN Advantage For BCN Advantage members, providers can find instructions in the “Utilization Management” chapter of the BCN Provider Manual. Look in the section titled “Appealing utilization management decisions.” Here’s a screenshot:
Don’t use F codes when requesting authorization for Medicare Advantage inpatient medical admissionsWhen requesting authorization for acute care inpatient medical (non‑behavioral health) admissions, select a medical ICD‑10 diagnosis code in the e-referral system — one that doesn’t begin with F. If you select an ICD‑10 diagnosis code that begins with F, the processing of your request will be delayed because:
Background We’ve noticed that for members admitted to a medical unit for acute detoxification (such as withdrawal from alcohol or other drugs), providers are sometimes submitting authorization requests with diagnosis codes that begin with F. However, these are considered medical — not behavioral health — admissions, even though the member’s condition involves the use of alcohol or other substances. Members this applies to This applies to members covered by these plans:
Medical benefit specialty drug prior authorization list changing in April for most membersStarting in April 2021, we’re adding prior authorization requirements for some drugs covered under the medical benefit. Providers must request prior authorization through AIM Specialty Health®. For dates of service on or after April 15, 2021, the following drug will require prior authorization for UAW Retiree Medical Benefits Trust PPO non-Medicare members:
For dates of service on or after April 22, 2021, the following drugs will require prior authorization for Blue Cross Blue Shield of Michigan commercial fully insured members and for Blue Care Network commercial, Medicare Plus Blue℠ and BCN Advantage℠ members:
These requirements don’t apply to members of the Blue Cross and Blue Shield Federal Employee Program® and MESSA. Submit authorization requests to AIM through the AIM provider portal** or by calling the AIM Contact Center at 1‑844‑377‑1278. For information about registering for and accessing the AIM ProviderPortal, see the Frequently Asked Questions page** on the AIM website. More about the authorization requirements Authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. For more information on requirements related to drugs covered under the medical benefit, see:
We’ll update these lists to reflect these changes prior to the effective dates. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Procedure codes *71271 and *33208 don’t require authorization for most membersServices associated with radiology CPT code *71271 and cardiology CPT code *33208 don’t require authorization for these members:
We’ve removed these procedure codes from the document, Procedures that require prior authorization by AIM Specialty Health®: Cardiology, radiology (high technology) and sleep studies (in lab).
We’re planning to update our clinical edits for Medicare Advantage PPO claimsBlue Cross Blue Shield of Michigan Medicare Advantage PPO will update clinical edits applied to claims starting in June or shortly thereafter. We’re enhancing the edits as part of our efforts to promote correct coding for claims. These improvements will help ensure that our claim payment policies align with nationally recognized sources of information and are easy to understand. They’ll also help us better meet the needs of a changing health care industry while maintaining alignment with national coding guidelines. MA PPO medical and payment policies will continue to comply with:
Some of the enhancements include, but are not limited to:
As with the application of all our clinical edits, the guidelines and regulations of these sources should be followed:
As the enhancements draw closer, we’ll provide updates. The appeal process won’t change with the expanded edits, but new edit codes will be published in the coming months. Continue to submit appeals on the Clinical Editing Appeal Form with the necessary supporting documentation. And remember to continue to fax one appeal at a time to avoid processing delays.
eviCore will no longer mail Practice Profile summaries and category information for outpatient physical therapy services starting in JulyBeginning with July 2021 data, eviCore will no longer mail paper copies of the Practice Profile Summary, which includes information about your assigned category, to health care providers. Instead, eviCore will post category updates on the first business day of February and August each year beginning in August 2021. Follow these steps to access your Practice Profile Summary and obtain your category:
If you believe there are circumstances adversely affecting your utilization data, you may still request reconsideration within 15 days of eviCore’s notification. Initiate your reconsideration request within the UM Category window. Additional information is available on the evicore.com** website as follows:
You can also contact Provider and Client Services at 1‑800‑646‑0418 for more information. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Optum to handle credit recovery efforts for Blue Cross and BCNEffective Jan. 1, 2021, Optum® has been assigned to identify and recover credit balance overpayments on behalf of Blue Cross Blue Shield of Michigan and Blue Care Network claims. Previously, these reviews may have been conducted by Conduent, formerly known as CDR Associates. Any review initiated by Conduent that is in progress will be completed by Conduent with an estimated completion date of February 2021. Optum conducts periodic claim reviews at provider locations. They’re a professional health care consulting firm that has focused on assisting both providers and payers by identifying and processing credit balances. Reviews only involve patient accounting records, not medical records. Claim recoveries will be handled through claims offset, not check refunds. Additionally, claims data will be available through a web-based tool for providers who choose to submit credit balance recoveries through Optum’s overpayment management tool. Note: For Medicare Plus Blue℠ overpayments, providers may continue to submit a Request for offset of a Medicare Advantage overpayment form directly to Blue Cross using the existing process. This involves identifying the reason for the overpayment of a medical claim paid through IKA. The claim is then adjusted in IKA, resulting in an offset of future claim payments.
We’ve added site‑of‑care requirements for Uplizna for Blue Cross commercial membersEffective Jan. 1, 2021, Blue Cross Blue Shield of Michigan has added site‑of‑care requirements for Uplizna® (inebilizumab‑cdon), HCPCS code J1823. This drug is covered under the medical benefit for our commercial members. Encourage your patients who have Blue Cross commercial coverage to select one of the following infusion locations instead of using a hospital outpatient facility:
If members currently receive infusions for these drugs at a hospital outpatient facility, providers must:
Override for infusions received from Jan. 1 through Feb. 18 However, you can receive an override for these dates of service so the claim will pay. To inquire about an override, call the Pharmacy Clinical Help Desk at 1‑800‑437‑3803. For dates of service on or after Feb. 19, all members must receive infusions at a covered infusion location, unless the provider obtains prior authorization for receiving the infusion at a hospital outpatient facility location. More about authorization requirements Note: Uplizna already has site‑of‑care requirements for Blue Care Network commercial members for dates of service on or after Aug. 1, 2020. Authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. List of requirements
Additional information
Lunch and learn webinars for physicians and coders focus on risk adjustment, codingSign up now for live, monthly, lunchtime webinars focusing on risk adjustment and coding. Starting in April, these educational sessions will update you on documentation and coding of common challenging diagnoses. You’ll also have an opportunity to ask questions. April through September’s webinars are led by physicians. The last three sessions of the year focus on coding guideline updates and are led by coders. While the session topics could change, our current schedule and tentative topics follow. All sessions start at 12:15 p.m. Eastern time and generally run for 15 to 30 minutes. Click on a Register here link below to sign up for a session.
If you have any questions about the sessions, contact April Boyce at aboyce@bcbsm.com. If you have questions regarding registration, email Patricia Scarlett at pscarlett@bcbsm.com.
Reminder: Sign up for additional training webinarsProvider Experience is continuing its series of training webinars for health care providers and staff. The webinars are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network. Here’s information on the upcoming training webinars:
The Blue Cross 201 webinar series provides an in‑depth learning opportunity and builds on information shared in our Blue Cross 101: Understanding the Basics webinar. This session reviews the processes and tools available when submitting professional claims. Recordings of previous webinars are available on web‑DENIS through the Blue Cross Provider Publications and Resources or BCN Provider Publications and Resources pages as follows: Blue Cross Provider Publications and Resources
You can also get more information about online training, presentations and videos by clicking on the E‑Learning icon at the top of the page. BCN Provider Publications and Resources
As additional training webinars become available, we’ll provide notices through web‑DENIS, The Record and BCN Provider News.
Medical benefit specialty drug prior authorization list changing in April for most membersStarting in April 2021, we’re adding prior authorization requirements for some drugs covered under the medical benefit. Providers must request prior authorization through AIM Specialty Health®. For dates of service on or after April 15, 2021, the following drug will require prior authorization for UAW Retiree Medical Benefits Trust PPO non-Medicare members:
For dates of service on or after April 22, 2021, the following drugs will require prior authorization for Blue Cross Blue Shield of Michigan commercial fully insured members and for Blue Care Network commercial, Medicare Plus Blue℠ and BCN Advantage℠ members:
These requirements don’t apply to members of the Blue Cross and Blue Shield Federal Employee Program® and MESSA. Submit authorization requests to AIM through the AIM provider portal** or by calling the AIM Contact Center at 1‑844‑377‑1278. For information about registering for and accessing the AIM ProviderPortal, see the Frequently Asked Questions page** on the AIM website. More about the authorization requirements Authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. For more information on requirements related to drugs covered under the medical benefit, see:
We’ll update these lists to reflect these changes prior to the effective dates. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Blue Cross and BCN Pharmacy to cover additional childhood vaccines, starting March 1To increase access to childhood vaccines and decrease the risk of vaccine‑preventable disease outbreaks among children, Blue Cross Blue Shield of Michigan and Blue Care Network Pharmacy Services is adding the following vaccines to its list of covered vaccines, starting March 1, 2021:
The following lists all the vaccines currently covered under eligible members’ prescription drug plans. Most Blue Cross commercial, non‑Medicare members with prescription drug coverage are eligible. If a member meets the coverage criteria, we cover the vaccine with no cost share.
If a member doesn’t meet the age requirement for a vaccine, Blue Cross won’t cover the vaccine under the prescription drug plan and the claim will reject. Certified, trained, qualified registered pharmacists must administer vaccines.
We’ve added site‑of‑care requirements for Uplizna for Blue Cross commercial membersEffective Jan. 1, 2021, Blue Cross Blue Shield of Michigan has added site‑of‑care requirements for Uplizna® (inebilizumab‑cdon), HCPCS code J1823. This drug is covered under the medical benefit for our commercial members. Encourage your patients who have Blue Cross commercial coverage to select one of the following infusion locations instead of using a hospital outpatient facility:
If members currently receive infusions for these drugs at a hospital outpatient facility, providers must:
Override for infusions received from Jan. 1 through Feb. 18 However, you can receive an override for these dates of service so the claim will pay. To inquire about an override, call the Pharmacy Clinical Help Desk at 1‑800‑437‑3803. For dates of service on or after Feb. 19, all members must receive infusions at a covered infusion location, unless the provider obtains prior authorization for receiving the infusion at a hospital outpatient facility location. More about authorization requirements Note: Uplizna already has site‑of‑care requirements for Blue Care Network commercial members for dates of service on or after Aug. 1, 2020. Authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. List of requirements
Additional information
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 When Blue Cross Blue Shield of Michigan and Blue Care Network move to the Availity® provider portal later in 2021, you’ll notice some updated features that will help you find what you need faster. Here’s a preview of the search capability that will be available on Availity.
When Blue Cross Blue Shield of Michigan and Blue Care Network move to the Availity® provider portal later in 2021, you’ll notice some updated features that will help you find what you need faster. Here’s a preview of the search capability that will be available on Availity.