
Subscribe | The Record Archive | Contacts | bcbsm.com
|
November 2020
What you need to know about doing business with Blue CrossThere’s certain information our participating health care providers need to know about doing business with Blue Cross Blue Shield of Michigan. This article provides a summary of key information. You should disregard the information in articles on this topic from previous years and use this article as a reference, as it provides the most up-to-date information. How to access our online provider manuals — Everything you need to do business with Blue Cross is included in our online provider manuals. From the home page of web-DENIS, click on Provider Manuals to access them. Access and availability guidelines — When a member requests an appointment, Blue Cross providers are required to comply with the following standards:
For more detailed information, see the “PPO Policies” chapter in the provider manual or contact your provider consultant. Affirmative statement about incentives — Medical decisions are based only on appropriateness of care and service and existence of coverage. See the affirmation statement in the “Participation” chapter of the provider manual. It’s located in the section titled Requirements and Guidelines. Clinical practice guidelines — For medical and behavioral health care, Blue Cross follows Michigan Quality Improvement Consortium guidelines, which can be found on the mqic.org** website. Comprehensive care management — To learn about Blue Cross’ comprehensive care management, use your online provider manual (“Health, Well-Being, and Care Management” chapter). To find the information on bcbsm.com, click here. Criteria used for level of care utilization management decisions Blue Cross modifications of the InterQual criteria (local rules) can be accessed online by following these steps:
If you have questions about InterQual, send an email to CESupport@mckesson.com. Provide your name and address, and reference that the question pertains to InterQual. Note: Criteria for Federal Employee Program® Service Benefit Plan utilization management decision-making can be found at fepblue.org. Medical policies
Note: FEP Service Benefit Plan policies can be found at fepblue.org. Member rights and responsibilities Pharmacy management Note: Generic substitution may be required for Blue Cross members. If both the generic and brand name are listed on our drug list, members are encouraged to receive the generic equivalent when available. Some members may be required to pay the difference between the brand-name and generic drug, as well as applicable copay, depending on the member’s plan. See the Pharmacy Services page on our website for more details. We recommend that you visit this page at least quarterly to access our drug lists and view updates. Go to bcbsm.com/providers. You can also call 1-800-437-3803 for the most up-to-date pharmaceutical information. Translation services Utilization management staff availability Behavioral health care — New Directions Contact information:
For more information
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Checking the status of temporary measures for COVID-19For the latest status of all temporary measures — including those related to utilization management, telehealth, billing and more — see the Temporary changes due to the COVID-19 pandemic document, which shows the start and end dates for each measure. You can find this and related documents on our coronavirus webpage, which is available through Provider Secured Services and on our public website at bcbsm.com/coronavirus.
Ascension to be network provider for Blue HPN in Southeast MichiganAs we told you in the October Record, Blue Cross Blue Shield of Michigan will offer health plans that use a new network called Blue High Performance Network℠, or Blue HPN℠. Starting in January 2021, Ascension will be the network provider for Blue HPN in Southeast Michigan. Blue Cross health plans with Blue HPN are EPO plan types, which means services are covered within the Blue HPN network. Members who have health plans with Blue HPN in Southeast Michigan can see certain Ascension health care providers for services and will only have to pay the plan’s out-of-pocket expenses. They will also be able to see HPN providers throughout the country, when they go out of state. If they see a non-Ascension health care provider, they’ll be responsible for the costs (except for emergency services and urgent care). You’ll know that a member has selected the Blue HPN plan by their Blue Cross ID card or in web-DENIS when you check eligibility. A sample card is included below. 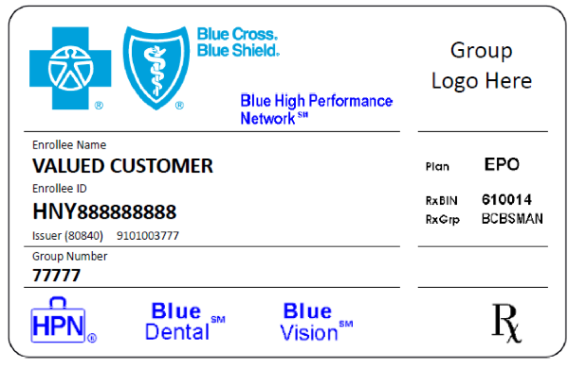 One important item to note on the card is the plan type. You’ll see the letters "EPO" in that area. EPO plan types require members to stay within the network for their plan and don’t allow for out-of-network coverage (with some exceptions). Also, the suitcase in the lower left corner of the card shows "HPN" inside the suitcase logo. That means that the member is in the Blue High Performance Network.
Availity multi-payer provider portal brings advantages to providers
This month, we’re focusing on the benefits of a multi-payer website. What is a multi-payer website? With a multi-payer provider portal like Availity, you log in to one website where you can find information for any health plan that uses Availity. This means you only need to learn how to use one system to find information for members associated with multiple health plans. In 2021, in Michigan, Availity will have member information for Blue Cross Blue Shield of Michigan, Blue Care Network, Aetna® and Humana®. What are the advantages of the Availity multi-payer website?
Watch for more information about Blue Cross and BCN’s move to the Availity provider portal in future issues of this newsletter.
Blue Cross and BCN clarify guidelines for pre-operative COVID-19 testingBlue Cross Blue Shield of Michigan and Blue Care Network are offering guidance for pre-operative COVID‑19 testing. Procedures conducted in hospital operating rooms and ambulatory surgical facilities are appropriate for pre-operative COVID-19 testing. In addition, aerosol-generating procedures, regardless of the location performed, such as oral surgery in the office setting, are appropriate for pre-operative COVID-19 testing. Examples where COVID-19 testing would not be appropriate include a simple wound closure, skin biopsy or routine medical or dental care in an office setting. Pre-operative COVID-19 testing should support the patient’s access to needed medical care and shouldn’t become a barrier to receiving care. The codes for pre-operative testing include:
This pre-op testing guidance is specific to the COVID-19 pandemic. For more information, see the Patient testing section of our COVID-19 webpages on our public website at bcbsm.com/coronavirus or within Provider Secured Services by clicking on Coronavirus (COVID-19).
Update: CMS opioid treatment programIn the February Record, we ran an article about a Centers for Medicare & Medicaid Services program that encourages providers to offer comprehensive opioid treatment. We want to let you know that the program now applies to services for our commercial members (both Blue Cross Blue Shield of Michigan and Blue Care Network), in addition to our Medicare Advantage members (Medicare Plus Blue℠ and BCN Advantage℠). As of Jan. 1, 2020, Blue Cross and BCN have been allowing bundled rates to reimburse providers who offer certified opioid treatment programs, or OTPs, according to CMS guidelines. Bundled payment codes that include both drug and non-drug components are available, and we only pay for non-drug components through bundled payments. For bundled opioid treatment services in non-OPT programs, the following codes are payable: G2086, G2087 and G2088. See the February Record article for more details about the CMS opioid treatment program.
COVID-19 CPT codes addedAmerican Medical Association has added some new COVID-19 codes. The codes, effective dates and Blue Cross Blue Shield of Michigan’s coverage decisions are below. Pathology and Laboratory
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
2021 early-release CPT code updatesCategory III
Category III
Category III
HCPCS replacement codes establishedJ1738 replaces J3490, J3590 and C9059 when billing for Anjeso (meloxicam) The Centers for Medicare & Medicaid Services has established a permanent procedure code for Anjeso. All services through Sept. 30, 2020, will continue to be reported with code J3490, J3590 or C9059. All services performed on and after Oct. 1, 2020, must be reported with J1738. J3032 replaces J3490, J3590 and C9063 when billing for VYEPTI (eptinezumab-jjmr) CMS has established a permanent procedure code for VYEPTI™. All services through Sept. 30, 2020, will continue to be reported with code J3490, J3590 or C9063. All services performed on and after Oct. 1, 2020, must be reported with J3032. Prior authorization is required for all groups unless they are opted out of the prior authorization program. For groups that have opted out of the prior authorization program, this code is covered for the FDA-approved indications. J3241 replaces J3490, J3590 and C9061 when billing for TEPEZZA (teprotumumab-trbw) CMS has established a permanent procedure code for TEPEZZA™. All services through Sept. 30, 2020, will continue to be reported with code J3490, J3590 or C9061. All services performed on and after Oct. 1, 2020, must be reported with J3241. Prior authorization is required for all groups unless they are opted out of the prior authorization program. For groups that have opted out of the prior authorization program, this code requires manual review for individual consideration. J7351 replaces J3490 and J3590 when billing for DURYSTA (bimatoprost) CMS has established a permanent procedure code for DURYSTA™. All services through Sept. 30, 2020, will continue to be reported with code J3490, or J3590. All services performed on and after Oct. 1, 2020, must be reported with J7351. J9227 replaces J3490 and J3590 when billing for SARCLISA (isatuximab-irfc) CMS has established a permanent procedure code for SARCLISA®. All services through Sept. 30, 2020, will continue to be reported with code J3490 or J3590. All services performed on and after Oct. 1, 2020, must be reported with J9227.
HCPCS third-quarter update: New and deleted codesModifiers
Skin codes
Outpatient Prospective Payment System/Radiologic Procedures Radiopharmaceuticals
Outpatient Prospective Payment System/Injections
Injections
Outpatient Prospective Payment System/Surgery
Outpatient Prospective Payment System/Radiology
Professional/Miscellaneous/Data Gathering codes
Temporary Q codes/unclassified
Professional/Miscellaneous/Medicaid only services
Optical Accessories
Durable Medical Equipment
Billing chart: Blues highlight medical, benefit policy changesYou’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart. This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures. You will also see that descriptions for the codes are no longer included. This is a result of recent negotiations with the AMA on use of the codes. We will publish information about new BCBS groups or changes to group benefits under the Group Benefit Changes heading. For more detailed descriptions of the BCBSM policies for these procedures, please check under the Medical/Payment Policy tab in Explainer on web-DENIS. To access this online information:
Here are guidelines for billing collaborative careThe Collaborative Care Model, also known as CoCM, is a benefit for all our members, including seniors and Blue Care Network members, who see a primary care physician who uses this model. There are no member cost-sharing requirements for the use of CoCM. As you read in an October Record article, this integrated behavioral care model allows a primary care physician to more effectively treat patients with behavioral health conditions, such as depression and anxiety. This model requires three provider types, working together as a team and focusing on the following responsibilities:
Keep in mind that there are some specific billing requirements when using this model. Neither the behavioral health care manager nor the psychiatrist submits claims for CoCM services. The primary care physician bills for services provided by the care team over a calendar-month service period. Billing basics
Billing codes for commercial members:
Billing codes for patients with Medicare, a Medicare Advantage plan or Medicaid:
Although CoCM has been a Blue Cross and BCN benefit since 2017, we’re working to expand its use through training and support opportunities, along with incentives. As always, please check the member’s benefits before providing services. Contact your physician organization if your practice is interested in learning more about training opportunities or incentives for using this model. **FQHC/RHC stands for Federally Qualified Health Center/Rural Health Clinic.
Changes to PGIP risk allocationIn the January 2019 issue of The Record, we announced the creation of the Physician Group Incentive Program Risk-Bearing Organized Systems of Care program. This directed 2% of the PGIP allocation to the risk allocation, funding the PGIP Risk-Bearing OSC program. The program focused on rewarding PGIP OSCs for managing the benefit cost trend of their attributed Blue Cross PPO patient population. The fund accumulation for the Risk-Bearing OSC program will end effective Dec 31, 2020 (with the rewards distributed to OSCs in 2021). Effective Jan. 1, 2021, the funds accumulated through the 2% risk allocation will be directed to the PGIP Reward Pool to fund physician organizations and OSC efforts to transform health care and improve the quality and efficiency of care. Providers contractually agree in their participation agreements to allocate a portion of their reimbursement to the PGIP fund. All funds allocated are distributed to physician organizations and OSCs that participate in PGIP to support physician practice and system transformation. No money is retained by Blue Cross Blue Shield of Michigan for administrative costs.
Additional laboratory services covered in office during COVID-19 pandemicUntil further notice, we’re covering some additional laboratory services when they’re provided in a physician’s office. These services are in addition to any laboratory services we already cover when they’re performed in a physician’s office. We’re doing this to make it easier for our providers to care for our members during the COVID-19 pandemic. Here are the codes for the additional laboratory services:
The laboratory services for the codes listed above can be performed in a physician’s office and billed to Blue Cross Blue Shield of Michigan or Blue Care Network, as appropriate. This applies to all our members covered by products from the lines of business listed below, with an effective date of Feb. 4, 2020:
Clarification: AllianceRx Walgreens Prime specialty pharmacy programAn article in the September Record, titled “AllianceRx Walgreens Prime specialty pharmacy program starts Jan. 1 for most Blue Cross commercial members,” should have specified that AllianceRx will be the exclusive specialty pharmacy provider for Blue Cross Blue Shield of Michigan fully insured commercial members. For more details on this program, see the September Record article.
We’re expanding our cardiology services authorization program with AIM Specialty HealthStarting Jan. 1, 2021, we’re adding some cardiology services that will require authorization by AIM Specialty Health® for certain commercial and Medicare Advantage members. The services include cardiac implantable devices and arterial ultrasounds for dates of service on or after Jan. 1, 2021. Please check your patient’s health plan, as follows, to see which services require authorization by AIM. For Medicare Plus Blue℠ PPO, BCN commercial and BCN Advantage℠ members:
For Medicare Plus Blue members only:
Authorization requests must be submitted to AIM prior to the service being performed. You’ll be able to submit authorization requests, starting Dec. 14, 2020. Procedure codes The chart below lists the codes for the additional cardiology services that require authorization.
Reminder: Oncology management program to include Blue Cross commercial members, starting Dec. 1As we reported in the September issue of The Record, Blue Cross Blue Shield of Michigan is expanding its utilization management program for medical oncology to include all fully insured commercial members in December 2020. Blue Cross commercial groups that are self-funded will have the option to add this program in 2021. Providers will need to request prior authorization from AIM Specialty Health® for certain medical oncology and supportive care medications for Blue Cross’ fully insured members. Note: You should continue submitting prior authorization requests for two drugs for Blue Cross’ fully insured members by using the NovoLogix® web tool. This applies to dates of service through Nov. 30, 2020. The drugs are:
For dates of service on or after Dec. 1, submit those requests to AIM. Learn more about the program The oncology management program through AIM Specialty Health is already in effect for Medicare Plus Blue℠, BCN commercial and BCN Advantage℠ members, and for UAW Retiree Medical Benefits Trust non-Medicare members. Providers can view a list of medications managed by AIM for Blue Cross fully insured members on the Blue Cross AIM-Managed Procedures page of our ereferrals.bcbsm.com website. You can request prior authorizations by going to the AIM ProviderPortal℠** or by calling AIM at 1-800-728-8008, beginning Nov. 16, 2020 (for services on or after Dec. 1, 2020). For details about registering for and accessing the AIM ProviderPortal, see the Frequently Asked Questions** page of the AIM website. For more information about our AIM medical oncology program, view these resources:
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
TurningPoint musculoskeletal authorization program to expand in JanuaryAs we communicated in previous issues, TurningPoint Healthcare Solutions LLC is expanding its surgical quality and safety management program for Blue Cross Blue Shield of Michigan and Blue Care Network members. In this article, we’re sharing information about:
Procedures affected by the TurningPoint program expansion
TurningPoint Provider Portal Provider offices can access the TurningPoint Provider Portal by following these steps:
If you’re having trouble accessing the TurningPoint Provider Portal using this process, contact Blue Cross’ Web Support Help Desk at 1-877-258-3932. For out-of-state providers: Log in to your local plan's website and select an ID card prefix from Michigan. This will take you to the Blue Cross Blue Shield of Michigan website. You can then click on the Musculoskeletal Service Authorizations through TurningPoint link and enter your NPI. You may need to complete a one-time registration process with TurningPoint; after you register, you’ll have access to the Musculoskeletal service authorization through TurningPoint link in Provider Secured Services. In addition, any provider can register for direct access to the TurningPoint Provider Portal through the TurningPoint website. For more information, see “How do I register for direct access to the TurningPoint Provider Portal?” in the Musculoskeletal procedure authorizations: Frequently asked questions for providers document. Submitting retrospective authorization requests For Medicare Plus Blue members, the expansion of the TurningPoint program also affects some pain management procedures that are managed by Medicare Plus Blue Utilization Management for dates of service prior to Jan. 1, 2021. You’ll be able to submit retrospective authorization requests to Medicare Plus Blue Utilization Management through March 31, 2021. TurningPoint webinar training sessions Professional provider training — Includes information about TurningPoint's clinical model and operational changes, along with information about using the TurningPoint Provider Portal.
Facility training — Includes information about TurningPoint's clinical model and operational changes and the facility verification process.
Portal training — Includes information about using the TurningPoint Provider Portal.
Additional information You can also find information about TurningPoint on the Musculoskeletal Services pages on the ereferrals.bcbsm.com website:
Medicare Advantage members transitioning to a new diabetic management programIn October, BCN Advantage℠ and Medicare Plus Blue℠ PPO members in the Fit4D diabetes management program, managed by Cecilia Health, began transitioning to Livongo for diabetic management services. Members enrolled in Fit4D will complete their programs before being offered the new program. The goal of the diabetic management program is to help patients self-manage their condition, improve medication adherence and reduce unnecessary use of emergency room visits and inpatient admissions. The target population for the program includes members with diabetes (Type 1 and Type 2) who have one of the following:
Our Care Management team will refer members to the program. Providers won’t need to make recommendations. Livongo will provide glucometers and supplies to monitor members’ glucose readings. Certain readings that are out of normal range will trigger an alert and follow-up by the Livongo clinical team. Members will have access to an app and web-based support and education. They’ll be co-managed by our Care Management department and Livongo.
Sign up for additional training webinarsProvider Experience is continuing its series of training webinars for health care providers and staff. The webinars are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network. Here’s information on the upcoming training webinars:
The Blue Cross 201 webinar provides an in-depth learning opportunity and builds on information shared in our Blue Cross 101: Understanding the Basics webinar. This session reviews the processes and tools available when resolving common issues with claims. Recordings of previous webinars are available on web-DENIS via the Blue Cross Provider Publications and Resources or BCN Provider Publications and Resources pages as follows. Blue Cross Provider Publications and Resources
You can also get more information about online training, presentations and videos by clicking on the E-Learning icon at the top of the page. BCN Provider Publications and Resources
As additional training webinars become available, we’ll provide notices through
We’ve added Flumist to list of vaccines that can be administered by pharmacies for commercial membersThis flu season we’ve added Flumist® (allV4) to the list of medical vaccines to be administered by pharmacies under CPT code *90694. Flumist® will also be added to the list of vaccines covered under our member’s pharmacy benefits, which can be billed under our claims processor, Express Scripts. These changes apply to Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial, non-Medicare members. Review the complete list of Vaccine Affiliation Program payable vaccine codes
A complete list of payable codes, including the associated administration codes, are available in the Vaccine Affiliation Program payable vaccine code document. Blue Cross and BCN review this document quarterly. Here’s how to find the latest version:
Update vendor billing software Reminders on the process for vaccine administration
Note: Only pharmacies that are contracted with Blue Cross and BCN’s Vaccine Affiliation Program are eligible to submit claims as medical providers. If you’re a Michigan pharmacy that isn’t already participating in the Vaccine Affiliation Program, you can sign up. See How to sign up for the Vaccine Affiliation Program below.
Checking a member’s eligibility and benefits following medical processes
Checking eligibility and benefits online:
Medical billing
Medical reimbursement Note: Fee revisions, new codes added after publishing and entire fee schedules are published on web-DENIS. How to sign up for the Vaccine Affiliation Program
Where to find help General questions about medical vaccines – If you have general questions, call Provider Inquiry at 1-800-344-8525. To reach a Customer Service representative call between 8:30 a.m. and 5 p.m. Monday through Friday. Electronic transactions – For help with electronic transactions, such as the 270/271 eligibility and benefit inquiry transaction, contact the Electronic Data Interchange Help Line at 1-800-542-0945 or e-mail EDICustMgmt@bcbsm.com. Issues not resolved – If you can’t get your issue resolved through the above methods, the pharmacy provider consultant for all Michigan pharmacies may be able to help. Contact: Charlie Bono Reminder: Pharmacies can bill for COVID-19 testing For commercial members (Blue Cross and BCN)
Prior authorization lists for medical specialty drugs will change in November for some membersFor dates of service on or after Nov. 20, 2020, we’re removing prior authorization requirements for one drug and adding prior authorization requirements for several drugs. Lartruvo will no longer require prior authorization For dates of service on or after Nov. 20, we’ll no longer require prior authorization for Lartruvo® (olaratumab), HCPCS code J9285. This applies to Medicare Plus Blue℠, BCN Advantage℠ and UAW Retiree Medical Benefits Trust PPO non-Medicare members. Drugs that will require prior authorization For dates of service on or after Nov. 20, we’re adding prior authorization requirements for specialty drugs covered under the medical benefit. Here are the requirements:
How to submit authorization requests Submit authorization requests to AIM using one of the following methods:
For information about registering for and accessing the AIM ProviderPortal, see the Frequently asked questions page** on the AIM website. Authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. For additional information on requirements related to drugs covered under the medical benefit, see the following documents:
We’ll update these lists with new information about these drugs prior to the effective dates. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Starting Jan. 1, 2021, we’re changing how we cover some drugsThe health of our members is important to Blue Cross Blue Shield of Michigan and Blue Care Network. We want to ensure safe, high-quality care to meet their needs. As part of our efforts, we’re making some changes to how we cover certain drugs on the Clinical, Custom, Custom Select and Preferred Drug Lists, starting Jan. 1, 2021. We’ll send letters to affected members and health care providers about these changes. Here’s an overview: Drugs on the Preferred Drug List that won’t be covered 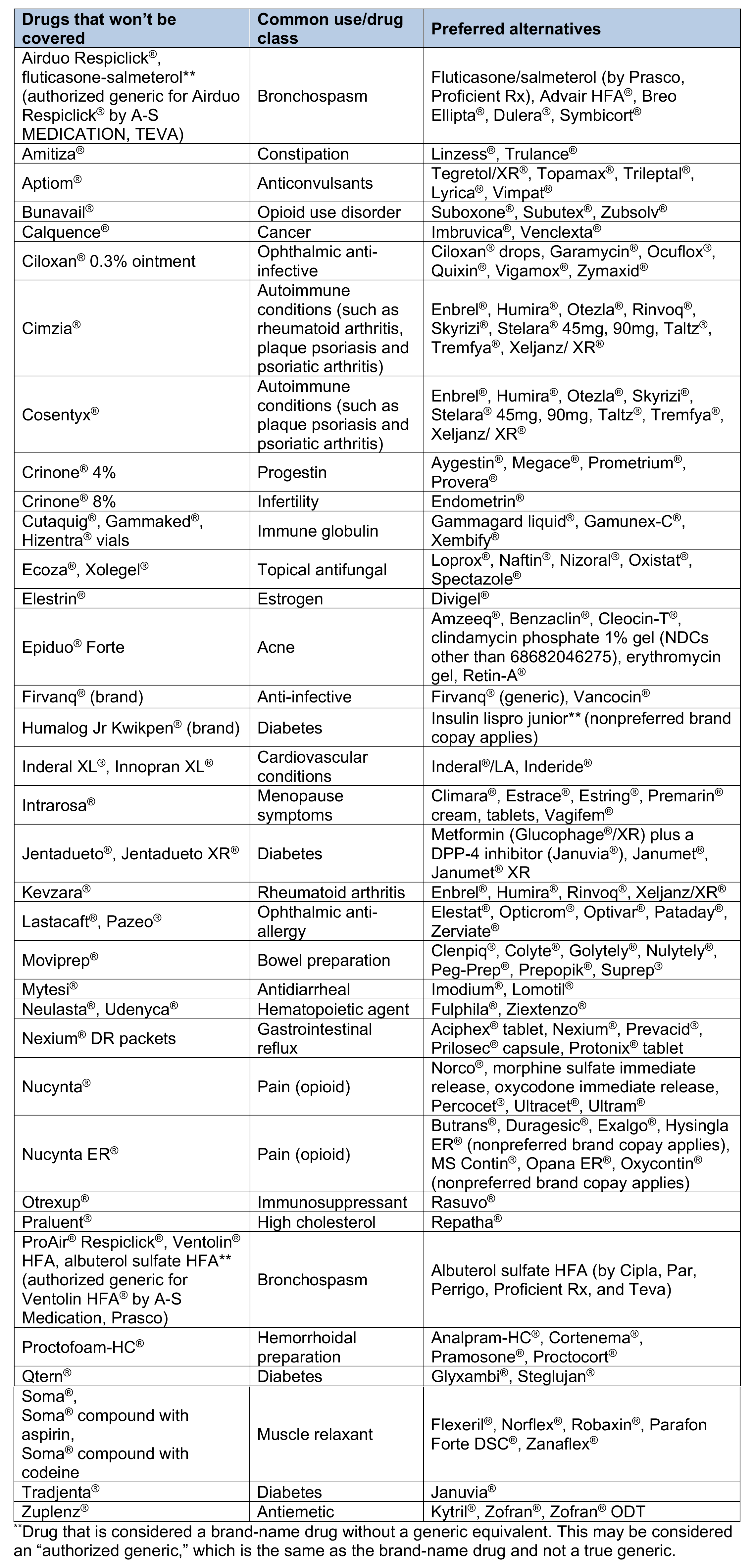 Drugs on the Preferred Drug List that will have a higher copayment 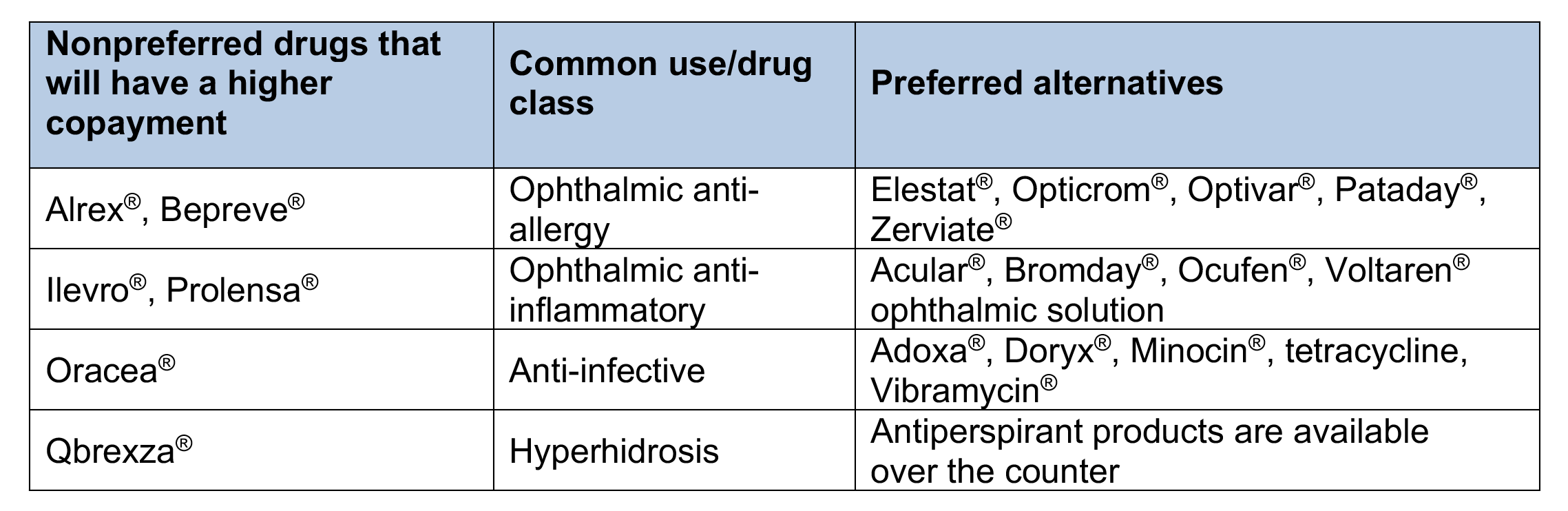 Drugs on the Preferred Drug List that will have quantity limits  Drugs on the Clinical and Custom Drug Lists that won’t be covered 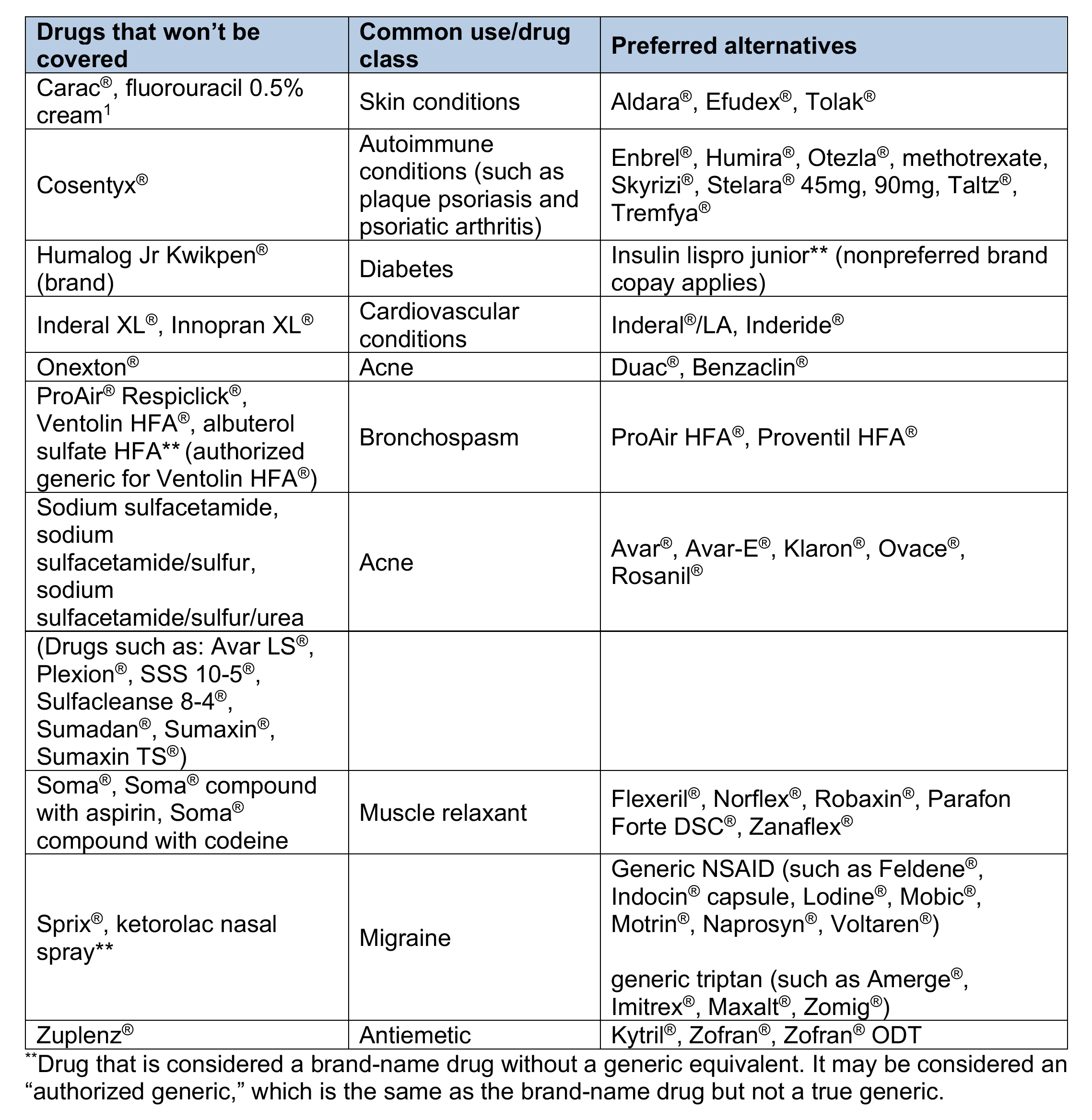 Drugs on the Custom Drug List that will have a higher copayment 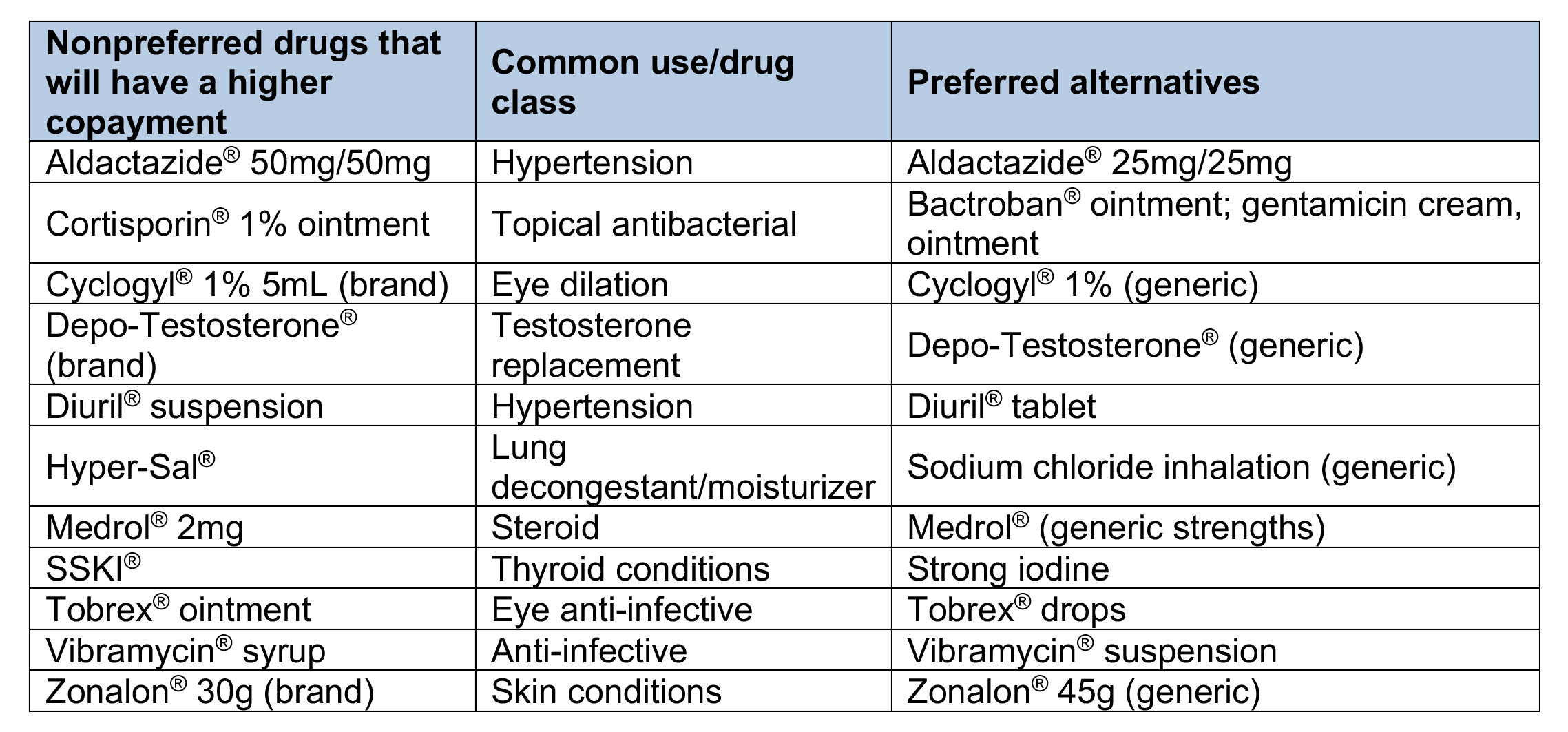 Drugs on the Custom Select Drug List that won’t be covered 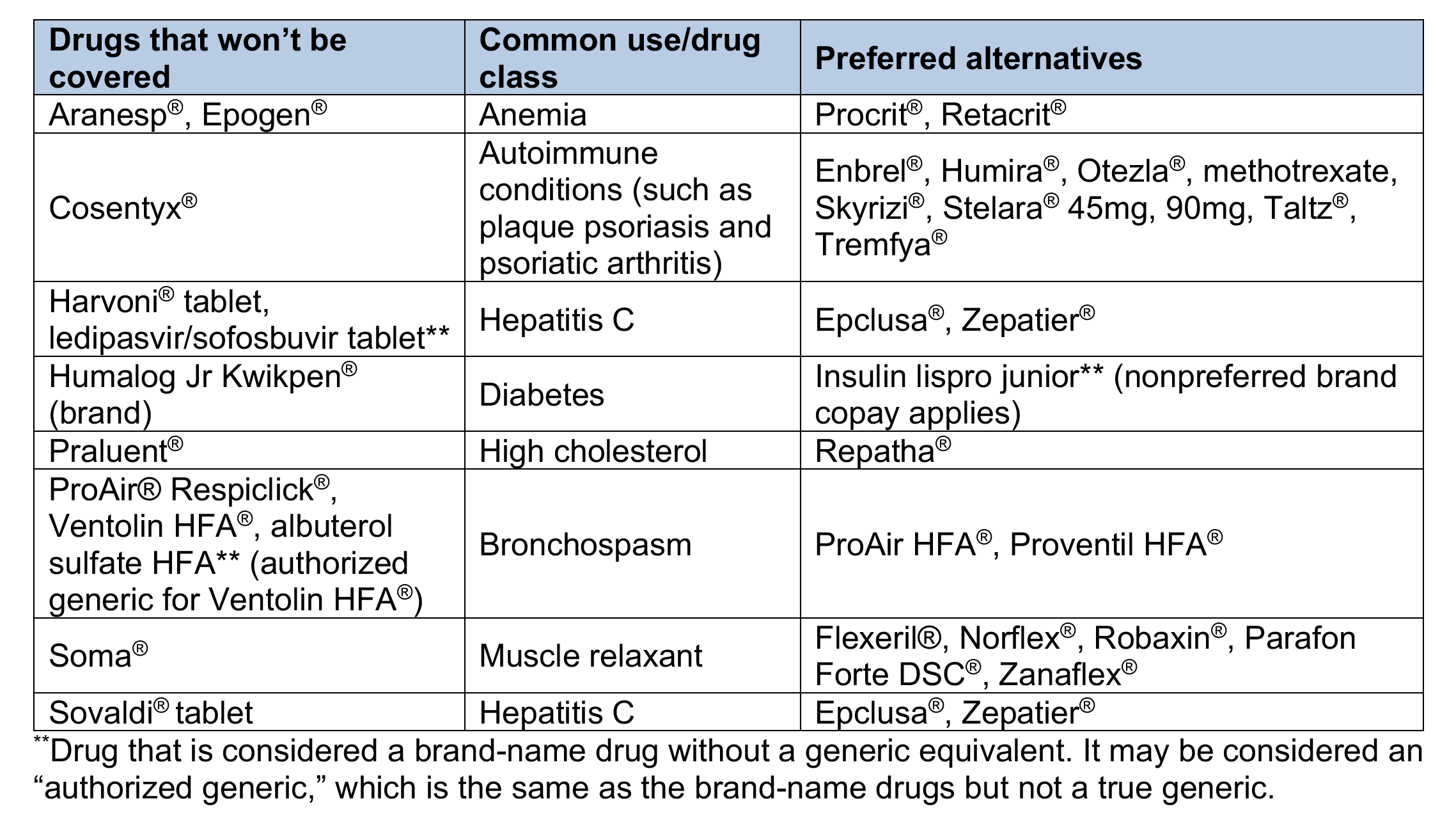 Drugs on the Clinical, Custom and Custom Select Drug Lists that will have quantity limits 
Medicare Part B medical specialty drug prior authorization list changing in January 2021We’re adding medications to the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue℠ and BCN Advantage℠ members. The specialty medications on this list are administered by a health care professional in a provider’s office, at the member’s home, in an off-campus outpatient hospital or in an ambulatory surgical center (place of service 11, 12, 19, 22 and 24). For dates of service on or after Jan. 1, 2021, the following CAR-T medications will require prior authorization through the NovoLogix® online tool:
The following medication will also require prior authorization through NovoLogix for dates of service on or after Jan. 1, 2021:
How to bill
Important reminder If you need to request access to Provider Secured Services, complete the Provider Secured Access Application form and fax it to the number on the form. List of requirements
Quarterly update: Requirements changed for some commercial medical benefit drugsBlue Cross Blue Shield of Michigan and Blue Care Network encourage proper utilization of high-cost medications covered under the medical benefit. One way we do this is by maintaining a comprehensive list of requirements for both Blue Cross and BCN commercial members. During July, August and September 2020, the following medical drugs had authorization requirement updates, site-of-care updates or both for Blue Cross commercial members:
For a detailed list of requirements, see the Blue Cross and BCN utilization management medical drug list. This list is available on the Blue Cross Medical Benefit Drugs page of the ereferrals.bcbsm.com website. The authorization requirements apply only to groups currently participating in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To view the list of Blue Cross commercial groups that don’t require members to participate in the program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group List. This list is also available on the Blue Cross Medical Benefit Drugs page of the ereferrals.bcbsm.com website. These changes don’t apply to Blue Cross and Blue Shield Federal Employee Program® members. As a reminder, an authorization approval isn’t a guarantee of payment. Health care providers need to verify eligibility and benefits for our members.
Starting Dec. 1, some drugs covered under medical benefit will require authorization for Blue Cross and Blue Shield FEP non-Medicare membersFor dates of service on or after Dec. 1, 2020, providers will have to request authorization from Blue Cross Blue Shield of Michigan for some drugs covered under the medical benefit for Blue Cross and Blue Shield Federal Employee Program® non-Medicare members. Authorization will be required only when members receive the drugs in Michigan. The drugs that will require authorization are listed in the Utilization management medical drug list for Blue Cross and Blue Shield Federal Employee Program non-Medicare members document. Note: For dates of service prior to Dec. 1, 2020, authorization isn’t required for drugs covered under the medical benefit for Blue Cross and Blue Shield FEP non-Medicare members. What you need to do
Resources The Blue Cross and Blue Shield FEP has its own policies for drugs that require authorization. The policies are available on the Medical Policies page of the Blue Cross and Blue Shield Federal Employee Program website. In mid-October, we’ll make available the list of medical benefit drugs that require authorization for Blue Cross and Blue Shield FEP non-Medicare members. Look for the list on the Blue Cross Medical Benefit Drugs page of the ereferrals.bcbsm.com website. We’ll have additional information in web-DENIS messages and in future issues of The Record. How to submit authorization requests You can submit authorization requests using one of the following methods:
Additional information Authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. The list of drugs in the Utilization management medical drug list for Blue Cross and Blue Shield Federal Employee Program non-Medicare members document applies only to Blue Cross and Blue Shield FEP non-Medicare members. For requirements related to drugs covered under the medical benefit for other Blue Cross commercial members and for BCN commercial members, see the following pages of the ereferrals.bcbsm.com website:
September, October questionnaire updates in e-referral systemWe use our authorization criteria, our medical policies and your answers to questionnaires in the e-referral system when making utilization management determinations on your authorization requests. In September and October:
As questionnaires are updated or removed, we’ll update or remove the corresponding preview questionnaires on ereferrals.bcbsm.com. Updated questionnaires
Removed questionnaire Preview questionnaires You can find the preview questionnaires as follows:
Authorization criteria and medical policies
We’re enhancing our Medical Policy Router’s search capabilitiesWe’re updating the Medical Policy Router with a new look and enhanced search capabilities. Beginning Nov. 17, 2020, the Medical Policy Router will allow multiple keyword searches, which can include procedure codes that are contained within the Medical Policy documents. The Medical Policy Router can be found in the Provider Secured Services area of bcbsm.com and on web-DENIS under BCBSM Provider Publications and Resources. We’ve simplified the tool by reducing it to the following six policy categories:
Note: Users of the router aren’t required to select a category.
ER follow-up care resources for FEP membersWhen patients are discharged after a visit to the emergency room, they’re encouraged to follow up with their primary care physician or mental health specialist, as appropriate. However, some patients don’t have a primary care physician or mental health specialist. So, to encourage Blue Cross and Blue Shield Service Benefit Plan members to schedule follow-up appointments, the Federal Employee Program® offers additional resources. The table below contains contact information available to FEP members to assist them with coordinating follow-up care and managing their condition.
For additional information about benefits and available support, FEP members can visit www.fepblue.org or call Customer Service at 1-800-482-3600.
How to use C3 to correctly bill multiple surgery outpatient facility claimsWhen two surgeries that have a mutually exclusive relationship or represent an overlap in services are billed on the same date, only one surgery is eligible for payment. To ensure proper reimbursement on outpatient claims, the charges for the claim should be billed on the line with the more extensive surgery. This can be determined by using the Clear Claim Connection™ tool, also known as C3. C3 enables you to view the Blue Cross Blue Shield of Michigan professional and outpatient facility claim combination rules and clinical rationale. Specifically, this web-based code-auditing reference tool does the following:
Obtaining access You can find the C3 web link on Provider Secured Services by following these steps:
If you don’t have access to web-DENIS, you can call our helpline toll-free at 1-877-258-3932, weekdays from 8 a.m. to 8 p.m. Or complete and return the Professional Secured Access and Use and Protection Agreement forms available on our website. From the Claim Entry screen, pictured below, follow these steps:
Note: Codes with letters must be keyed in upper case. 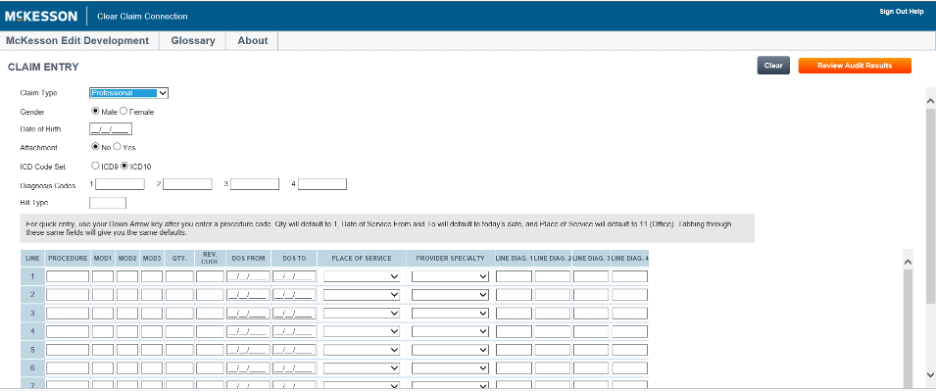 The C3 entry screen initially allows 10 rows for entering procedure codes. An additional 10 rows may be added by clicking the Add More Procedures line located directly under the procedure code entry field.
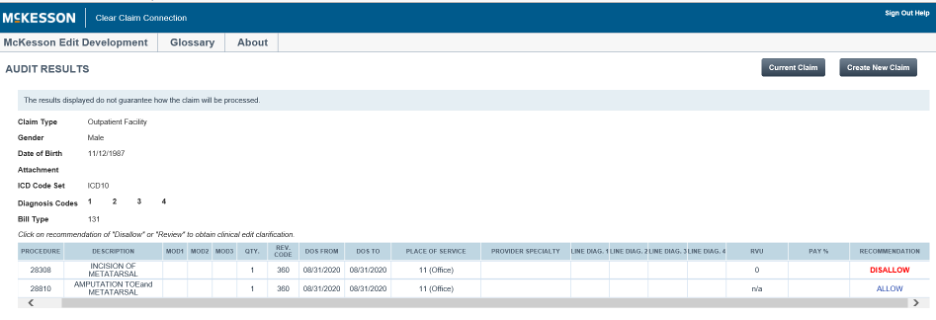 The results from entering the code combinations will be displayed in the Recommend column as Allow, Disallow or Review. A clinical edit clarification is provided for those claims with a recommendation of Disallow or Review. The above screen will help you identify primary surgery and secondary (or inclusive) surgeries so that you can roll up charges correctly on the primary surgery claim line. To view a clinical edit clarification, click on the procedure line that displays Disallow or Review. From this screen you can print the rationale (Printable Version), choose to enter a new claim (New Claim), go back to the original claim entry screen (Current Claim) or review the decision for the original claim (Review Claim Audit Results). 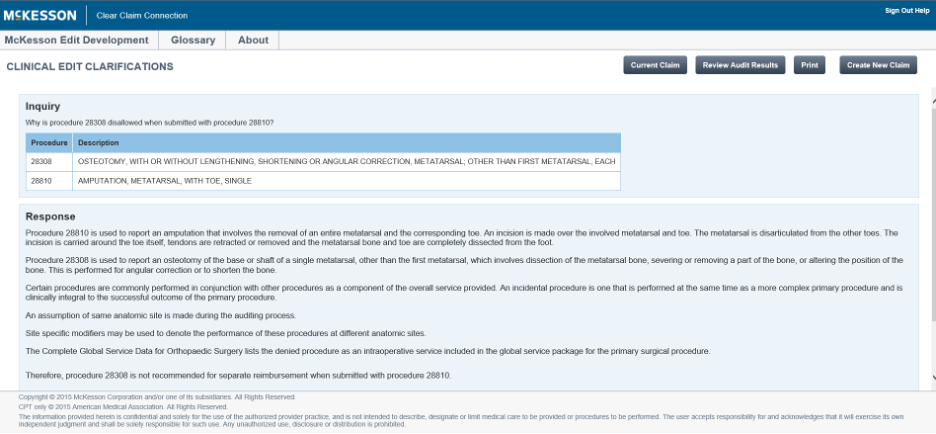 Please note that the clinical edits and rationale contained within C3 aren’t to be used as a guarantee of payment or a source for benefit policy information. Note: When all billed surgeries performed on the same day are payable, then repeat the following steps to identify most intensive surgery:
The claim scenario below shows that both procedures, 58140 and 29860, are payable when performed on the same date of service. However, the relative value unit, or RVU, of procedure 58140 is 26.92, and the relative value unit of procedure 29860 is 19.24. Therefore, procedure 58140 is more intensive, and the provider may roll up charges on the claim line reported with procedure 58140. 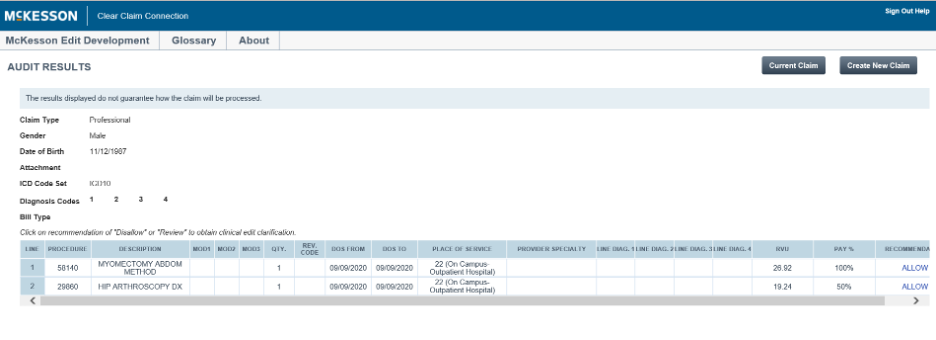 To end the session, click on Logoff. Note: The information contained in C3 is based on the date of service or the date the procedure code combination is entered for review. Exclusions C3 isn’t intended for use with combination rules that include the following:
C3 may occasionally be unavailable on Saturdays from 9 a.m. to 1 p.m. for maintenance.
Clarification: AllianceRx Walgreens Prime specialty pharmacy programAn article in the September Record, titled “AllianceRx Walgreens Prime specialty pharmacy program starts Jan. 1 for most Blue Cross commercial members,” should have specified that AllianceRx will be the exclusive specialty pharmacy provider for Blue Cross Blue Shield of Michigan fully insured commercial members. For more details on this program, see the September Record article.
We’re expanding our cardiology services authorization program with AIM Specialty HealthStarting Jan. 1, 2021, we’re adding some cardiology services that will require authorization by AIM Specialty Health® for certain commercial and Medicare Advantage members. The services include cardiac implantable devices and arterial ultrasounds for dates of service on or after Jan. 1, 2021. Please check your patient’s health plan, as follows, to see which services require authorization by AIM. For Medicare Plus Blue℠ PPO, BCN commercial and BCN Advantage℠ members:
For Medicare Plus Blue members only:
Authorization requests must be submitted to AIM prior to the service being performed. You’ll be able to submit authorization requests, starting Dec. 14, 2020. Procedure codes The chart below lists the codes for the additional cardiology services that require authorization.
Know how to avoid SNF denials for Medicare Advantage claimsIn November 2020, Blue Cross Blue Shield of Michigan and Blue Care Network will begin denying skilled nursing facility claims when patient-driven payment model, or PDPM, levels don’t match the levels naviHealth authorized. This applies to SNF claims for Medicare Plus Blue℠ and BCN Advantage℠ members. Facilities can resubmit denied claims with the approved PDPM levels. In future communications, we’ll let you know the exact date on which we’ll begin denying claims. As a reminder, naviHealth:
For more information, see Post-acute care services: Frequently asked questions for providers.
Reminder: Oncology management program to include Blue Cross commercial members, starting Dec. 1As we reported in the September issue of The Record, Blue Cross Blue Shield of Michigan is expanding its utilization management program for medical oncology to include all fully insured commercial members in December 2020. Blue Cross commercial groups that are self-funded will have the option to add this program in 2021. Providers will need to request prior authorization from AIM Specialty Health® for certain medical oncology and supportive care medications for Blue Cross’ fully insured members. Note: You should continue submitting prior authorization requests for two drugs for Blue Cross’ fully insured members by using the NovoLogix® web tool. This applies to dates of service through Nov. 30, 2020. The drugs are:
For dates of service on or after Dec. 1, submit those requests to AIM. Learn more about the program The oncology management program through AIM Specialty Health is already in effect for Medicare Plus Blue℠, BCN commercial and BCN Advantage℠ members, and for UAW Retiree Medical Benefits Trust non-Medicare members. Providers can view a list of medications managed by AIM for Blue Cross fully insured members on the Blue Cross AIM-Managed Procedures page of our ereferrals.bcbsm.com website. You can request prior authorizations by going to the AIM ProviderPortal℠** or by calling AIM at 1-800-728-8008, beginning Nov. 16, 2020 (for services on or after Dec. 1, 2020). For details about registering for and accessing the AIM ProviderPortal, see the Frequently Asked Questions** page of the AIM website. For more information about our AIM medical oncology program, view these resources:
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
TurningPoint musculoskeletal authorization program to expand in JanuaryAs we communicated in previous issues, TurningPoint Healthcare Solutions LLC is expanding its surgical quality and safety management program for Blue Cross Blue Shield of Michigan and Blue Care Network members. In this article, we’re sharing information about:
Procedures affected by the TurningPoint program expansion
TurningPoint Provider Portal Provider offices can access the TurningPoint Provider Portal by following these steps:
If you’re having trouble accessing the TurningPoint Provider Portal using this process, contact Blue Cross’ Web Support Help Desk at 1-877-258-3932. For out-of-state providers: Log in to your local plan's website and select an ID card prefix from Michigan. This will take you to the Blue Cross Blue Shield of Michigan website. You can then click on the Musculoskeletal Service Authorizations through TurningPoint link and enter your NPI. You may need to complete a one-time registration process with TurningPoint; after you register, you’ll have access to the Musculoskeletal service authorization through TurningPoint link in Provider Secured Services. In addition, any provider can register for direct access to the TurningPoint Provider Portal through the TurningPoint website. For more information, see “How do I register for direct access to the TurningPoint Provider Portal?” in the Musculoskeletal procedure authorizations: Frequently asked questions for providers document. Submitting retrospective authorization requests For Medicare Plus Blue members, the expansion of the TurningPoint program also affects some pain management procedures that are managed by Medicare Plus Blue Utilization Management for dates of service prior to Jan. 1, 2021. You’ll be able to submit retrospective authorization requests to Medicare Plus Blue Utilization Management through March 31, 2021. TurningPoint webinar training sessions Professional provider training — Includes information about TurningPoint's clinical model and operational changes, along with information about using the TurningPoint Provider Portal.
Facility training — Includes information about TurningPoint's clinical model and operational changes and the facility verification process.
Portal training — Includes information about using the TurningPoint Provider Portal.
Additional information You can also find information about TurningPoint on the Musculoskeletal Services pages on the ereferrals.bcbsm.com website:
Reminder: Skilled nursing facilities must sign up for e-referral to submit authorization requests; training availableWe’re reminding skilled nursing facilities to sign up for e-referral as soon as possible. SNFs must submit authorization requests for Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members through the e-referral system, starting Dec. 1, 2020. We communicated this information in the September Record. If you haven’t already, sign up now. It may take some time to gain access to the system. Currently, SNFs complete a form and submit it by fax. When the new requirement goes into effect in December, you’ll still need to complete the form, but you’ll attach it to the request in the e-referral system instead of faxing it. This requirement will apply to requests for admissions and requests for additional SNF days. Information on how to sign up is on our eferrals.bcbsm.com website. In addition, here are some new details you need to know:
Use the online tools to learn the e-referral system — before attending a webinar It’s important that you use the online tools to learn how to use the e-referral system before attending a webinar — especially:
Sign up for a webinar overview of the e-referral system
Sign up for additional training webinarsProvider Experience is continuing its series of training webinars for health care providers and staff. The webinars are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network. Here’s information on the upcoming training webinars:
The Blue Cross 201 webinar provides an in-depth learning opportunity and builds on information shared in our Blue Cross 101: Understanding the Basics webinar. This session reviews the processes and tools available when resolving common issues with claims. Recordings of previous webinars are available on web-DENIS via the Blue Cross Provider Publications and Resources or BCN Provider Publications and Resources pages as follows. Blue Cross Provider Publications and Resources
You can also get more information about online training, presentations and videos by clicking on the E-Learning icon at the top of the page. BCN Provider Publications and Resources
As additional training webinars become available, we’ll provide notices through
Prior authorization lists for medical specialty drugs will change in November for some membersFor dates of service on or after Nov. 20, 2020, we’re removing prior authorization requirements for one drug and adding prior authorization requirements for several drugs. Lartruvo will no longer require prior authorization For dates of service on or after Nov. 20, we’ll no longer require prior authorization for Lartruvo® (olaratumab), HCPCS code J9285. This applies to Medicare Plus Blue℠, BCN Advantage℠ and UAW Retiree Medical Benefits Trust PPO non-Medicare members. Drugs that will require prior authorization For dates of service on or after Nov. 20, we’re adding prior authorization requirements for specialty drugs covered under the medical benefit. Here are the requirements:
How to submit authorization requests Submit authorization requests to AIM using one of the following methods:
For information about registering for and accessing the AIM ProviderPortal, see the Frequently asked questions page** on the AIM website. Authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. For additional information on requirements related to drugs covered under the medical benefit, see the following documents:
We’ll update these lists with new information about these drugs prior to the effective dates. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Medicare Part B medical specialty drug prior authorization list changing in January 2021We’re adding medications to the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue℠ and BCN Advantage℠ members. The specialty medications on this list are administered by a health care professional in a provider’s office, at the member’s home, in an off-campus outpatient hospital or in an ambulatory surgical center (place of service 11, 12, 19, 22 and 24). For dates of service on or after Jan. 1, 2021, the following CAR-T medications will require prior authorization through the NovoLogix® online tool:
The following medication will also require prior authorization through NovoLogix for dates of service on or after Jan. 1, 2021:
How to bill
Important reminder If you need to request access to Provider Secured Services, complete the Provider Secured Access Application form and fax it to the number on the form. List of requirements
Quarterly update: Requirements changed for some commercial medical benefit drugsBlue Cross Blue Shield of Michigan and Blue Care Network encourage proper utilization of high-cost medications covered under the medical benefit. One way we do this is by maintaining a comprehensive list of requirements for both Blue Cross and BCN commercial members. During July, August and September 2020, the following medical drugs had authorization requirement updates, site-of-care updates or both for Blue Cross commercial members:
For a detailed list of requirements, see the Blue Cross and BCN utilization management medical drug list. This list is available on the Blue Cross Medical Benefit Drugs page of the ereferrals.bcbsm.com website. The authorization requirements apply only to groups currently participating in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To view the list of Blue Cross commercial groups that don’t require members to participate in the program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group List. This list is also available on the Blue Cross Medical Benefit Drugs page of the ereferrals.bcbsm.com website. These changes don’t apply to Blue Cross and Blue Shield Federal Employee Program® members. As a reminder, an authorization approval isn’t a guarantee of payment. Health care providers need to verify eligibility and benefits for our members.
We’re enhancing our Medical Policy Router’s search capabilitiesWe’re updating the Medical Policy Router with a new look and enhanced search capabilities. Beginning Nov. 17, 2020, the Medical Policy Router will allow multiple keyword searches, which can include procedure codes that are contained within the Medical Policy documents. The Medical Policy Router can be found in the Provider Secured Services area of bcbsm.com and on web-DENIS under BCBSM Provider Publications and Resources. We’ve simplified the tool by reducing it to the following six policy categories:
Note: Users of the router aren’t required to select a category.
Clarification: AllianceRx Walgreens Prime specialty pharmacy programAn article in the September Record, titled “AllianceRx Walgreens Prime specialty pharmacy program starts Jan. 1 for most Blue Cross commercial members,” should have specified that AllianceRx will be the exclusive specialty pharmacy provider for Blue Cross Blue Shield of Michigan fully insured commercial members. For more details on this program, see the September Record article.
Reminder: Oncology management program to include Blue Cross commercial members, starting Dec. 1As we reported in the September issue of The Record, Blue Cross Blue Shield of Michigan is expanding its utilization management program for medical oncology to include all fully insured commercial members in December 2020. Blue Cross commercial groups that are self-funded will have the option to add this program in 2021. Providers will need to request prior authorization from AIM Specialty Health® for certain medical oncology and supportive care medications for Blue Cross’ fully insured members. Note: You should continue submitting prior authorization requests for two drugs for Blue Cross’ fully insured members by using the NovoLogix® web tool. This applies to dates of service through Nov. 30, 2020. The drugs are:
For dates of service on or after Dec. 1, submit those requests to AIM. Learn more about the program The oncology management program through AIM Specialty Health is already in effect for Medicare Plus Blue℠, BCN commercial and BCN Advantage℠ members, and for UAW Retiree Medical Benefits Trust non-Medicare members. Providers can view a list of medications managed by AIM for Blue Cross fully insured members on the Blue Cross AIM-Managed Procedures page of our ereferrals.bcbsm.com website. You can request prior authorizations by going to the AIM ProviderPortal℠** or by calling AIM at 1-800-728-8008, beginning Nov. 16, 2020 (for services on or after Dec. 1, 2020). For details about registering for and accessing the AIM ProviderPortal, see the Frequently Asked Questions** page of the AIM website. For more information about our AIM medical oncology program, view these resources:
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
We’ve added Flumist to list of vaccines that can be administered by pharmacies for commercial membersThis flu season we’ve added Flumist® (allV4) to the list of medical vaccines to be administered by pharmacies under CPT code *90694. Flumist® will also be added to the list of vaccines covered under our member’s pharmacy benefits, which can be billed under our claims processor, Express Scripts. These changes apply to Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial, non-Medicare members. Review the complete list of Vaccine Affiliation Program payable vaccine codes
A complete list of payable codes, including the associated administration codes, are available in the Vaccine Affiliation Program payable vaccine code document. Blue Cross and BCN review this document quarterly. Here’s how to find the latest version:
Update vendor billing software Reminders on the process for vaccine administration
Note: Only pharmacies that are contracted with Blue Cross and BCN’s Vaccine Affiliation Program are eligible to submit claims as medical providers. If you’re a Michigan pharmacy that isn’t already participating in the Vaccine Affiliation Program, you can sign up. See How to sign up for the Vaccine Affiliation Program below.
Checking a member’s eligibility and benefits following medical processes
Checking eligibility and benefits online:
Medical billing
Medical reimbursement Note: Fee revisions, new codes added after publishing and entire fee schedules are published on web-DENIS. How to sign up for the Vaccine Affiliation Program
Where to find help General questions about medical vaccines – If you have general questions, call Provider Inquiry at 1-800-344-8525. To reach a Customer Service representative call between 8:30 a.m. and 5 p.m. Monday through Friday. Electronic transactions – For help with electronic transactions, such as the 270/271 eligibility and benefit inquiry transaction, contact the Electronic Data Interchange Help Line at 1-800-542-0945 or e-mail EDICustMgmt@bcbsm.com. Issues not resolved – If you can’t get your issue resolved through the above methods, the pharmacy provider consultant for all Michigan pharmacies may be able to help. Contact: Charlie Bono Reminder: Pharmacies can bill for COVID-19 testing For commercial members (Blue Cross and BCN)
Prior authorization lists for medical specialty drugs will change in November for some membersFor dates of service on or after Nov. 20, 2020, we’re removing prior authorization requirements for one drug and adding prior authorization requirements for several drugs. Lartruvo will no longer require prior authorization For dates of service on or after Nov. 20, we’ll no longer require prior authorization for Lartruvo® (olaratumab), HCPCS code J9285. This applies to Medicare Plus Blue℠, BCN Advantage℠ and UAW Retiree Medical Benefits Trust PPO non-Medicare members. Drugs that will require prior authorization For dates of service on or after Nov. 20, we’re adding prior authorization requirements for specialty drugs covered under the medical benefit. Here are the requirements:
How to submit authorization requests Submit authorization requests to AIM using one of the following methods:
For information about registering for and accessing the AIM ProviderPortal, see the Frequently asked questions page** on the AIM website. Authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. For additional information on requirements related to drugs covered under the medical benefit, see the following documents:
We’ll update these lists with new information about these drugs prior to the effective dates. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Starting Jan. 1, 2021, we’re changing how we cover some drugsThe health of our members is important to Blue Cross Blue Shield of Michigan and Blue Care Network. We want to ensure safe, high-quality care to meet their needs. As part of our efforts, we’re making some changes to how we cover certain drugs on the Clinical, Custom, Custom Select and Preferred Drug Lists, starting Jan. 1, 2021. We’ll send letters to affected members and health care providers about these changes. Here’s an overview: Drugs on the Preferred Drug List that won’t be covered 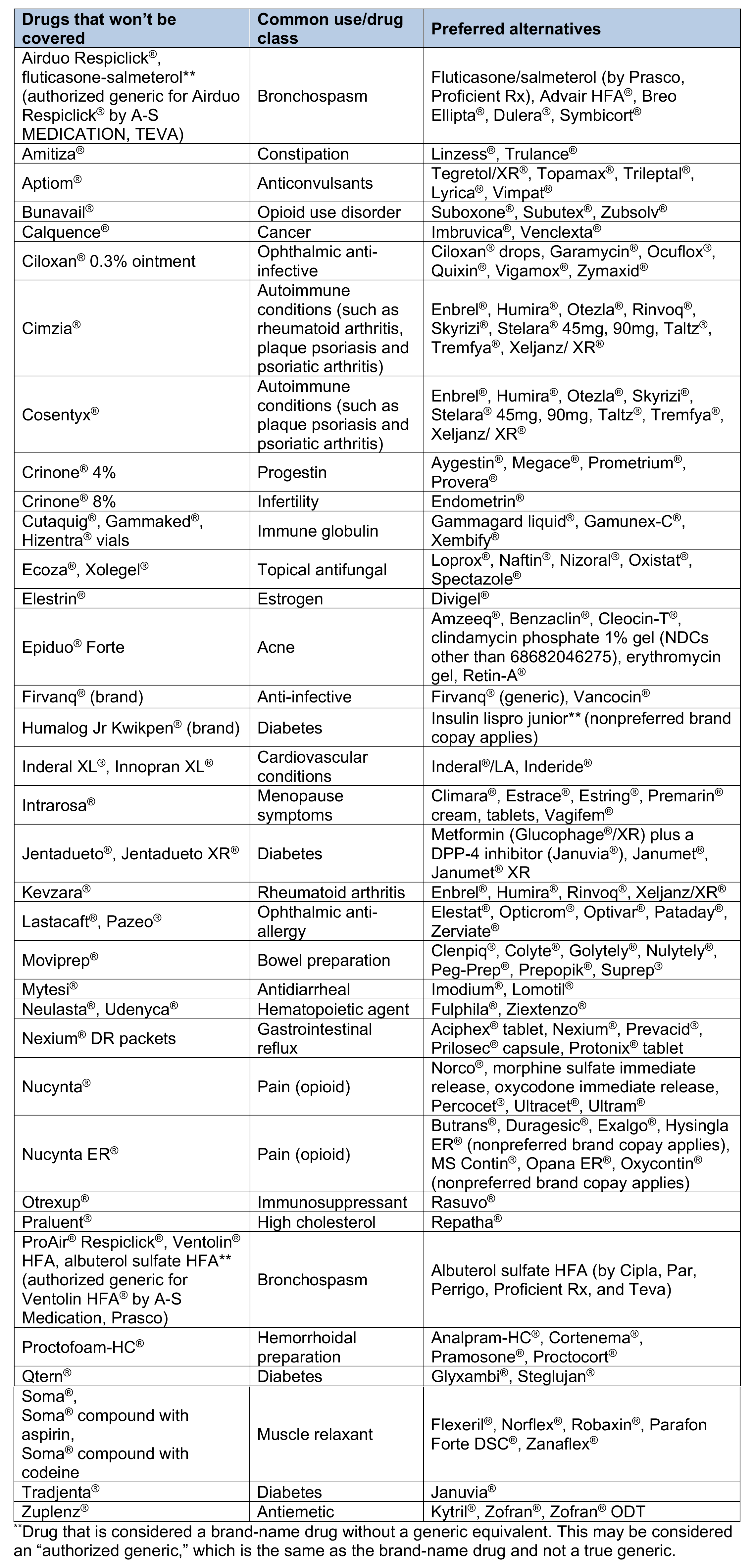 Drugs on the Preferred Drug List that will have a higher copayment 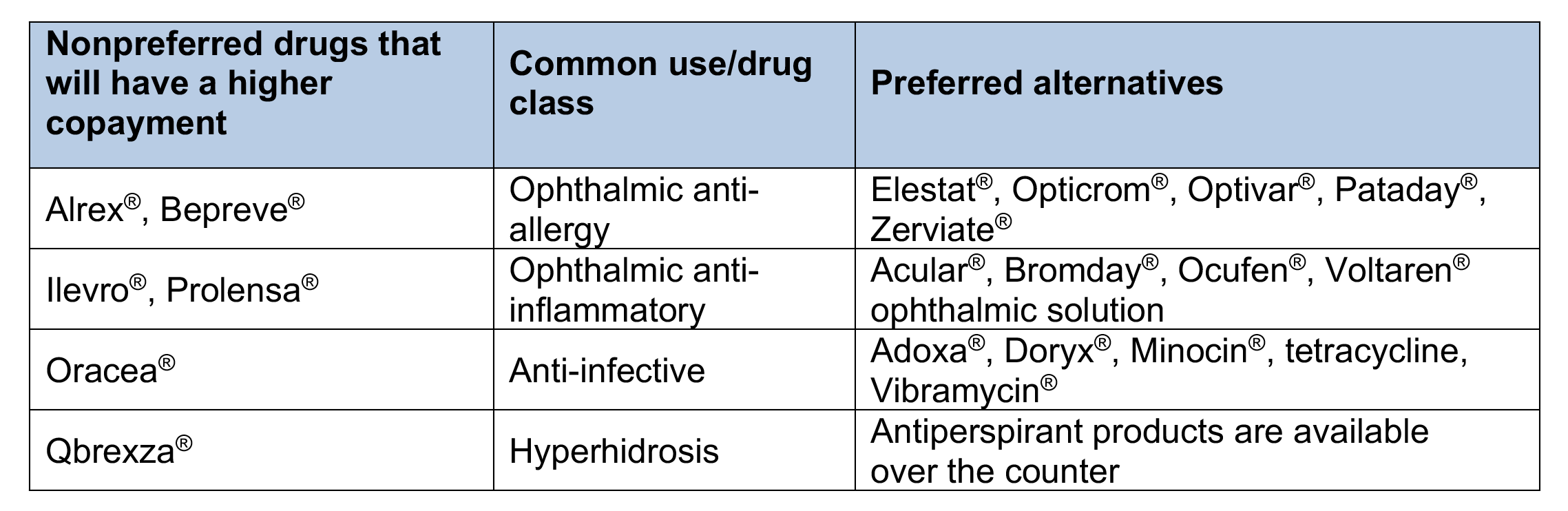 Drugs on the Preferred Drug List that will have quantity limits 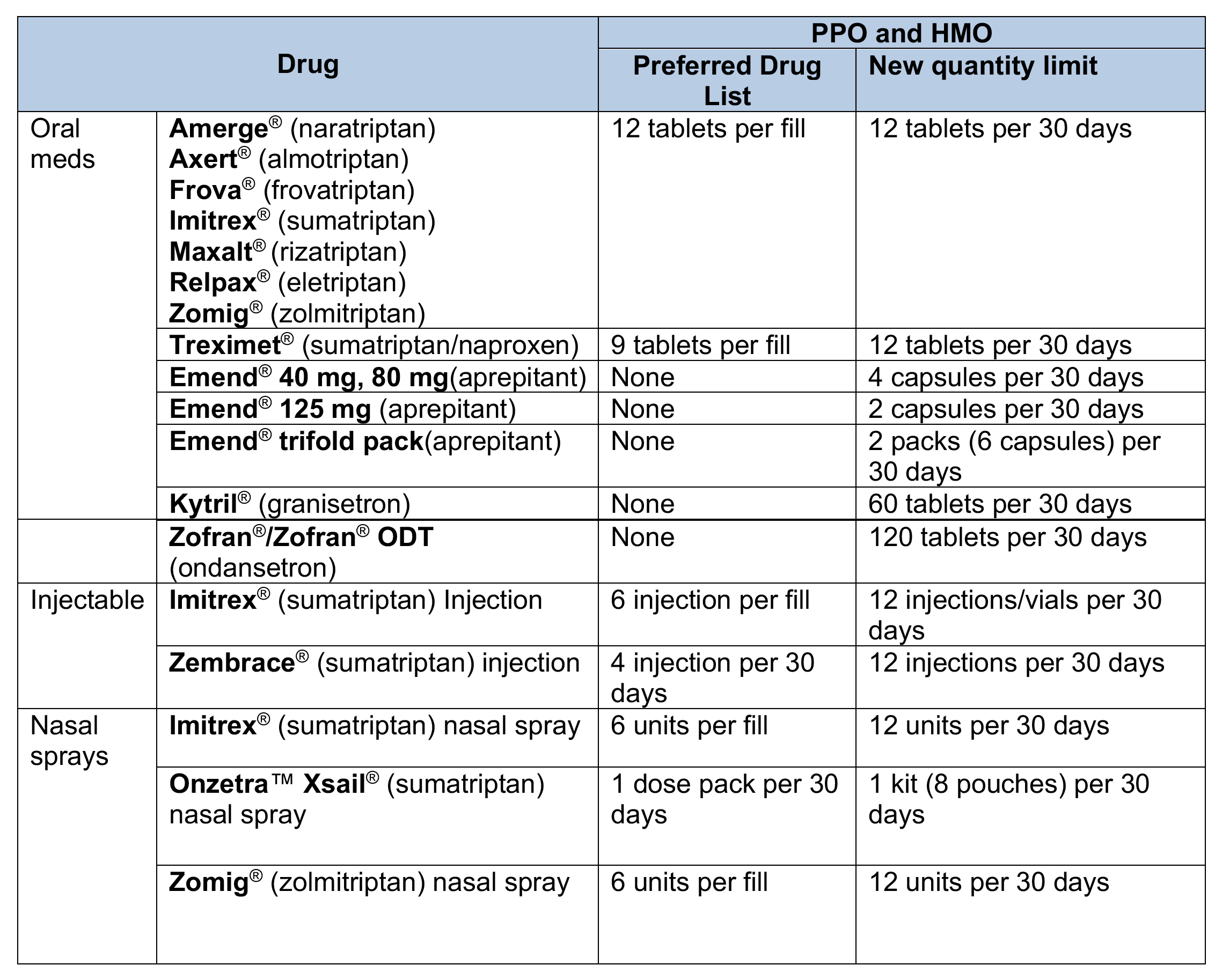 Drugs on the Clinical and Custom Drug Lists that won’t be covered 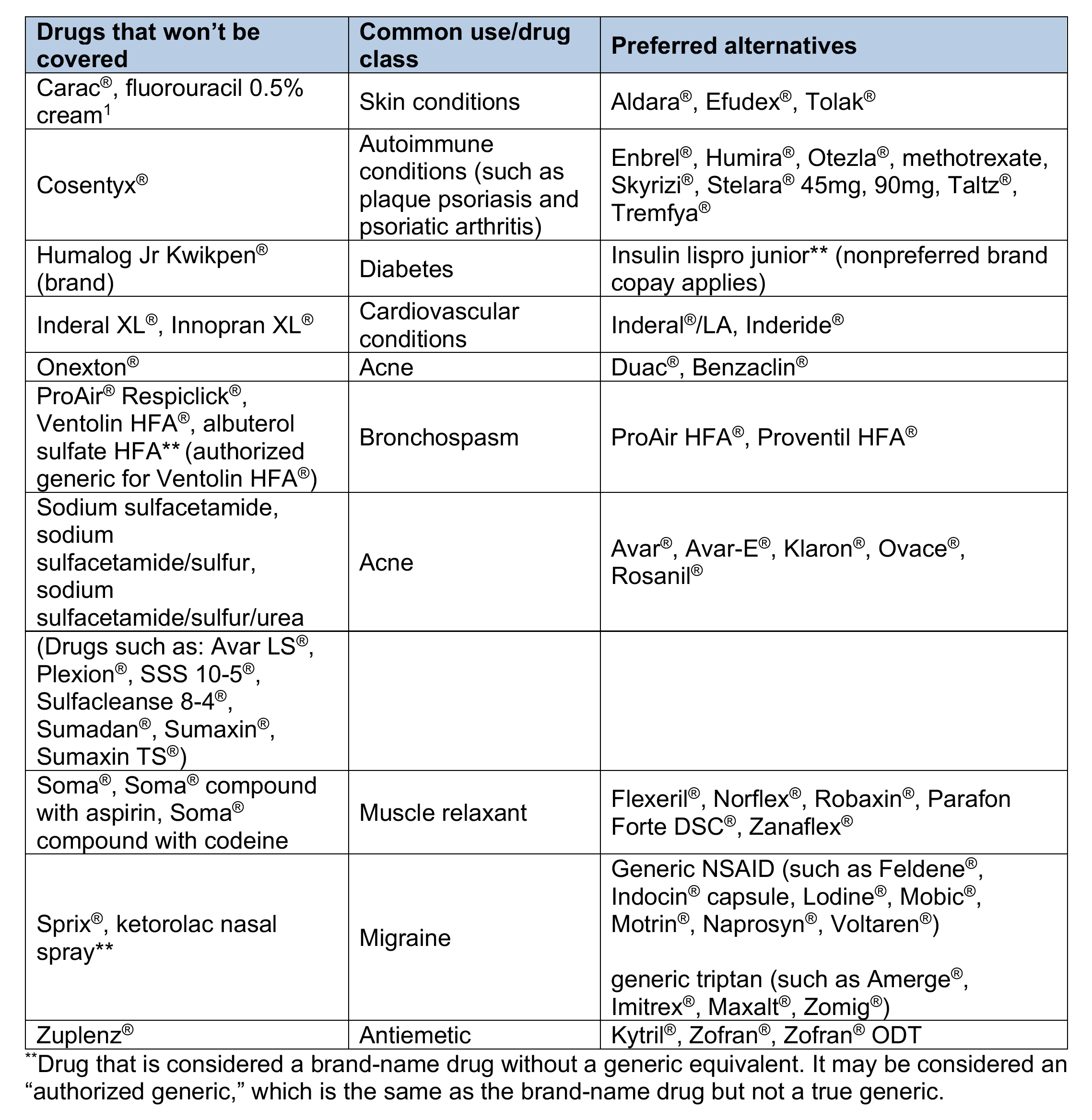 Drugs on the Custom Drug List that will have a higher copayment 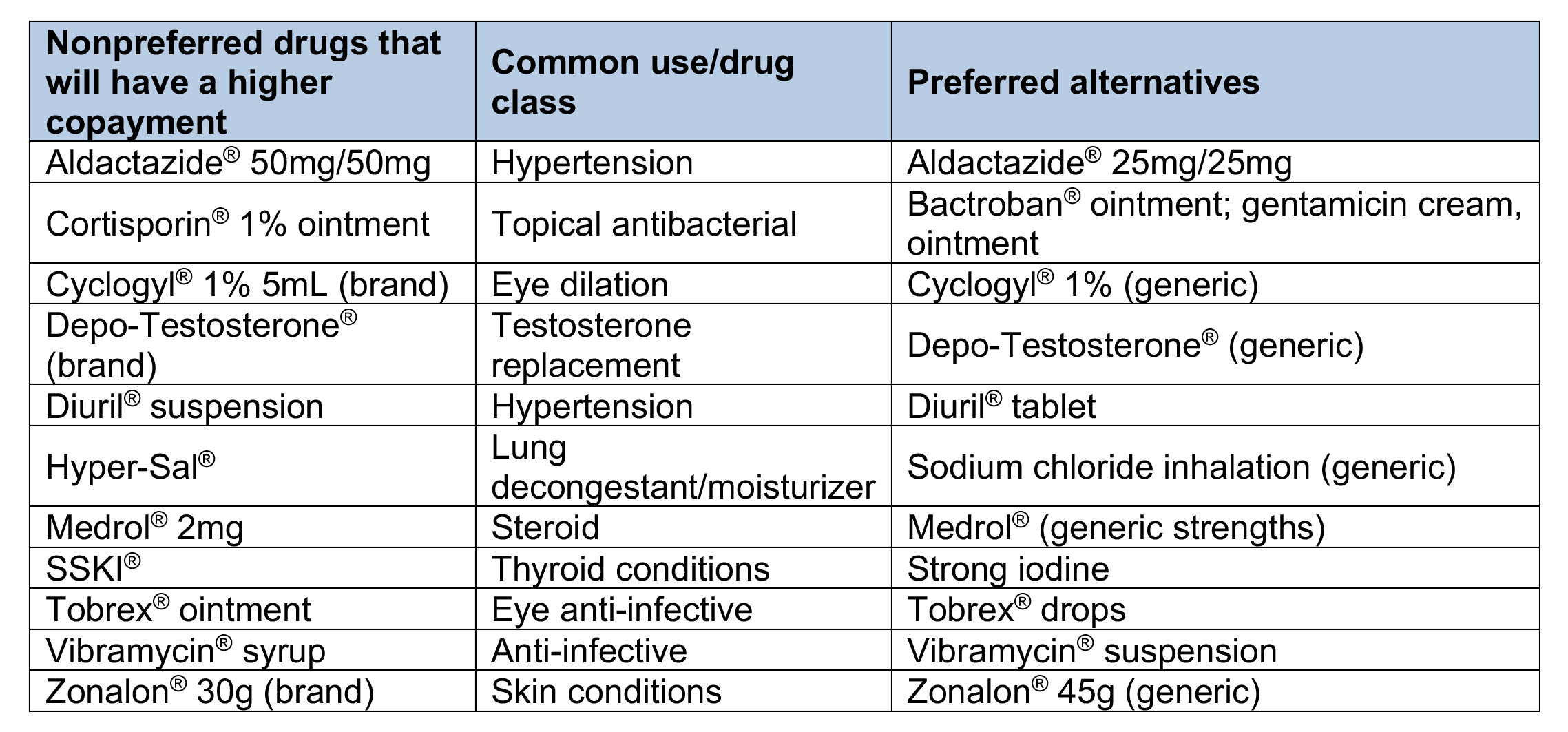 Drugs on the Custom Select Drug List that won’t be covered 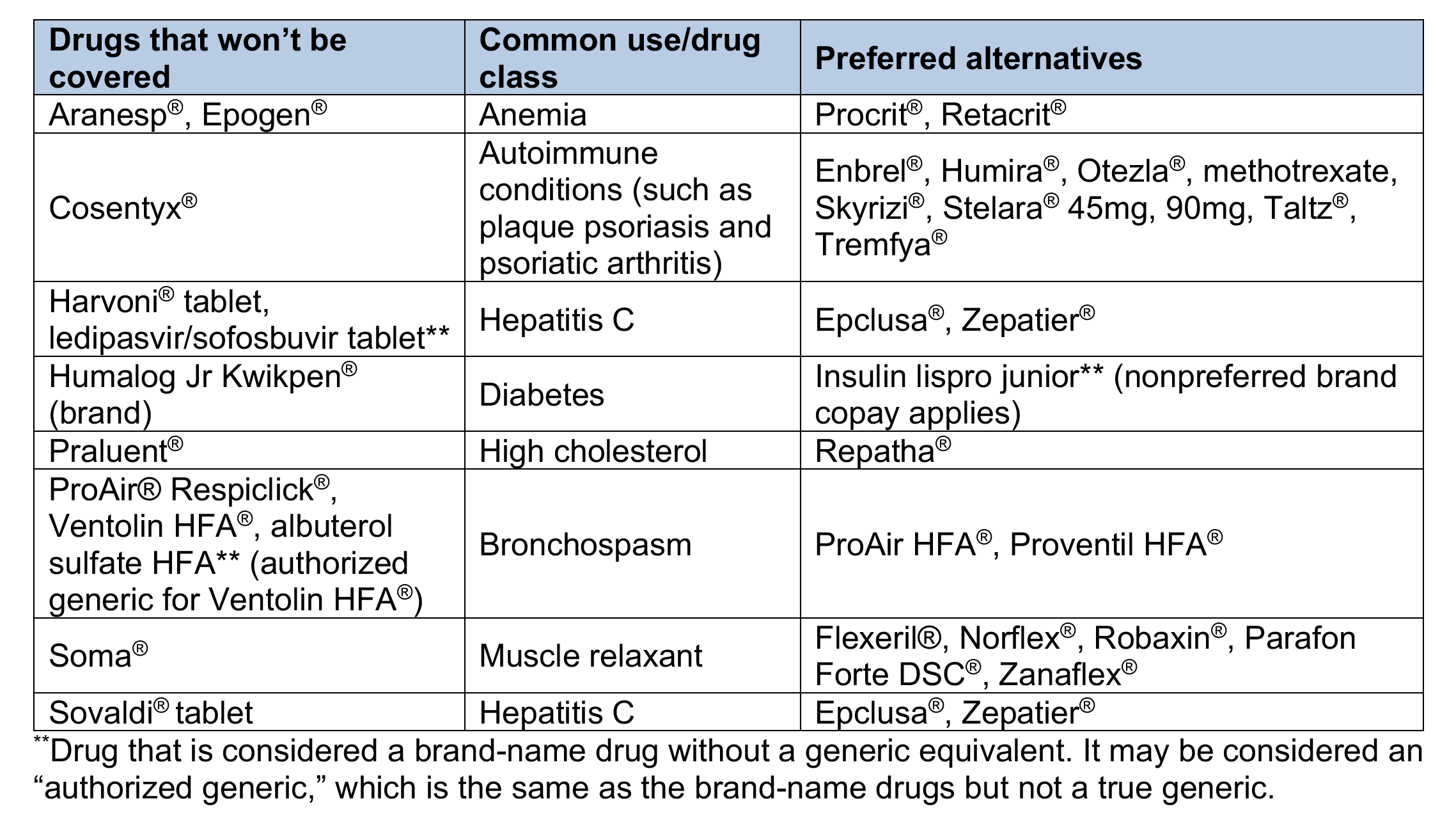 Drugs on the Clinical, Custom and Custom Select Drug Lists that will have quantity limits 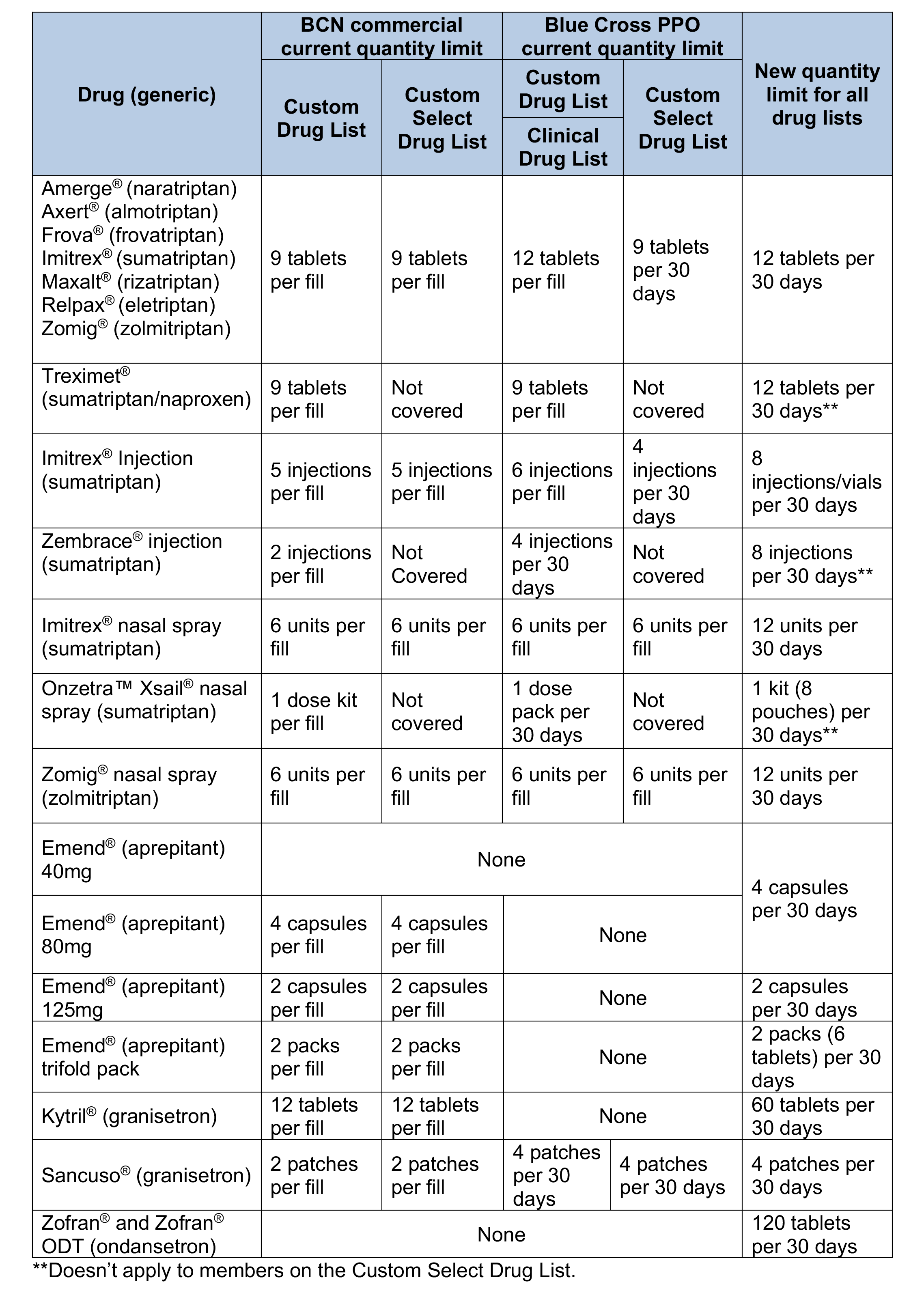
Medicare Part B medical specialty drug prior authorization list changing in January 2021We’re adding medications to the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue℠ and BCN Advantage℠ members. The specialty medications on this list are administered by a health care professional in a provider’s office, at the member’s home, in an off-campus outpatient hospital or in an ambulatory surgical center (place of service 11, 12, 19, 22 and 24). For dates of service on or after Jan. 1, 2021, the following CAR-T medications will require prior authorization through the NovoLogix® online tool:
The following medication will also require prior authorization through NovoLogix for dates of service on or after Jan. 1, 2021:
How to bill
Important reminder If you need to request access to Provider Secured Services, complete the Provider Secured Access Application form and fax it to the number on the form. List of requirements
Quarterly update: Requirements changed for some commercial medical benefit drugsBlue Cross Blue Shield of Michigan and Blue Care Network encourage proper utilization of high-cost medications covered under the medical benefit. One way we do this is by maintaining a comprehensive list of requirements for both Blue Cross and BCN commercial members. During July, August and September 2020, the following medical drugs had authorization requirement updates, site-of-care updates or both for Blue Cross commercial members:
For a detailed list of requirements, see the Blue Cross and BCN utilization management medical drug list. This list is available on the Blue Cross Medical Benefit Drugs page of the ereferrals.bcbsm.com website. The authorization requirements apply only to groups currently participating in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To view the list of Blue Cross commercial groups that don’t require members to participate in the program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group List. This list is also available on the Blue Cross Medical Benefit Drugs page of the ereferrals.bcbsm.com website. These changes don’t apply to Blue Cross and Blue Shield Federal Employee Program® members. As a reminder, an authorization approval isn’t a guarantee of payment. Health care providers need to verify eligibility and benefits for our members.
Starting Dec. 1, some drugs covered under medical benefit will require authorization for Blue Cross and Blue Shield FEP non-Medicare membersFor dates of service on or after Dec. 1, 2020, providers will have to request authorization from Blue Cross Blue Shield of Michigan for some drugs covered under the medical benefit for Blue Cross and Blue Shield Federal Employee Program® non-Medicare members. Authorization will be required only when members receive the drugs in Michigan. The drugs that will require authorization are listed in the Utilization management medical drug list for Blue Cross and Blue Shield Federal Employee Program non-Medicare members document. Note: For dates of service prior to Dec. 1, 2020, authorization isn’t required for drugs covered under the medical benefit for Blue Cross and Blue Shield FEP non-Medicare members. What you need to do
Resources The Blue Cross and Blue Shield FEP has its own policies for drugs that require authorization. The policies are available on the Medical Policies page of the Blue Cross and Blue Shield Federal Employee Program website. In mid-October, we’ll make available the list of medical benefit drugs that require authorization for Blue Cross and Blue Shield FEP non-Medicare members. Look for the list on the Blue Cross Medical Benefit Drugs page of the ereferrals.bcbsm.com website. We’ll have additional information in web-DENIS messages and in future issues of The Record. How to submit authorization requests You can submit authorization requests using one of the following methods:
Additional information Authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. The list of drugs in the Utilization management medical drug list for Blue Cross and Blue Shield Federal Employee Program non-Medicare members document applies only to Blue Cross and Blue Shield FEP non-Medicare members. For requirements related to drugs covered under the medical benefit for other Blue Cross commercial members and for BCN commercial members, see the following pages of the ereferrals.bcbsm.com website:
Blue Cross and BCN further extend authorization end dates on select medical and pharmacy benefit drugs for Medicare Advantage membersIn April 2020, we extended the authorization end dates for select medical and pharmacy benefit drugs for Medicare Plus Blue℠ and BCN Advantage℠ members. We did this to support our health care workers during the COVID-19 pandemic and to ensure that members’ access to medications wasn’t disrupted. We’re now further extending the end dates on authorizations for select medical and pharmacy benefit drugs for Medicare Plus Blue and BCN Advantage members.
Consult the Temporary changes due to the COVID-19 pandemic document for other changes temporarily put in place for the public health crisis. You can find this document on our public website at bcbsm.com/coronavirus and through Provider Secured Services.
Certain ambulatory infusion pump purchases to reject if not billed as rentals starting in JanuaryStarting on Jan. 1, 2021, the following HCPCS codes for ambulatory infusion pumps will only be reimbursed when billed as a rental:
The purchase of an ambulatory infusion pump will reject as provider liable. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 In the September Record, we announced that
In the September Record, we announced that