Subscribe | The Record Archive | Contacts | bcbsm.com
|
June 2025
Clinical editing updates: Prostate specimen re-bundle, biopsy specimen analysis; postpartum, global delivery; modifier 79; preadmission tests; place of service; anatomical modifiers; telehealth; code G2211In support of correct coding and payment accuracy, we are providing the information below to keep you informed about forthcoming payment policy updates, new policies and coding reminders. Blue Cross Blue Shield of Michigan commercial Prostate specimen re-bundle In June 2024, we communicated that Blue Cross commercial would be introducing a new edit starting Sept. 9, 2024, for prostate specimen re-bundling that would require code G0416 to be billed for prostate biopsies instead of *88305. After further consideration, we’ve decided not to implement this policy. This applies to professional and facility claims. Prostate biopsy specimen analysis We previously implemented editing for a prostate biopsy specimen analysis laboratory policy. Due to a system issue, editing for this policy hasn’t been enforced. The system issue has been fixed and editing on this policy resumed in April 2025. This applies to professional and facility claims. Reminder: Postpartum and global delivery Most delivery codes (for example, *59400 and *59510) already include postpartum care as part of the global service. It’s not appropriate to bill separate evaluation and management, or E/M, codes during the postpartum period. E/M services submitted during the postpartum period may be denied if the service is maternity-related. Unrelated E/M codes that require separate evaluation and management are allowed with the appropriate modifier. This applies to professional claims. Reminder: Modifier 79 Modifier 79 is used to indicate that the performance of a procedure or service during the postoperative period was unrelated to the original procedure. If no global procedure code was previously performed or billed for the member, the current claim with modifier 79 may not be reimbursed as this is inappropriate usage of modifier 79. This applies to professional claims. Modifier 79 description: Performance of a procedure or service during the postoperative period was unrelated to the original procedure. Reminder: Preadmission tests Blue Cross payment policy requires diagnosis-related group reimbursed hospitals to include all preadmission testing, given up to seven days before admission, on the inpatient claim. Claims submitted for preadmission testing services within seven days of a related inpatient stay may be denied if billed separately. If the inpatient claim has already been submitted without the preadmission tests, submit a corrected claim using type of bill 117 to replace the previous claim. This applies to facility claims. Reminder: Bill claims with correct place of service Select services have separate rates for physician services when given in facility and non-facility settings. The place of service submitted on a claim should reflect the setting the service was given. Claims submitted with an incorrect place of service may be denied. This applies to professional claims. Medicare Plus Blue℠ Radiology procedures requiring anatomical modifiers Correct coding guidelines regarding anatomical modifiers are important. Without the proper anatomical modifier applied to the procedure code, there is a risk of duplicate claims payment, incorrect procedure-to-procedure bundling, incorrect frequency limitations and potentially unnecessary medical record review. In May 2025, Medicare Plue Blue implemented an edit that denies radiology procedure codes requiring anatomical modifiers when the modifier isn’t present. Radiology codes with descriptors that don’t support the use of an anatomical modifier are exempt. The following are omitted modifiers affected by this edit:
If a provider receives a denial for a missing anatomical modifier, an appeal isn’t required. The radiology procedure can be resubmitted with the appropriate anatomical modifier for payment reconsideration. Blue Care Network commercial Telehealth Effective July 1, 2025, telehealth E/M procedure codes *98000, *98001, *98002, *98003, *98004, *98005, *98006, *98007, *98008, *98009, *98010, *98011, *98012, *98013, *98014 and *98015 will only be allowed when billed with place of service 02 or 10. Telehealth E/M procedure codes submitted without a telehealth place of service will be denied. Telehealth modifiers 93, 95, GT or FQ aren’t required for the telehealth E/M procedure codes. Also effective July 1, 2025, E/M procedure codes *99202, *99203, *99204, *99205, *99212, *99213, *99214 and *99215 billed with telehealth place of service 02 or 10 or telehealth modifiers 93, 95, GT or FQ will deny as provider liability. This applies to professional claims. BCN Advantage℠ Office, outpatient E/M visit complexity add-on code G2211 The Centers for Medicare & Medicaid Services added information on how to use G2211 with modifier 25 for certain Medicare Part B services starting Jan. 1, 2025. BCN Advantage is aware of the update and has worked diligently to update the system to accommodate these changes. System updates were finalized in May 2025. This applies to professional claims. None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Suicide prevention resources available for assessing at-risk patientsBlue Cross Blue Shield of Michigan supports the Zero Suicide Initiative, a Collaborative Quality Initiative supporting suicide prevention across Michigan. If a behavioral health screening indicates that a patient has risk factors for attempting suicide, the current standard of care is to assess the patient’s intent and risk. We’ve compiled best practices that all medical care and behavioral health providers should incorporate into the assessments of their patients. Resources for outpatient providers Question No. 9 asks patients if they’ve had “thoughts that you would be better off dead, or of hurting yourself.” If a patient responds with an affirmative answer to that question, then an additional assessment should be conducted. A provider can use a tool such as Ask Suicide-Screening Questions.** If a screening indicates that a patient has a significant risk of suicidal ideation, the provider should complete the Columbia-Suicide Severity Rating Scale for adults** or children or adolescents.** It’s a precise and valid method that helps determine suicide risk factors to discuss with family members or other supporters of the patient. Recognizing warning signs is a reasonable step to assess and protect patients from harm. Examples of warning signs are a patient’s history of previous suicide attempts, the specificity of a patient’s intent and plan, and the availability of lethal means (ideation, method, access and intent). Based on the assessment, here are options for interventions:
If providers don’t feel comfortable with or aren’t trained in performing these interventions, they should refer the patient to a mobile crisis team that can see him or her immediately. Mobile crisis teams can visit patients wherever they may be in their provider’s office, a school or work setting, their home or anywhere else. More information, including a list of behavioral health specialists and contact information, can be found at the Behavioral Health Crisis Care site. The National Action Alliance for Suicide Prevention** has a host of resources to assist providers in assessing and helping maintain patient safety in the face of suicidal ideation. The Recommended Standard Care for People with Suicide Risk: Making Health Care Suicide Safe** is a summary report with recommendations for outpatient behavioral health, emergency room and primary care settings. The Collaborative Care Model includes behavioral health specialists, such as a psychiatric consultant and behavioral health case manager, to assist medical practices in improving the mental health of their patients. Training and incentives are available to practices that register to become Collaborative Care practices. Behavioral health specialists who are part of the medical team — and assist the practice in treating behavioral health conditions — add backup and depth to the practice. These providers address situations with patients who are contemplating suicide and can provide expert direction in safely triaging or treating them. Primary care or obstetric/gynecologic practices interested in joining the Collaborative Care initiative should contact their physician organization for more information. Other questions can be directed to valuepartnerships@bcbsm.com. Note: If providers encounter patients who present an imminent risk of harm to themselves or others, it’s their professional and legal responsibility to take appropriate steps to help ensure their safety. The steps include notifying family, and law enforcement if appropriate, to assist the patient in getting mental health treatment. Table 2 of this American Family Physician article** has a list of questions that can help outpatient providers assess suicidal intent and risk. Resources for inpatient providers The Columbia-Suicide Severity Rating Scale serves multiple functions for inpatient behavioral health providers. It should be routinely administered for both internal and external documentation requirements. For inpatient behavioral health providers, using the scale for adults** or children or adolescents** serves several purposes:
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Starting July 7, Provider Inquiry will use one mailing address for Blue Cross commercial routine inquiriesAs we announced in a May 7, 2025, provider alert, starting July 7, 2025, Provider Inquiry will begin using one mailing address for all Blue Cross Blue Shield of Michigan commercial routine inquiries that can’t be handled by phone for health care providers in Michigan and outside of Michigan. For inquires that can’t be handled by phone, submit all routine inquiries to the following address to ensure they are handled as efficiently as possible: Provider Inquiry Routine inquiries regarding claims, eligibility and benefits can be handled more quickly and efficiently by calling Provider Inquiry. To speak with a Provider Inquiry representative, call one of the following numbers from 8:30 a.m. to 5 p.m. Eastern time Monday through Friday:
Do you have time for a Quality Minute about kidney health?This is another article in an ongoing series of quick tips designed to be read in 60 seconds or less and provide your practice with information about performance in key areas. Kidney Health Evaluation for Patients with Diabetes (KED) Did you know that kidney disease affects 35.5 million adults in the U.S., but 90% of them don’t know they have it? The HEDIS® measure Kidney Health Evaluation for Patients with Diabetes (KED) was developed to improve kidney disease testing in people with diabetes, because diabetes is a key risk factor for developing kidney disease. Tips to successfully close the KED gap
HEDIS®, which stands for Healthcare Effectiveness Data and Information Set, is a registered trademark of the National Committee for Quality Assurance or NCQA.
2025 CPT 2nd-quarter update: New, deleted codesThe American Medical Association has added 28 new proprietary laboratory analysis and vaccine codes as part of its CPT update. The codes, effective dates and Blue Cross Blue Shield of Michigan’s coverage decisions are below. Pathology and laboratory/proprietary laboratory analyses
Injection/vaccine
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Billing chart: Blue Cross highlights medical, benefit policy changesYou’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the “Billing chart.” The billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures. We’ll publish information about new Blue Cross groups or changes to group benefits under the Group Benefit Changes heading. For more detailed descriptions of Blue Cross’ policies for these procedures, check under the Commercial Policy tab in Benefit Explainer on Availity Essentials™. To access this online information:
To view the “June 2025 Billing chart,” click here. **Blue Cross Blue Shield of Michigan doesn’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Voluntary webinar series focuses on creating a welcoming environmentWhat you need to know This is a voluntary two-part webinar series on providing care to aging patients within the LGBTQ+ community. As we celebrate Pride Month in June, we're reminded of how important it is to provide quality care to all patients, including LGBTQ+ patients. At Blue Cross Blue Shield of Michigan and Blue Care Network, we're committed to helping primary care providers and office staff create a welcoming environment for all patients, regardless of their sexual orientation or gender identity. Creating a welcoming environment, such as offering staff training and the importance of updating patient intake forms, is crucial for providing high-quality care to all patients. By doing so, you can help improve patient outcomes. On-demand webinar series: Inclusive Care for LGBTQ+ Older Adults In partnership with the Michigan LGBTQ+ Elders Network, we're offering a voluntary, on-demand two-part webinar series, Inclusive Care for LGBTQ+ Older Adults, that focuses on the care needs of older LGBTQ+ patients. This series is available to providers, office staff and anyone interested in learning more about providing quality care. Here’s a brief breakdown of each webinar in the series: Part 1: Foundational concepts The first part of this series is focused on foundational concepts including:
Part 2: Creating a welcoming environment The second part of the series focuses on practical ways to make medical offices a welcoming environment including:
How to access the inclusive care webinar series
If you don’t have access to the provider portal, you can directly access the training through the provider training website. Earn credits and meet training requirements Medical assistants and other health care professionals can earn continuing education credits with a certificate of completion. Physicians are eligible for continuing medical education credits upon successful completion of this course and many other patient experience courses. For Patient-Centered Medical Home designated practices, completion of this webinar series supports training requirements for PCMH capability 5.16. See PCMH Interpretive Guidelines for more information. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. MiGen Michigan LGBTQ+ Elders Network is an independent nonprofit organization providing support to the LGBTQ+ senior community.
Review 2025 billing changes affecting provider-delivered care management servicesHere’s a summary of 2025 billing changes that affect provider-delivered care management services for Medicare Plus Blue℠ and BCN Advantage℠ members. Advanced primary care management services For 2025, the following HCPCS codes have been added for advanced primary care management, or APCM, services:
These HCPCS codes:
The HCPCS codes for APCM services are considered duplicative with procedure codes for chronic care management, principal care management, provider-delivered care management and transitional care management services. As a result, the APCM codes aren’t payable in the same month as the CCM, PCM, PDCM or TCM codes. Note: The new codes for APCM aren’t included in Blue Cross Blue Shield of Michigan or Blue Care Network’s PDCM program. Important: HCPCS codes G0556, G0557 and G0558 aren’t payable for Blue Cross or BCN commercial members. Rural health clinics and federally qualified health clinics As outlined by CMS, billing will change as follows for Medicare Advantage members who receive care management services at RHCs or FQHCs.
Medicare Advantage members who receive the above services at RHCs or FQHCs aren’t included in the denominator for our PDCM program.
Fees for new telemedicine E/M procedure codes to start July 1Blue Cross Blue Shield of Michigan and Blue Care Network will change practitioner fees for certain services provided on or after July 1, 2025. These changes may affect all health care providers — including behavioral health providers — for evaluation and management services provided through synchronous audio-video visits. Commercial members For Blue Cross and BCN commercial members, the Blue Cross and BCN fee schedules are the primary source of information about fees. To find the fee schedules:
Note: We published the article “Blue Cross’ updates to practitioner fees will take effect July 1” on March 31, 2025, in the April 2025 issue of The Record. Medicare Advantage members For Medicare Plus Blue℠ and BCN Advantage℠ members, follow the guidance from the Centers for Medicare & Medicaid Services when billing for telemedicine E/M services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Coding corner: Acute conditions not typically managed in office settingWhat you need to know
Accurate diagnosis coding is essential in risk-adjusted payment models, including Medicare Advantage and the ACA Marketplace. Some conditions, especially acute or life-threatening diagnoses, are expected to be treated in inpatient or emergency settings, not routinely managed in physician offices (place of service 11). Misreporting these diagnoses in outpatient settings can lead to improper risk score inflation and noncompliance with ICD-10 coding guidelines. Below are examples of acute conditions that shouldn’t be coded during an office visit unless clearly supported by documentation and appropriate clinical context. Cerebrovascular accident and acute ill-defined stroke An acute cerebrovascular accident, or CVA, is a medical emergency requiring inpatient care. If the patient has a history of stroke, the outpatient documentation must reflect “history of CVA” and specify any lasting deficits (for example, hemiparesis or aphasia) using appropriate late effects codes. Avoid using acute CVA codes (for example, I63.x) in outpatient settings unless the event is actively occurring and the patient is being evaluated emergently. Unstable angina, acute coronary syndrome and NSTEMI Unstable angina, acute coronary syndrome, or ACS, and non-ST-elevation myocardial infarction, or NSTEMI, represent acute cardiac syndromes and are typically managed in emergency departments or inpatient settings. Coding these diagnoses in an outpatient setting requires clear documentation that the patient was transferred for emergent evaluation. Office visits should not assign ACS, NSTEMI or unstable angina codes unless supported by documentation of active symptoms prompting urgent evaluation. Acute respiratory failure and acute on chronic respiratory failure Acute respiratory failure and acute on chronic respiratory failure signify a critical loss of respiratory function requiring immediate intervention and usually hospitalization. Coding acute respiratory failure in the office requires documentation of a recent hospitalization or a direct referral to higher care. If the patient has chronic respiratory failure without acute decompensation, use the chronic condition code (for example, J96.10). Sepsis and septicemia Sepsis represents a systemic, life-threatening response to infection and is almost always managed in a hospital. A diagnosis of sepsis in an office setting should only be coded if the provider is directly involved in acute care coordination, monitoring medications for treatment or the patient is being transferred for emergent treatment. If sepsis occurred in the past, and there are ongoing sequelae, use history of sepsis or appropriate late effect codes. Acute myocardial infarction Acute myocardial infarction, or MI, should only be coded when the patient is experiencing the event and receiving emergent treatment, typically in a hospital setting (POS 21 or 23). Outpatient visits after the acute episode must indicate a history of MI if the event occurred more than four weeks prior. Avoid using acute MI codes (for example, I21.x) in an office visit without supporting documentation of a recent or active event under evaluation. If follow-up of an NSTEMI is done within four weeks of a hospital stay, and the provider appropriately documents the care and treatment of the NSTEMI in the record, the NSTEMI can be coded on the outpatient record.
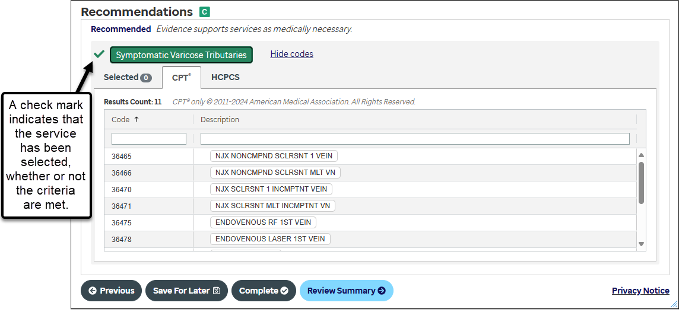
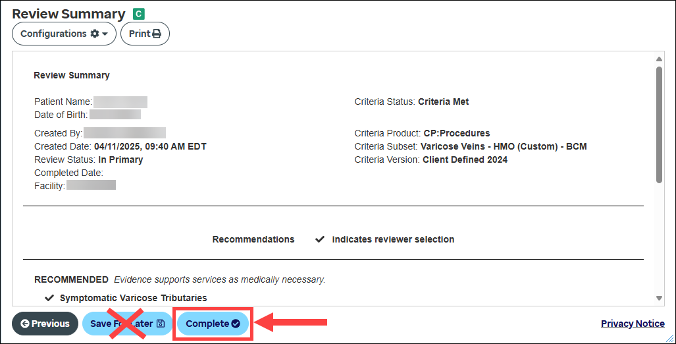
Best practices for prior authorization requests with InterQual Connect questions in e-referral systemAfter answering InterQual Connect questions in the e-referral system, do the following to ensure prior authorization requests for Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members are processed as quickly as possible:
Here’s what to do to submit a request after answering InterQual Connect questions in the e‑referral system:
Home health agencies now have more time to fulfill documentation requirement related to PT, OTBeginning June 1, 2025, Blue Cross Blue Shield of Michigan is expanding the commercial PPO documentation guidelines to allow home health agencies to obtain the health care provider’s signature within 60 days. Previously, home health agencies were required to obtain the provider’s signature within 30 days of the verbal order. Home health agencies must follow the other general documentation guidelines for physical therapy and occupational therapy. These guidelines can be found in the Blue Cross Commercial Provider Manual. There are no changes to the requirements for:
Select Medicare Advantage members will receive Cologuard test kits in JulyBlue Cross Blue Shield of Michigan and Blue Care Network are working with Exact Sciences, a credentialed colorectal cancer screening provider, to distribute in-home Cologuard® test kits in July to select Medicare Plus Blue℠ and BCN Advantage℠ members. Health care providers with patients who receive an advance notice about the kits should encourage them to take advantage of this convenient, no-cost screening. Members who have a gap in care for colorectal cancer screening will receive Cologuard screening kits. Members who received kits from a Blue Cross or BCN program in 2023 or 2024, or are due for a colonoscopy in 2025, are excluded. Members will be encouraged to discuss test results with their primary care providers. Test result notification
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Cologuard® by Exact Sciences is an independent company that provides colorectal testing services to Blue Cross Blue Shield of Michigan and Blue Care Network members.
Bill HCPCS code J3490 for Depo-Provera for commercial membersWhen submitting claims for Depo-Provera® (medroxyprogesterone) for Blue Cross Blue Shield of Michigan and Blue Care Network commercial members, do the following:
Use RC Claim Assist to identify the correct HCPCS code based on the NDC. For more information, see the document titled Using the RC Claim Assist tool: Frequently asked questions for providers. The Blue Cross or BCN Pharmacy department will look for the information specified above when reviewing claims for Depo-Provera. Note: Although Depo-Provera has an active HCPCS code, refer to RC Claim Assist to determine how to bill.
Pharmacy news roundupWhat you need to know To view all — including the most recent — pharmacy-related provider alerts:
Here are links to pharmacy-related provider alerts from April:
Tip: You can also subscribe to Provider Alerts Weekly to receive a weekly email with links to the previous week’s provider alerts. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Reminder: Chiropractors invited to join new quality reward program; enrollment closes June 30, 2025Action Item To reap the benefits of the new quality reward program, chiropractors need to opt in by June 30, 2025. For details, visit the chiropractic quality rewards website. As we told you in the January issue of The Record, Blue Cross Blue Shield of Michigan is offering all participating chiropractors the chance to join our new low back pain quality reward program. As part of the program, engaged chiropractors have an opportunity to earn a value-based reimbursement of 5% on eligible PPO professional claims for the pay period of Sept. 1, 2026, through Aug. 31, 2027. But you need to sign up by June 30, 2025, to be eligible. For more information about the program, see the January issue of The Record and the chiropractic quality rewards website.
Webinar for providers, office staff focuses on prior authorization best practicesAction item Visit our provider training site to register for a June webinar on prior authorization requests managed by Carelon Medical Benefits Management. Provider Experience continues to offer training resources for health care providers and staff. On-demand courses are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network. The following new learning opportunity is available: Prior authorization best practices — for requests managed by Carelon Medical Benefits Management: Register now for the webinar from 1 to 2 p.m. June 17. Topics include a walkthrough on how to determine if authorization is needed and case studies that show the most crucial elements for submitting requests. How to access provider training To access the training site, follow these steps:
Those who don’t have a provider portal account can directly access the training through the Provider training website. Questions? For more information about using the provider training website, contact the provider training team at ProviderTraining@bcbsm.com. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services.
Reminder: Registration still open for 2025 virtual provider symposium sessionsRegistration remains open for the four virtual health care provider symposiums in June. Physicians, physician assistants, nurse practitioners, nurses and coders can receive continuing education credits for attending. All the times listed below are Eastern time. All Star Performance-HEDIS®/Star Rating Measure Overview: The Golden Star Awards For physicians and office staff responsible for closing gaps in care related to quality measures for adults
Conducting an Internal Chart Audit: Livestreaming with April For physicians, coders, billers and administrative staff
Providers can find these symposiums on the provider training website. Once logged in to the site, open the event calendar to sign up. How to register on the provider training website Provider portal users with an Availity Essentials™ account can access the provider training website:
You can also directly access the training website if you don’t have a provider portal account. Questions?
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. HEDIS® is a registered trademark of the National Committee for Quality Assurance. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. Accreditation statement: This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of the Minnesota Medical Association and Blue Cross Blue Shield of Michigan. The Minnesota Medical Association (MMA) is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. CME statement: The Minnesota Medical Association designates this internet live activity for a maximum of 2 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Webinars for physicians, coders focus on documentation, codingAction item Register for our 2025 monthly Lunch & Learn webinars focusing on coding and documentation. In 2025, we’ll continue to offer webinars about documentation and coding of common challenging diagnoses. These live, lunchtime educational sessions will also include an opportunity to ask questions.
If you have an Availity Essentials™ account, you can access the provider training website this way:
Existing users who used the same email address as their provider portal profile email will be directed to the training site. If you used a different email address, contact ProviderTraining@bcbsm.com to update your profile. You can also directly access the training website if you don’t have a provider portal account by clicking here. After logging in to the provider training website, look in Event Calendar to sign up for your desired session. You can also quickly search for all the sessions with the keyword “lunchtime” and then look under the results for Events. You can listen to the previously recorded sessions, too. Check out the following:
Questions?
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Facts, figures, resources about cancer screeningThis is part of an ongoing series of articles focusing on the tools and resources available to help FEP® members manage their health. Cancer screening reduces the death rate for breast, cervical and colon cancers, according to information in the American Cancer Society’s Cancer Facts & Figures 2025** report. We have information that you can distribute to patients and HEDIS® tip sheets to help you close gaps in care for cancer screening. Breast cancer Since 1989, the female breast cancer death rate has declined by 44% as of 2022, according to the American Cancer Society’s report. This is due to early detection with screening mammography and increased awareness as well as improved treatment. This translates to approximately 517,900 fewer breast cancer deaths.
Cervical cancer Cervical cancer mortality rates have dropped by more than half since the mid-1970s due to early detection through screening and prevention. From 2003 to 2022, the rate stabilized at 0.7%, according to the American Cancer Society’s report.
Colon cancer Widespread use of colorectal cancer screenings began around 2000 for adults 50 and older. The overall rate for colon cancer has decreased by 1% per year. However, rates increased by 2.4% per year in people younger than 50, according to the American Cancer Society’s report.
If providers or members have questions about Federal Employee Program® benefits, they can call Customer Service at 1-800-482-3600 for Federal Employees Health Benefits or 1-877-760-8574 for Postal Service Health Benefits, or go to fepblue.org. **Blue Cross Blue Shield of Michigan doesn’t own or control this website. HEDIS®, which stands for Healthcare Effectiveness Data and Information Set, is a registered trademark of the National Committee for Quality Assurance or NCQA.
Reminder: Follow correct billing guidelines when submitting claims for secondary paymentHealth care facilities should submit secondary claims with a B3 amount equal to total charges only when the primary payer hasn’t made payment. We’re receiving claims that are billed incorrectly when payment has already been made by the primary payer. Billing errors cause a delay in payment due to the additional review that is required. This applies to claims for Blue Cross Blue Shield of Michigan commercial, Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members. Check out the following examples that demonstrate correct billing. Example 1 – Coordination of Benefits COB – Coordination of Benefits COB Value codes and amounts (FL 39-41 A-D) Electronic 837I loop 2300 HI01-2 through HI12-2
Example 2 – Coordination of Benefits COB – Primary Payer Rejected Entire Claim Value codes and amounts (FL 39-41 A-D) Electronic 837I loop 2300 HI01-2 through HI12-2
Example 3 - Coordination of Benefits COB – Primary Applied Deductible Value codes and amounts (FL 39-41 A-D) Electronic 837I loop 2300 HI01-2 through HI12-2
For more information on billing, refer to our provider manuals.
Fees for new telemedicine E/M procedure codes to start July 1Blue Cross Blue Shield of Michigan and Blue Care Network will change practitioner fees for certain services provided on or after July 1, 2025. These changes may affect all health care providers — including behavioral health providers — for evaluation and management services provided through synchronous audio-video visits. Commercial members For Blue Cross and BCN commercial members, the Blue Cross and BCN fee schedules are the primary source of information about fees. To find the fee schedules:
Note: We published the article “Blue Cross’ updates to practitioner fees will take effect July 1” on March 31, 2025, in the April 2025 issue of The Record. Medicare Advantage members For Medicare Plus Blue℠ and BCN Advantage℠ members, follow the guidance from the Centers for Medicare & Medicaid Services when billing for telemedicine E/M services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Coding corner: Acute conditions not typically managed in office settingWhat you need to know
Accurate diagnosis coding is essential in risk-adjusted payment models, including Medicare Advantage and the ACA Marketplace. Some conditions, especially acute or life-threatening diagnoses, are expected to be treated in inpatient or emergency settings, not routinely managed in physician offices (place of service 11). Misreporting these diagnoses in outpatient settings can lead to improper risk score inflation and noncompliance with ICD-10 coding guidelines. Below are examples of acute conditions that shouldn’t be coded during an office visit unless clearly supported by documentation and appropriate clinical context. Cerebrovascular accident and acute ill-defined stroke An acute cerebrovascular accident, or CVA, is a medical emergency requiring inpatient care. If the patient has a history of stroke, the outpatient documentation must reflect “history of CVA” and specify any lasting deficits (for example, hemiparesis or aphasia) using appropriate late effects codes. Avoid using acute CVA codes (for example, I63.x) in outpatient settings unless the event is actively occurring and the patient is being evaluated emergently. Unstable angina, acute coronary syndrome and NSTEMI Unstable angina, acute coronary syndrome, or ACS, and non-ST-elevation myocardial infarction, or NSTEMI, represent acute cardiac syndromes and are typically managed in emergency departments or inpatient settings. Coding these diagnoses in an outpatient setting requires clear documentation that the patient was transferred for emergent evaluation. Office visits should not assign ACS, NSTEMI or unstable angina codes unless supported by documentation of active symptoms prompting urgent evaluation. Acute respiratory failure and acute on chronic respiratory failure Acute respiratory failure and acute on chronic respiratory failure signify a critical loss of respiratory function requiring immediate intervention and usually hospitalization. Coding acute respiratory failure in the office requires documentation of a recent hospitalization or a direct referral to higher care. If the patient has chronic respiratory failure without acute decompensation, use the chronic condition code (for example, J96.10). Sepsis and septicemia Sepsis represents a systemic, life-threatening response to infection and is almost always managed in a hospital. A diagnosis of sepsis in an office setting should only be coded if the provider is directly involved in acute care coordination, monitoring medications for treatment or the patient is being transferred for emergent treatment. If sepsis occurred in the past, and there are ongoing sequelae, use history of sepsis or appropriate late effect codes. Acute myocardial infarction Acute myocardial infarction, or MI, should only be coded when the patient is experiencing the event and receiving emergent treatment, typically in a hospital setting (POS 21 or 23). Outpatient visits after the acute episode must indicate a history of MI if the event occurred more than four weeks prior. Avoid using acute MI codes (for example, I21.x) in an office visit without supporting documentation of a recent or active event under evaluation. If follow-up of an NSTEMI is done within four weeks of a hospital stay, and the provider appropriately documents the care and treatment of the NSTEMI in the record, the NSTEMI can be coded on the outpatient record.
Best practices for prior authorization requests with InterQual Connect questions in e-referral systemAfter answering InterQual Connect questions in the e-referral system, do the following to ensure prior authorization requests for Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members are processed as quickly as possible:
Here’s what to do to submit a request after answering InterQual Connect questions in the e‑referral system:
Medicare Advantage members can request a non-emergency transfer from one acute care facility to another at any timeFor Blue Cross Blue Shield of Michigan and Blue Care Network members, facilities must obtain authorization from Blue Cross or BCN before any non-emergency transfer of a member from one acute care inpatient medical or surgical (non-behavioral health) facility to another. As a reminder, Medicare Advantage (Medicare Plus Blue℠ and BCN Advantage℠) members who are currently admitted to an acute care inpatient medical or surgical facility can request a non-emergency transfer to another acute care inpatient facility of their choice at any time. For more information about acute care facility transfers, including urgent transfers, refer to the document Submitting acute inpatient authorization requests: Frequently asked questions for providers.
Home health agencies now have more time to fulfill documentation requirement related to PT, OTBeginning June 1, 2025, Blue Cross Blue Shield of Michigan is expanding the commercial PPO documentation guidelines to allow home health agencies to obtain the health care provider’s signature within 60 days. Previously, home health agencies were required to obtain the provider’s signature within 30 days of the verbal order. Home health agencies must follow the other general documentation guidelines for physical therapy and occupational therapy. These guidelines can be found in the Blue Cross Commercial Provider Manual. There are no changes to the requirements for:
Bill HCPCS code J3490 for Depo-Provera for commercial membersWhen submitting claims for Depo-Provera® (medroxyprogesterone) for Blue Cross Blue Shield of Michigan and Blue Care Network commercial members, do the following:
Use RC Claim Assist to identify the correct HCPCS code based on the NDC. For more information, see the document titled Using the RC Claim Assist tool: Frequently asked questions for providers. The Blue Cross or BCN Pharmacy department will look for the information specified above when reviewing claims for Depo-Provera. Note: Although Depo-Provera has an active HCPCS code, refer to RC Claim Assist to determine how to bill.
Pharmacy news roundupWhat you need to know To view all — including the most recent — pharmacy-related provider alerts:
Here are links to pharmacy-related provider alerts from April:
Tip: You can also subscribe to Provider Alerts Weekly to receive a weekly email with links to the previous week’s provider alerts. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||