Subscribe | The Record Archive | Contacts | bcbsm.com
|
March 2023
Provider Resources site adds new search toolSince launching our Blue Cross Blue Shield of Michigan and Blue Care Network Provider Resources site, we’ve continued to expand and improve it. We now have a search tool available to assist you in finding the information you need. You’ll find the search box in the upper right corner of every page and can use it to search the entire site, including PDFs. Like many searches, the Provider Resources search will return results even if your spelling isn’t quite right. Search hint: To search for an entire phrase, or to make sure you get your specific keyword higher in the search results, put quotation marks around it. As a reminder, the Provider Resources site replaced the BCBSM Newsletters and Resources and the BCN Provider Publications and Resources sites when we moved to our new provider portal. It has information for all lines of business, including provider alerts, forms and provider manuals. To get to the Provider Resources site:
To get to the Provider Resources site more quickly, make it a favorite in Availity® Essentials. On the Resources tab within our Payer Space, click on the heart icon next to Secure Provider Resources (Blue Cross and BCN). You’ll then be able to go directly to the Provider Resources site from the My Favorites drop-down menu in the top menu bar on any page of the provider portal. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
We’re migrating Medicare Plus Blue membership to new operating system beginning in 2024Blue Cross Blue Shield of Michigan is updating its internal processes in preparation for moving its Medicare Plus Blue℠ membership to a new operating system next year. The migration will take place in phases for groups and individual members in the January 2024 through January 2025 time frame.
Here are some key changes you should expect:
We’ll be providing more information about the migration in future issues of The Record over the next several months. Sample of new format Here’s a sample of what the first page of the new voucher will look like:
Blue Cross commercial subscriber IDs that started with 99 have changedSome Blue Cross Blue Shield of Michigan commercial group members had subscriber or enrollee IDs that began with 99. In January 2023, the subscriber/enrollee ID numbers for these members changed. This change didn’t affect the members’ benefits. For additional information — including how to look up members’ eligibility and benefits in our provider portal without entering a subscriber or enrollee ID — see the Jan. 6 provider alert. Billing chart: Blue Cross highlights medical, benefit policy changesYou’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart. This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures. We'll will publish information about new Blue Cross groups or changes to group benefits under the Group Benefit Changes heading. For more detailed descriptions of the Blue Cross' policies for these procedures, check under the Commercial Policy tab in Benefit Explainer on Availity®. To access this online information:
None of the information included in this billing chart is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Let’s focus on providing a stellar patient experienceThis is the first in a series of articles on the patient experience and why it matters to health care providers. Beginning this month and running through May, our members — your patients — will be asked to complete the annual CAHPS member survey. CAHPS, which stands for Consumer Assessment of Healthcare Providers and Systems, asks patients to report on a wide range of health care services they receive. A large portion of the CAHPS survey is driven by the patient’s experience with his or her primary health care provider and the provider’s health care team, including such factors as the ability to get timely doctor’s appointments and follow-up on labs and imaging. That’s why it’s so important for health care providers to focus on the patient experience. Patients who experience high-quality care and services from their doctor and health care team are more likely to be satisfied, loyal patients who make regular appointments and adhere to their treatment plans. This leads to healthier patients, better health care outcomes and, overall, lower health care costs since chronic conditions are better managed when a patient sees a primary care physician regularly. How to improve the patient experience What exactly can practices do to improve the patient experience? Here are some guidelines:
New tools you can use Our 2021 Blue Cross Blue Shield of Michigan physician survey showed that only 6 in 10 providers believe that Blue Cross is providing sufficient support to practices to help them improve the patient experience. That’s why we’ve ramped up our support for providers in this area over the past two years. Here are a few examples:
These offerings are fun, engaging and respectful of your busy schedules. You can participate at your convenience and also receive continuing education credits. CAHPS survey: A closer look The CAHPS survey, administered by the Agency for Healthcare Research and Quality, is sent to a random sample of members every spring to measure their experience with their health plan, prescription drug plan, health care providers and office staff. Many providers have asked us what kinds of questions patients are asked on the CAHPS survey. Here’s a sampling of the questions members will be asked about their health care experience when they receive their survey:
Answers that members provide influence the overall CAHPS score that a health plan receives. This score, in turn, plays a big role in a plan’s Medicare Star Ratings performance. CAHPS and Star Ratings are important to providers because they indicate how well patients think physicians and staff are performing in areas that matter most to them. “Many CAHPS metrics assess patient interactions with physicians and care delivery, including access to care, communication with physicians and the exchange of information between physicians,” said Sherri Dansby, director of Patient Experience. “Satisfied patients are more likely to trust physicians with their care and be more compliant with treatment plans, which can positively impact patient outcomes.” Over the past several years, the patient experience has played an increasingly important role in Medicare Star Ratings. In 2017, it represented 18% of our Star Ratings, but now accounts for 34% of our ratings. The link between patient experience and physician satisfaction Dansby added that practices offering a positive patient experience can also benefit physicians and staff. Good relationships with loyal patients can decrease staff burnout, stress and turnover. According to our 2021 physician survey, two-thirds of physicians (63%) reported feelings of burnout — levels that have more than doubled since 2017 — and 70% agree they struggle with staffing challenges. A total of 428 physicians responded to the survey. We appreciate all you do to improve the patient experience and hope your ongoing efforts lead to higher levels of physician and staff satisfaction as well. For information or to request a patient experience consultation, email PatientExperience@bcbsm.com. None of the information included in this article is intended to be medical advice and, as such, it remains the provider’s responsibility to ensure that any medical treatment is done in accordance with all applicable state, federal laws, regulations and/or medical board standards.
New Directions is now LucetOn Jan. 18, 2023, New Directions Behavioral Health changed its name to Lucet. Lucet will continue to provide behavioral health utilization management and case management services to Blue Cross Blue Shield of Michigan commercial members. Contact information, including phone and fax numbers, won’t change. You’ll continue to see New Directions’ name on our documents and webpages. For more information, see the Lucet Launches to Redefine Behavioral Health** blog post on lucethealth.com.** Lucet is an independent company that manages authorizations for behavioral health and autism services for Blue Cross Blue Shield of Michigan members who have commercial plans. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Legislation removes barriers to using buprenorphine to treat people with opioid use disorderThe Omnibus Spending Bill, which passed in December, marked a step forward in addressing the problem of opioid use disorder, or OUD. It included the Mainstreaming Addiction Treatment Act, which is a bipartisan effort that will help prevent overdoses, increase access to treatment and reduce stigma. The act removes many barriers in the prescription of medications for medication-assisted treatment for opioid use disorder, specifically buprenorphine, the most commonly prescribed of the MAT medications. This medication, along with naltrexone and naloxone, is considered by many to be among the principal tools in the treatment of OUD. However, medications are only part of the solution for treating people with OUD. Other approaches include:
“Case management can also be an effective tool in helping to ensure continued engagement, removing barriers to treatment and identifying non-adherence to treatment early so patients can get back on track more quickly,” said William Beecroft, M.D., medical director of behavioral health for Blue Cross Blue Shield of Michigan. “One of the main hallmarks of successful treatment is the patient’s continued engagement with the treatment program with no future use of the substance. OUD is a chronic illness, such as diabetes and heart disease, and needs to be addressed as such.” For more information about the Mainstreaming Addiction Treatment Act — and what barriers have been removed by this legislation — see this document** from the End Substance Use Disorder campaign. We’ll also include a column from Dr. Beecroft with additional details in the March-April issue of Hospital and Physician Update, which publishes in mid-March. To subscribe to Hospital and Physician Update or any of our other provider publications, click on this link. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Behavioral health providers: Hold claims for dates of service on or after Jan. 1, 2023, with codes *99354 and *99355Until further notice, behavioral health providers should hold claims for dates of service on or after Jan. 1, 2023, that contain procedure codes *99354 and *99355. These codes are for non-medical behavioral health prolonged services. The American Medical Association terminated codes *99354 and *99355, effective Jan. 1, 2023. If you submit claims with these codes for dates of service on or after Jan. 1, 2023, they won’t be accepted, even if the claims contain codes that are payable. Claims with dates of service prior to Jan. 1, 2023, can still be billed with these codes. We’re working on identifying active codes that can be billed in place of the terminated codes. Once we have a solution:
This applies to all our lines of business:
CoCM providers can now be found on Find a Doctor search toolHealth care providers who have received designation in our Collaborated Care Model, or CoCM, program were added to Blue Cross Blue Shield of Michigan’s Find a Doctor search feature in January. This means that our members can now more easily locate a provider who delivers Collaborative Care in their practice — much like they do to find doctors who participate in other key programs, such as our Patient-Centered Medical Home program. Designated providers, including OB/GYN providers, will be added to the provider search annually once PCMH and Collaborative Care designations are finalized. Here’s how to find a CoCM-designated provider:
Click on the CoCM logo to get more information about Collaborative Care.
Background The Collaborative Care Model is a value-based program based on the PCMH foundation. Providers with a Collaborative Care designation have a wide range of services and resources designed to:
Here’s what you need to know about SecureCareIn July 2022, Blue Cross Blue Shield of Michigan began working with SecureCare®, an independent network performance management company, to manage the provider utilization process for:
This management process program aims to obtain optimal outcomes for patients, while providing efficient, cost-effective care. Since the implementation of our collaboration with SecureCare, we’ve received some questions related to the program and wanted to provide the following information for clarification:
For more information
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Extended: Pilot program with TurningPoint to support patients’ musculoskeletal careIn March 2022, we started working with TurningPoint Healthcare Solutions LLC, an independent company, to offer the TurningPoint digital joint and spine pilot program. This program will run through June 2023. It was originally scheduled to end in December 2022. As a reminder, here are details about the program. The TurningPoint digital joint and spine pilot program aims to help:
The program is available to Blue Cross Blue Shield of Michigan commercial members. Blue Cross will identify members who are candidates for this program, and TurningPoint will reach out to those members to encourage them to register for the program. Members who engage with the program will complete an assessment through the TurningPoint Digital: Joint and Spine mobile app. Through their responses, TurningPoint will get an understanding of each member’s current treatment path or stage of treatment, which will enable TurningPoint to recommend next steps. In addition, the mobile app includes a library of physical therapy exercises that are developed by clinical experts and can help relieve members’ pain. When a member who is engaged in this program requires a musculoskeletal procedure, less clinical review will be required because the member has already been working with TurningPoint. There is no cost to members for this program. If you have questions about this program, send them to umproviderconcerns@bcbsm.com.
Guidelines recommend conservative care for acute low back pain and acute bronchitisThis is part of an ongoing series of articles focusing on the tools and resources available to help FEP members manage their health. The Michigan Quality Improvement Consortium guidelines recommend conservative treatment for acute low back pain** and acute bronchitis.** Following are a couple of resources that may help patients understand why a more conservative approach is better for acute low back pain and acute bronchitis conditions: Health care providers and members can call Customer Service at 1-800-482-3600 or go online to fepblue.org if they have questions about FEP support services and benefits. None of the information included in this article is intended to be medical advice and, as such, it remains the health care provider’s responsibility to ensure that any medical treatment is done in accordance with all applicable state, federal laws, regulations and/or medical board standards. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
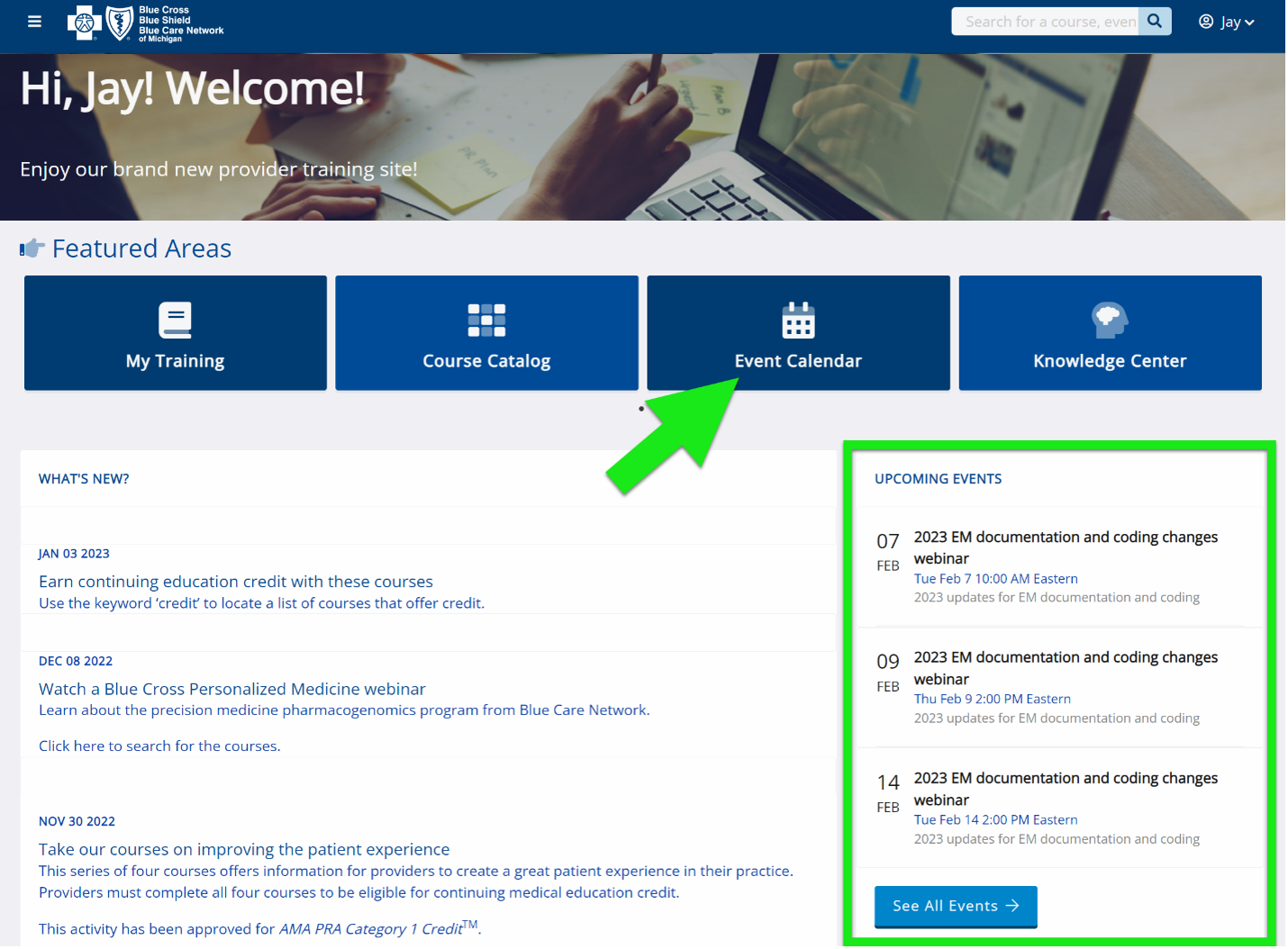
Lunch and learn webinars for physicians and coders focus on risk adjustment, codingBeginning in April 2023, we’ll be offering webinars that will provide updated information on documentation and coding of common challenging diagnoses. These live lunchtime educational sessions will also include an opportunity to ask any questions that you may have. Here’s our current schedule and the tentative topics for the sessions. All sessions start at noon Eastern time and generally last for 30 minutes. Log in to the provider training website and register for the session that best works with your schedule.
Click here if you are already registered for the provider training website. After logging in to the provider training website, look in Event Calendar to sign up for the desired session.
To request access to the provider training website:
If you have any questions about the sessions, contact April Boyce at aboyce@bcbsm.com. If you have questions regarding registration, email ProviderTraining@bcbsm.com.
Reminder: Register now for 2023 virtual provider symposium sessionsAs you may have read in the February Record, this year’s virtual provider symposiums run throughout May and June. Physicians, physician assistants, nurse practitioners, nurses and coders can receive continuing education credits for attending. You’re welcome to register for any session listed below. Click here to log in to the provider training website to register for sessions. You can easily create an account if you don’t already have access: Click here to register. We recommend that you use the same email address you use to communicate with Blue Cross Blue Shield of Michigan when creating the account. Once you’re logged in to the provider training site, open the event calendar to sign up for any of the following sessions. Reach for the Stars-HEDIS®/Star Measure Overview: For physicians and office staff responsible for closing gaps in care related to quality adult measures.
Patient Experience: For physicians and office staff responsible for creating positive patient experiences. Learn how to ensure your practice has the knowledge and tools needed to set and meet patients’ expectations.
Coding Complex Cases: For physicians, coders, billers and administrative staff
Questions? Contact Ellen Kraft at ekraft@bcbsm.com if you have questions about the sessions. Contact the provider training team at ProviderTraining@bcbsm.com if you have questions about registration or using the provider training website. HEDIS® is a registered trademark of the National Committee for Quality Assurance.
Additional drugs to require prior authorization for Medicare Advantage members, starting March 1For dates of service on or after March 1, 2023, the following drugs will require prior authorization for Medicare Plus Blue℠ and BCN Advantage℠ members. These drugs are part of members’ medical benefits, not their pharmacy benefits.
Submit prior authorization requests through the NovoLogix® online tool. When prior authorization is required These medications require prior authorization when they’re administered by a health care provider in sites of care such as outpatient facilities or physicians’ offices, and are billed in one of the following ways:
Submit prior authorization requests through NovoLogix To access NovoLogix, log in to our provider portal (availity.com),** click on Payer Spaces in the menu bar and then click on the BCBSM and BCN logo. You’ll find links to the NovoLogix tools on the Applications tab. Note: If you need to request access to our provider portal, follow the instructions on the Register for web tools webpage on bcbsm.com/providers. List of requirements For a list of requirements related to drugs covered under the medical benefit, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members. We'll update the list to reflect these changes prior to the effective date. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield and Blue Care Network don’t own or control this website.
Byooviz is no longer preferred ranibizumab drug for Medicare Advantage membersBecause Byooviz® is no longer the preferred ranibizumab drug for Medicare Plus Blue℠ and BCN Advantage℠ members, it’s no longer a step therapy requirement when prescribing Lucentis®. As a result, providers no longer need to include clinical documentation showing that the patient has tried Byooviz when submitting prior authorization requests for Lucentis with dates of service on or after Jan. 9, 2023. We continue to require that the member first try and fail Avastin® (bevacizumab) before Byooviz or Lucentis are prescribed. The HCPCS codes for Avastin are J3590 for Medicare Plus Blue and J9035 for BCN Advantage. As a reminder, Avastin doesn’t require prior authorization when used for retinal conditions. These drugs are covered under members’ medical benefits. Prior authorization still required Both Byooviz and Lucentis continue to require prior authorization when administered by a health care provider in sites of care such as outpatient facilities or physician offices and billed in one of the following ways:
Submit prior authorization requests through the NovoLogix® tool Submit prior authorization requests for both Byooviz and Lucentis using NovoLogix. It offers real-time status checks and immediate approvals for certain medications. To access NovoLogix, log in to our provider portal (availity.com),** click on Payer Spaces and then click on the BCBSM and BCN logo. This will take you to the Blue Cross and BCN payer space, where you’ll find links to the NovoLogix tools on the Applications tab. If you need to request access to Availity®, follow the instructions on the Register for web tools webpage at bcbsm.com/providers. Reminder about requirements for other retinal drugs All other intravitreal drugs for retinal conditions still have Avastin as a step therapy requirement. These drugs are:
List of requirements For a list of requirements related to drugs covered under the medical benefit, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Leqembi to require prior authorization for Medicare Advantage members starting Jan. 13For dates of service on or after Jan. 13, 2023, we’ve added a prior authorization requirement for Medicare Plus Blue℠ and BCN Advantage℠ members for the following drug:
This drug is a part of members’ medical benefits, not their pharmacy benefits. When prior authorization is required Leqembi requires prior authorization when it’s administered by a health care provider in sites of care such as outpatient facilities or physician offices, and is billed in one of the following ways:
Submit prior authorization requests through the NovoLogix tool To access NovoLogix, log in to our provider portal (availity.com),** click on Payer Spaces and then click on the BCBSM and BCN logo. This will take you to the Blue Cross and BCN payer space, where you’ll find links to the NovoLogix tools on the Applications tab. Note: If you need to request access to Availity®, follow the instructions on the Register for web tools webpage at bcbsm.com/providers. List of requirements For a list of requirements related to drugs covered under the medical benefit, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members. Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Generic pemetrexed requires prior authorization for Medicare Advantage membersFor dates of service on or after Jan. 1, 2023, the following drug requires prior authorization through AIM Specialty Healthl®:
As a reminder, we previously communicated the following requirements for brand-name drugs:
These requirements apply to Medicare Plus Blue℠ and BCN Advantage℠ members. These medications are part of members’ medical benefits, not their pharmacy benefits. When prior authorization is required These drugs require prior authorization when administered by a health care provider in an outpatient facility or physician’s office and billed in one of the following ways:
How to submit authorization requests Submit prior authorization requests to AIM using one of the following methods:
List of requirements For a list of requirements related to drugs covered under the medical benefit, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. AIM Specialty Health is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services. For more information, go to our ereferrals.bcbsm.com website. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Rebyota to require prior authorization for Medicare Advantage members starting March 1For dates of service on or after March 1, 2023, the following drug will require prior authorization for Medicare Plus Blue℠ and BCN Advantage℠ members. This drug is part of members’ medical benefits, not their pharmacy benefits.
Submit prior authorization requests through the NovoLogix® online tool. When prior authorization is required Rebyota will require prior authorization when it’s administered by a health care provider in sites of care such as outpatient facilities or physician offices and billed in one of the following ways:
Submit prior authorization requests through the NovoLogix tool To access NovoLogix, log in to our provider portal (availity.com),** click on Payer Spaces in the menu bar and then click on the BCBSM and BCN logo. You’ll find links to the NovoLogix tools on the Applications tab. Note: If you need to request access to our provider portal, follow the instructions on the Register for web tools webpage on bcbsm.com/providers. List of requirements For a list of requirements related to drugs covered under the medical benefit, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue PPO and BCN Advantage members. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Transfer Medicare Advantage members to post-acute care facilities immediately after appeals are approvedAction item You should transfer patients as soon as you receive notification that an appeal has been approved. Don’t wait to receive an authorization number, which will be provided later. When you submit an expedited appeal to Blue Cross Blue Shield of Michigan or Blue Care Network, we have 72 hours to approve or deny the appeal. Within those 72 hours, we’ll send a fax to inform you of our determination. Once you receive a fax from us stating that an appeal has been approved, you can immediately transfer the member to a post-acute care facility. Although naviHealth will provide an authorization number later, don’t wait for that number to transfer the patient. The fax you received serves as proof of the approval. Post-acute care providers should accept the transfer based on the faxed notification stating that we approved the appeal. If you’d like a status update on an appeal request, call us at:
How to submit an appeal to get the fastest response For the fastest response to your appeal request:
If you don’t have a copy of the denial letter, you can request a copy from naviHealth by calling 1-855-851-0843 or by submitting a request through nH Access. For your convenience, the fax numbers for submitting appeals are:
Reminder As a reminder, the Medicare Plus Blue and BCN Advantage Grievance and Appeals units handle requests to appeal denials of post-acute care services for both prior authorization requests and retroactive authorization requests. Additional information For additional information about post-acute care services for Medicare Advantage members, see the Post-acute care services: Frequently asked questions for providers document. naviHealth Inc. is an independent company that manages authorizations for post-acute care services for Blue Cross Blue Shield of Michigan and Blue Care Network members who have Medicare Advantage plans.
New Directions is now LucetOn Jan. 18, 2023, New Directions Behavioral Health changed its name to Lucet. Lucet will continue to provide behavioral health utilization management and case management services to Blue Cross Blue Shield of Michigan commercial members. Contact information, including phone and fax numbers, won’t change. You’ll continue to see New Directions’ name on our documents and webpages. For more information, see the Lucet Launches to Redefine Behavioral Health** blog post on lucethealth.com.** Lucet is an independent company that manages authorizations for behavioral health and autism services for Blue Cross Blue Shield of Michigan members who have commercial plans. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Legislation removes barriers to using buprenorphine to treat people with opioid use disorderThe Omnibus Spending Bill, which passed in December, marked a step forward in addressing the problem of opioid use disorder, or OUD. It included the Mainstreaming Addiction Treatment Act, which is a bipartisan effort that will help prevent overdoses, increase access to treatment and reduce stigma. The act removes many barriers in the prescription of medications for medication-assisted treatment for opioid use disorder, specifically buprenorphine, the most commonly prescribed of the MAT medications. This medication, along with naltrexone and naloxone, is considered by many to be among the principal tools in the treatment of OUD. However, medications are only part of the solution for treating people with OUD. Other approaches include:
“Case management can also be an effective tool in helping to ensure continued engagement, removing barriers to treatment and identifying non-adherence to treatment early so patients can get back on track more quickly,” said William Beecroft, M.D., medical director of behavioral health for Blue Cross Blue Shield of Michigan. “One of the main hallmarks of successful treatment is the patient’s continued engagement with the treatment program with no future use of the substance. OUD is a chronic illness, such as diabetes and heart disease, and needs to be addressed as such.” For more information about the Mainstreaming Addiction Treatment Act — and what barriers have been removed by this legislation — see this document** from the End Substance Use Disorder campaign. We’ll also include a column from Dr. Beecroft with additional details in the March-April issue of Hospital and Physician Update, which publishes in mid-March. To subscribe to Hospital and Physician Update or any of our other provider publications, click on this link. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Behavioral health providers: Hold claims for dates of service on or after Jan. 1, 2023, with codes *99354 and *99355Until further notice, behavioral health providers should hold claims for dates of service on or after Jan. 1, 2023, that contain procedure codes *99354 and *99355. These codes are for non-medical behavioral health prolonged services. The American Medical Association terminated codes *99354 and *99355, effective Jan. 1, 2023. If you submit claims with these codes for dates of service on or after Jan. 1, 2023, they won’t be accepted, even if the claims contain codes that are payable. Claims with dates of service prior to Jan. 1, 2023, can still be billed with these codes. We’re working on identifying active codes that can be billed in place of the terminated codes. Once we have a solution:
This applies to all our lines of business:
Here’s what you need to know about SecureCareIn July 2022, Blue Cross Blue Shield of Michigan began working with SecureCare®, an independent network performance management company, to manage the provider utilization process for:
This management process program aims to obtain optimal outcomes for patients, while providing efficient, cost-effective care. Since the implementation of our collaboration with SecureCare, we’ve received some questions related to the program and wanted to provide the following information for clarification:
For more information
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Reminder: Here’s information skilled nursing facilities must submit to naviHealth for services provided to Medicare Advantage membersFor Medicare Plus Blue℠ and BCN Advantage℠ members, skilled nursing facilities must submit certain items to naviHealth within specific time frames. Therapy and nursing assessments Skilled nursing facilities must submit physical therapy, occupational therapy, speech therapy and nursing assessments to naviHealth within 48 hours of a member’s admission to a skilled nursing facility. naviHealth uses these assessments to:
Clinical documentation and assessments for calculating CMG levels By Day 7 of a member’s stay, skilled nursing facilities must submit the following items to naviHealth, so it can calculate the case mix group, or CMG, level:
naviHealth will calculate the CMG level within two days of receiving clinical documentation and assessments. It will use the CMG level to generate patient-driven payment model, or PDPM, codes. Those codes are used for billing. Requirements for reassessments of CMG levels After naviHealth has calculated the CMG level, skilled nursing facilities can submit requests to reassess CMG levels. Be sure to request the reassessment prior to discharging the member from skilled services. Send the clinical documentation required for the reassessment to naviHealth as soon as possible. Clinical documentation for the reassessment of CMG levels includes — but isn’t limited to — information from the most recent history and physical, transfer documents, physician progress notes, discharge summaries, nursing assessments, nursing care plans, medication sheets, doctor’s orders, consults and diagnostic reports. naviHealth will use the clinical documentation to determine whether to change the CMG level. The health care provider must identify where the supporting documentation appears within the clinical documentation. If naviHealth determines that the CMG level should change, it will change the level retroactive to the day of admission. You can use the Request for a Reassessment of the CMG Level worksheet to ensure that you submit comprehensive clinical documentation to support the request. You can find this worksheet two ways:
Note: The decision to change a CMG level may require review of the request by a naviHealth medical director. Additional information If you have questions about the information in this article, contact your naviHealth care coordinator or your naviHealth provider relations manager. You can also find more information in Post-acute care services: Frequently asked questions for providers. naviHealth Inc. is an independent company that manages authorizations for post-acute care services for Blue Cross Blue Shield of Michigan and Blue Care Network members who have Medicare Advantage plans. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Extended: Pilot program with TurningPoint to support patients’ musculoskeletal careIn March 2022, we started working with TurningPoint Healthcare Solutions LLC, an independent company, to offer the TurningPoint digital joint and spine pilot program. This program will run through June 2023. It was originally scheduled to end in December 2022. As a reminder, here are details about the program. The TurningPoint digital joint and spine pilot program aims to help:
The program is available to Blue Cross Blue Shield of Michigan commercial members. Blue Cross will identify members who are candidates for this program, and TurningPoint will reach out to those members to encourage them to register for the program. Members who engage with the program will complete an assessment through the TurningPoint Digital: Joint and Spine mobile app. Through their responses, TurningPoint will get an understanding of each member’s current treatment path or stage of treatment, which will enable TurningPoint to recommend next steps. In addition, the mobile app includes a library of physical therapy exercises that are developed by clinical experts and can help relieve members’ pain. When a member who is engaged in this program requires a musculoskeletal procedure, less clinical review will be required because the member has already been working with TurningPoint. There is no cost to members for this program. If you have questions about this program, send them to umproviderconcerns@bcbsm.com.
Lunch and learn webinars for physicians and coders focus on risk adjustment, codingBeginning in April 2023, we’ll be offering webinars that will provide updated information on documentation and coding of common challenging diagnoses. These live lunchtime educational sessions will also include an opportunity to ask any questions that you may have. Here’s our current schedule and the tentative topics for the sessions. All sessions start at noon Eastern time and generally last for 30 minutes. Log in to the provider training website and register for the session that best works with your schedule.
Click here if you are already registered for the provider training website. After logging in to the provider training website, look in Event Calendar to sign up for the desired session.
To request access to the provider training website:
If you have any questions about the sessions, contact April Boyce at aboyce@bcbsm.com. If you have questions regarding registration, email ProviderTraining@bcbsm.com.
Additional drugs to require prior authorization for Medicare Advantage members, starting March 1For dates of service on or after March 1, 2023, the following drugs will require prior authorization for Medicare Plus Blue℠ and BCN Advantage℠ members. These drugs are part of members’ medical benefits, not their pharmacy benefits.
Submit prior authorization requests through the NovoLogix® online tool. When prior authorization is required These medications require prior authorization when they’re administered by a health care provider in sites of care such as outpatient facilities or physicians’ offices, and are billed in one of the following ways:
Submit prior authorization requests through NovoLogix To access NovoLogix, log in to our provider portal (availity.com),** click on Payer Spaces in the menu bar and then click on the BCBSM and BCN logo. You’ll find links to the NovoLogix tools on the Applications tab. Note: If you need to request access to our provider portal, follow the instructions on the Register for web tools webpage on bcbsm.com/providers. List of requirements For a list of requirements related to drugs covered under the medical benefit, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members. We'll update the list to reflect these changes prior to the effective date. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield and Blue Care Network don’t own or control this website.
Byooviz is no longer preferred ranibizumab drug for Medicare Advantage membersBecause Byooviz® is no longer the preferred ranibizumab drug for Medicare Plus Blue℠ and BCN Advantage℠ members, it’s no longer a step therapy requirement when prescribing Lucentis®. As a result, providers no longer need to include clinical documentation showing that the patient has tried Byooviz when submitting prior authorization requests for Lucentis with dates of service on or after Jan. 9, 2023. We continue to require that the member first try and fail Avastin® (bevacizumab) before Byooviz or Lucentis are prescribed. The HCPCS codes for Avastin are J3590 for Medicare Plus Blue and J9035 for BCN Advantage. As a reminder, Avastin doesn’t require prior authorization when used for retinal conditions. These drugs are covered under members’ medical benefits. Prior authorization still required Both Byooviz and Lucentis continue to require prior authorization when administered by a health care provider in sites of care such as outpatient facilities or physician offices and billed in one of the following ways:
Submit prior authorization requests through the NovoLogix® tool Submit prior authorization requests for both Byooviz and Lucentis using NovoLogix. It offers real-time status checks and immediate approvals for certain medications. To access NovoLogix, log in to our provider portal (availity.com),** click on Payer Spaces and then click on the BCBSM and BCN logo. This will take you to the Blue Cross and BCN payer space, where you’ll find links to the NovoLogix tools on the Applications tab. If you need to request access to Availity®, follow the instructions on the Register for web tools webpage at bcbsm.com/providers. Reminder about requirements for other retinal drugs All other intravitreal drugs for retinal conditions still have Avastin as a step therapy requirement. These drugs are:
List of requirements For a list of requirements related to drugs covered under the medical benefit, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Leqembi to require prior authorization for Medicare Advantage members starting Jan. 13For dates of service on or after Jan. 13, 2023, we’ve added a prior authorization requirement for Medicare Plus Blue℠ and BCN Advantage℠ members for the following drug:
This drug is a part of members’ medical benefits, not their pharmacy benefits. When prior authorization is required Leqembi requires prior authorization when it’s administered by a health care provider in sites of care such as outpatient facilities or physician offices, and is billed in one of the following ways:
Submit prior authorization requests through the NovoLogix tool To access NovoLogix, log in to our provider portal (availity.com),** click on Payer Spaces and then click on the BCBSM and BCN logo. This will take you to the Blue Cross and BCN payer space, where you’ll find links to the NovoLogix tools on the Applications tab. Note: If you need to request access to Availity®, follow the instructions on the Register for web tools webpage at bcbsm.com/providers. List of requirements For a list of requirements related to drugs covered under the medical benefit, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members. Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Generic pemetrexed requires prior authorization for Medicare Advantage membersFor dates of service on or after Jan. 1, 2023, the following drug requires prior authorization through AIM Specialty Healthl®:
As a reminder, we previously communicated the following requirements for brand-name drugs:
These requirements apply to Medicare Plus Blue℠ and BCN Advantage℠ members. These medications are part of members’ medical benefits, not their pharmacy benefits. When prior authorization is required These drugs require prior authorization when administered by a health care provider in an outpatient facility or physician’s office and billed in one of the following ways:
How to submit authorization requests Submit prior authorization requests to AIM using one of the following methods:
List of requirements For a list of requirements related to drugs covered under the medical benefit, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. AIM Specialty Health is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services. For more information, go to our ereferrals.bcbsm.com website. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Rebyota to require prior authorization for Medicare Advantage members starting March 1For dates of service on or after March 1, 2023, the following drug will require prior authorization for Medicare Plus Blue℠ and BCN Advantage℠ members. This drug is part of members’ medical benefits, not their pharmacy benefits.
Submit prior authorization requests through the NovoLogix® online tool. When prior authorization is required Rebyota will require prior authorization when it’s administered by a health care provider in sites of care such as outpatient facilities or physician offices and billed in one of the following ways:
Submit prior authorization requests through the NovoLogix tool To access NovoLogix, log in to our provider portal (availity.com),** click on Payer Spaces in the menu bar and then click on the BCBSM and BCN logo. You’ll find links to the NovoLogix tools on the Applications tab. Note: If you need to request access to our provider portal, follow the instructions on the Register for web tools webpage on bcbsm.com/providers. List of requirements For a list of requirements related to drugs covered under the medical benefit, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue PPO and BCN Advantage members. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||