Subscribe | The Record Archive | Contacts | bcbsm.com
|
March 2025
We’ll use 2025 InterQual criteria starting June 1For dates of service on or after June 1, 2025, Blue Cross Blue Shield of Michigan and Blue Care Network will use 2025 InterQual® criteria to make determinations on the prior authorization requests for the medical (nonbehavioral health) services we manage for these members:
Note: If the InterQual criteria are updated to correct known issues or errors, we’ll use the updated criteria as soon as they’re available. For Blue Cross and BCN commercial members, we also use Local Rules when making determinations on post-acute care (inpatient rehabilitation, skilled nursing facility and long-term acute care) prior authorization requests. These Local Rules are modifications of InterQual criteria that we use in making determinations. You can access the Local Rules on the Services That Need Prior Authorization page on bcbsm.com. We’ll update that page to include the most current version of the Local Rules. Refer to the table below for specific information about which criteria we use in making determinations for various types of nonbehavioral health prior authorization requests.
When clinical information is requested for a medical or surgical admission or other services, we require providers to submit specific components of the medical record that show the request meets the criteria. We review this information when making determinations on prior authorization requests. Note: The information in this article applies to members whose authorizations are managed by Blue Cross or BCN directly and not by independent companies that provide services to Blue Cross or BCN.
How to find which procedure codes require authorization by Carelon or EviCoreWe’ve retired the documents listed below:
To determine which procedure codes require prior authorization, use the document titled Procedure codes for which providers must request prior authorization. Here’s what you need to know:
Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services. EviCore by Evernorth is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services.
Reminder: Follow guidelines established for processing Medicare primary claimsWhat you need to know
Medicare primary claims must be submitted to Medicare for processing. Medicare is then responsible for forwarding the claims to Blue Cross Blue Shield of Michigan through a crossover arrangement for secondary payment determinations. Blue Cross requires, at minimum, a 30-day waiting period after the Medicare remittance date before we can accept and process a health care provider-submitted Medicare supplemental claim that is eligible for crossover. Electronic professional and facility claims received before the 30-day waiting period will obtain the following Blue Cross front-end edit:
Check your response files (acknowledgments and reports) and payer (277CA) reports for front-end edits through Availity Essentials™, our provider portal. Edited claims can’t be resubmitted until 30 days after the Medicare remittance date has lapsed. You should only bill Blue Cross directly before the 30-day remittance date for a patient with Medicare primary coverage when the service provided is statutorily excluded from Medicare coverage. For statutorily excluded services, it’s important to note:
Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Get easy access to information about our care management, utilization management programsAction item Bookmark the Care management and utilization management programs: Overview for providers document in your internet browser to make it faster and easier to access the most up-to-date information about these programs. We publish the Care management and utilization management programs: Overview for providers document to help you navigate Blue Cross Blue Shield of Michigan’s and Blue Care Network’s care management and utilization management programs. We recently updated it — and the documents linked within it — to reflect changes that went into effect Jan. 1, 2025. We’ll continue to make updates as information changes. This easy-to-use, one-page document tells you what you need to know about these two categories of programs:
The programs vary based on member coverage and may be administered by Blue Cross or BCN staff or by independent companies. You can also access the document by clicking on the Care and utilization management programs: Overview for providers link at the bottom of each page of our ereferrals.bcbsm.com website.
Pharmacy news roundupWhat you need to know To view all — including the most recent — pharmacy-related provider alerts:
Here are links to pharmacy-related provider alerts from January:
Tip: You can also subscribe to Provider Alerts Weekly to receive a weekly email with links to the previous week’s provider alerts. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Patient experience resources to support your practiceWhat you need to know Blue Cross encourages health care providers to explore the expanded library of content on patient experience. Blue Cross Blue Shield of Michigan has expanded the patient experience library of content, which is found on the provider training website. Patient experience refers to all interactions patients have with their doctors and staff. Positive patient experiences can drive patient loyalty and promote a cohesive environment for health care providers. To access the patient experience library of content, log in to the provider training homepage through our provider portal, Availity Essentials™:
If you don’t have access to Availity, you can directly log in to the training website. You can also check out courses on other topics while you’re browsing. If you have questions about the provider training website, email ProviderTraining@bcbsm.com. Best practices to implement We invite all providers to explore our three-part recorded webinar series, “Best Practices for Improving Patient Experience.” These sessions are packed with insights to help your practice consistently deliver exceptional care and optimize patient care and interactions. Free materials are also available upon request and include posters and reminders for patients and staff. In the “Best Practices for Improving Patient Experience” series, you'll gain practical tips and strategies used by doctors’ offices in the following areas:
Medical assistants and other health care professionals can earn continuing education credits with a certificate of completion. Physicians are eligible for continuing medical education credits upon successful completion of these courses and many other patient experience courses. The expanded patient experience content is designed with you in mind, making it easier for practice leaders and staff to access a comprehensive collection of resources. You'll find best practices for streamlining office processes, enhancing patient interactions and boosting professional development — all in one convenient location. We appreciate all you do to enhance the patient experience and are excited to support you in further developing your skills and expertise. For information, email PatientExperience@bcbsm.com. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Online behavioral health care navigation solution to end March 2025As we announced in a Dec. 23, 2024, provider alert, the online behavioral health care navigation solution that Blue Cross Blue Shield of Michigan and Blue Care Network implemented with vendor Quartet will end March 31, 2025. This resource connected Blue Cross and BCN fully insured commercial and Medicare Advantage adult members in Michigan with outpatient behavioral health providers. Blue Cross and BCN have notified behavioral health providers who joined the Quartet online platform about this change. Quartet will provide behavioral health referrals into March 2025. Specifically:
After March, members who need help finding outpatient behavioral health providers can search our online provider directory or call the phone number on the back of their Blue Cross or BCN member ID cards. Use our new online tool to enhance your provider directory listing Blue Cross and BCN offer Enhanced Provider Data, a new online tool available on our provider portal designed to help you strengthen your Blue Cross provider directory listing. If you’re an independent provider not affiliated with a large health system, you can use Enhanced Provider Data to include additional, personalized information to help patients seeking care better understand you and your practice, including:
To access the Enhanced Provider Data tool:
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Quartet is an independent company contracted by Blue Cross Blue Shield of Michigan to connect Blue Cross and BCN members seeking outpatient behavioral health services with the appropriate behavioral health providers. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Billing chart: Blue Cross highlights medical, benefit policy changesYou’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the “Billing chart.” The billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures. We’ll publish information about new Blue Cross groups or changes to group benefits under the Group Benefit Changes heading. For more detailed descriptions of Blue Cross’ policies for these procedures, check under the Commercial Policy tab in Benefit Explainer on Availity®. To access this online information:
2 .Click on Payer Spaces on the Availity menu bar. 3. Click on the BCBSM and BCN logo. 4. Click on Benefit Explainer on the Applications tab. 5. Click on the Commercial Policy tab. 6. Click on Topic. 7. Under Topic Criteria, click on the circle for Unique Identifier and click the drop-down arrow next to Choose Identifier Type, then click on HCPCS Code. 8. Enter the procedure code. 9. Click on Finish. 10. Click on Search. To view the “March 2025 Billing chart,” click here. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Submit reconsideration requests for commercial members through TurningPoint provider portalHealth care providers can now submit requests for the reconsideration of denied prior authorization requests for Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members through the TurningPoint provider portal. You can submit additional clinical documentation, test results and other information for reconsideration. Although you can still fax reconsideration requests, submitting them through the portal will help facilitate a faster response from TurningPoint. Reconsiderations are available only for commercial members. For additional information, see pages 10 and 11 of the TurningPoint Provider Portal User Guide. Note: For Medicare Plus Blue℠ and BCN Advantage℠ members, there isn’t a reconsideration process. However, you can file an appeal. See the document titled Musculoskeletal procedure authorizations: Frequently asked questions for providers for details. For additional information about the TurningPoint Musculoskeletal Surgical Quality & Safey Management program, see the following pages on ereferrals.bcbsm.com:
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Star, HEDIS Measure Tip sheets updated for 2025We’ve updated our series of Star and HEDIS® Measure Tip sheets for 2025 and posted them on our provider portal, Availity Essentials™. These tip sheets have been developed to assist health care providers and their staff in their efforts to improve overall health care quality for their patients and prevent or control diseases and chronic conditions. The new tip sheets are current as of this publication. However, when the National Committee for Quality Assurance, or NCQA, publishes final updates to the 2025 HEDIS specifications, we may need to update the tip sheets again. As updated versions are produced, we’ll post the new ones and announce them in The Record. The tip sheets highlight select measures in the Medicare Star Ratings program. Most of the measures featured in the tip sheets are HEDIS measures. HEDIS is one of the most widely used performance improvement tools in the U.S. Accessing the tip sheets The tip sheets are housed on the Secure Provider Resources section of Availity. You can get there by following these steps:
**Blue Cross Blue Shield of Michigan doesn’t own or control this website. HEDIS®, which stands for Healthcare Effectiveness Data and Information Set, is a registered trademark of the National Committee for Quality Assurance, or NCQA. Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
How to enter subscriber IDs when submitting electronic prior authorization requests for pharmacy benefit drugsWhen submitting electronic prior authorization, or ePA, requests for pharmacy benefit drugs, enter the Blue Cross Blue Shield of Michigan commercial, Medicare Plus Blue℠, Blue Care Network commercial or BCN Advantage℠ subscriber or enrollee ID as follows:
Make sure you have the member’s most recent Blue Cross or BCN ID card as the member information may have changed, including the subscriber or enrollee ID. For the steps required to submit an electronic prior authorization request and more, see the document Save time and submit your prior authorization requests electronically for pharmacy benefit drugs.
Clinical editing updates: Modifier remindersIn support of correct coding and payment accuracy, we are providing the information below to keep you informed about forthcoming payment policy updates, new policies and coding reminders. Blue Cross Blue Shield of Michigan commercial Modifier to procedure code validation reminder Modifiers are used to indicate whether a service or procedure has been altered by some specific circumstance, or to provide more specific information regarding the procedure performed. Most modifiers apply to a specific group of codes and may only be reported with those specified codes. Please remember to use modifiers that are valid and appropriate for the procedure code reported. Claims submitted with procedure codes and modifiers that are inappropriate together may be rejected. Modifier 78 reminder Modifier 78 is used to indicate an unplanned return to the operating room during the postoperative period following surgical procedures. It’s inappropriate to use modifier 78 if there isn’t a return trip to the operating room within the postoperative period. Claims that are inappropriately billed with modifier 78 may be rejected. Modifier 78 description: Unplanned Return to the Operating/Procedure Room by the Same Physician Following Initial Procedure for a Related Procedure During the Postoperative Period.
We’ll no longer require prior authorization for pain management procedures for Medicare Advantage membersIn second-quarter 2025, Blue Cross Blue Shield of Michigan and Blue Care Network will no longer require prior authorization for pain management procedures for Medicare Plus Blue℠ and BCN Advantage℠ members. Any Medicare Advantage members who have active authorizations and receive pain management injections during this transition will continue to receive communications from TurningPoint Healthcare Solutions. As part of our commitment to deliver care in line with standards set by the Centers for Medicare & Medicaid Services, we’ll continue to monitor compliance with these standards through claims review, post-payment audits and strategic collaboration with health care providers who are in shared- and full-risk arrangements. Watch our provider alerts and newsletter articles for additional information. Notes:
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
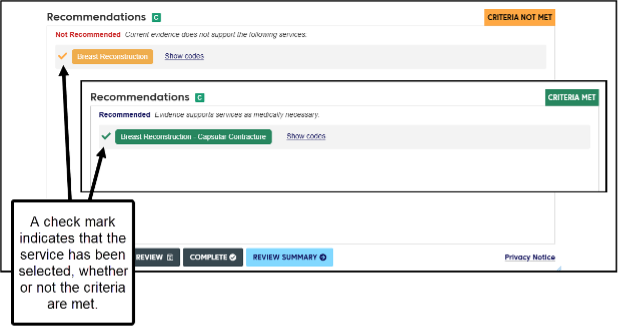
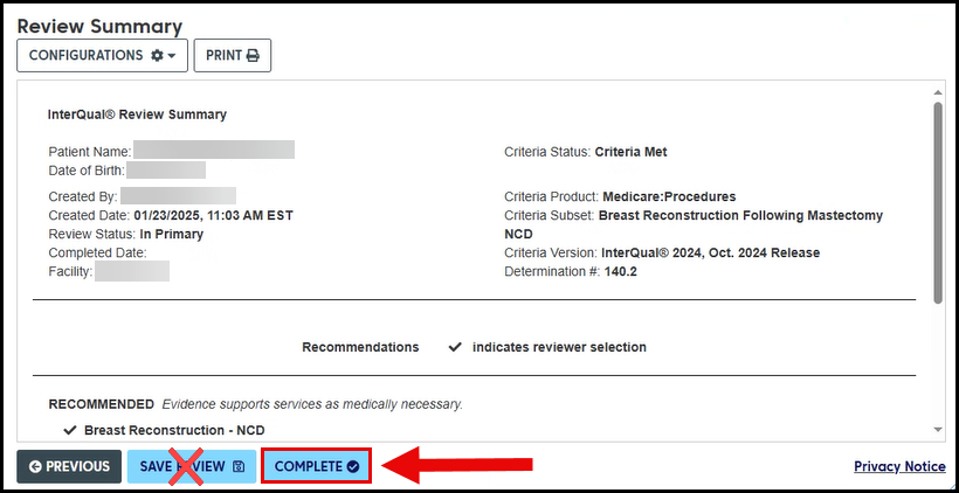
Continue to answer InterQual Connect questions in e-referral system while we investigate technical issuesIn December 2024, we made minor changes to the InterQual® Connect™ process we use to review certain prior authorization requests in the e-referral system for Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members. This change introduced a glitch that causes prior authorization requests to pend for review for certain services, even if the answers provided meet criteria. We’re investigating the issue. In the meantime, continue answering the InterQual Connect questions when they appear, so we can make determinations more quickly. Here’s what to do after answering the questions:
Important: Don’t click SAVE REVIEW. This will cause your request to pend — even if criteria are met — and will delay the processing of your request. Always click COMPLETE to submit the request.
Members can schedule annual physical each calendar yearWhat you need to know Most Blue Cross Blue Shield of Michigan and Blue Care Network members are eligible for an annual physical every calendar year. We’re frequently asked how often members are permitted to have a physical examination. Under the terms of the Affordable Care Act, Blue Cross Blue Shield of Michigan and Blue Care Network commercial members typically qualify for an annual physical. Health care providers scheduling annual physical appointments should remember that our plans allow an annual physical exam every calendar year. That means most members don’t need to wait 366 days for their next physical appointment. As long as the member’s plan is ACA-compliant, you can generally schedule a physical within the calendar year time frame. Because of variations in coverage, it’s always best to check benefits and eligibility for your patients on our provider portal, Availity Essentials™.** Here are some other guidelines to keep in mind:
Medicare Advantage Medicare Plus Blue℠ and BCN Advantage℠ follow guidelines set by the Centers for Medicare & Medicaid Services. More information on the frequency of Medicare screenings is available at cms.gov.** **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
We’re updating our coverage of limb compression devices and accessories, starting April 1Blue Cross Blue Shield of Michigan and Blue Care Network are changing our reimbursement policy for intermittent limb compression devices and accessories. Beginning April 1, 2025, limb compression devices and accessories will no longer be eligible for reimbursement when a durable medical equipment supplier provides them for use in an ambulatory surgical center. Coverage will be limited to devices and accessories delivered to the patient’s home. There’s no change to the requirement for members to meet the clinical criteria in our medical policies. Patients use limb compression devices for venous thromboembolism prophylaxis after they’ve had surgery and are recovering at home. To qualify for coverage of those devices, one of these criteria must be met:
Review these policies to determine if your patient meets the clinical requirements:
You can find these policies using the Medical Policy Router Search.
Reminder for breast MRIs: Patients must meet certain criteria to receive prior authorization approvalBlue Cross Blue Shield of Michigan considers the use of magnetic resonance imaging of the breast to a be a useful diagnostic tool. To receive prior authorization approval for a breast MRI, patients must meet criteria outlined in our Magnetic Resonance Imaging for Breast Cancer medical policy. When the MRI is used as an annual screening tool, patients must have a high risk of breast cancer, as listed in our medical policy criteria. The service is used in addition to mammography. The service isn’t approved as a screening service for individuals at a low to moderate risk for developing breast cancer. Refer to the Magnetic Resonance Imaging for Breast Cancer medical policy for the high-risk considerations. You may sequence the screening encounter ICD-10-CM code in the primary position on the claim, when this service is used as a screening procedure for an individual at heightened risk. However, you must include an ICD-10-CM code representing the qualifying heightened risk within the first four diagnoses sequenced on the claim.
How to obtain CGM products for commercial, Medicare Advantage membersAs we announced in August and December 2024, the methods for obtaining continuous glucose monitor, or CGM, products have changed, as explained in the table below.
To help health care providers navigate this change, we’ve published a new document titled Continuous glucose monitors: Frequently asked questions for prescribing providers. It includes:
There are links to the new FAQ document on the Diabetes Supplies pages and the DME/P&O pages on ereferrals.bcbsm.com. Here are links to earlier provider alerts about this change:
Diclofenac 1% gel prescription formulation discontinuedThe prescription version of diclofenac 1% gel, a nonsteroidal anti-inflammatory drug usually used for temporary relief of arthritis pain and inflammation, has been discontinued. It’s currently listed on Blue Cross Blue Shield of Michigan’s and Blue Care Network’s Medicare Advantage and Part D plan formularies but will be removed March 1, 2025. Pharmacies may still dispense the prescription version if they have it in stock. No additional product will be available for the member to fill once the pharmacy runs out. An over-the-counter version of this pain reliever, Voltaren gel, is available for members to purchase, but it’s not eligible for insurance coverage.
Piasky, Tremfya to have site-of-care requirement for most commercial members, starting June 1For dates of service on or after June 1, 2025, we’re adding a site-of-care requirement for most Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members for the following drugs covered under medical benefits:
When you submit prior authorization requests for these drugs, you’ll be prompted to select a site of care. If the request meets the clinical criteria for the drug and is for one of the following sites of care, it will be approved automatically:
Additional information or documentation may be required for requests to administer Piasky or Tremfya in an outpatient hospital setting. Please remember, these drugs already require prior authorization. The new site-of-care requirement is in addition to the current prior authorization requirement. Members who start courses of treatment with Piasky or Tremfya before June 1, 2025, will be able to continue receiving these drugs in their current locations until their existing authorizations expire. If these members then continue treatment under new prior authorizations, the site-of-care requirement outlined above will apply. Some Blue Cross commercial groups aren’t subject to these requirements Prior authorization and site-of-care requirements apply only to Blue Cross commercial groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under medical benefits. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. While UAW Retiree Medical Benefits Trust non-Medicare members don’t participate in the standard prior authorization program, these requirements apply to them. Note: These requirements don’t apply to Blue Cross and Blue Shield Federal Employee Program® members. Lists of requirements For more information about requirements related to drugs covered under medical benefits, see these lists:
We’ll update these lists before the effective date. You can access these lists and other information about requesting prior authorization at ereferrals.bcbsm.com, at these locations: Prior authorization isn't a guarantee of payment. Health care providers need to verify eligibility and benefits for members.
We’re changing how we manage Stelara, Stelara biosimilar therapies for most commercial members, starting April 1, May 1Yesintek™ (ustekinumab-kfce) will be the preferred ustekinumab product for most Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members, as follows:
Members on a plan using the Preferred Drug List are excluded from this change. This change doesn’t apply to Medicare Advantage groups or members. In addition, for dates of service on or after May 1, 2025, the subcutaneous, or SC, formulations of ustekinumab will no longer be payable under the member’s medical benefit. Members who continue to receive SC ustekinumab administered by a health care provider (billed under medical benefits) on or after May 1 may be responsible for the full cost. How this will affect members under pharmacy benefits Authorizations for Stelara SC, brand ustekinumab, will remain in effect until March 31, 2025. New authorizations for Yesintek SC will be approved April 1, 2025, and active through March 31, 2026, so members can continue therapy without interruption. If members decide to use Stelara SC on or after April 1, they’ll be responsible for the full cost. Filling the prescription We’ll only pay for Yesintek SC when filled through Walgreens Specialty Pharmacy, an independent company that provides specialty pharmacy services to Blue Cross and BCN. Members who are currently filling Stelara SC prescriptions at the Michigan Medicine Specialty Pharmacy may continue filling Yesintek SC there. If members are currently filling Stelara SC through Walgreens:
If members are currently filling their prescriptions through a pharmacy other than those mentioned above:
Prescribers can send a new prescription for Yesintek SC by one of the following methods:
How this will affect members under medical benefits The nonpreferred ustekinumab products are Imuldosa™, Otulfi™, Pyzchiva®, Selarsdi™, Stelara®, Steqeyma® and Wezlana™. Members who have active authorizations for the IV formulation of Yesintek won’t be affected by this change. Members who have active authorizations for a nonpreferred ustekinumab product or SC ustekinumab product are authorized to continue their current therapy under medical benefits through April 30, 2025. We’re issuing authorizations for Yesintek SC under pharmacy benefits from May 1, 2025, to April 30, 2026, to avoid any interruptions in care.
To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. How to submit prior authorization requests For a self-administered ustekinumab SC product (covered under pharmacy benefits), submit the request using an electronic prior authorization, or ePA, tool such as CoverMyMeds® or Surescripts®. For an ustekinumab IV product that requires administration by a health care provider (covered under medical benefits), submit the request through the NovoLogix® online tool. NovoLogix® is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network. Walgreens Specialty Pharmacy is an independent company that provides specialty pharmacy services covered under the pharmacy benefit for various Blue Cross Blue Shield of Michigan and Blue Care Network members with commercial plans.
New Acute inpatient hospital assessment form for commercial, Medicare Advantage membersOn Jan. 28, 2025, we published a new Acute inpatient hospital assessment form. Use this form for Blue Cross Blue Shield of Michigan commercial, Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members. Both Michigan and non-Michigan health care providers must now use the Acute inpatient hospital assessment form for acute inpatient medical and surgical admission requests for all members. Follow the instructions on the form. The new form replaces the separate commercial and Medicare Advantage forms you’ve previously used.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Live Q&A, on-demand training opportunities availableAction item Visit our provider training site to register for a March Q&A session and find resources on topics that are important to your role. Provider Experience continues to offer training resources for health care providers and staff. On-demand courses are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network. The following learning opportunities are available: Live Q&A session about prior authorization of post-acute care services for Medicare Advantage members: This session is for providers who have questions about processing requests for prior authorization of post-acute care services for Medicare Plus Blue℠ and BCN Advantage℠ members through the e-referral system. Blue Cross and BCN took over managing prior authorizations for these services starting with dates of service on and after Oct. 1, 2024, as we detailed in an October 2024 Record article. The session is from noon to 12:45 p.m. March 20, 2025. Registration is now open. Medicare Advantage post-acute care mini modules: We also have two mini modules for post-acute care facilities about using e-referral. These modules blend the process and system steps in a flow that shows you exactly what to do. Each only takes a few minutes to complete:
Benefit Explainer overview: Providers use the Benefit Explainer tool to check on member-specific and general benefit details, coverage and limitations. Provider Training has revamped the course to create an interactive walk-through to show the navigation and functionalities of Benefit Explainer. The new e-learning course gives essential information, including various ways to reach Benefit Explainer and how to use each of the tabs within the tool. How to access provider training To access the training site, follow these steps:
Those who don’t have a provider portal account can directly access the training through the Provider training website. Questions? For more information about using the provider training website, contact the provider training team at ProviderTraining@bcbsm.com. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Register now for 2025 virtual provider symposium sessionsThis year’s virtual health care provider symposiums start in May. They’ll focus on quality measures and review of evaluation and management guidelines. Registration is now open on the provider training website. Physicians, physician assistants, nurse practitioners, nurses and coders can receive continuing education credits for attending. Once you’re logged in to the provider training site, open the event calendar to sign up for any of the sessions listed below. All times are Eastern time. All Star Performance-HEDIS®/Star Rating Measure Overview: The Golden Star Awards For physicians and office staff responsible for closing gaps in care related to quality measures for adults
Conducting an Internal Chart Audit: Livestreaming with April For physicians, coders, billers and administrative staff
How to register on the provider training website Provider portal users with an Availity Essentials™ account can access the provider training website:
You can also directly access the training website if you don’t have a provider portal account. Questions?
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. HEDIS® is a registered trademark of the National Committee for Quality Assurance. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. Accreditation statement: This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of the Minnesota Medical Association and Blue Cross Blue Shield of Michigan. The Minnesota Medical Association (MMA) is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. CME statement: The Minnesota Medical Association designates this internet live activity for a maximum of 2 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Join monthly webinars for physicians, coders focused on documentation, codingIn 2025, we’ll continue to offer webinars on documentation and coding of common challenging diagnoses. These live, lunchtime educational sessions will also include an opportunity to ask questions. Below is our schedule and topics for the sessions. All sessions start at noon Eastern time and should last for 30 minutes. Register for the sessions on the provider training website.
Provider training website access If you have an Availity Essentials™ account can access the provider training website this way:
Existing users who used the same email address as their provider portal profile email will be directed to the training site. If you used a different email address, contact ProviderTraining@bcbsm.com to update your profile. You can also directly access the training website if you don’t have a provider portal account by clicking here. After logging in to the provider training website, look in Event Calendar to sign up for your desired session. You can also quickly search for all the sessions with the keyword “lunchtime” and then look under the results for Events. Questions?
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Reminder: Select 1 PO with affiliated medical care group to support all Blue Cross, BCN businessBefore Jan. 1, 2026, each primary care provider must align with one physician organization and that PO’s affiliated medical care group. It’s important for primary care providers to receive support for all Blue Cross Blue Shield of Michigan and Blue Care Network lines of business in which they choose to participate. This includes our commercial and Medicare Advantage plans. We first told you about this in the July 2024 Record. Primary care providers who haven’t yet aligned their PO and medical care group affiliations are urged to do so now. Any changes must occur before Jan. 1, 2026. Once you align your PO and medical care group affiliations, you’ll benefit from reduced administrative work and have more time for patient care. What primary care providers need to do Review the list of POs and their corresponding medical care groups.
Notes:
For more information Here’s where you can learn more:
Reminder: Chiropractors invited to join new quality reward programAction item To reap the benefits of the new quality reward program, chiropractors need to opt in by June 30, 2025. For details, visit the chiropractic quality rewards website. As we told you about in the January issue of The Record, Blue Cross Blue Shield of Michigan is offering all participating chiropractors the chance to join our new low back pain quality reward program. As part of the program, engaged chiropractors have an opportunity to earn a value-based reimbursement of 5% on eligible PPO professional claims for the pay period of Sept. 1, 2026, through Aug. 31, 2027. But you need to sign up prior to June 30, 2025, to be eligible. For more information about the program, see the January issue of The Record and the chiropractic quality rewards website.
Questionnaire changes in e-referral systemOn Dec. 22, 2024, and Feb. 2, 2025, we updated and deleted questionnaires in the e-referral system. We’ve updated the Authorization criteria and preview questionnaires document on the ereferrals.bcbsm.com website to reflect these changes. Please remember, we use our authorization criteria, our medical policies and your answers to the questionnaires in the e-referral system when making utilization management determinations on your prior authorization requests. What changed Dec. 22, 2024 We updated the following questionnaires in the e-referral system.
We removed the following questionnaires from the e-referral system. Note: The listed procedure codes continue to require prior authorization.
What changed Feb. 2, 2025 We made the following changes for the lines of business listed in the second column of the table.
Preview questionnaires Preview questionnaires show the questions you’ll need to answer in the e-referral system, so you can prepare your answers ahead of time. To find the preview questionnaires, see the document titled Authorization criteria and preview questionnaires. You can access this document by going to ereferrals.bcbsm.com and doing the following:
Authorization criteria and medical policies The Authorization criteria and preview questionnaires document explains how to access the pertinent authorization criteria and medical policies.
Article correction: Providers can upload medical records through Availity Essentials for additional types of requestsIn the January 2025 Record, we published an article with incorrect information. For Medicare Plus Blue℠ claims, the expanded ability to upload medical records through Availity Essentials™ is available for claims with 14-digit claim numbers (not 16). We’ve updated the article below with the correct information. On Dec. 16, 2024, Blue Cross Blue Shield of Michigan further expanded the ability to upload medical records through our provider portal, Availity Essentials™. Specifically, health care providers can upload medical records for Blue Cross commercial and Medicare Plus Blue℠ members for these reasons:**
How to upload medical records Providers can submit medical records using the Send Attachments feature, which is available on the Claim Status screen in Availity Essentials. For step-by-step instructions, see the Submitting medical records through Availity Essentials document. Notes:
Availity Essentials recorded training webinar Availity® is offering a recorded webinar where you can learn about the latest changes. You can view Availity’s Learn How to Submit Claim Attachments for BCBSM Providers recorded training for information about the new functionality. To access the recorded webinar:
Additional information
**For Medicare Plus Blue, this functionality is available for claims with 14-digit claim numbers. ***Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Conservative care for acute low back pain, acute bronchitisThis is part of an ongoing series of articles focusing on the tools and resources available to help FEP® members manage their health. Blue Cross Blue Shield of Michigan has developed helpful HEDIS® Measure Tip sheets for health care providers on Use of Imaging Studies for Low Back Pain and Avoidance of Antibiotic Treatment for Acute Bronchitis/Bronchiolitis. Low back pain Since acute low back pain typically resolves in four to six weeks and imaging such as X-rays, CT scans and MRIs aren’t recommended, treatment focuses on symptom management for the pain. The HEDIS Measure Tip sheet on acute low back pain aims to help providers reduce the use of imaging and provides helpful suggestions for treatment. Additionally, Blue Cross is offering all participating chiropractors the opportunity to join a new quality reward program related to imaging of low back pain. For more information, see the January Record. Acute bronchitis Typically, it isn’t recommended to use antibiotics to treat patients who have acute bronchitis. Blue Cross’ HEDIS Measure Tip sheet has helpful suggestions to avoid the use of antibiotics for acute bronchitis. The Improving Antibiotic Use** flyer from the Centers for Disease Control and Prevention can help patients understand why antibiotics aren’t used, common side effects and ways to feel better. FEP contact information If providers have questions about Blue Cross and Blue Shield Federal Employee Program® support services and benefits, call Customer Service at 1-800-482-3600 for Federal Employee Health Benefits information or 1-877-760-8574 for Postal Service Health Benefits information, or go to fepblue.org. ***Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. HEDIS®, which stands for Healthcare Effectiveness Data and Information Set, is a registered trademark of the National Committee for Quality Assurance or NCQA.
External Review Reimbursement Policy implemented March 1Based on Blue Cross Blue Shield of Michigan’s review of the External Review Reimbursement Policy responses, the policy will be implemented March 1, 2025, for Blue Cross commercial acute care hospitals. Please remember, these are second level medical necessity reviews. If all the information is provided in the first level review or during the peer-to-peer discussion, there is less chance a second level external review will be needed. If the second level review is requested and the denial is upheld, then the cost to the hospital for the appeal is $205 for a non-urgent, non-complicated review. There are no attorney fees associated with this policy. The Contract Administration Process for the External Review Reimbursement Policy ended with the presentations at the Dec. 11, 2024, Staff Liaison meeting and at the Jan. 30, 2025, PHA Advisory Committee.
Multiple Therapies Reimbursement Policy will be implemented April 1Based on Blue Cross Blue Shield of Michigan’s review of the Multiple Therapies Reimbursement Policy responses, the policy will be implemented April 1, 2025, for professional providers and facilities. Please remember, the reduction in the policy only comes on the practice expense portion of therapy services that are the secondary or subsequent procedures provided on a single date of service by the same group physician or other qualified health care professional. This policy does not apply to therapy services rendered with a behavioral health diagnosis. The Contract Administration Process for the policy ended with presentation at the Dec. 11, 2024, Staff Liaison meeting and at the Jan. 30, 2025, PHA Advisory Committee.
Submit reconsideration requests for commercial members through TurningPoint provider portalHealth care providers can now submit requests for the reconsideration of denied prior authorization requests for Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members through the TurningPoint provider portal. You can submit additional clinical documentation, test results and other information for reconsideration. Although you can still fax reconsideration requests, submitting them through the portal will help facilitate a faster response from TurningPoint. Reconsiderations are available only for commercial members. For additional information, see pages 10 and 11 of the TurningPoint Provider Portal User Guide. Note: For Medicare Plus Blue℠ and BCN Advantage℠ members, there isn’t a reconsideration process. However, you can file an appeal. See the document titled Musculoskeletal procedure authorizations: Frequently asked questions for providers for details. For additional information about the TurningPoint Musculoskeletal Surgical Quality & Safey Management program, see the following pages on ereferrals.bcbsm.com:
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
How to enter subscriber IDs when submitting electronic prior authorization requests for pharmacy benefit drugsWhen submitting electronic prior authorization, or ePA, requests for pharmacy benefit drugs, enter the Blue Cross Blue Shield of Michigan commercial, Medicare Plus Blue℠, Blue Care Network commercial or BCN Advantage℠ subscriber or enrollee ID as follows:
Make sure you have the member’s most recent Blue Cross or BCN ID card as the member information may have changed, including the subscriber or enrollee ID. For the steps required to submit an electronic prior authorization request and more, see the document Save time and submit your prior authorization requests electronically for pharmacy benefit drugs.
Clinical editing updates: Modifier remindersIn support of correct coding and payment accuracy, we are providing the information below to keep you informed about forthcoming payment policy updates, new policies and coding reminders. Blue Cross Blue Shield of Michigan commercial Modifier to procedure code validation reminder Modifiers are used to indicate whether a service or procedure has been altered by some specific circumstance, or to provide more specific information regarding the procedure performed. Most modifiers apply to a specific group of codes and may only be reported with those specified codes. Please remember to use modifiers that are valid and appropriate for the procedure code reported. Claims submitted with procedure codes and modifiers that are inappropriate together may be rejected. Modifier 78 reminder Modifier 78 is used to indicate an unplanned return to the operating room during the postoperative period following surgical procedures. It’s inappropriate to use modifier 78 if there isn’t a return trip to the operating room within the postoperative period. Claims that are inappropriately billed with modifier 78 may be rejected. Modifier 78 description: Unplanned Return to the Operating/Procedure Room by the Same Physician Following Initial Procedure for a Related Procedure During the Postoperative Period.
We’ll no longer require prior authorization for pain management procedures for Medicare Advantage membersIn second-quarter 2025, Blue Cross Blue Shield of Michigan and Blue Care Network will no longer require prior authorization for pain management procedures for Medicare Plus Blue℠ and BCN Advantage℠ members. Any Medicare Advantage members who have active authorizations and receive pain management injections during this transition will continue to receive communications from TurningPoint Healthcare Solutions. As part of our commitment to deliver care in line with standards set by the Centers for Medicare & Medicaid Services, we’ll continue to monitor compliance with these standards through claims review, post-payment audits and strategic collaboration with health care providers who are in shared- and full-risk arrangements. Watch our provider alerts and newsletter articles for additional information. Notes:
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
How to obtain CGM products for commercial, Medicare Advantage membersAs we announced in August and December 2024, the methods for obtaining continuous glucose monitor, or CGM, products have changed, as explained in the table below.
To help health care providers navigate this change, we’ve published a new document titled Continuous glucose monitors: Frequently asked questions for prescribing providers. It includes:
There are links to the new FAQ document on the Diabetes Supplies pages and the DME/P&O pages on ereferrals.bcbsm.com. Here are links to earlier provider alerts about this change:
Diclofenac 1% gel prescription formulation discontinuedThe prescription version of diclofenac 1% gel, a nonsteroidal anti-inflammatory drug usually used for temporary relief of arthritis pain and inflammation, has been discontinued. It’s currently listed on Blue Cross Blue Shield of Michigan’s and Blue Care Network’s Medicare Advantage and Part D plan formularies but will be removed March 1, 2025. Pharmacies may still dispense the prescription version if they have it in stock. No additional product will be available for the member to fill once the pharmacy runs out. An over-the-counter version of this pain reliever, Voltaren gel, is available for members to purchase, but it’s not eligible for insurance coverage.
Piasky, Tremfya to have site-of-care requirement for most commercial members, starting June 1For dates of service on or after June 1, 2025, we’re adding a site-of-care requirement for most Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members for the following drugs covered under medical benefits:
When you submit prior authorization requests for these drugs, you’ll be prompted to select a site of care. If the request meets the clinical criteria for the drug and is for one of the following sites of care, it will be approved automatically:
Additional information or documentation may be required for requests to administer Piasky or Tremfya in an outpatient hospital setting. Please remember, these drugs already require prior authorization. The new site-of-care requirement is in addition to the current prior authorization requirement. Members who start courses of treatment with Piasky or Tremfya before June 1, 2025, will be able to continue receiving these drugs in their current locations until their existing authorizations expire. If these members then continue treatment under new prior authorizations, the site-of-care requirement outlined above will apply. Some Blue Cross commercial groups aren’t subject to these requirements Prior authorization and site-of-care requirements apply only to Blue Cross commercial groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under medical benefits. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. While UAW Retiree Medical Benefits Trust non-Medicare members don’t participate in the standard prior authorization program, these requirements apply to them. Note: These requirements don’t apply to Blue Cross and Blue Shield Federal Employee Program® members. Lists of requirements For more information about requirements related to drugs covered under medical benefits, see these lists:
We’ll update these lists before the effective date. You can access these lists and other information about requesting prior authorization at ereferrals.bcbsm.com, at these locations: Prior authorization isn't a guarantee of payment. Health care providers need to verify eligibility and benefits for members.
We’re changing how we manage Stelara, Stelara biosimilar therapies for most commercial members, starting April 1, May 1Yesintek™ (ustekinumab-kfce) will be the preferred ustekinumab product for most Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members, as follows:
Members on a plan using the Preferred Drug List are excluded from this change. This change doesn’t apply to Medicare Advantage groups or members. In addition, for dates of service on or after May 1, 2025, the subcutaneous, or SC, formulations of ustekinumab will no longer be payable under the member’s medical benefit. Members who continue to receive SC ustekinumab administered by a health care provider (billed under medical benefits) on or after May 1 may be responsible for the full cost. How this will affect members under pharmacy benefits Authorizations for Stelara SC, brand ustekinumab, will remain in effect until March 31, 2025. New authorizations for Yesintek SC will be approved April 1, 2025, and active through March 31, 2026, so members can continue therapy without interruption. If members decide to use Stelara SC on or after April 1, they’ll be responsible for the full cost. Filling the prescription We’ll only pay for Yesintek SC when filled through Walgreens Specialty Pharmacy, an independent company that provides specialty pharmacy services to Blue Cross and BCN. Members who are currently filling Stelara SC prescriptions at the Michigan Medicine Specialty Pharmacy may continue filling Yesintek SC there. If members are currently filling Stelara SC through Walgreens:
If members are currently filling their prescriptions through a pharmacy other than those mentioned above:
Prescribers can send a new prescription for Yesintek SC by one of the following methods:
How this will affect members under medical benefits The nonpreferred ustekinumab products are Imuldosa™, Otulfi™, Pyzchiva®, Selarsdi™, Stelara®, Steqeyma® and Wezlana™. Members who have active authorizations for the IV formulation of Yesintek won’t be affected by this change. Members who have active authorizations for a nonpreferred ustekinumab product or SC ustekinumab product are authorized to continue their current therapy under medical benefits through April 30, 2025. We’re issuing authorizations for Yesintek SC under pharmacy benefits from May 1, 2025, to April 30, 2026, to avoid any interruptions in care.
To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. How to submit prior authorization requests For a self-administered ustekinumab SC product (covered under pharmacy benefits), submit the request using an electronic prior authorization, or ePA, tool such as CoverMyMeds® or Surescripts®. For an ustekinumab IV product that requires administration by a health care provider (covered under medical benefits), submit the request through the NovoLogix® online tool. NovoLogix® is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network. Walgreens Specialty Pharmacy is an independent company that provides specialty pharmacy services covered under the pharmacy benefit for various Blue Cross Blue Shield of Michigan and Blue Care Network members with commercial plans.
New Acute inpatient hospital assessment form for commercial, Medicare Advantage membersOn Jan. 28, 2025, we published a new Acute inpatient hospital assessment form. Use this form for Blue Cross Blue Shield of Michigan commercial, Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members. Both Michigan and non-Michigan health care providers must now use the Acute inpatient hospital assessment form for acute inpatient medical and surgical admission requests for all members. Follow the instructions on the form. The new form replaces the separate commercial and Medicare Advantage forms you’ve previously used.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Questionnaire changes in e-referral systemOn Dec. 22, 2024, and Feb. 2, 2025, we updated and deleted questionnaires in the e-referral system. We’ve updated the Authorization criteria and preview questionnaires document on the ereferrals.bcbsm.com website to reflect these changes. Please remember, we use our authorization criteria, our medical policies and your answers to the questionnaires in the e-referral system when making utilization management determinations on your prior authorization requests. What changed Dec. 22, 2024 We updated the following questionnaires in the e-referral system.
We removed the following questionnaires from the e-referral system. Note: The listed procedure codes continue to require prior authorization.
What changed Feb. 2, 2025 We made the following changes for the lines of business listed in the second column of the table.
Preview questionnaires Preview questionnaires show the questions you’ll need to answer in the e-referral system, so you can prepare your answers ahead of time. To find the preview questionnaires, see the document titled Authorization criteria and preview questionnaires. You can access this document by going to ereferrals.bcbsm.com and doing the following:
Authorization criteria and medical policies The Authorization criteria and preview questionnaires document explains how to access the pertinent authorization criteria and medical policies.
Article correction: Providers can upload medical records through Availity Essentials for additional types of requestsIn the January 2025 Record, we published an article with incorrect information. For Medicare Plus Blue℠ claims, the expanded ability to upload medical records through Availity Essentials™ is available for claims with 14-digit claim numbers (not 16). We’ve updated the article below with the correct information. On Dec. 16, 2024, Blue Cross Blue Shield of Michigan further expanded the ability to upload medical records through our provider portal, Availity Essentials™. Specifically, health care providers can upload medical records for Blue Cross commercial and Medicare Plus Blue℠ members for these reasons:**
How to upload medical records Providers can submit medical records using the Send Attachments feature, which is available on the Claim Status screen in Availity Essentials. For step-by-step instructions, see the Submitting medical records through Availity Essentials document. Notes:
Availity Essentials recorded training webinar Availity® is offering a recorded webinar where you can learn about the latest changes. You can view Availity’s Learn How to Submit Claim Attachments for BCBSM Providers recorded training for information about the new functionality. To access the recorded webinar:
Additional information
**For Medicare Plus Blue, this functionality is available for claims with 14-digit claim numbers. ***Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
We’re updating our coverage of limb compression devices and accessories, starting April 1Blue Cross Blue Shield of Michigan and Blue Care Network are changing our reimbursement policy for intermittent limb compression devices and accessories. Beginning April 1, 2025, limb compression devices and accessories will no longer be eligible for reimbursement when a durable medical equipment supplier provides them for use in an ambulatory surgical center. Coverage will be limited to devices and accessories delivered to the patient’s home. There’s no change to the requirement for members to meet the clinical criteria in our medical policies. Patients use limb compression devices for venous thromboembolism prophylaxis after they’ve had surgery and are recovering at home. To qualify for coverage of those devices, one of these criteria must be met:
Review these policies to determine if your patient meets the clinical requirements:
You can find these policies using the Medical Policy Router Search.
Reminder for breast MRIs: Patients must meet certain criteria to receive prior authorization approvalBlue Cross Blue Shield of Michigan considers the use of magnetic resonance imaging of the breast to a be a useful diagnostic tool. To receive prior authorization approval for a breast MRI, patients must meet criteria outlined in our Magnetic Resonance Imaging for Breast Cancer medical policy. When the MRI is used as an annual screening tool, patients must have a high risk of breast cancer, as listed in our medical policy criteria. The service is used in addition to mammography. The service isn’t approved as a screening service for individuals at a low to moderate risk for developing breast cancer. Refer to the Magnetic Resonance Imaging for Breast Cancer medical policy for the high-risk considerations. You may sequence the screening encounter ICD-10-CM code in the primary position on the claim, when this service is used as a screening procedure for an individual at heightened risk. However, you must include an ICD-10-CM code representing the qualifying heightened risk within the first four diagnoses sequenced on the claim. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|