Subscribe | The Record Archive | Contacts | bcbsm.com
|
July 2025
Let’s work together to address health care affordabilityHealth care costs in Michigan and across the U.S. are rising to unaffordable levels, straining the budgets of the patients and customers we all serve. Affordability is a major concern that touches all of us. The health care affordability crisis isn’t one that any individual company or health care provider can resolve on its own. Solving the problem requires partnerships to deliver systemwide solutions. Insurers, physicians, hospital leaders, government regulators, pharmaceutical companies and others can all play a role in improving the U.S. health care system. We need to work together for the benefit of our shared patients and customers. At Blue Cross Blue Shield of Michigan, we stand for partnering with those who share our commitment to affordability, ensuring that we all can have access to affordable health care. In Michigan, we have a long history of successful partnership that has improved the quality of health care for us all and has inspired similar efforts in other states and countries. We’ve been proud to develop programs, fund care improvement efforts and lead discussions with physicians and hospital leaders across the state. The Blue Cross Value Partnerships programs just celebrated 20 years of collaborative work that improved the quality of health care in Michigan and avoided $6.3 billion in costs. More than 20,000 physicians and 100 hospitals are working with us in patient-centered medical home programs, Collaborative Quality Initiatives focused on specific hospital procedures, and Blueprint for Affordability contracts that share financial responsibility for patient outcomes. Now, Blue Cross is starting a public conversation about health care affordability and encouraging more change to improve the system for everyone. We’ll talk about the issues on our new online affordability hub at MIBlueDaily.com/affordability and through our social media channels, newsletters and in media interviews. Our core principles in this effort include:
We encourage you to visit our affordability hub often for updated information about this important issue that we’re committed to addressing. Let’s work together to solve the health care affordability problem.
Review these tips on how to properly document autism and other neurodevelopmental disordersAction item Use the information provided here as a quick reference on how to correctly and accurately document autism and other neurodevelopmental disorders. Health care providers’ accurate documentation of autism and other neurodevelopmental disorders is essential for optimal care coordination and risk adjustment accuracy. Clear documentation improves coding completeness, supports appropriate reimbursement and reflects patient complexity. Below are important information and instructions, which providers can find in the 2025 Risk Adjustment Coding Guidance, to keep in mind when documenting these conditions. Note: None of the information included here is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations. Key documentation elements
Common pitfalls when documenting these elements include:
Here’s an example of how correct documentation should look: Patient with autism spectrum disorder, with significant difficulty in social communication, limited eye contact and repetitive speech. Requires substantial support at school. Diagnosis is supported by developmental history and clinical evaluation. Medications Review and identify medications in each patient encounter. For example, Risperdal® is commonly used to treat schizophrenia and bipolar disorder. Providers are required to document this medication when prescribing it to treat autism. See a couple of examples on how to document medications identified during a patient encounter:
Conditions All associated medical conditions, such as epilepsy and developmental disability, must be reviewed in the patient encounter. Here’s an example: A child with a diagnosis of autism. The patient’s progress note also mentions having a language deficit. The correct code selection is F84.0, with a secondary code of R48.8 because of the underlying medical diagnosis contributing to the language problems. When medical etiology is not documented, only F80.2 should be assigned. It’s equally important to evaluate all conditions mentioned in the patient encounter, including other impairment or behavior issues that could affect the current patient encounter and treatment. For example: An encounter for an autistic child with an upper-respiratory infection. In the History of Present Illness, the provider refers to the patient as autistic but doesn’t assess the condition by itself or how it affects the treatment for the upper-respiratory infection. A review of past medical history is important for overall patient care. Chronic conditions that are actively being treated should be assessed for diagnosis closure submissions or to support a higher specificity ICD-10 code for autistic spectrum disorder or pervasive developmental disorder. To recap, providers must address all conditions in the patient encounter and thoroughly document them in the medical record to help ensure coding accuracy and high-quality care. Quick documentation checklist
Billing chart: Blue Cross highlights medical, benefit policy changesYou’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the “Billing chart.” The billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures. We’ll publish information about new Blue Cross groups or changes to group benefits under the Group Benefit Changes heading. For more detailed descriptions of Blue Cross’ policies for these procedures, check under the Commercial Policy tab in Benefit Explainer on Availity Essentials™. To access this online information:
To view the “July 2025 Billing chart,” click here. **Blue Cross Blue Shield of Michigan doesn’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
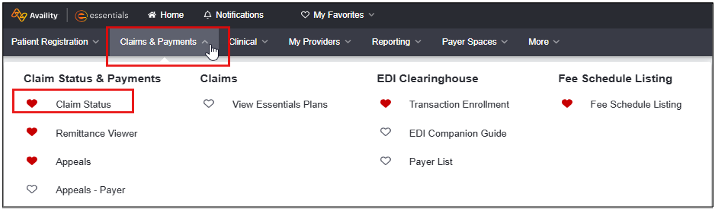
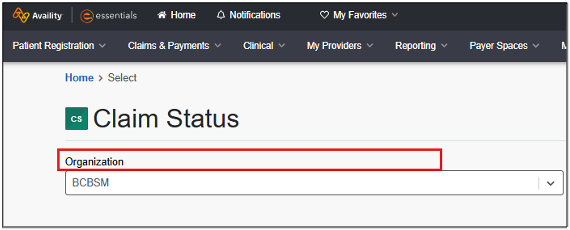
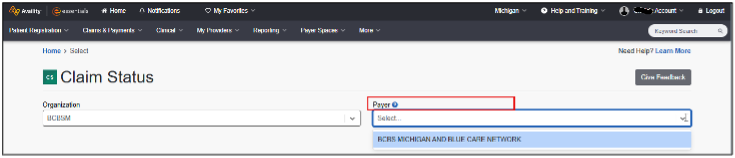
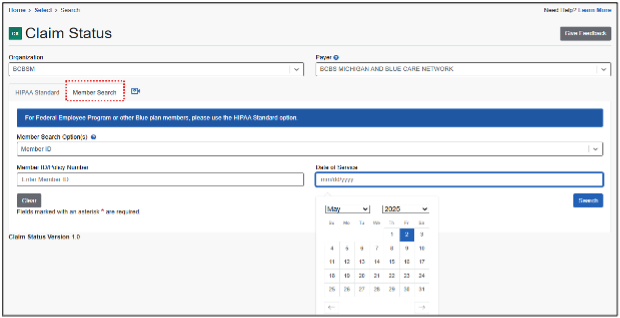
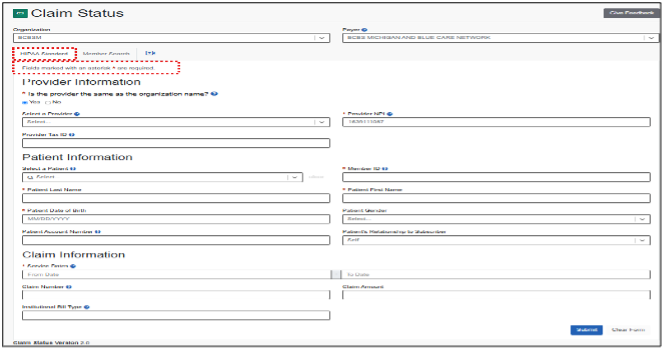
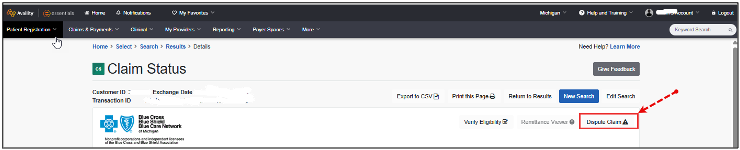
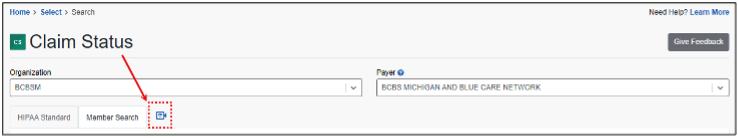
Provider portal pointersThis is an article ongoing series of tips and tricks designed to help you do your job more efficiently by getting the most out of the applications and tools available on our provider portal. Claims status inquiry process The claims status inquiry process is designed to streamline access to insurance claim statuses, identify issues and dispute claims, when necessary. Note: To conduct a claims status inquiry, administrators must first assign the user the Claims Status role using Manage My Team(s), as previously discussed on Page 9 of the May-June issue of BCN Provider News. Without this role, users will be unable to access the claims status inquiry tool within the portal. The steps to conduct a claims status inquiry are as follows:
If the user is tied to only one organization, it will be selected automatically. Those with access to multiple organizations will see all options displayed alphabetically.
Hint: In cases where a patient appears multiple times due to coverage types or group changes, select the correct record carefully.
Hint: For best search results, only enter data for required fields marked with an asterisk.
Note: Appeals are based on EX codes, which differ for each line of business. To access EX code lists for each line of business:
Additional help is available A short video demonstrating the claims status process is also available. To view the video, click the camera icon on the Claim Status page.
Help us help you If you have a suggestion for a provider portal topic you would like to see in future issues of The Record or BCN Provider News, contact us at bcnprovidernews@bcbsm.com. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
2025 CPT Category III update: New, deleted codesThe American Medical Association has added 40 new Category III codes as part of its CPT update. The codes, effective dates and Blue Cross Blue Shield of Michigan’s coverage decisions for commercial PPO members are below. Surgery Male genital system/prostate
Surgery/auditory system
Surgery/nervous system
Pathology and laboratory/surgical pathology
Medicine
Medicine/cardiovascular
Surgery/digestive system
Surgery/cardiovascular
Surgery/therapeutic services
Surgery/integumentary
Other medical services
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Talk with patients now about Health Outcomes Survey topicsWhy is the Health Outcomes Survey, or HOS, important? The goal of the HOS is to gather clinically meaningful health status data from Medicare Advantage patients to support quality improvement activities, monitor health plan performance and improve the health of this patient population. Health care providers can significantly affect how patients assess their health care experience in response to HOS questions through discussions at your annual wellness visits. Five HOS topics are included in Star Ratings Questions relative to physical activity, improving bladder control and reducing the risk of falls are asked annually. The following are examples of questions included in these categories:
To assist patients who receive the survey, and to reinforce the discussions you’ve had with them, here are some ideas for addressing these topics:
It’s important to note that many of the HOS questions ask patients whether their provider discussed these concerns with them. For this reason, we suggest that these topics become part of each patient’s annual wellness visit. Need more information related to HOS? On our provider training site, we have several webinars on the Health Outcomes Survey, including an overview as part of the 2025 series of mini modules on CMS Star measures. To access the training site, follow these steps:
Existing users who used the same email address as their provider portal profile email will be directed to the training site. If you used a different email address, contact ProviderTraining@bcbsm.com to update your profile. Use the keyword “HOS” once on the training site. If you’re a new training site user, complete the one-time registration by entering your role and creating a password. This allows you to access the training site outside of the provider portal if needed. You can also check out our Health Outcomes Survey (HOS) tip sheet. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
How to protect yourself from NPI-related fraudYour national provider identifier, or NPI, is a unique number assigned to you as a health care provider to process claims and conduct other administrative tasks. But, because these identifiers are publicly available, they’re at risk of being used in fraudulent schemes. Bad actors can obtain these NPIs from online directories or other public sources and use them to submit false claims or commit other types of health care fraud. This can lead to financial losses, damage to the provider's reputation and legal consequences. It's essential for providers to be aware of this risk and take steps to monitor their claims and billing statements for any suspicious activity. To protect yourself from NPI-related fraud, it's crucial to be vigilant and proactive.
By taking these steps, you can help protect your practice and prevent financial losses due to NPI theft. And reporting any suspicious activity can help prevent further harm to your practice and reputation. Our organization recently encountered a real-life example of NPI theft. We received an influx of durable medical equipment claims with rendering provider NPIs. Many of the providers contacted during the verification process said they had no knowledge of the patients related to those claims and suspected their NPIs had been used without their consent. If we had not reached out to the providers, they may have remained unaware that their NPIs were being used for fraudulent activity. This highlights the importance of vigilance and proactive monitoring to detect and prevent NPI theft. By working together, we can help prevent these types of scams and protect the integrity of the health care system. If you suspect that your NPI has been compromised, report it to CMS and take steps to protect your practice and reputation. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Do you have time for a Quality Minute about medication adherence?This is another article in an ongoing series of quick tips designed to be read in 60 seconds or less and provide your practice with information about performance in key areas. Medication adherence and medication review Remind patients to bring their medications to each visit by adding messaging to appointment reminders. During the visit, use a standard phrase, such as “I’m going to review your medications.” This will help patients recall if they were asked about their medications, if they receive a request to complete a Consumer Assessment of Healthcare Providers and Systems, or CAHPS, survey. Cost, side effects and barriers to picking up their prescriptions may affect your patients’ medication adherence. Here are other tips related to medication adherence:
By following these simple tips, you’ll positively affect several Star measures. For more information, refer to the Medication Adherence Star measure tip sheet. Here’s how to find it:
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Clarification on when billing E/M code with preventive visit is appropriateIn June 2024, Blue Cross Blue Shield of Michigan modified a payment policy that allows for reimbursement of an evaluation and management, or E/M, code at the same date of service as a wellness or preventive visit. We intended for the modification to assist health care providers with reimbursement for services provided and our members receiving care when needed at the time of a preventive visit. However, there has been some confusion as to when it’s appropriate to use this policy, as well as when the member should be informed that the extra code is being billed. Please see below for clarification. When to bill both an E/M and preventative visit on the same date of service You may bill an E/M code with the wellness or preventive visit code when all the following are true:
Examples of when it may be appropriate to bill both an E/M and preventative visit on the same date of service:
Examples of when it’s inappropriate to bill an E/M and a preventative visit on the same date of service:
More information Here are links to earlier articles on this topic:
Pharmacy news roundupWhat you need to know To view all — including the most recent — pharmacy-related provider alerts:
Here are links to pharmacy-related provider alerts from May:
Tip: You can also subscribe to Provider Alerts Weekly to receive a weekly email with links to the previous week’s provider alerts. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Webinars for physicians, coders focus on documentation, codingAction item Register for our 2025 monthly Lunch & Learn webinars focusing on coding and documentation. In 2025, we’ll continue to offer webinars about documentation and coding of common challenging diagnoses. These live, lunchtime educational sessions will also include an opportunity to ask questions.
Provider training website access If you have an Availity Essentials™ account, you can access the provider training website this way:
Existing users who used the same email address as their provider portal profile email will be directed to the training site. If you used a different email address, contact ProviderTraining@bcbsm.com to update your profile. You can also directly access the training website here if you don’t have a provider portal account. After logging in to the provider training website, look in Event Calendar to sign up for your desired session. You can also quickly search for all the sessions with the keyword “lunchtime” and then look under the results for Events. You can listen to the previously recorded sessions, too. Check out the following:
Questions?
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Recorded webinar for providers, office staff focuses on prior authorization best practicesAction item Visit our provider training site to view a recorded webinar on prior authorization requests managed by Carelon Medical Benefits Management. We continue to offer training resources for health care providers and staff. On-demand courses are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network. The following new learning opportunity is available: Prior authorization best practices — for requests managed by Carelon Medical Benefits Management presentation: A recorded version of the June 17 webinar is now available for on-demand viewing. Topics include a walkthrough on how to determine if authorization is needed and case studies that show the most critical elements for submitting requests. How to access provider training To access the training site, follow these steps:
Those who don’t have a provider portal account can directly access the training through the Provider training website. Questions? For more information about using the provider training website, contact the provider training team at ProviderTraining@bcbsm.com. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services.
Clinical editing updates: Claim resubmissions; modifiers; nongenetic prenatal testing; Excludes1 notesIn support of correct coding and payment accuracy, we are providing the information below to keep you informed about forthcoming payment policy updates, new policies and coding reminders. Blue Cross Blue Shield of Michigan commercial Claim resubmission As a reminder, resubmitting a claim before the first claim has been processed can lead to processing delays and duplicate denials. Avoid potential claim processing issues by allowing claims to finalize prior to submitting a new claim. This applied to both professional and facility claims. Inappropriate modifier to diagnosis combination As a reminder, when an ICD-10-CM diagnosis code has a specified anatomical laterality within the code description, the anatomical modifier that is appended to the CPT or HCPCS code must correspond to the laterality within the ICD-10-CM description. Claim lines may be denied that have a laterality diagnosis submitted with a CPT or HCPCS modifier that doesn’t correspond to the diagnosis code. This applies to professional claims. Nongenetic prenatal testing To ensure adherence to clinical guidelines and support accurate claims processing, Blue Cross will enhance its claim editing process for nongenetic prenatal testing. Claims that aren’t billed in accordance with clinical guidelines may be denied. This applies to professional and outpatient facility claims. Medicare Plus Blue℠ Inappropriate diagnosis combinations — Excludes1 notes The Excludes1 notes in the ICD-10-CM diagnosis code set indicate that the excluded code listed in the note can’t be billed with the codes listed above the note. The two conditions shouldn’t be reported together under any circumstance (for example, a congenital form versus an acquired form of the same condition). These conditions are mutually exclusive code combinations. Excludes1 notes are listed within ICD-10-CM chapter levels, under ICD-10-CM codes and elsewhere in the code book. Keep this information in mind:
Claim lines reported with mutually exclusive code combinations, according to the guideline policy for Excludes1 notes, may receive a denial. If you receive a denial, you’ll need to submit a corrected claim. This applies to professional and facility claims. Nongenetic prenatal testing To ensure adherence to clinical guidelines and support accurate claims processing, Blue Cross will enhance its claim editing process for nongenetic prenatal testing. Claims that aren’t billed in accordance with clinical guidelines may be denied. This applies to professional and outpatient facility claims.
Resources for providers, patients to manage chronic conditions, hospital services, follow-up careThis is part of an ongoing series of articles focusing on the tools and resources available to help FEP® members manage their health. When chronic conditions — such as diabetes, hypertension, cardiovascular disease, depression or substance misuse — are managed, complications are reduced. Here are some resources for health care providers and Blue Cross and Blue Shield Federal Employee Program® patients on managing these chronic conditions. For providers The following resources are from the Michigan Quality Improvement Consortium, American Diabetes Association and the American Psychological Association:
For patients The following resources are from the American Heart Association, National Institute of Mental Health, the Asthma and Allergy Foundation of America and the Centers for Disease Control and Prevention to help your patients manage chronic conditions:
Know where to go for care When urgent care is needed, the FEP’s Know Where to Go guide may help your patients decide their best options for care. Follow-up care Encouraging patients to follow up seven and 30 days after discharge from an emergency room or hospital admission can help reduce their risk of readmission and any additional ER visits. FEP member support
If providers or members have questions about FEP benefits or programs, call Customer Service at 1-800-482-3600 for Federal Employees Health Benefits or 1-877-760-8574 for Postal Service Health Benefits, or go to fepblue.org. **Blue Cross Blue Shield of Michigan doesn’t own or control this website. Livongo® is an independent company that provides diabetes management services to Blue Cross and Blue Shield Service Benefit Plan members.
Medical records are now required for some Medicare Advantage claims on skin and tissue substitutesMedicare Plus Blue℠ and BCN Advantage℠ claims received for skin and soft tissue substitutes that fall into the Exclusion Guidelines of our Medicare Advantage Medical Policy must be submitted with medical records. We’ll review the records for reasonableness and necessity. Claims that are submitted without medical records will be denied. Skin substitutes are used to replace or support damaged or lost skin or soft tissue. Guidance on the appropriate use of skin substitutes from the Centers for Medicare & Medicaid Services is not fully developed, which is why we apply Blue Cross Blue Shield of Michigan’s internal policy to claims.
Changes coming to prior authorization process for in-lab sleep studies for most commercial membersStarting Oct. 1, 2025, Carelon Medical Benefits Management will no longer manage prior authorizations for in-lab sleep studies for most Blue Cross Blue Shield of Michigan and Blue Care Network commercial members. These sleep studies will continue to require prior authorization, but the prior authorizations will be managed by Blue Cross and BCN. Submit prior authorization requests through the e-referral system. Watch for provider alerts and articles in The Record and BCN Provider News with additional information about this change, including:
Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services.
New, updated requirements for some medical benefit drugs for Blue Cross commercial URMBT members start Aug. 20For dates of service on or after Aug. 20, 2025, there will be new and changed requirements for some medical benefit drugs for Blue Cross Blue Shield of Michigan commercial UAW Retiree Medical Benefits Trust members. These requirements will apply only when the drugs are administered in an outpatient setting. Note: The requirements don’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714). New requirements for Rytelo, Piasky and Tecelra The drugs listed below will have requirements for Blue Cross commercial UAW Retiree Medical Benefits Trust members. Submit requests as indicated below when these drugs will be billed as a medical benefit.
Changes to requirements for Reblozyl Prior authorizations for Reblozyl® (luspatercept-aamt), HCPCS J0896, will be managed by Carelon. Currently, providers submit prior authorization requests for this drug through the Medical and Pharmacy Drug PA Portal. How to submit authorization requests To submit requests, log in to our provider portal at availity.com,** click on Payer Spaces, and then click on the BCBSM and BCN logo. Click the appropriate tile in the Applications tab:
Note: If you need to request access to our provider portal, see the Register for web tools webpage on bcbsm.com. More about requirements for medical benefit drugs For additional information on requirements related to drugs covered under the medical benefit for URMBT members with Blue Cross non-Medicare plans, see:
We’ll update the pertinent drug lists to reflect the information in this message before the effective date. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services. For more information, go to our ereferrals.bcbsm.com website.
Starting Aug. 1, 2025, we’ll change how we cover RevlimidBlue Cross Blue Shield of Michigan and Blue Care Network will change how we cover Revlimid® on the drug lists associated with our prescription drug plans, starting Aug. 1, 2025. This change will affect most Blue Cross and BCN commercial members under pharmacy benefits. Brand-name Revlimid will no longer be covered for members starting Aug. 1, Instead, we’ll cover the generic equivalent, lenalidomide. If our members continue to stay on Revlimid, they’ll be responsible for the full cost. Members can talk to their doctor if they have concerns about this change. If the member’s pharmacy is unable to fill the prescription with generic lenalidomide, Walgreens Specialty Pharmacy can fill the prescription. If members have questions, they can call the Walgreens Specialty Pharmacy team at 1-866-515-1355. Walgreens Specialty Pharmacy, an independent company, provides specialty pharmacy services to Blue Cross Blue Shield of Michigan and Blue Care Network members.
Yesintek to have a site-of-care requirement for most commercial members, starting Sept. 1For dates of service on or after Sept. 1, 2025, we’re adding a site-of-care requirement for most Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members for Yesintek™ IV and SC (ustekinumab-kfce), HCPCS code Q5100. This drug is covered under medical benefits. You’ll be prompted to select a site of care when you submit prior authorization requests for this drug. If the request meets the clinical criteria for the drug and is for one of the following sites of care, it will be approved automatically:
We may require additional information or documentation for requests to administer Yesintek in an outpatient hospital setting. As a reminder, this drug already requires prior authorization. Providers can submit prior authorization requests using the Medical and Pharmacy Drug PA Portal. Members who start courses of treatment with Yesintek before Sept. 1, 2025, will be able to continue receiving this drug in their current location until their existing authorization expires. If these members continue treatment under a new prior authorization, the site-of-care requirement outlined above will apply. Some commercial groups aren’t subject to these requirements For Blue Cross commercial, prior authorization and site-of-care requirements apply only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. While UAW Retiree Medical Benefits Trust non-Medicare members don’t participate in the standard prior authorization program, these requirements apply to them. Note: These requirements don’t apply to Blue Cross and Blue Shield Federal Employee Program® members. Lists of requirements For more information about requirements related to drugs covered under the medical benefit, see these lists:
We’ll update these lists before the effective date. You can access these lists and other information about requesting prior authorization at ereferrals.bcbsm.com, at these locations: Prior authorization isn't a guarantee of payment. Health care providers need to verify eligibility and benefits for members.
Pharmacy news roundupWhat you need to know To view all — including the most recent — pharmacy-related provider alerts:
Here are links to pharmacy-related provider alerts from May:
Tip: You can also subscribe to Provider Alerts Weekly to receive a weekly email with links to the previous week’s provider alerts. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Clinical editing updates: Claim resubmissions; modifiers; nongenetic prenatal testing; Excludes1 notesIn support of correct coding and payment accuracy, we are providing the information below to keep you informed about forthcoming payment policy updates, new policies and coding reminders. Blue Cross Blue Shield of Michigan commercial Claim resubmission As a reminder, resubmitting a claim before the first claim has been processed can lead to processing delays and duplicate denials. Avoid potential claim processing issues by allowing claims to finalize prior to submitting a new claim. This applied to both professional and facility claims. Inappropriate modifier to diagnosis combination As a reminder, when an ICD-10-CM diagnosis code has a specified anatomical laterality within the code description, the anatomical modifier that is appended to the CPT or HCPCS code must correspond to the laterality within the ICD-10-CM description. Claim lines may be denied that have a laterality diagnosis submitted with a CPT or HCPCS modifier that doesn’t correspond to the diagnosis code. This applies to professional claims. Nongenetic prenatal testing To ensure adherence to clinical guidelines and support accurate claims processing, Blue Cross will enhance its claim editing process for nongenetic prenatal testing. Claims that aren’t billed in accordance with clinical guidelines may be denied. This applies to professional and outpatient facility claims. Medicare Plus Blue℠ Inappropriate diagnosis combinations — Excludes1 notes The Excludes1 notes in the ICD-10-CM diagnosis code set indicate that the excluded code listed in the note can’t be billed with the codes listed above the note. The two conditions shouldn’t be reported together under any circumstance (for example, a congenital form versus an acquired form of the same condition). These conditions are mutually exclusive code combinations. Excludes1 notes are listed within ICD-10-CM chapter levels, under ICD-10-CM codes and elsewhere in the code book. Keep this information in mind:
Claim lines reported with mutually exclusive code combinations, according to the guideline policy for Excludes1 notes, may receive a denial. If you receive a denial, you’ll need to submit a corrected claim. This applies to professional and facility claims. Nongenetic prenatal testing To ensure adherence to clinical guidelines and support accurate claims processing, Blue Cross will enhance its claim editing process for nongenetic prenatal testing. Claims that aren’t billed in accordance with clinical guidelines may be denied. This applies to professional and outpatient facility claims.
Changes coming to prior authorization process for in-lab sleep studies for most commercial membersStarting Oct. 1, 2025, Carelon Medical Benefits Management will no longer manage prior authorizations for in-lab sleep studies for most Blue Cross Blue Shield of Michigan and Blue Care Network commercial members. These sleep studies will continue to require prior authorization, but the prior authorizations will be managed by Blue Cross and BCN. Submit prior authorization requests through the e-referral system. Watch for provider alerts and articles in The Record and BCN Provider News with additional information about this change, including:
Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services.
New, updated requirements for some medical benefit drugs for Blue Cross commercial URMBT members start Aug. 20For dates of service on or after Aug. 20, 2025, there will be new and changed requirements for some medical benefit drugs for Blue Cross Blue Shield of Michigan commercial UAW Retiree Medical Benefits Trust members. These requirements will apply only when the drugs are administered in an outpatient setting. Note: The requirements don’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714). New requirements for Rytelo, Piasky and Tecelra The drugs listed below will have requirements for Blue Cross commercial UAW Retiree Medical Benefits Trust members. Submit requests as indicated below when these drugs will be billed as a medical benefit.
Changes to requirements for Reblozyl Prior authorizations for Reblozyl® (luspatercept-aamt), HCPCS J0896, will be managed by Carelon. Currently, providers submit prior authorization requests for this drug through the Medical and Pharmacy Drug PA Portal. How to submit authorization requests To submit requests, log in to our provider portal at availity.com,** click on Payer Spaces, and then click on the BCBSM and BCN logo. Click the appropriate tile in the Applications tab:
Note: If you need to request access to our provider portal, see the Register for web tools webpage on bcbsm.com. More about requirements for medical benefit drugs For additional information on requirements related to drugs covered under the medical benefit for URMBT members with Blue Cross non-Medicare plans, see:
We’ll update the pertinent drug lists to reflect the information in this message before the effective date. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services. For more information, go to our ereferrals.bcbsm.com website.
Starting Aug. 1, 2025, we’ll change how we cover RevlimidBlue Cross Blue Shield of Michigan and Blue Care Network will change how we cover Revlimid® on the drug lists associated with our prescription drug plans, starting Aug. 1, 2025. This change will affect most Blue Cross and BCN commercial members under pharmacy benefits. Brand-name Revlimid will no longer be covered for members starting Aug. 1, Instead, we’ll cover the generic equivalent, lenalidomide. If our members continue to stay on Revlimid, they’ll be responsible for the full cost. Members can talk to their doctor if they have concerns about this change. If the member’s pharmacy is unable to fill the prescription with generic lenalidomide, Walgreens Specialty Pharmacy can fill the prescription. If members have questions, they can call the Walgreens Specialty Pharmacy team at 1-866-515-1355. Walgreens Specialty Pharmacy, an independent company, provides specialty pharmacy services to Blue Cross Blue Shield of Michigan and Blue Care Network members.
Yesintek to have a site-of-care requirement for most commercial members, starting Sept. 1For dates of service on or after Sept. 1, 2025, we’re adding a site-of-care requirement for most Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members for Yesintek™ IV and SC (ustekinumab-kfce), HCPCS code Q5100. This drug is covered under medical benefits. You’ll be prompted to select a site of care when you submit prior authorization requests for this drug. If the request meets the clinical criteria for the drug and is for one of the following sites of care, it will be approved automatically:
We may require additional information or documentation for requests to administer Yesintek in an outpatient hospital setting. As a reminder, this drug already requires prior authorization. Providers can submit prior authorization requests using the Medical and Pharmacy Drug PA Portal. Members who start courses of treatment with Yesintek before Sept. 1, 2025, will be able to continue receiving this drug in their current location until their existing authorization expires. If these members continue treatment under a new prior authorization, the site-of-care requirement outlined above will apply. Some commercial groups aren’t subject to these requirements For Blue Cross commercial, prior authorization and site-of-care requirements apply only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. While UAW Retiree Medical Benefits Trust non-Medicare members don’t participate in the standard prior authorization program, these requirements apply to them. Note: These requirements don’t apply to Blue Cross and Blue Shield Federal Employee Program® members. Lists of requirements For more information about requirements related to drugs covered under the medical benefit, see these lists:
We’ll update these lists before the effective date. You can access these lists and other information about requesting prior authorization at ereferrals.bcbsm.com, at these locations: Prior authorization isn't a guarantee of payment. Health care providers need to verify eligibility and benefits for members. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||