Subscribe | The Record Archive | Contacts | bcbsm.com
|
October 2024
2024 CPT 3rd-quarter updates: New codes added, deletedThe American Medical Association has added several new codes as part of its quarterly Current Procedural Terminology update. The codes, effective dates and Blue Cross Blue Shield of Michigan’s coverage decisions are below. Pathology and laboratory/proprietary laboratory analysis
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Carelon introduces provider portal feature to enhance prior authorization processIn early October, Carelon Medical Benefits Management is introducing a pilot program to allow health care providers to upload clinical documentation to their provider portal pages when submitting prior authorization requests. This pilot feature applies to Medicare Plus Blue℠ members only and is part of our ongoing effort to enhance the health care provider experience. Providers must still answer all clinical attestation questions pertaining to the case to ensure prompt medical criteria review. An “Attach File” feature will be available when the case requires additional documentation. Click on this button to upload documents to potentially avoid the need for a peer-to-peer review and an appeal. Currently, providers can upload documentation after the prior authorization is submitted, until a decision is made and the case is closed. This feature stays unchanged. During the pilot program period, providers will also be able to upload the documents along with the prior authorization request, if necessary. Carelon performs medical appropriateness reviews of the following services for Medicare Plus Blue members: high-tech radiology, cardiology, radiation oncology and medical oncology. Prior authorization programs vary based on the member’s group contract and benefits. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services.
Billing chart: Blue Cross highlights medical, benefit policy changesYou’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart. This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures. We'll publish information about new Blue Cross groups or changes to group benefits under the Group Benefit Changes heading. For more detailed descriptions of the Blue Cross' policies for these procedures, check under the Commercial Policy tab in Benefit Explainer on Availity®. To access this online information:
2 .Click on Payer Spaces on the Availity menu bar. 3. Click on the BCBSM and BCN logo. 4. Click on Benefit Explainer on the Applications tab. 5. Click on the Commercial Policy tab. 6. Click on Topic. 7. Under Topic Criteria, click on the circle for Unique Identifier and click the drop-down arrow next to Choose Identifier Type, then click on HCPCS Code. 8. Enter the procedure code. 9. Click on Finish. 10. Click on Search. To view the “October 2024 Billing chart,” click here. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Provider enrollment phone line closed Mondays, Fridays in September, OctoberDuring the months of September and October, the provider enrollment phone line (1‑800‑822‑2761) will be closed on Mondays and Fridays, but will remain open on Tuesdays, Wednesdays and Thursdays from 8 a.m. to 4 p.m., except for holiday closures. Why we’re making this temporary change We’re doing this so we can focus resources on processing provider enrollment and change requests. We’re behind in processing these requests, and the temporary phone line closures will allow us to dedicate more staff to complete this work. What we recommend Given the current backlog of requests, we recommend that you don’t call requesting a status on enrollment or change requests submitted less than 30 days ago. If you call our provider enrollment phone line and the wait is expected to be 30 minutes or more, you’ll hear a message asking you to call back at another time. We’re doing this to help you avoid long wait times. We apologize for any inconvenience and appreciate your patience until we’re back to our usual service levels.
Medicare Plus Blue expands membership migration from IkaSystems to NASCO in 2025Blue Cross Blue Shield of Michigan will continue the transition of its Medicare Plus Blue℠ electronic membership files from ikaSystems to the NASCO operating system. This is an important step in enhancing our service delivery and ensuring a seamless claims handling process. Members will receive new ID numbers that must be used in claims submission as part of this process. Timeline and implementation Last year, we began updating our internal processes in preparation for moving our Medicare Plus Blue membership to the NASCO operating system. We’ve already started processing groups new to Medicare Plus Blue in 2024 on the NASCO platform.
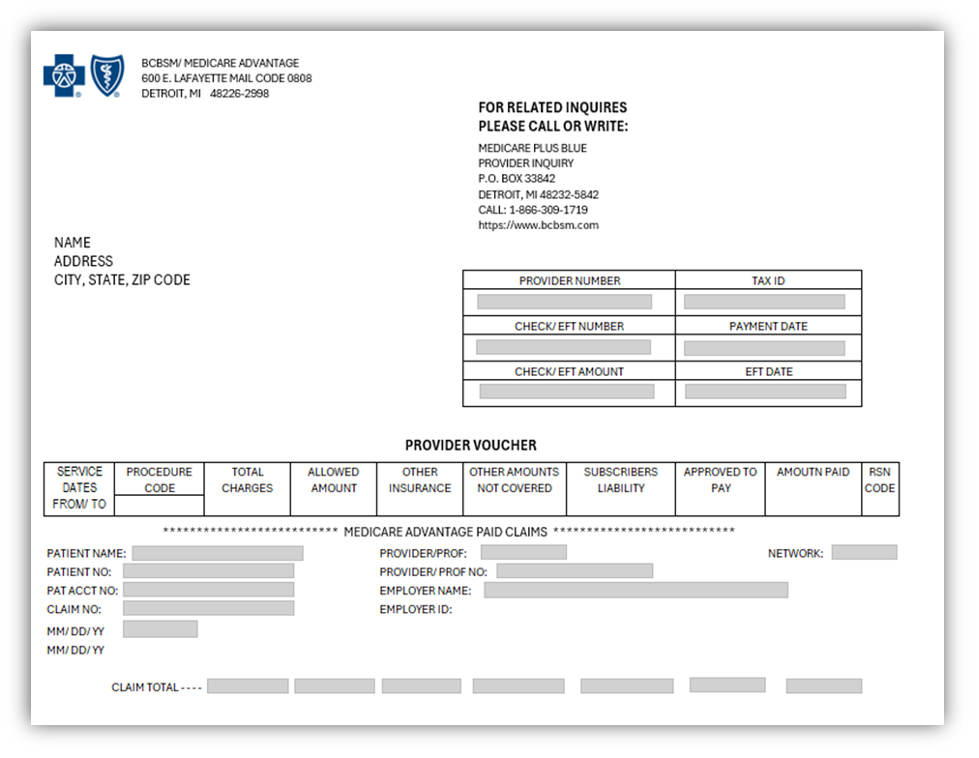
Changes to the provider vouchers As outlined in the sample in the December 2023 issue of The Record, the Medicare Plus Blue voucher looks similar to the Blue Cross commercial voucher but has undergone the following changes to improve clarity and accuracy:
Outpatient claims will continue to be listed on the claim line level. See sample below.
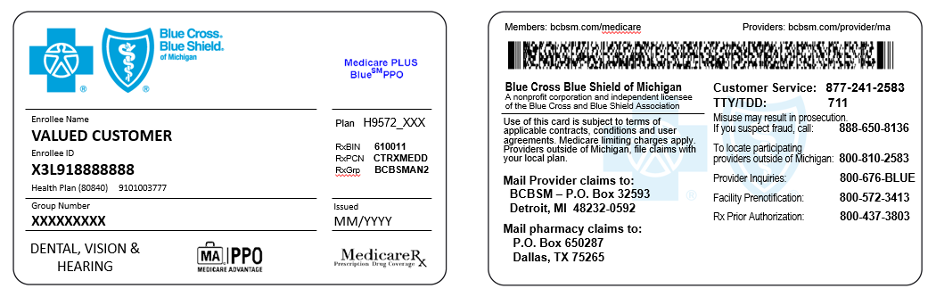
Member ID cards update The format of member ID cards will also be revised to include:
Individual Medicare Plus Blue PPO card with Medicare Rx
Further information Please refer to the October 2023 issue of The Record for additional details on the changes to the check and EFT number series to prepare adequately for these updates. We appreciate your cooperation and understanding as we enhance our systems to serve you better.
Webinars for physicians, coders focus on risk adjustment, codingWe’re offering webinars to explain documentation and coding of common challenging diagnoses. These live, lunchtime educational sessions will also include an opportunity to ask questions. Below is our schedule and the tentative topics for the sessions. All sessions start at noon Eastern time and generally last for 30 minutes. Register for the session that best works with your schedule on the provider training website.
Provider training website access Provider portal users with an Availity Essentials™ account can access the provider training website by logging in to availity.com,** clicking on Payer Space in the top menu bar and then clicking on the BCBSM and BCN logo. Then click on the Applications tab, scroll down to the Provider Training Site tile and click on it. You can also directly access the training website if you don’t have a provider portal account by clicking here. After logging in to the provider training website, look in Event Calendar to sign up for your desired session. You can also quickly search for all the sessions with the keyword “lunchtime” and then look under the results for Events. You can listen to the previously recorded sessions too. Check out the following:
Questions?
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Clinical editing policy updatedTo support correct coding and payment accuracy, we’re providing the information below to keep you informed about forthcoming payment policy updates, new policies and coding reminders. Blue Cross Blue Shield of Michigan commercial: Soft tissue tumor removal claims When procedure codes that represent soft tissue tumor removal are submitted, the diagnosis codes should support that level of service. The appropriate procedure codes representing benign and malignant integumentary lesion excisions should be reported for excision of cutaneous lesions and superficial subcutaneous lesions, rather than the higher-level soft tissue tumor excision codes. This editing will identify soft tissue tumor removal codes when diagnoses on the claim only describe a skin lesion, such as a sebaceous cyst or benign neoplasm. Claims that contain a procedure code for soft tissue tumor removal with a diagnosis that doesn’t support that level of service may be denied.
Follow these guidelines for billing split or shared visitsWe have noticed that members who are involved in physical therapy, occupational therapy, speech therapy and applied behavior analysis are sometimes receiving two or more of these therapies in the same time interval. As a result, we’re providing guidelines for how to bill when more than one therapy provider has provided services to the same Blue Cross Blue Shield of Michigan or Blue Care Network member during the same time interval — for example, from 1 to 2 p.m. on a specific day. For our commercial members For Blue Cross and BCN commercial members:
This applies to but isn’t limited to procedure codes *97153, *97155, *0362T and *0373T. For our Medicare Advantage members For our Medicare Plus Blue℠ and BCN Advantage℠ members, follow the Centers for Medicare & Medicaid Services billing guidelines. For all members Providers are not prohibited from seeing a member at different times during the same day and billing for services. For example, if a patient receives an hour of physical therapy in the morning and an hour of occupational therapy in the afternoon, both providers can bill because the services occurred in different time intervals. This applies to all of our members.
Tips when billing E/M with preventive servicesWhat you need to know To improve the patient experience, let the patient know when a preventive encounter may be expanding to include treatment that could result in costs to the patient. Explaining this up front will save you from patient complaints later. Blue Cross Blue Shield of Michigan and Blue Care Network commercial plans recently began reimbursing evaluation and management, or E/M, services at 50% of the allowed amount when billed on the same day as a preventive service. This was effective with dates of service beginning June 1, 2024, and was announced in the June 2024 issue of The Record and the July-August 2024 issue of BCN Provider News, Page 29. Since June, some members have complained about being charged a copay, coinsurance or deductible following their preventive service when an E/M service was also billed. To maintain a positive member experience, Blue Cross and BCN recommend the following:
Notes
Additional musculoskeletal spinal procedures may be covered, but will require prior authorization for Blue Cross commercial membersFor dates of service on or after Nov. 27, 2024, spinal procedure codes *0164T, *0165T, *22857 and *22862 will no longer be considered experimental for Blue Cross Blue Shield of Michigan commercial members. These procedure codes will require prior authorization through TurningPoint Healthcare Solutions LLC. What you need to know
For more information about TurningPoint’s musculoskeletal surgical quality and safety management program, see the following pages on ereferrals.bcbsm.com:
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and other related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Share information about childhood immunizations, prenatal care, where to go for care with FEP membersThis is part of an ongoing series of articles focusing on the tools and resources available to help FEP® members manage their health. Disease prevention and management support a healthy life. But when urgent or emergent care is needed, knowing where to get treatment can help patients get back on track quickly. Childhood immunizations Routine immunizations can help prevent viral illnesses that may cause long-term health effects. Here is a vaccine schedule from healthychildren.org** listing vaccines needed by age 6** to share with patients. Prenatal care Reminders of the importance of prenatal care for patients in their childbearing years can help prevent pregnancy and delivery complications. The Blue Cross and Blue Shield Federal Employee Program® offers benefits and incentives to encourage members to seek prenatal care:
Follow-up care When urgent or emergent care is needed, educating patients on where to go for care can help reduce their health care costs and possibly save a life. The Know Where to Go guide may help FEP members remember your recommendation in case of an emergency. If a patient is discharged from the emergency room or hospital, encouraging them to follow up seven and 30 days after discharge can help reduce their risk of readmission. For more information on FEP benefits and incentive programs, members and health care providers should call Customer Service at 1-800-482-3600 or go to fepblue.org. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Webinar, on-demand opportunities available for trainingWhat you need to know There’s still time to register for the “Prior Authorizations Programs with Carelon” webinar in October. Provider Experience continues to offer training resources for health care providers and staff. Live webinars and on-demand courses are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network. The following learning opportunities are available now. “Prior Authorization Programs with Carelon” — Oct. 10, 10 to 11 a.m. Eastern time — This live session builds on the first webinar earlier this year to deep dive into some intermediate topics, such as denials and appeals. The presentation is followed by a question-and-answer period. Register for this webinar on the provider training website. To help prepare for the webinar, take one of the courses about working with Carelon:
Medicare Advantage Post-Acute Care Prior Authorization Program — Learn about the changes related to post-acute care services for Medicare Advantage members. This recorded presentation discusses the process changes and what providers need to do starting Oct. 1, 2024. How to access provider training To access the training site, follow these steps:
Those who don’t have a provider portal account can directly access the training through the Provider training website. Questions? For more information about using the provider training website, contact the provider training team at ProviderTraining@bcbsm.com. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Reminder: Home health care services won’t require prior authorization for Medicare Advantage members, starting Oct. 1As we announced in a July 2, 2024, provider alert, home health care services for Medicare Advantage members will no longer require prior authorization, starting Oct. 1, 2024. For claims that are submitted on or after Oct. 1, 2024, our systems won’t look for an approved prior authorization. In addition, we won’t accept retroactive authorization requests. Our provider manuals and related documents have been updated to reflect these changes. Reminders:
Oncology medical drug management moving to OncoHealth for most members Jan. 1For dates of service on or after Jan. 1, 2025, OncoHealth® will manage prior authorizations for medical benefit oncology drugs through the Oncology Value Management program. These drugs are managed by Carelon Medical Benefits Management for dates of service before Jan. 1, 2025. Pharmacy benefit oncology drugs will continue to be managed by Blue Cross and BCN for until March 31, 2025. OncoHealth will begin managing these drugs through the Oncology Value Management program for dates of service on or after April 1, 2025. Watch for provider alerts and articles in our provider newsletters about this upcoming change. OncoHealth will manage the following:
This change will affect the following groups and members:
Watch for additional provider alerts and newsletter articles about this change, including how to register for webinars. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services. OncoHealth is an independent company supporting Blue Cross Blue Shield of Michigan and Blue Care Network by providing cancer support services.
Our program to help reduce avoidable inpatient readmissions for Medicare Advantage members is changingWe’re offering a new program through Blue Cross Coordinated Care℠ Core to reduce avoidable inpatient admissions for Medicare Plus Blue℠ and BCN Advantage℠ members. On Sept. 30, 2024, the nonclinical, transitional care program through Home & Community Care (formerly known as naviHealth, Inc.) for members who are discharged from acute inpatient facilities to certain post-acute care facilities in Michigan will end. Home & Community Care navigation specialists provided support to all members who engaged with the program before the end date. Starting Oct. 1, 2024, care managers from Blue Cross Coordinated Care will work with members who are eligible for the Blue Cross Coordinated Care program and are at risk for unsuccessful discharge to their homes from acute inpatient facilities or from post-acute care facilities. For more information about Blue Cross Coordinated Care, see the document titled Blue Cross Coordinated Care Core: For members with complex, chronic and acute conditions. Home & Community Care is an independent company that provides nonclinical, transitional care services for Blue Cross Blue Shield of Michigan and Blue Care Network members who have Medicare Advantage plans.
Learn more about changes related to post-acute care services for Medicare Advantage members, starting Oct. 1In a May 15, 2024, provider alert, we announced that Home & Community Care (formerly known as naviHealth, Inc.) will no longer manage prior authorizations of post‑acute care services for Medicare Plus Blue℠ and BCN Advantage℠ members starting this fall. Instead, Blue Cross Blue Shield of Michigan and Blue Care Network will manage prior authorizations for these services. Here’s the timeline for this change:
Note: For retroactive authorization requests with dates of service on or before Sept. 30, submit requests to Blue Cross or BCN through the e-referral system. Be sure to enter the Centers for Medicare & Medicaid Services-determined PDPM code in the Case Communication field. We’ll accept retroactive requests through Sept. 30, 2025. If you have questions, send them to UMMedicarePACCA@bcbsm.com. Training resources To access the recorded webinar or register for a live Q&A session about this change, log in to the Provider Training site and search on post-acute care. Look for the following training opportunities:
To access the Provider Training site:
If you have issues regarding access to or navigating the site, email ProviderTraining@bcbsm.com. If you’ve been submitting requests through CarePort Care Management Starting Oct. 1, you’ll no longer be able to submit prior authorization requests for post-acute care services through CarePort Care Management. You’ll need to log in to our provider portal, Availity Essentials, and submit prior authorization requests through the e‑referral system, as you do for prior authorization requests for other services, such as inpatient admissions and post-acute care requests for commercial members. Additional information We’re updating our provider manuals and related resources to reflect this change. For information about post-acute care, see the post-acute care pages on our ereferrals.bcbsm.com website. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. Home & Community Care is an independent company that manages prior authorizations for post-acute care services for Blue Cross Blue Shield of Michigan and Blue Care Network members who have Medicare Advantage plans.
Prior authorization changes for blepharoplasty, enteral nutrition, percutaneous left atrial appendage, varicose vein treatmentFor dates of service on or after Sept. 8, 2024, Blue Cross Blue Shield of Michigan and Blue Care Network changed the prior authorization process for the following services for the lines of business listed in the second column of the table.
We’ve updated the Authorization criteria and preview questionnaires document on ereferrals.bcbsm.com to reflect these changes. Training is available. To view the training:
** Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Call Provider Inquiry to initiate Level 1 appeal according to the claim inquiry and appeal process in the provider manual for commercial PPOBlue Cross Blue Shield of Michigan has updated the filing guidelines for submitting post service, commercial PPO claim appeals. We’ve updated the provider Level 1 appeal process in the Blue Cross Commercial Provider Manual with the new information. There is no change to how Level 1 appeals are handled and reviewed. How to file an appeal To submit a post service claim appeal, health care providers must first contact Provider Inquiry by phone. If you choose to request to an appeal during the phone call, and you have additional documentation to be reviewed, we’ll fax or mail you a Provider Level 1 Appeal Fax Cover Sheet, if you meet eligibility criteria. Post service claim appeals must be received with the Provider Level 1 Appeal Fax Cover Sheet from Provider Inquiry or on the provider’s office letterhead. If you submit an appeal on office letterhead, you must include the reference number, date and time of your call to Provider Inquiry and the representative’s name. The appeal will be considered ineligible if you use any other cover sheets or appeal forms. You won’t be eligible to make further attempts to appeal the claim. The filing guidelines under the Appeals and Problem Resolution chapter of the provider manual has been updated with this information.
Blue Cross will directly handle network performance management duties, starting Nov. 1Starting Nov. 1, 2024, Blue Cross Blue Shield of Michigan will monitor network performance, a service currently performed by SecureCare, an independent company. Blue Cross will directly conduct any future reviews.
There is no action required of health care providers at this time. If a provider is currently on a corrective action plan, the provider should continue working toward the goals put in place by SecureCare. Any follow-up communication about the corrective action plans will come directly from Blue Cross. Please watch for more communications in our provider portal through Availity Essentials™ and The Record as we progress toward this change. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
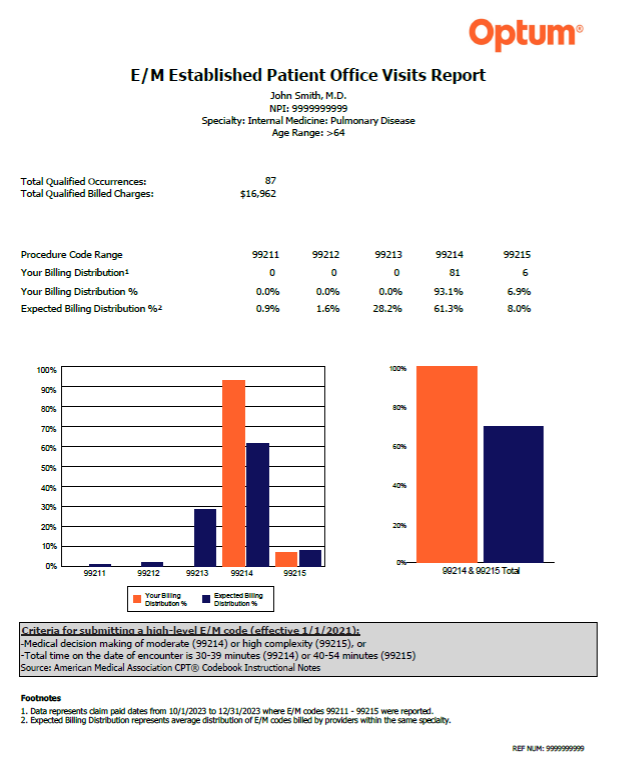
Coding Advisor reviews now called Optum Coding AdvisorIt can be challenging for health care providers and their office staff to select the Current Procedural Terminology, or CPT®, codes that best reflect the complexity of a patient visit. That’s why Blue Cross Blue Shield of Michigan contracted with Optum to implement our Coding Advisor program in 2024. Now called Optum Coding Advisor, the program reviews evaluation and management codes billed and other scenarios (such as modifier 25, observation care and nursing facility care) on claims submitted to Blue Cross. The program provides useful data insights to the provider community and works to maximize coding efficiency and accuracy through up-front education, rather than a traditional post-claim review process. For your reference, we’ve included an example of a physician profile below. Throughout the course of this program, Optum Coding Advisor will continue to monitor billing practices and send updated reports periodically. It may contact your practice to discuss coding variances and to offer one-on-one coding education. You’ll receive all correspondence from Optum. If you have any questions, call the Optum Coding Advisor customer support line at Example of a physician profile:
Do you have time for a Quality Minute about transitional, follow-up care?This is another article in our ongoing series of quick tips designed to be read in 60 seconds or less, and provide your practice with information about performance in key areas. Transitions of Care
Follow-Up After Emergency Department Visit for People with Multiple High-Risk Chronic Conditions
For more information, see the Transitions of Care (TRC) or Follow-Up After Emergency Department Visit for People with Multiple High-Risk Chronic Conditions (FMC) tip sheets. Here’s how to find them.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Blue Cross, BCN cover additional RSV vaccineTo increase access to vaccines and decrease the risk of vaccine-preventable disease outbreaks, Blue Cross Blue Shield of Michigan and Blue Care Network have added the following to our list of vaccines covered under pharmacy benefits.
The following lists all the vaccines that are covered under eligible members’ prescription drug plans. Most Blue Cross and BCN commercial (non-Medicare) members with prescription drug coverage are eligible. If a member meets the coverage criteria, the vaccine is covered with no member out-of-pocket cost. Vaccines with age requirements
If a member doesn’t meet the age requirement for a vaccine, Blue Cross and BCN won’t cover the vaccine under the prescription drug plan, and the claim will reject. Vaccines must be administered by certified, trained and qualified registered pharmacists.
Zynyz, Talvey will require prior authorization for URMBT members with Blue Cross non-Medicare plansThe following drugs will require prior authorization through Carelon Medical Benefits Management for UAW Retiree Medical Benefits Trust members with Blue Cross Blue Shield of Michigan non-Medicare plans. This change will be for dates of service on or after Nov. 21, 2024.
These drugs are covered under medical benefits. This requirement applies only when these drugs are administered in an outpatient setting. Note: This requirement doesn’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714). How to submit authorization requests To access the Carelon provider portal, log in to our provider portal at availity.com,** click on Payer Spaces in the menu bar, and then click the BCBSM and BCN logo. On the Applications tab, click the tile for the Carelon provider portal. If you need to request access to our provider portal, see the Register for web tools webpage on bcbsm.com/providers. You can also log in directly to the Carelon provider portal at providerportal.com** or call Carelon at 1-844-377-1278. More about requirements for medical benefit drugs For additional information on requirements related to drugs covered under medical benefits for URMBT members with Blue Cross non-Medicare plans, see:
We’ll update the drug lists to reflect the information in this message prior to the effective date. As a reminder, prior authorization isn’t a guarantee of payment. Health care providers need to verify eligibility and benefits for members. **Blue Cross Blue Shield of Michigan doesn’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services. For more information, go to our ereferrals.bcbsm.com website.
Webinars for physicians, coders focus on risk adjustment, codingWe’re offering webinars to explain documentation and coding of common challenging diagnoses. These live, lunchtime educational sessions will also include an opportunity to ask questions. Below is our schedule and the tentative topics for the sessions. All sessions start at noon Eastern time and generally last for 30 minutes. Register for the session that best works with your schedule on the provider training website.
Provider training website access Provider portal users with an Availity Essentials™ account can access the provider training website by logging in to availity.com,** clicking on Payer Space in the top menu bar and then clicking on the BCBSM and BCN logo. Then click on the Applications tab, scroll down to the Provider Training Site tile and click on it. You can also directly access the training website if you don’t have a provider portal account by clicking here. After logging in to the provider training website, look in Event Calendar to sign up for your desired session. You can also quickly search for all the sessions with the keyword “lunchtime” and then look under the results for Events. You can listen to the previously recorded sessions too. Check out the following:
Questions?
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Clinical editing policy updatedTo support correct coding and payment accuracy, we’re providing the information below to keep you informed about forthcoming payment policy updates, new policies and coding reminders. Blue Cross Blue Shield of Michigan commercial: Soft tissue tumor removal claims When procedure codes that represent soft tissue tumor removal are submitted, the diagnosis codes should support that level of service. The appropriate procedure codes representing benign and malignant integumentary lesion excisions should be reported for excision of cutaneous lesions and superficial subcutaneous lesions, rather than the higher-level soft tissue tumor excision codes. This editing will identify soft tissue tumor removal codes when diagnoses on the claim only describe a skin lesion, such as a sebaceous cyst or benign neoplasm. Claims that contain a procedure code for soft tissue tumor removal with a diagnosis that doesn’t support that level of service may be denied.
Follow these guidelines for billing split or shared visitsWe have noticed that members who are involved in physical therapy, occupational therapy, speech therapy and applied behavior analysis are sometimes receiving two or more of these therapies in the same time interval. As a result, we’re providing guidelines for how to bill when more than one therapy provider has provided services to the same Blue Cross Blue Shield of Michigan or Blue Care Network member during the same time interval — for example, from 1 to 2 p.m. on a specific day. For our commercial members For Blue Cross and BCN commercial members:
This applies to but isn’t limited to procedure codes *97153, *97155, *0362T and *0373T. For our Medicare Advantage members For our Medicare Plus Blue℠ and BCN Advantage℠ members, follow the Centers for Medicare & Medicaid Services billing guidelines. For all members Providers are not prohibited from seeing a member at different times during the same day and billing for services. For example, if a patient receives an hour of physical therapy in the morning and an hour of occupational therapy in the afternoon, both providers can bill because the services occurred in different time intervals. This applies to all of our members.
Additional musculoskeletal spinal procedures may be covered, but will require prior authorization for Blue Cross commercial membersFor dates of service on or after Nov. 27, 2024, spinal procedure codes *0164T, *0165T, *22857 and *22862 will no longer be considered experimental for Blue Cross Blue Shield of Michigan commercial members. These procedure codes will require prior authorization through TurningPoint Healthcare Solutions LLC. What you need to know
For more information about TurningPoint’s musculoskeletal surgical quality and safety management program, see the following pages on ereferrals.bcbsm.com:
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and other related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Reminder: Home health care services won’t require prior authorization for Medicare Advantage members, starting Oct. 1As we announced in a July 2, 2024, provider alert, home health care services for Medicare Advantage members will no longer require prior authorization, starting Oct. 1, 2024. For claims that are submitted on or after Oct. 1, 2024, our systems won’t look for an approved prior authorization. In addition, we won’t accept retroactive authorization requests. Our provider manuals and related documents have been updated to reflect these changes. Reminders:
Oncology medical drug management moving to OncoHealth for most members Jan. 1For dates of service on or after Jan. 1, 2025, OncoHealth® will manage prior authorizations for medical benefit oncology drugs through the Oncology Value Management program. These drugs are managed by Carelon Medical Benefits Management for dates of service before Jan. 1, 2025. Pharmacy benefit oncology drugs will continue to be managed by Blue Cross and BCN for until March 31, 2025. OncoHealth will begin managing these drugs through the Oncology Value Management program for dates of service on or after April 1, 2025. Watch for provider alerts and articles in our provider newsletters about this upcoming change. OncoHealth will manage the following:
This change will affect the following groups and members:
Watch for additional provider alerts and newsletter articles about this change, including how to register for webinars. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services. OncoHealth is an independent company supporting Blue Cross Blue Shield of Michigan and Blue Care Network by providing cancer support services.
Our program to help reduce avoidable inpatient readmissions for Medicare Advantage members is changingWe’re offering a new program through Blue Cross Coordinated Care℠ Core to reduce avoidable inpatient admissions for Medicare Plus Blue℠ and BCN Advantage℠ members. On Sept. 30, 2024, the nonclinical, transitional care program through Home & Community Care (formerly known as naviHealth, Inc.) for members who are discharged from acute inpatient facilities to certain post-acute care facilities in Michigan will end. Home & Community Care navigation specialists provided support to all members who engaged with the program before the end date. Starting Oct. 1, 2024, care managers from Blue Cross Coordinated Care will work with members who are eligible for the Blue Cross Coordinated Care program and are at risk for unsuccessful discharge to their homes from acute inpatient facilities or from post-acute care facilities. For more information about Blue Cross Coordinated Care, see the document titled Blue Cross Coordinated Care Core: For members with complex, chronic and acute conditions. Home & Community Care is an independent company that provides nonclinical, transitional care services for Blue Cross Blue Shield of Michigan and Blue Care Network members who have Medicare Advantage plans.
Learn more about changes related to post-acute care services for Medicare Advantage members, starting Oct. 1In a May 15, 2024, provider alert, we announced that Home & Community Care (formerly known as naviHealth, Inc.) will no longer manage prior authorizations of post‑acute care services for Medicare Plus Blue℠ and BCN Advantage℠ members starting this fall. Instead, Blue Cross Blue Shield of Michigan and Blue Care Network will manage prior authorizations for these services. Here’s the timeline for this change:
Note: For retroactive authorization requests with dates of service on or before Sept. 30, submit requests to Blue Cross or BCN through the e-referral system. Be sure to enter the Centers for Medicare & Medicaid Services-determined PDPM code in the Case Communication field. We’ll accept retroactive requests through Sept. 30, 2025. If you have questions, send them to UMMedicarePACCA@bcbsm.com. Training resources To access the recorded webinar or register for a live Q&A session about this change, log in to the Provider Training site and search on post-acute care. Look for the following training opportunities:
To access the Provider Training site:
If you have issues regarding access to or navigating the site, email ProviderTraining@bcbsm.com. If you’ve been submitting requests through CarePort Care Management Starting Oct. 1, you’ll no longer be able to submit prior authorization requests for post-acute care services through CarePort Care Management. You’ll need to log in to our provider portal, Availity Essentials, and submit prior authorization requests through the e‑referral system, as you do for prior authorization requests for other services, such as inpatient admissions and post-acute care requests for commercial members. Additional information We’re updating our provider manuals and related resources to reflect this change. For information about post-acute care, see the post-acute care pages on our ereferrals.bcbsm.com website. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. Home & Community Care is an independent company that manages prior authorizations for post-acute care services for Blue Cross Blue Shield of Michigan and Blue Care Network members who have Medicare Advantage plans.
Call Provider Inquiry to initiate Level 1 appeal according to the claim inquiry and appeal process in the provider manual for commercial PPOBlue Cross Blue Shield of Michigan has updated the filing guidelines for submitting post service, commercial PPO claim appeals. We’ve updated the provider Level 1 appeal process in the Blue Cross Commercial Provider Manual with the new information. There is no change to how Level 1 appeals are handled and reviewed. How to file an appeal To submit a post service claim appeal, health care providers must first contact Provider Inquiry by phone. If you choose to request to an appeal during the phone call, and you have additional documentation to be reviewed, we’ll fax or mail you a Provider Level 1 Appeal Fax Cover Sheet, if you meet eligibility criteria. Post service claim appeals must be received with the Provider Level 1 Appeal Fax Cover Sheet from Provider Inquiry or on the provider’s office letterhead. If you submit an appeal on office letterhead, you must include the reference number, date and time of your call to Provider Inquiry and the representative’s name. The appeal will be considered ineligible if you use any other cover sheets or appeal forms. You won’t be eligible to make further attempts to appeal the claim. The filing guidelines under the Appeals and Problem Resolution chapter of the provider manual has been updated with this information.
Blue Cross plans to reimplement an existing policy for payment of external facility reviewsBlue Cross Blue Shield of Michigan plans to reimplement an existing policy that determines payment responsibility for external facility medical necessity reviews. We plan to do this for our commercial PPO (non-Medicare) business starting March 1, 2025, for inpatient medical necessity appeals. This is the same policy used when facilities appeal audits. Second level external appeals in cases involving medical necessity, site of care or quality of care will be reviewed by a peer review organization composed of practicing physicians. If the peer review agency upholds Blue Cross’ decision, the facility will pay the cost of the appeal. What this means to facilities Facilities may incur attorney fees and other expenses in preparation for external reviews for upheld appeals (where the final decision is in Blue Cross' favor). These costs will be the facilities’ responsibility. Independent external review process
Input requested According to the Contract Administration Process — part of the Participating Hospital Agreement that went into effect July 1, 2021 — we allow non-binding input from participating facilities about such proposals. After input is received, Blue Cross has 30 calendar days to respond.
Blue Cross proposes new policy for multiple therapy servicesIn 2022, Blue Cross Blue Shield of Michigan took the proposed payment reduction policy for physical, occupational and speech therapy through the Contract Administration Process. Based on the industry input that we received, the policy was put on hold. Over the past couple of years, we’ve completed further analysis on the industry responses that lead to a policy modification. The proposed policy now excludes all therapy claims with a behavioral health diagnosis. With this change, Blue Cross is looking to implement this proposed policy in March 2025. The proposed CMS multiple therapy policy will apply a reduction in reimbursement for the practice expense portions of therapy procedures when those services are the secondary or subsequent procedures provided on a single date of service by the same group physician and/or other qualified health care professional. This policy will not apply for therapy services rendered for behavioral health diagnoses.
What this means to facilities When multiple therapy services are rendered on the same day, we’ll apply a “therapy pay percent edit.” The primary service will be reimbursed at 100% of the allowed amount, while secondary procedures performed on the same day will be reduced by 50% of the practice expense RVU. The service with the highest RVU is considered the primary service. The practice expense RVU includes the nonphysician clinical and nonclinical labor of the practice, as well as expenses for building space, equipment and office supplies. Such expenses are considered duplicative for each subsequent therapy service and therefore will be reduced accordingly. This practice expense reduction will result in an approximate average reimbursement of 83% of the allowed amount for all subsequent therapy services rendered on the same day. The top five procedure codes that would receive the facility edit (reduced payment) include:
Input requested According to the Contract Administration Process — part of the Participating Hospital Agreement that went into effect July 1, 2021 — we allow non-binding input from participating facilities about such proposals. Input from facilities is requested by Oct. 31, 2024. Send any input you may have to Liz Bowman at ebowman@bcbsm.com. After input is received, Blue Cross has 30 calendar days to respond. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|