Subscribe | The Record Archive | Contacts | bcbsm.com
|
May 2024
Reminder: Supporting documentation required for certain claim typesSpecific documentation should be attached to the Medical Record Routing Form when health care providers bill certain claim types for Blue Cross Blue Shield of Michigan commercial (non-Medicare) members. The form is used to submit required documentation for a previously submitted claim or to link required documentation to an electronically submitted original claim. The supporting documentation is necessary to ensure the claim can be reviewed in a timely manner to determine a procedure’s medical appropriateness and service payment amount. When the necessary documentation isn’t attached, claims will be denied. Blue Cross requires providers to send additional documentation in medical records supporting the treatment provided to the patient for these claim types:
The Medical Record Routing form should not be used for secondary claims and timely filing requests. Instead, these should be discussed with Provider Inquiry. Claim denials not related to medical record requests should also be discussed with Provider Inquiry. If you have any questions or need to speak with Provider Inquiry, call:
Practice caution with requests for patient informationOur Corporate and Financial Investigations Unit has been made aware of provider offices receiving fraudulent requests for patient information, national provider identifier numbers and provider signatures. These requests, which may come to you by standard mail, email or fax, often include clues that indicate they are not legitimate; for example:
DME fraud is becoming more common One of the largest health care fraud schemes of the past few years involves durable medical equipment, costing the health care industry tens of millions of dollars a year. Our Medicare members can be particularly susceptible to these schemes. For example, fraudulent telemarketers may reach out to seniors offering “free” DME equipment to members, intentionally trying to confuse them to get Medicare to pay for equipment that isn’t actually vetted by a medical professional (and that the member often never receives). If you suspect a request may be fraudulent, don’t respond to it When we conduct mass requests for medical records or patient information, we often notify you through a provider newsletter article or a provider alert. If you’re suspicious of a request that you receive, you can contact our Fraud Hotline at 1-844-STOP-FWA (1-844-786-7392) or send an email to StopFraud@bcbsm.com. We may ask you to share the request so we can check its legitimacy. For more useful information, check out the Victimized Provider Project section** of the Centers for Medicare & Medicaid website. The Victimized Provider Project helps keep providers from being held liable for overpayment for claims paid that are the result of identity theft. By working together, we can help eliminate fraud, an effort that will improve patient safety and reduce costs. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
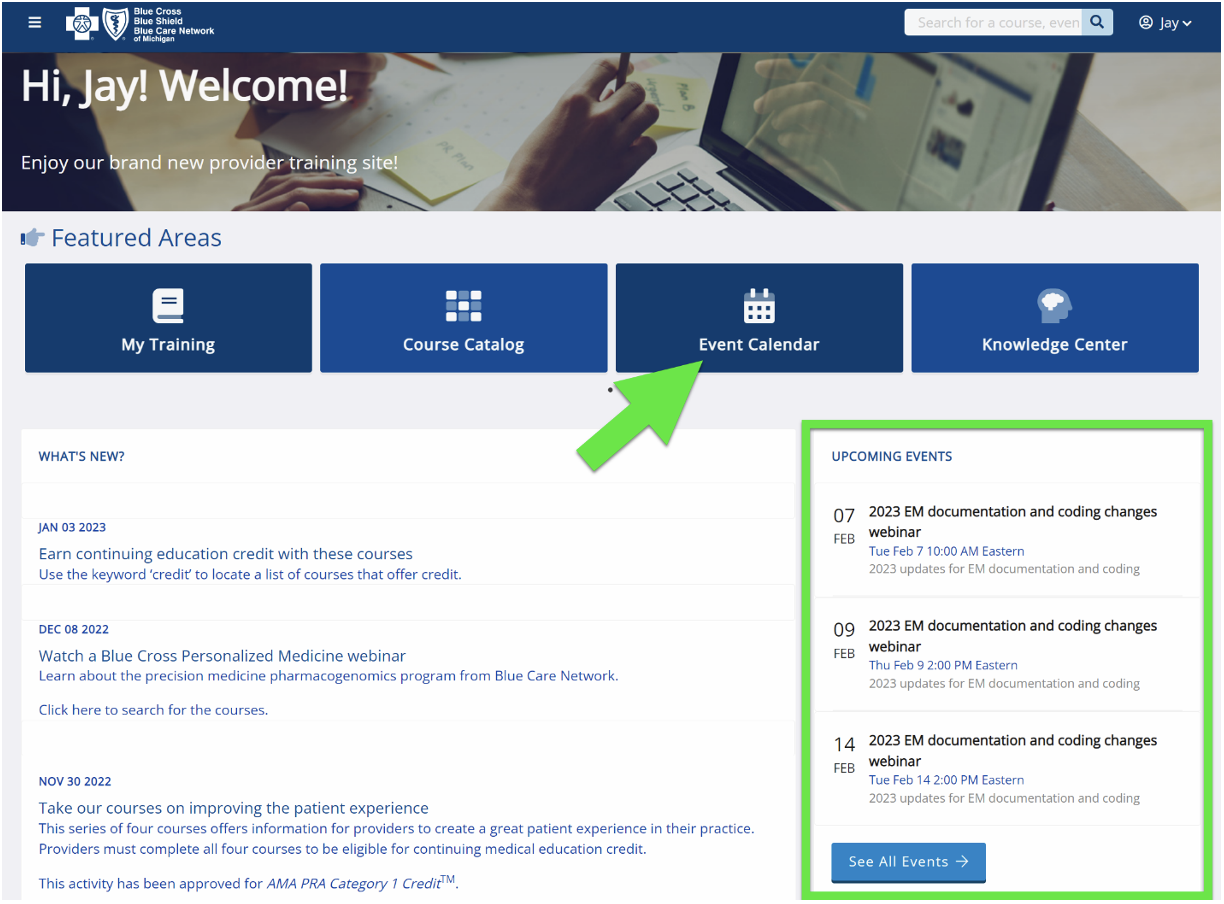
Register now for Prior Authorization Programs with Carelon webinarProvider office personnel responsible for obtaining prior authorizations are encouraged to register now for a webinar about Blue Cross Blue Shield of Michigan’s utilization management program with Carelon Medical Benefits Management (formerly AIM Specialty Health). Carelon performs medical appropriateness reviews on for the following services: high-tech radiology, cardiology, radiation oncology, medical oncology and in-lab sleep studies. Prior authorization programs vary based on the member group contract and benefits. This live session will present an educational overview of all the programs, as well as a demonstration of how to navigate the Carelon portal to submit, view and manage a prior authorization request. The presentation is followed by a question and answer period. You can register for this webinar on our provider training website.
Provider training website access Provider portal users with an Availity Essentials account can access the provider training website on the Applications tab in the BCBSM/BCN Payer Space. Log in through availity.com.** You can also directly access the training website if you don’t have a provider portal account: Provider training website. After logging in to the provider training website, look in Event Calendar to sign up for your desired session. Or quickly search for the session with the keyword “Carelon” and then look under the results for Events.
Questions?
Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Billing chart: Blue Cross highlights medical, benefit policy changesYou’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart. This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures. We'll publish information about new Blue Cross groups or changes to group benefits under the Group Benefit Changes heading. For more detailed descriptions of the Blue Cross' policies for these procedures, check under the Commercial Policy tab in Benefit Explainer on Availity®. To access this online information:
2 .Click on Payer Spaces on the Availity menu bar. 3. Click on the BCBSM and BCN logo. 4. Click on Benefit Explainer on the Applications tab. 5. Click on the Commercial Policy tab. 6. Click on Topic. 7. Under Topic Criteria, click on the circle for Unique Identifier and click the drop-down arrow next to Choose Identifier Type, then click on HCPCS Code. 8. Enter the procedure code. 9. Click on Finish. 10. Click on Search.
None of the information included in this billing chart is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
High-level professional emergency department claims must be supported in medical recordsOptum is requesting medical records on behalf of Blue Cross Blue Shield of Michigan for the pre-pay program. Medical records for professional emergency department PPO claims will be requested to verify that documentation supports a high-level of medical decision making for claims billed with CPT code *99285. CPT code *99285 is used to report emergency department visits requiring a medically appropriate history and/or examination and high medical decision-making. Here are some key documentation reminders to support CPT code *99285:
Remember, per CPT guidelines, “Time is not a descriptive component for the emergency department levels of E/M services because emergency department services are typically provided on a variable intensity basis, often involving multiple encounters with several patients over an extended period of time.” Refer to the American College of Emergency Physicians MDM Grid** for leveling guidelines. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Register now for 2024 virtual provider symposium sessionsThis year’s virtual provider symposiums focusing on quality measures, documentation and coding guidelines will start in May. Registration is now open on the provider training website. Physicians, physician assistants, nurse practitioners, nurses and coders can receive continuing education credits for attending. Once you’re logged in to the provider training site, open the event calendar to sign up for any of the sessions listed below. You can also quickly search for all the sessions with the keyword “symposium” by looking under the results for Events. All Star Performance-HEDIS® / Star Rating Measure Overview: For physicians and office staff responsible for closing gaps in care related to quality adult measures
Coding and Documentation Tips for 2024 and Beyond: For physicians, coders, billers and administrative staff
Provider training website access Provider portal users with an Availity® Essentials account can access the provider training website by logging in to availity.com,** clicking on Payer Space in the top menu bar and then clicking on the BCBSM and BCN logo. Then click on the Applications tab, scroll down to the Provider Training Site tile and click on it. You can also directly access the training website if you don’t have a provider portal account. Questions?
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. HEDIS® is a registered trademark of the National Committee for Quality Assurance. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. Accreditation Statement: CME Statement:
Register now for our Behavioral Health SummitProfessional behavioral health providers and billers are invited to our upcoming Behavioral Health Summit. Attendees can interact with Provider Engagement & Transformation consultants, receive tailored presentations from various behavioral health-specific departments and network with peers and industry leaders. The summit will be held in person on Thursday, May 9, and Thursday, June 6, and virtually Thursday, Aug. 8.
For more information about the summit, contact providerengagement@bcbsm.com.
Resources can help educate patients about flu vaccine, acute bronchitisThis is part of an ongoing series of articles focusing on the tools and resources available to help FEP® members manage their health. Half of U.S. adults hospitalized for the flu have heart disease, and the risk of having a first heart attack is six times greater following a flu infection, according to the American Heart Association.** That risk can be substantially lowered by receiving the flu vaccine, but less than half of U.S. adults do so. The Centers for Disease Control and Prevention developed a flyer, Treating Influenza: Information for People at High Risk for Serious Flu Complications,** to help health care providers educate patients with chronic conditions on the importance of flu vaccinations. Preventing and treating bronchitis If a patient develops acute bronchitis or bronchiolitis, the CDC also developed a patient education flyer, Preventing and Treating Bronchitis,** you can distribute. The flyer provides information on what acute bronchitis is, symptoms, when to seek medical care and treatment recommendations, including why antibiotics aren’t used. Information about FEP For information on Blue Cross and Blue Shield Federal Employee Program® benefits, providers and members can visit fepblue.org or call Customer Service at 1-800-482-3600. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Do you have time for a Quality Minute?Quality Minute will be an ongoing series of quick tips designed to be read in 60 seconds or less and provide your practice with information about performance in key areas. Medicare wellness visits
For more information Refer to the Medicare Wellness Visits tip sheet. Here’s how to find it:
Review medications at every patient visit
Cost, side effects and barriers to pharmacy pickup may affect medication adherence
By following these simple tips, you’ll improve patients’ experience measured by several Medicare Star measures. For more information, refer to the Medication Adherence Star measure tip sheet. CAHPS®, Consumer Assessment of Healthcare Providers and Systems, is a registered trademark of the Agency for Healthcare Quality and Research. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Changes coming to coverage of some prescription drugsStarting July 1, 2024, we’re changing how we cover some medications on the drug lists associated with our prescription drug plans. The following list detail these changes. We’ll notify affected members, their groups and their health care providers in writing about the changes, see below for more information. Drugs that will have a higher copayment Unless noted, both the brand name and available generic equivalents of the following drugs won’t be covered. If a member fills a prescription for one of these drugs on or after July 1, 2024, they’ll be responsible for the full cost. The brand-name drug that will have a higher copayment is listed along with suggested, covered preferred alternatives that have similar effectiveness, quality and safety. When pharmacies fill prescriptions with preferred alternatives, the generic equivalents are dispensed, if available. Additional coverage requirements may apply for preferred alternatives.
**Nonpreferred brand drugs are not covered for members with a closed benefit.
Webinars for physicians, coders focus on risk adjustment, codingWe’re offering webinars about documentation and coding of common challenging diagnoses. These live, lunchtime educational sessions will also include an opportunity to ask questions. Below is our schedule and the tentative topics for the sessions. All sessions start at noon Eastern time and generally last for 30 minutes. Register for the session that best works with your schedule on the provider training website.
Provider training website access Provider portal users with an Availity® Essentials account can access the provider training website by logging in to availity.com,** clicking on Payer Space in the top menu bar and then clicking on the BCBSM and BCN logo. Then click on the Applications tab, scroll down to the Provider Training Site tile and click on it. You can also directly access the training website if you don’t have a provider portal account: Provider training website. After logging in to the provider training website, look in Event Calendar to sign up for your desired session. You can also quickly search for all the sessions with the keyword “lunchtime" and then look under the results for Events. You can listen to the previously recorded sessions too. Check out the following:
Questions?
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
We’re reminding members about important preventive cancer screeningsBlue Cross Blue Shield of Michigan and Blue Care Network want to help members live their healthiest lives and help providers close gaps in care. We’ll begin sending targeted communications throughout May and in to early June to members who haven’t had recommended cancer screenings to encourage them to discuss their cancer risk and testing options with their physicians. Health care providers can help members by scheduling time to discuss the importance of cervical, breast and colorectal cancer screenings. Providers play an important role in this preventive care by discussing lifestyle, family history and a screening schedule that’s right for each patient. Effective cancer screening and early detection has led to declining death rates from cancer. The Healthcare Effectiveness Data, or HEDIS®, measures for screening are below: Colorectal cancer The Colorectal Cancer Screening HEDIS® Star Measure assesses patients ages 45 to 75 who had appropriate screenings for colorectal cancer. Colonoscopy is the gold standard for colorectal cancer screening. Providers can discuss alternative options for patients who are reluctant to have one. Providers can discuss lifestyle modifications for members. More than half of all cases and deaths are attributable to modifiable risk factors, such as smoking, an unhealthy diet, high alcohol consumption, physical inactivity and excess body weight. Breast cancer Breast cancer is the second most common cancer in women, according to the American Cancer Society. Cervical cancer Cervical cancer is the fourth most common cancer in women globally, according to the World Health Organization. The HEDIS measure for cervical cancer screening uses the following criteria for those who were recommended for routine screening:
New reporting system for 2024 HEDIS measures The National Committee for Quality Assurance has developed a new reporting standard for HEDIS, called electronic clinical data systems, or ECDS. This reporting standard defines the data sources and types of structured data acceptable for use for a measure. Data systems that may be eligible for ECDS reporting include administrative claims, clinical registries, health information exchanges, immunization information systems, disease and case management systems, and electronic health records. HEDIS quality measures reported using ECDS inspire innovative use of electronic clinical data to document high-quality patient care, according to NCQA. Breast cancer and colorectal cancer screenings are ECDS measures for 2024. Information about ECDS is available on the NQCA** website. Healthcare Effectiveness Data Information Set, or HEDIS®, is a registered trademark of the National Committee for Quality Assurance (NCQA). **Blue Cross and BCN don’t own or control this website.
Register now for the virtual series: Equitable Care for Older AdultsThis May, Blue Cross Blue Shield of Michigan will present a three-part webinar series highlighting some of the conditions commonly experienced by older patients and how each of these conditions presents barriers to obtaining care. This “Equitable Care for Older Adults” series will explore the effects that hearing loss, vision impairments and cognitive decline can have on patient care. We’ll also discuss best practices that can make care more equitable for those experiencing these impairments. Register below for each session in this series: Part 1: May 21, 2024, from noon to 12:45 p.m. Part 2: May 23, 2024, from noon to 12:45 p.m. Part 3: May 30, 2024, from noon to 12:45 p.m. Register by visiting the Upcoming Webinars page of the Blue Cross Patient Experience site. Recordings will be available on-demand at the Patient Experience site after the live sessions. Continuing medical education, or CME, credits are available for physicians. Continuing education units, or CEU, are available for medical assistants and other health care professionals. Strategies to care for older patients and manage challenging patients Visit the on-demand page of the Patient Experience site to view recently added educational resources. Our April series, “Improving Health Outcomes for Older Adults,” is now available on demand.
The “Managing Challenging Patient Interactions” webinar, which is also available on demand, provides strategies for health care professionals to manage upset or frustrated patients or caregivers in the office setting. It covers tactics to prevent challenging situations, tips to stay calm and de-escalation strategies. This session is also available as an in-office lunch-and-learn meeting for practices. (1 hour) For these and other on-demand resources, CME credits are available for physicians and CEUs are available for medical assistants and other health care professionals. For more information, email PatientExperience@bcbsm.com or visit the Blue Cross Patient Experience site.
Requirements and codes changed for some medical benefit drugsBlue Cross Blue Shield of Michigan and Blue Care Network encourage proper utilization of high-cost medications that are covered under the medical benefit. As part of this effort, we maintain comprehensive lists of requirements for our members. In January, February and March 2024, we added requirements for some medical benefit drugs. These requirements went into effect on various dates. In addition, some drugs were assigned new HCPCS codes. Changes in requirements For Blue Cross commercial and BCN commercial members, we added prior authorization requirements, site-of-care requirements or both for the following drugs:
For Medicare Plus Blue℠ and BCN Advantage℠ members, we added prior authorization requirements for the following drugs:
Code changes The table below shows HCPCS code changes that were effective January 2024 for the medical benefit drugs managed by Blue Cross and BCN.
Drug lists For additional details, see the following drug lists:
These lists are also available on the following pages of the ereferrals.bcbsm.com website: Additional information about these requirements We communicated these changes previously through provider alerts, which contain additional details. You can view the provider alerts on ereferrals.bcbsm.com and on our Provider Resources site, which is accessible through our provider portal, availity.com.*** Additional information for Blue Cross commercial groups For Blue Cross commercial groups, authorization requirements apply only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group List. A link to this list is also available on the Blue Cross Medical Benefit Drugs page of the ereferrals.bcbsm.com website. Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don't participate in the standard prior authorization program. Reminder An authorization approval isn’t a guarantee of payment. Health care providers need to verify eligibility and benefits for members. **May be assigned a unique code in the future. ***Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Prior authorization requirements changing for musculoskeletal pain management, spinal procedure codesFor dates of service on or after June 3, 2024, we’re adding prior authorization requirements for several pain management and spinal procedure codes that are managed through TurningPoint Healthcare Solutions LLC’s Musculoskeletal Surgical Quality and Safety Management program. The tables below outline the changes. In the tables:
Note: This change doesn’t affect MESSA members. For additional information about which members are affected, see the Musculoskeletal Services and Pain Management Services pages on ereferrals.bcbsm.com. Pain management procedure codes
Spinal procedure codes
Additional information We updated the document titled Musculoskeletal procedure codes that require authorization by TurningPoint to reflect these changes. For more information about TurningPoint’s Musculoskeletal Surgical Quality and Safety Management program, see the following pages on the ereferrals.bcbsm.com website:
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and other related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Step therapy requirement to be added for VPRIV, Elelyso for Medicare Advantage members, starting June 1For dates of service on or after June 1, 2024, health care providers must show that Medicare Plus Blue℠ and BCN Advantage℠ members tried and failed Cerezyme® (imiglucerase) when requesting prior authorization for the following drugs:
Cerezyme is Blue Cross Blue Shield of Michigan and Blue Care Network’s preferred enzyme replacement therapy for Gaucher disease. These drugs are covered under members’ medical benefits, not their pharmacy benefits. Providers should submit prior authorization requests for VPRIV and Elelyso through the NovoLogix® online tool. As a reminder, Cerezyme doesn’t require prior authorization for dates of service on or after Jan. 1, 2024. When prior authorization is required VPRIV and Elelyso require prior authorization when they are administered by a provider in sites of care such as outpatient facilities or physician offices and are billed in one of the following ways:
Submit prior authorization requests through NovoLogix To access NovoLogix, log in to our provider portal at availity.com,** click Payer Spaces in the menu bar and then click the BCBSM and BCN logo. You’ll find links to the NovoLogix tools on the Applications tab. If you need to request access to our provider portal, follow the instructions on the Register for web tools page on bcbsm.com. List of requirements For a list of requirements related to drugs covered under the medical benefit, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members. We’ll update this list prior to the effective date. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. NovoLogix is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network. Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Clinical editing policies updatedTo ensure correct coding and payment accuracy, we’re sharing the below information about forthcoming payment policy updates, new policies and coding reminders. Blue Cross Blue Shield of Michigan commercial Modifier “AS” is required for assistant at surgery billing The modifier “AS” is used to indicate that the assistant at the time of surgery was a physician's assistant, certified nurse practitioner, clinical nurse specialist or doctor of podiatric medicine. Claims submitted without the modifier may be denied when major surgical procedures have also been billed by a physician. In August, we plan to add a new line appending modifier AS to ensure services are reimbursed at the correct rate. Don’t bill multiple anesthesia codes Only one anesthesia code should be reported per anesthesia administration encounter and when multiple surgical procedures are performed during a single anesthesia administration. Claims submitted for more than one anesthesia code may receive a denial. Blue Care Network commercial Preadmission testing Testing that is related to an inpatient admission is considered inclusive to the inpatient stay. Claims submitted for preadmission testing when related to inpatient admission may receive a denial. BCN Advantage℠ Frequency limit for subsequent visits BCN commercial and BCN Advantage Reporting multiple visits Both BCN commercial and BCN Advantage don’t reimburse more than one emergency room visit on the same day. Multiple visits reported on the same day, with same revenue code, without condition code GO aren’t allowed.
Elrexfio, Talvey to require prior authorization for most members, starting June 20For dates of service on or after June 20, 2024, the following drugs will require prior authorization through the Oncology Value Management program:
The Oncology Value Management program is administered by Carelon Medical Benefits Management. These drugs are part of members’ medical benefits, not their pharmacy benefits. Prior authorization requirements apply when these drugs are administered in outpatient settings for:
How to submit prior authorization requests Submit prior authorization requests to Carelon using one of the following methods:
Note: If you need to request access to our provider portal, see the Register for web tools webpage on bcbsm.com. Drug lists For additional information on requirements related to drugs covered under the medical benefit, refer to the following drug lists:
We’ll update the pertinent drug lists to reflect the information in this message prior to the effective date. As a reminder, prior authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services.
Columvi, Daxxify, Qalsody to require prior authorization for URMBT members with Blue Cross non-Medicare plansFor dates of service on or after July 1, 2024, the drugs listed below will require prior authorization for UAW Retiree Medical Benefits Trust members with Blue Cross Blue Shield of Michigan non‑Medicare plans. These drugs are part of members’ medical benefits, not their pharmacy benefits. See the table below for:
The prior authorization requirement applies apply only when these drugs are administered in an outpatient setting. Note: The requirement doesn’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714). How to submit prior authorization requests To access the Carelon provider portal or the NovoLogix online tool, log in to our provider portal (availity.com),** click Payer Spaces in the menu bar and then click the BCBSM and BCN logo. On the Applications tab, click the tile for the Carelon provider portal or the appropriate NovoLogix tool. If you need to request access to our provider portal, see the Register for web tools webpage on bcbsm.com. You can also log in directly to the Carelon provider portal at providerportal.com.** More about requirements for medical benefit drugs For additional information on requirements related to drugs covered under the medical benefit for URMBT members with Blue Cross non-Medicare plans, see:
We’ll update the drug lists to reflect the information in this message prior to the effective date. As a reminder, prior authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. ** Blue Cross Blue Shield of Michigan doesn’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services.
Cinryze, Elfabrio, Evkeeza to have site-of-care requirement for most commercial members, starting July 1For dates of service on or after July 1, 2024, we’re adding a site-of-care requirement for Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members for the following drugs covered under the medical benefit:
The NovoLogix® online tool will prompt you to select a site of care when you submit prior authorization requests for these drugs. If the request meets the clinical criteria for the drug and is for one of the following sites of care, it will be approved automatically:
Additional information or documentation may be required for requests to administer Cinryze, Elfabrio and Evkeeza in an outpatient hospital setting. As a reminder, these drugs already require prior authorization; providers can submit prior authorization requests using NovoLogix. The new site-of-care requirement is in addition to the current prior authorization requirement. Members who start courses of treatment with Cinryze, Elfabrio or Evkeeza before July 1, 2024, will be able to continue receiving the drug in their current location until their existing authorization expires. If these members then continue treatment under a new prior authorization, the site-of-care requirement outlined above will apply. Some Blue Cross commercial groups aren’t subject to these requirements For Blue Cross commercial groups, prior authorization and site-of-care requirements apply only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. Note: Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don’t participate in the standard prior authorization program. List of requirements For a full list of requirements related to drugs covered under the medical benefit, see the Blue Cross and BCN utilization management medical drug list for Blue Cross commercial and BCN commercial members. We’ll update this list prior to the effective date. You can access this list and other information about requesting prior authorization at ereferrals.bcbsm.com, at these locations: Prior authorization isn't a guarantee of payment. Health care providers need to verify eligibility and benefits for members. NovoLogix is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network.
Udenyca Onbody to require prior authorization for most commercial members effective immediatelyFor dates of service on or after March 5, 2024, we’ve added a prior authorization requirement for most Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members for the following drug covered under the medical benefit:
Note: This change applies to UAW Retiree Medical Benefits Trust (non-Medicare) members. How to submit prior authorization requests Submit prior authorization requests through the NovoLogix® online tool. It offers real-time status checks and immediate approvals for certain medications. To access NovoLogix, log in to our provider portal at availity.com,** click Payer Spaces in the menu bar, and then click the BCBSM and BCN logo. You’ll find links to the NovoLogix tools on the Applications tab. Note: If you need to request access to our provider portal, see the Register for web tools webpage on bcbsm.com. Some Blue Cross commercial groups aren’t subject to this requirement For Blue Cross commercial groups, this prior authorization requirement applies only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group List. Note: Blue Cross and Blue Shield Federal Employee Program® members don’t participate in the standard prior authorization program. List of requirements For a full list of requirements related to drugs covered under the medical benefit, see the Blue Cross and BCN utilization management medical drug list for Blue Cross commercial and BCN commercial members. Prior authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. ** Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Questionnaire changes in e-referral systemOn March 31, 2024, we added one questionnaire and updated other questionnaires in the e-referral system. We’ve updated the Authorization criteria and preview questionnaires document on the ereferrals.bcbsm.com website to reflect these changes. As a reminder, we use our authorization criteria, our medical policies and your answers to the questionnaires in the e-referral system when making utilization management determinations on your prior authorization requests. New questionnaire We’ve added the following questionnaire to the e-referral system.
Updated questionnaires We’ve updated the following questionnaires in the e-referral system.
Preview questionnaires Preview questionnaires show the questions you’ll need to answer in the e-referral system so you can prepare your answers ahead of time. To find the preview questionnaires, see the document titled Authorization criteria and preview questionnaires. You can access this document by going to ereferrals.bcbsm.com and doing the following:
Authorization criteria and medical policies The Authorization criteria and preview questionnaires document explains how to access the pertinent authorization criteria and medical policies.
Most commercial members must try preferred product for ZyntegloFor dates of service on or after April 19, 2024, we’ve added a step therapy requirement for Zynteglo™ (betibeglogene autotemcel), HCPCS code J3590.
We’ve updated the Blue Cross and BCN utilization management medical drug list to reflect the preferred drug. The drugs discussed above continue to require prior authorization through the NovoLogix® online tool. Some Blue Cross commercial groups aren’t subject to these requirements For Blue Cross commercial groups, this prior authorization requirement applies only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. Note: Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don’t participate in the standard prior authorization program. Additional information For more information about medical benefit drugs, see the following pages on ereferrals.bcbsm.com: Prior authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. NovoLogix is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network.
Changes coming to coverage of some prescription drugsStarting July 1, 2024, we’re changing how we cover some medications on the drug lists associated with our prescription drug plans. The following list detail these changes. We’ll notify affected members, their groups and their health care providers in writing about the changes, see below for more information. Drugs that will have a higher copayment Unless noted, both the brand name and available generic equivalents of the following drugs won’t be covered. If a member fills a prescription for one of these drugs on or after July 1, 2024, they’ll be responsible for the full cost. The brand-name drug that will have a higher copayment is listed along with suggested, covered preferred alternatives that have similar effectiveness, quality and safety. When pharmacies fill prescriptions with preferred alternatives, the generic equivalents are dispensed, if available. Additional coverage requirements may apply for preferred alternatives.
**Nonpreferred brand drugs are not covered for members with a closed benefit.
Webinars for physicians, coders focus on risk adjustment, codingWe’re offering webinars about documentation and coding of common challenging diagnoses. These live, lunchtime educational sessions will also include an opportunity to ask questions. Below is our schedule and the tentative topics for the sessions. All sessions start at noon Eastern time and generally last for 30 minutes. Register for the session that best works with your schedule on the provider training website.
Provider training website access Provider portal users with an Availity® Essentials account can access the provider training website by logging in to availity.com,** clicking on Payer Space in the top menu bar and then clicking on the BCBSM and BCN logo. Then click on the Applications tab, scroll down to the Provider Training Site tile and click on it. You can also directly access the training website if you don’t have a provider portal account: Provider training website. After logging in to the provider training website, look in Event Calendar to sign up for your desired session. You can also quickly search for all the sessions with the keyword “lunchtime" and then look under the results for Events. You can listen to the previously recorded sessions too. Check out the following:
Questions?
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
We’re reminding members about important preventive cancer screeningsBlue Cross Blue Shield of Michigan and Blue Care Network want to help members live their healthiest lives and help providers close gaps in care. We’ll begin sending targeted communications throughout May and in to early June to members who haven’t had recommended cancer screenings to encourage them to discuss their cancer risk and testing options with their physicians. Health care providers can help members by scheduling time to discuss the importance of cervical, breast and colorectal cancer screenings. Providers play an important role in this preventive care by discussing lifestyle, family history and a screening schedule that’s right for each patient. Effective cancer screening and early detection has led to declining death rates from cancer. The Healthcare Effectiveness Data, or HEDIS®, measures for screening are below: Colorectal cancer The Colorectal Cancer Screening HEDIS® Star Measure assesses patients ages 45 to 75 who had appropriate screenings for colorectal cancer. Colonoscopy is the gold standard for colorectal cancer screening. Providers can discuss alternative options for patients who are reluctant to have one. Providers can discuss lifestyle modifications for members. More than half of all cases and deaths are attributable to modifiable risk factors, such as smoking, an unhealthy diet, high alcohol consumption, physical inactivity and excess body weight. Breast cancer Breast cancer is the second most common cancer in women, according to the American Cancer Society. Cervical cancer Cervical cancer is the fourth most common cancer in women globally, according to the World Health Organization. The HEDIS measure for cervical cancer screening uses the following criteria for those who were recommended for routine screening:
New reporting system for 2024 HEDIS measures The National Committee for Quality Assurance has developed a new reporting standard for HEDIS, called electronic clinical data systems, or ECDS. This reporting standard defines the data sources and types of structured data acceptable for use for a measure. Data systems that may be eligible for ECDS reporting include administrative claims, clinical registries, health information exchanges, immunization information systems, disease and case management systems, and electronic health records. HEDIS quality measures reported using ECDS inspire innovative use of electronic clinical data to document high-quality patient care, according to NCQA. Breast cancer and colorectal cancer screenings are ECDS measures for 2024. Information about ECDS is available on the NQCA** website. Healthcare Effectiveness Data Information Set, or HEDIS®, is a registered trademark of the National Committee for Quality Assurance (NCQA). **Blue Cross and BCN don’t own or control this website.
Register now for the virtual series: Equitable Care for Older AdultsThis May, Blue Cross Blue Shield of Michigan will present a three-part webinar series highlighting some of the conditions commonly experienced by older patients and how each of these conditions presents barriers to obtaining care. This “Equitable Care for Older Adults” series will explore the effects that hearing loss, vision impairments and cognitive decline can have on patient care. We’ll also discuss best practices that can make care more equitable for those experiencing these impairments. Register below for each session in this series: Part 1: May 21, 2024, from noon to 12:45 p.m. Part 2: May 23, 2024, from noon to 12:45 p.m. Part 3: May 30, 2024, from noon to 12:45 p.m. Register by visiting the Upcoming Webinars page of the Blue Cross Patient Experience site. Recordings will be available on-demand at the Patient Experience site after the live sessions. Continuing medical education, or CME, credits are available for physicians. Continuing education units, or CEU, are available for medical assistants and other health care professionals. Strategies to care for older patients and manage challenging patients Visit the on-demand page of the Patient Experience site to view recently added educational resources. Our April series, “Improving Health Outcomes for Older Adults,” is now available on demand.
The “Managing Challenging Patient Interactions” webinar, which is also available on demand, provides strategies for health care professionals to manage upset or frustrated patients or caregivers in the office setting. It covers tactics to prevent challenging situations, tips to stay calm and de-escalation strategies. This session is also available as an in-office lunch-and-learn meeting for practices. (1 hour) For these and other on-demand resources, CME credits are available for physicians and CEUs are available for medical assistants and other health care professionals. For more information, email PatientExperience@bcbsm.com or visit the Blue Cross Patient Experience site.
Requirements and codes changed for some medical benefit drugsBlue Cross Blue Shield of Michigan and Blue Care Network encourage proper utilization of high-cost medications that are covered under the medical benefit. As part of this effort, we maintain comprehensive lists of requirements for our members. In January, February and March 2024, we added requirements for some medical benefit drugs. These requirements went into effect on various dates. In addition, some drugs were assigned new HCPCS codes. Changes in requirements For Blue Cross commercial and BCN commercial members, we added prior authorization requirements, site-of-care requirements or both for the following drugs:
For Medicare Plus Blue℠ and BCN Advantage℠ members, we added prior authorization requirements for the following drugs:
Code changes The table below shows HCPCS code changes that were effective January 2024 for the medical benefit drugs managed by Blue Cross and BCN.
Drug lists For additional details, see the following drug lists:
These lists are also available on the following pages of the ereferrals.bcbsm.com website: Additional information about these requirements We communicated these changes previously through provider alerts, which contain additional details. You can view the provider alerts on ereferrals.bcbsm.com and on our Provider Resources site, which is accessible through our provider portal, availity.com.*** Additional information for Blue Cross commercial groups For Blue Cross commercial groups, authorization requirements apply only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group List. A link to this list is also available on the Blue Cross Medical Benefit Drugs page of the ereferrals.bcbsm.com website. Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don't participate in the standard prior authorization program. Reminder An authorization approval isn’t a guarantee of payment. Health care providers need to verify eligibility and benefits for members. **May be assigned a unique code in the future. ***Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Prior authorization requirements changing for musculoskeletal pain management, spinal procedure codesFor dates of service on or after June 3, 2024, we’re adding prior authorization requirements for several pain management and spinal procedure codes that are managed through TurningPoint Healthcare Solutions LLC’s Musculoskeletal Surgical Quality and Safety Management program. The tables below outline the changes. In the tables:
Note: This change doesn’t affect MESSA members. For additional information about which members are affected, see the Musculoskeletal Services and Pain Management Services pages on ereferrals.bcbsm.com. Pain management procedure codes
Spinal procedure codes
Additional information We updated the document titled Musculoskeletal procedure codes that require authorization by TurningPoint to reflect these changes. For more information about TurningPoint’s Musculoskeletal Surgical Quality and Safety Management program, see the following pages on the ereferrals.bcbsm.com website:
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and other related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Step therapy requirement to be added for VPRIV, Elelyso for Medicare Advantage members, starting June 1For dates of service on or after June 1, 2024, health care providers must show that Medicare Plus Blue℠ and BCN Advantage℠ members tried and failed Cerezyme® (imiglucerase) when requesting prior authorization for the following drugs:
Cerezyme is Blue Cross Blue Shield of Michigan and Blue Care Network’s preferred enzyme replacement therapy for Gaucher disease. These drugs are covered under members’ medical benefits, not their pharmacy benefits. Providers should submit prior authorization requests for VPRIV and Elelyso through the NovoLogix® online tool. As a reminder, Cerezyme doesn’t require prior authorization for dates of service on or after Jan. 1, 2024. When prior authorization is required VPRIV and Elelyso require prior authorization when they are administered by a provider in sites of care such as outpatient facilities or physician offices and are billed in one of the following ways:
Submit prior authorization requests through NovoLogix To access NovoLogix, log in to our provider portal at availity.com,** click Payer Spaces in the menu bar and then click the BCBSM and BCN logo. You’ll find links to the NovoLogix tools on the Applications tab. If you need to request access to our provider portal, follow the instructions on the Register for web tools page on bcbsm.com. List of requirements For a list of requirements related to drugs covered under the medical benefit, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members. We’ll update this list prior to the effective date. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. NovoLogix is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network. Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Michigan acute inpatient facilities should submit peer-to-peer review requests, appeals through the e-referral systemAcute inpatient facilities in Michigan should use the e-referral system to submit peer-to-peer review requests and appeals related to prior authorization requests for inpatient acute care medical and surgical (non-behavioral health) admissions. Submitting these requests through the e-referral system involves completing questionnaires and attaching clinical documentation when applicable. Submitting through the e-referral system offers a streamlined process that:
Here are some resources you can use to learn more:
When the e-referral system is not available, you can:
You can’t use the e-referral system to submit a peer-to-peer review request or appeal for prior authorization requests that:
Non-Michigan facilities can’t use the e-referral system to submit peer-to-peer review or appeal requests. They must continue to:
Emergency Department Facility Evaluation and Management Coding Policy takes effect June 1Blue Cross Blue Shield of Michigan began using the Optum Emergency Department Claims Analyzer, or EDCA, Jan. 4, 2023, after adoption through the Participating Hospital Agreement contract administration process. Last fall, we paused the program to continue discussions with health care providers about coding variations and algorithms to see if there were alternative ways to reduce the trend of higher-level emergency department coding. Based on these discussions, we’ll begin using the EDCA again June 1, 2024, in conjunction with a new Emergency Department Facility Evaluation and Management Coding Policy. We developed this reimbursement policy to ensure that facilities are reimbursed based on the consistent coding that correctly describes a patient’s clinical condition and the health care services provided in accordance with industry standards and guidelines. Why implement the Emergency Department Facility Evaluation and Management Coding Policy? This policy will provide guidance for how Blue Cross will reimburse UB (facility) claims billed with evaluation and management, or E/M, codes at the appropriate level of service, based on the complexity of patient condition and diagnostic services provided in the outpatient emergency department. The policy is based on coding principles established by the Centers for Medicare & Medicaid Services and the CPT and HCPCS code descriptions. What does this mean to facilities? Blue Cross will initially review claims that are billed with a level 4 or 5 E/M code for the appropriate level of care on a prepayment basis. Claims that don’t meet the policy criteria will be adjusted and reimbursed at the appropriate level. How will claims be reviewed? An algorithm will be applied that takes three factors into account to determine a calculated visit level for the emergency department E/M services provided. The three factors are:
Applicable codes:
Facility claims may receive adjustments to the level 4 or 5 E/M codes submitted to reflect a lower E/M code calculated by the EDC analyzer or may receive a denial for the code level submitted. For those that are denied, facilities should review remittance information, as Blue Cross will indicate the appropriate E/M code for the claim to be accepted in accordance with the policy. Facilities that are reimbursed for outpatient services on a percent of charge basis may rebill a denied level 4 or 5 E/M code with a correct E/M code and the corresponding corrected charge in accordance with their chargemaster. Exclusions Claims for the following may be excluded from an adjustment or denial:
The Emergency Department Facility Evaluation and Management Coding Policy can be found on the Provider Resources website:
You can find additional information about the policy on the Provider Resources website. **Blue Cross and BCN don’t own or control this website.
Clinical editing policies updatedTo ensure correct coding and payment accuracy, we’re sharing the below information about forthcoming payment policy updates, new policies and coding reminders. Blue Cross Blue Shield of Michigan commercial Modifier “AS” is required for assistant at surgery billing The modifier “AS” is used to indicate that the assistant at the time of surgery was a physician's assistant, certified nurse practitioner, clinical nurse specialist or doctor of podiatric medicine. Claims submitted without the modifier may be denied when major surgical procedures have also been billed by a physician. In August, we plan to add a new line appending modifier AS to ensure services are reimbursed at the correct rate. Don’t bill multiple anesthesia codes Only one anesthesia code should be reported per anesthesia administration encounter and when multiple surgical procedures are performed during a single anesthesia administration. Claims submitted for more than one anesthesia code may receive a denial. Blue Care Network commercial Preadmission testing Testing that is related to an inpatient admission is considered inclusive to the inpatient stay. Claims submitted for preadmission testing when related to inpatient admission may receive a denial. BCN Advantage℠ Frequency limit for subsequent visits BCN commercial and BCN Advantage Reporting multiple visits Both BCN commercial and BCN Advantage don’t reimburse more than one emergency room visit on the same day. Multiple visits reported on the same day, with same revenue code, without condition code GO aren’t allowed.
Elrexfio, Talvey to require prior authorization for most members, starting June 20For dates of service on or after June 20, 2024, the following drugs will require prior authorization through the Oncology Value Management program:
The Oncology Value Management program is administered by Carelon Medical Benefits Management. These drugs are part of members’ medical benefits, not their pharmacy benefits. Prior authorization requirements apply when these drugs are administered in outpatient settings for:
How to submit prior authorization requests Submit prior authorization requests to Carelon using one of the following methods:
Note: If you need to request access to our provider portal, see the Register for web tools webpage on bcbsm.com. Drug lists For additional information on requirements related to drugs covered under the medical benefit, refer to the following drug lists:
We’ll update the pertinent drug lists to reflect the information in this message prior to the effective date. As a reminder, prior authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services.
Columvi, Daxxify, Qalsody to require prior authorization for URMBT members with Blue Cross non-Medicare plansFor dates of service on or after July 1, 2024, the drugs listed below will require prior authorization for UAW Retiree Medical Benefits Trust members with Blue Cross Blue Shield of Michigan non‑Medicare plans. These drugs are part of members’ medical benefits, not their pharmacy benefits. See the table below for:
The prior authorization requirement applies apply only when these drugs are administered in an outpatient setting. Note: The requirement doesn’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714). How to submit prior authorization requests To access the Carelon provider portal or the NovoLogix online tool, log in to our provider portal (availity.com),** click Payer Spaces in the menu bar and then click the BCBSM and BCN logo. On the Applications tab, click the tile for the Carelon provider portal or the appropriate NovoLogix tool. If you need to request access to our provider portal, see the Register for web tools webpage on bcbsm.com. You can also log in directly to the Carelon provider portal at providerportal.com.** More about requirements for medical benefit drugs For additional information on requirements related to drugs covered under the medical benefit for URMBT members with Blue Cross non-Medicare plans, see:
We’ll update the drug lists to reflect the information in this message prior to the effective date. As a reminder, prior authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. ** Blue Cross Blue Shield of Michigan doesn’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services.
Cinryze, Elfabrio, Evkeeza to have site-of-care requirement for most commercial members, starting July 1For dates of service on or after July 1, 2024, we’re adding a site-of-care requirement for Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members for the following drugs covered under the medical benefit:
The NovoLogix® online tool will prompt you to select a site of care when you submit prior authorization requests for these drugs. If the request meets the clinical criteria for the drug and is for one of the following sites of care, it will be approved automatically:
Additional information or documentation may be required for requests to administer Cinryze, Elfabrio and Evkeeza in an outpatient hospital setting. As a reminder, these drugs already require prior authorization; providers can submit prior authorization requests using NovoLogix. The new site-of-care requirement is in addition to the current prior authorization requirement. Members who start courses of treatment with Cinryze, Elfabrio or Evkeeza before July 1, 2024, will be able to continue receiving the drug in their current location until their existing authorization expires. If these members then continue treatment under a new prior authorization, the site-of-care requirement outlined above will apply. Some Blue Cross commercial groups aren’t subject to these requirements For Blue Cross commercial groups, prior authorization and site-of-care requirements apply only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. Note: Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don’t participate in the standard prior authorization program. List of requirements For a full list of requirements related to drugs covered under the medical benefit, see the Blue Cross and BCN utilization management medical drug list for Blue Cross commercial and BCN commercial members. We’ll update this list prior to the effective date. You can access this list and other information about requesting prior authorization at ereferrals.bcbsm.com, at these locations: Prior authorization isn't a guarantee of payment. Health care providers need to verify eligibility and benefits for members. NovoLogix is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network.
Udenyca Onbody to require prior authorization for most commercial members effective immediatelyFor dates of service on or after March 5, 2024, we’ve added a prior authorization requirement for most Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members for the following drug covered under the medical benefit:
Note: This change applies to UAW Retiree Medical Benefits Trust (non-Medicare) members. How to submit prior authorization requests Submit prior authorization requests through the NovoLogix® online tool. It offers real-time status checks and immediate approvals for certain medications. To access NovoLogix, log in to our provider portal at availity.com,** click Payer Spaces in the menu bar, and then click the BCBSM and BCN logo. You’ll find links to the NovoLogix tools on the Applications tab. Note: If you need to request access to our provider portal, see the Register for web tools webpage on bcbsm.com. Some Blue Cross commercial groups aren’t subject to this requirement For Blue Cross commercial groups, this prior authorization requirement applies only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group List. Note: Blue Cross and Blue Shield Federal Employee Program® members don’t participate in the standard prior authorization program. List of requirements For a full list of requirements related to drugs covered under the medical benefit, see the Blue Cross and BCN utilization management medical drug list for Blue Cross commercial and BCN commercial members. Prior authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. ** Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Questionnaire changes in e-referral systemOn March 31, 2024, we added one questionnaire and updated other questionnaires in the e-referral system. We’ve updated the Authorization criteria and preview questionnaires document on the ereferrals.bcbsm.com website to reflect these changes. As a reminder, we use our authorization criteria, our medical policies and your answers to the questionnaires in the e-referral system when making utilization management determinations on your prior authorization requests. New questionnaire We’ve added the following questionnaire to the e-referral system.
Updated questionnaires We’ve updated the following questionnaires in the e-referral system.
Preview questionnaires Preview questionnaires show the questions you’ll need to answer in the e-referral system so you can prepare your answers ahead of time. To find the preview questionnaires, see the document titled Authorization criteria and preview questionnaires. You can access this document by going to ereferrals.bcbsm.com and doing the following:
Authorization criteria and medical policies The Authorization criteria and preview questionnaires document explains how to access the pertinent authorization criteria and medical policies.
Most commercial members must try preferred product for ZyntegloFor dates of service on or after April 19, 2024, we’ve added a step therapy requirement for Zynteglo™ (betibeglogene autotemcel), HCPCS code J3590.
We’ve updated the Blue Cross and BCN utilization management medical drug list to reflect the preferred drug. The drugs discussed above continue to require prior authorization through the NovoLogix® online tool. Some Blue Cross commercial groups aren’t subject to these requirements For Blue Cross commercial groups, this prior authorization requirement applies only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. Note: Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don’t participate in the standard prior authorization program. Additional information For more information about medical benefit drugs, see the following pages on ereferrals.bcbsm.com: Prior authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. NovoLogix is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||