Subscribe | The Record Archive | Contacts | bcbsm.com
|
November 2023
Blue Cross and BCN receive 4-Star ratings from CMSThe Centers for Medicare & Medicaid Services recently announced its 2024 Medicare Star Ratings. Both our BCN Advantage℠ HMO plan and our Medicare Plus Blue℠ PPO plan captured 4-Star ratings, making our plans once again among the highest rated Medicare Advantage plans in the country. Star Ratings are CMS’ measure of how well health plans serve MA members. They’re designed to evaluate how well plans that contract with Medicare perform, and to help consumers select a Medicare Advantage plan that works best for them. “Star Ratings are vital to our mission to serve our Medicare Advantage members,” said Daniel J. Loepp, Blue Cross Blue Shield of Michigan president and CEO. “We value the provider community’s partnership when it comes to delivering exceptional, high-quality care — a key factor that drove our strong ratings.” Why value-based care matters when it comes to Star Ratings “When we look at these performance measures and how our Star Ratings are calculated, it’s clear that value-based care is a winning path forward for everyone,” said Dr. James Grant, senior vice president and chief medical officer for Blue Cross. “We couldn’t have achieved these Star Ratings without our physician partners, and we look forward to the future as we continue to meaningfully engage everyone in value-based arrangements that will benefit our members.” The goal for the 2025 rating year is to maintain or exceed 4-Star ratings for the PPO and HMO. A deeper dive into the ratings Medicare considers five categories when assigning Star Ratings:
Blue Cross’ 4-Star ratings for 2024 reflect sustained performance in several key areas, including HEDIS® measures** and CAHPS® surveys.*** The Consumer Assessment of Healthcare Providers and Systems surveys, developed by the Agency for Healthcare Research and Quality, evaluate a member’s experience with their plan, quality of care received and access to care. **HEDIS®, which stands for Healthcare Effectiveness and Information Set, is a registered trademark of the National Committee for Quality Assurance. ***CAHPS®, which stands for Consumer Assessment of Healthcare Providers and Systems, is a registered trademark of the Agency for Healthcare Quality and Research.
Your patients can order free, at-home COVID-19 testsDue to an increase in demand for COVID-19 testing, the federal government is restarting a program for each U.S. household to order four free COVID-19 rapid tests for mail delivery. These tests can be ordered through COVIDtests.gov.** Share this information with your patients who may benefit from having at-home COVID-19 rapid tests. Note: COVIDtests.gov** also provides the following information:
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Where to view provider portal change and status updatesAre you curious about what’s new with our provider portal, Availity® Essentials? We’re always working to improve your experience in our provider portal. Here are a couple of examples:
To stay up to date with the latest provider portal news, you can access the Provider Portal Change and Status Updates document, which includes information about important updates, known defects and workarounds. We update this document monthly or more often, as needed. To view this document:
Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
New location of pharmacy services information for providers on our public websiteWe’ve relocated our pharmacy services information for providers on our public website. This site contains information on medical and pharmacy benefit drug lists for both Blue Cross Blue Shield of Michigan and Blue Care Network, Medicare and pharmacy forms and documents, prior authorization request information and other resources. Here’s how to find it:
HCPCS 3rd-quarter update: New and deleted codesThe Centers for Medicare & Medicaid Services has added several new codes as part of its quarterly Health Care Procedure Coding System updates. The codes, effective dates and Blue Cross Blue Shield of Michigan’s coverage decisions are below. Radiopharmaceuticals Radiology
Injections/Outpatient PPS
Injections
Surgery/Drugs Administered Other Than Oral Method
Behavioral Health
Durable Medical Equipment
Prosthetic and Orthotic
Surgery/Skin Substitutes
Other Medical Services
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
HCPCS replacement codes established, effective Oct. 1J0801 replaces J0800 when billing for Acthar Gel (corticotropin) Effective Oct. 1, 2023, the Centers for Medicare & Medicaid Services has established a new procedure code for specialty medical drug Acthar Gel (corticotropin). All services through Sept. 30, 2023, should be reported with code J0800. All services performed on and after Oct. 1, 2023, must be reported with J0801. Prior authorization is required through the Medical Benefit Drug Program for J0801 for all groups unless they have opted out of the program. For groups that have opted out of the prior authorization program, this service requires manual review for individual consideration. J0802 replaces C9399, J3490, J3590 and J9999 when billing for Purified Cortrophin Gel (corticotropin) Effective Oct. 1, 2023, CMS has established a permanent procedure code for specialty medical drug Purified Cortrophin Gel (corticotropin). All services through Sept. 30, 2023, should be reported with code C9399, J3490, J3590 and J9999. All services performed on and after Oct. 1, 2023, must be reported with J0802. Prior authorization is required through the Medical Benefit Drug Program for J0802 for all groups unless they have opted out of the program For groups that have opted out of the prior authorization program, this service requires manual review for individual consideration. J2781 replaces C9399, J3490, J3590 and J9999 when billing for Syfovre (pegcetacoplan) Effective Oct. 1, 2023, CMS has established a permanent procedure code for specialty medical drug Syfovre (pegcetacoplan). All services through Sept. 30, 2023, should be reported with code C9399, J3490, J3590 and J9999. All services performed on and after Oct. 1, 2023, must be reported with J2781. Prior authorization is required through the Medical Benefit Drug Program for J2781 for all groups unless they have opted out of the program. For groups that have opted out of the prior authorization program, this service requires manual review for individual consideration. None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations. Billing chart: Blue Cross highlights medical, benefit policy changesYou’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart. This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures. We'll publish information about new Blue Cross groups or changes to group benefits under the Group Benefit Changes heading. For more detailed descriptions of the Blue Cross' policies for these procedures, check under the Commercial Policy tab in Benefit Explainer on Availity®. To access this online information:
2 .Click on Payer Spaces on the Availity menu bar. 3. Click on the BCBSM and BCN logo. 4. Click on Benefit Explainer on the Applications tab. 5. Click on the Commercial Policy tab. 6. Click on Topic. 7. Under Topic Criteria, click on the circle for Unique Identifier and click the drop-down arrow next to Choose Identifier Type, then click on HCPCS Code. 8. Enter the procedure code. 9. Click on Finish. 10. Click on Search.
Teladoc Health is an independent company that provides virtual care solutions for Blue Cross Blue Shield of Michigan. None of the information included in this billing chart is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
2 new Medicare Plus Blue plans can help members save in 2024This fall, during open enrollment for 2024, Blue Cross Blue Shield of Michigan is offering two new Medicare Plus Blue℠ plans for individual plan members. In addition to the Essential, Vitality, Signature or Assure plans, members can now choose:
Here are key details about the plans and benefits, which will take effect Jan. 1, 2024: Medicare Plus Blue Part B Credit Our Medicare Plus Blue Part B Credit plan reduces the Part B premium that all Medicare beneficiaries have to pay each month. Members who enroll in this plan will:
Members aren’t eligible for the Part B Credit plan if they receive premium assistance from Medicaid or another source. Medicare Plus Blue PPO + Meijer Blue Cross is working with retail supercenter Meijer to offer the new Medicare Plus Blue PPO + Meijer plan with a $0 premium. This plan offers an affordable, convenient option for Medicare Plus Blue members who shop at Meijer. The plan adds Meijer to the list of plan-approved retailers that members can choose from to use their over-the-counter allowance benefit. Members who enroll in the Medicare Plus Blue PPO + Meijer plan can use their $660 annual in-store allowance in Meijer stores to purchase:
Both the Medicare Plus Blue PPO Part B Credit and the Medicare Plus Blue PPO + Meijer plans offer the same large array of preventive and supplemental benefits our current members have to help keep them healthy. This includes:
Note: You’ll want to check your patient’s eligibility and benefits to ensure they have access to the SilverSneakers fitness program. SilverSneakers is a registered trademark of Tivity Health, Inc. © 2023 Tivity Health, Inc. All rights reserved.
New enhanced benefits will be available to Medicare Advantage members in 2024Medicare Plus Blue℠ and BCN Advantage℠ are adding three new enhanced benefits to their comprehensive Medicare Advantage plans for the 2024 plan year. Beginning Jan. 1, 2024, members can capitalize on the following new benefits:
Note: Check your patient’s eligibility and benefits in our provider portal (availity.com)** to verify coverage for these new benefits. Details on new enhanced benefits Ambulance services without transport: Currently, if a member or another person calls for an ambulance for a member’s health emergency, and the member isn’t transported, the service isn’t covered. Beginning Jan. 1, 2024, if the ambulance providers are able to stabilize the member at the current location without transporting to a facility, the plan covers the services with the applicable cost sharing. This service isn’t covered outside of the U.S. or its territories. Enhanced annual wellness visit: After having Medicare Part B for longer than 12 months, members can get an annual wellness visit every 12 months. The annual wellness visit:
No cost sharing applies for this benefit. Mobile crisis and crisis stabilization for behavioral health: This benefit offers improved care for people experiencing a behavioral health crisis. Services include mobile crisis intervention by eligible providers through telehealth or face-to-face, on-site services and crisis stabilization. Members can be treated at their home or another location, and at participating outpatient psychiatric centers available in certain counties in Michigan. Cost sharing applies for these services. For more information on crisis care services and locations, visit our crisis care webpage. Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
We’re making some changes in behavioral health processes beginning Jan. 1What you need to know New Directions, now known as Lucet, won’t handle requests for Blue Cross Blue Shield of Michigan commercial members related to dates of service before Jan. 1, 2024, a change from what was originally published. Submit requests for prior authorization, continued stay reviews and appeals related to dates of service before Jan. 1, 2024, using one of these methods:
When contacting Blue Cross by email or phone, you’ll need to provide the following:
We communicated in previous articles that starting Jan. 1, 2024, Blue Cross Blue Shield of Michigan and Blue Care Network will consolidate the prior authorization and case management functions for behavioral health services, including treatment for autism. This will affect all members covered by Blue Cross commercial, Medicare Plus Blue℠, BCN commercial and BCN Advantage℠ plans, except those in certain employer groups. Refer to the Mental Health and Substance Use Disorder Carve-Out List for more information. The programs are called:
These programs will align and standardize prior authorization and case management functions for Blue Cross and BCN members. We expect this consistency across lines of business to simplify processes for health care providers. Consistent processes The main benefit for providers is consistency across all lines of business. For example, for dates of service on or after Jan. 1, 2024:
FAQ document We’ve published the Blue Cross Behavioral Health: Frequently asked questions for providers document, which contains many details you’ll need to know. In the FAQ document, you’ll find important information that will help you navigate this change, including how to submit requests for prior authorization, continued stay reviews and appeals for all dates of service. We’ll update the FAQ document with additional information as it becomes available. Key change for Blue Cross commercial prior authorization requests Starting Jan. 1, 2024, New Directions, now known as Lucet, won’t handle requests for Blue Cross commercial members with dates of service on or after Jan. 1, 2024. Also, Lucet won’t handle requests related to dates of service before Jan. 1, 2024, a change from what was originally published. For Blue Cross commercial members, submit requests for prior authorization, continued stay reviews and appeals related to dates of service before Jan. 1, 2024, using one of these methods:
When you email or call, provide:
Medical necessity criteria For dates of service on or after Jan. 1, 2024, Blue Cross Behavioral Health will use the following to make determinations on prior authorization requests:
Later in 2023, you’ll be able to access these criteria on our Services That Need Prior Authorization webpage at bcbsm.com. Appeals process Starting in 2024, the addresses for submitting appeals of prior authorization requests that aren’t approved will change. Refer to the determination letters for the addresses. Training We’ll offer training for providers to learn how to access and use the new provider portal to submit prior authorization requests. Watch for more information.
Washtenaw County Community Mental Health joins crisis services programWashtenaw County Community Mental Health is the newest organization to join Blue Cross Blue Shield of Michigan’s crisis services program. It offers both mobile crisis and residential crisis services. For mobile crisis services or to determine the location of the appropriate facility for the member, call 734-544-3050. Our crisis services program was designed to offer our members (and their family members) a wider array of care options if they’re experiencing a mental health crisis. To learn more about the program and to see a list of other participating facilities, visit the Crisis Care section of our behavioral health website. Here are some claim editing remindersCPT Category II codes: The lab codes below require a CPT Category II code when you’re providing test results and the test was performed in an office location. CPT Category II codes are a set of tracking codes that can be used to measure performance. They may be used to describe results from clinical laboratory or radiology tests and other procedures intended to address patient safety issues. *80061 — Lipid panel. This panel must include the following:
*83036 — Hemoglobin; glycosylated (A1c) Claims that are submitted without the associated CPT Category II code may undergo claim editing and be denied. If you receive a claim denial, submit a corrected claim with the appropriate Category II code, not an appeal. New patient visit edits: A new patient is one who hasn’t received any professional services from the physician or another physician of the same specialty who belongs to the same group practice within the past three years. Prior visits are those indicated with evaluation and management codes or other face-to-face professional services billed within a three-year period. A face-to-face professional service includes E&M codes, surgical procedures and other procedures or services. Only one new patient visit is allowed in a three-year period. New patient claims that are submitted within three years of a prior new patient visit or any face-to-face service may be denied. If you receive a claim denial, submit a corrected claim using the appropriate established patient E&M code, not an appeal. None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations. Reminder: Signature required on medical recordsWhat you need to know Medical records require a provider’s signature. This article reviews what constitutes acceptable electronic and handwritten signatures.
A signature is mandatory on medical records to identify who provided services for the patient. It also validates the services were documented, reviewed and authenticated by the provider. Requirements for an acceptable signature depend on whether the medical record is generated by an electronic health record or is handwritten. Services performed by nonphysician practitioners who require physician supervision must be signed by the overseeing provider. Examples of services requiring a supervising physician signature include therapeutic and behavioral health. This includes providers supervising licensed social workers, behavioral health therapists, massage therapists and registered nurses performing administration of drugs. Electronic signatures Electronic signatures must be generated by encrypted or password-protected software and used solely by the author of the report or record. The Medicare Integrity Manual (Ch. 3, 3.3.2.4) states: “Providers using electronic systems need to recognize that there is a potential for misuse or abuse with alternate signature methods. For example, providers need a system and software products that are protected against modification, etc., and should apply adequate administrative procedures that correspond to recognized standards and laws. The individual whose name is on the alternate signature method and the provider bear the responsibility for the authenticity of the information for which an attestation has been provided. Physicians are encouraged to check with their attorneys and malpractice insurers concerning the use of alternative signature methods.” Electronic signatures must contain the following key elements:
Acceptable attestation statements include the following:
Example (electronic signature and attestation statement):
Unacceptable electronic signatures include the following:
Examples:
Handwritten signatures Handwritten signatures may only be used on handwritten, transcribed or dictated reports. Handwritten signatures aren’t valid on reports generated from an electronic health records system.
The Medicare Program Integrity Manual (Chapter 3) requires a handwritten signature be legible and include the provider’s credentials. An illegible signature is allowed when the letterhead or other information on the page indicates the identity and credential of the signer. For additional guidance, refer to the Medicare Program Integrity Manual** and the June 2018 Record article, “Medical Record Signatures: What’s acceptable?” **Blue Cross Blue Shield of Michigan doesn’t own or control this website. Update: Starting Jan. 1, 2024, all DME codes will be removed from the CareCentrix HIT and AIS programThis is an update to previous newsletter articles on this topic that ran in The Record and BCN Provider News. The articles contained three incorrect HCPCS codes. Use the following article as your reference going forward. For dates of service on or after Jan. 1, 2024, the durable medical equipment codes listed in the table below will be removed from the CareCentrix network management program for home infusion therapy and ambulatory infusion suite providers.
This change applies to:
These codes are still part of the DME benefit. Providers who participate in Blue Cross’ or BCN’s DME network can bill them in accordance with existing Blue Cross or BCN billing guidelines. Prior to Jan. 1, 2024, we’ll update the Home infusion therapy and ambulatory infusion suite provider network management: Frequently asked questions document to reflect this change. CareCentrix is an independent company that manages the in-state, independent home infusion services and ambulatory infusion center provider network for Blue Cross Blue Shield of Michigan and Blue Care Network members who have commercial plans. Northwood to manage outpatient diabetes supplies for some members, starting Jan. 1Starting Jan. 1, 2024, Northwood Inc., an independent company, will manage outpatient diabetes supplies that are covered under the medical benefit for members with:
For these members, Northwood will:
Outpatient diabetes supplies include items such as continuous glucose monitors, insulin pumps and supplies, and testing supplies. Contact Northwood starting Jan. 1 Starting Jan. 1, for diabetes supplies for Medicare Plus Blue, BCN commercial and BCN Advantage members, health care providers can call Northwood's Customer Service department at 1 800-393-6432 to locate the nearest supplier contracted with Northwood. The contracted supplier will:
Providers who currently submit orders directly to J&B Medical may continue to do so. J&B Medical is an independent company that participates in the Northwood network. Some diabetes drugs to require prior authorization for Blue Cross and BCN members, starting Jan. 1Beginning Jan. 1, 2024, the presence of prior pharmacy claims for insulin alone will no longer qualify Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members for coverage of the medications in the table listed below. We’ll require a prior authorization to confirm that the medications listed below are being used for Type 2 diabetes for members who don’t have a supporting prescription or medical record with a diabetes diagnosis. The full-coverage requirements are listed in the table below.
**Effective Jan. 1, 2024, previous trial of only insulin will no longer qualify members for coverage without prior authorization if they don’t have a medical diagnosis of Type 2 diabetes. For more information on how to submit an authorization electronically:
A complete list of included drugs and coverage requirements for all drug lists is available at bcbsm.com/druglists. Blue Cross and BCN covering additional vaccinesTo increase access to vaccines and decrease the risk of vaccine-preventable disease outbreaks, Blue Cross Blue Shield of Michigan and Blue Care Network will add the following vaccines to our list of vaccines covered under the pharmacy benefit:
For information about the procedure codes to use when billing for these vaccines, see the article “Updated COVID-19 vaccines approved by FDA,” also in this issue. Vaccine list Following is a list of all the vaccines that are covered under eligible members’ prescription drug plans. Most Blue Cross and BCN commercial (non-Medicare) members with prescription drug coverage are eligible. If a member meets the coverage criteria, the vaccine is covered with no cost sharing. Vaccines that have an age requirement
Vaccines that have no age requirement
COVID-19 vaccines
Notes:
Updated COVID-19 vaccines approved by FDAThe U.S. Food and Drug Administration recently amended the emergency use authorization of COVID-19 vaccines from Moderna,** Novavax** and Pfizer-BioNTech** to include the 2023-24 formula. Use the following procedure codes for COVID-19 monovalent vaccine administration and products: *90480, *91304, *91318, *91319, *91320, *91321 and *91322. For more information, see the following:
The vaccine administration and products are part of members’ preventive benefits. For most health plans, there’s no member cost sharing. See below for information about checking vaccine benefits for Blue Cross Blue Shield of Michigan commercial groups that may have cost sharing or may not have vaccine coverage. Blue Cross commercial groups that may have cost sharing or may not have vaccine coverage For members who have coverage through Blue Cross commercial groups that are exempt from the Patient Protection and Affordable Care Act, members may have cost sharing or they may not have vaccine coverage. Here’s how to check member eligibility and benefits for vaccines:
For more information on our vaccines, see the article “Blue Cross and BCN covering additional vaccines,” also in this issue. None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **Blue Cross Blue Shield of Michigan doesn’t own or control this website. Requirements and codes changed for some medical benefit drugsAs part of our efforts to encourage appropriate use of high-cost medications covered under the medical benefit, we recently added requirements for some medical benefit drugs. Also, the Centers for Medicare & Medicaid Services assigned some drugs new HCPCS codes. The changes went into effect on various dates in July, August and September. Changes in requirements For Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members, we added prior authorization requirements for the following:
For Medicare Plus Blue℠ and BCN Advantage℠ members, we added prior authorization requirements for the following:
Code changes The table below shows HCPCS code changes that were effective July 1, 2023, (unless otherwise noted) for medical benefit drugs we manage.
Drug lists For additional details, see the following drug lists:
These lists are also available on the following pages of the ereferrals.bcbsm.com website: More information about these requirements We communicated these changes previously through provider alerts. Those alerts contain additional details. You can view the provider alerts on ereferrals.bcbsm.com and on our Provider Resources site, which is accessible through our provider portal (availity.com).*** More information for Blue Cross commercial groups For Blue Cross commercial groups, authorization requirements apply only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. A link to this list is also available on the Blue Cross Medical Benefit Drugs page of the ereferrals.bcbsm.com website. Note: Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don't participate in the standard prior authorization program Reminder An authorization approval isn’t a guarantee of payment. As always, health care providers need to verify eligibility and benefits for members. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **May be assigned a unique code in the future. ***Blue Cross Blue Shield of Michigan and Blue Care Network doesn’t own or control this website. Starting Jan. 1, we’ll change how we cover some drugs on Clinical, Custom, Custom Select and Preferred drug listsOur goal at Blue Cross Blue Shield of Michigan and Blue Care Network is to provide our members with safe, high-quality prescription drug therapies. We continually review prescription drugs so we can provide the best value for our members, control costs and make sure our members are using the right drugs for the right situations. Starting Jan. 1, 2024, we’ll change how we cover some medications on the Clinical, Custom, Custom Select and Preferred drug lists. We’ll send letters to notify affected members, their groups and their health care providers about these changes. Drugs that won’t be covered on the Clinical, Custom and Custom Select Drug lists The drugs that won’t be covered are listed along with suggested covered preferred alternatives that have similar effectiveness, quality and safety. When pharmacies fill prescriptions with preferred alternatives, the generic equivalents are dispensed, if available. Additional coverage requirements may apply for preferred alternatives, such as prior authorization.
Drugs that will have a higher copayment on Clinical, Custom and Custom Select drug lists The brand-name drugs that will have a higher copayment are listed in the table below along with suggested covered preferred alternatives that have similar effectiveness, quality and safety. When pharmacies fill prescriptions with preferred alternatives, the generic equivalents are dispensed, if available. Additional coverage requirements may apply for preferred alternatives.
**Nonpreferred brand drugs aren’t covered for members with a closed benefit. Brand-name drugs no longer covered with generic copay on HMO Custom Drug List On some of our drug lists, select brand-name drugs are covered at a generic copay and the generic equivalent drug isn’t covered. These brand-name drugs will no longer be covered at the generic copay. Members can fill prescriptions with the generic equivalent.
Drugs that won’t be covered on the Preferred Drug List We’ll no longer cover the drugs in the table below. Unless noted, both the brand name and available generic equivalents won’t be covered. If a member fills a prescription for one of these drugs on or after Jan.1, 2024, they’ll be responsible for the full cost. The drugs that won’t be covered are listed in the table below along with suggested covered preferred alternatives that have similar effectiveness, quality and safety. When pharmacies fill prescriptions with preferred alternatives, the generic equivalents are dispensed, if available. Additional coverage requirements may apply for preferred alternatives, such as prior authorization.
Drugs that will have a higher copayment on the Preferred Drug List The brand-name drugs that will have a higher copayment are listed along with suggested covered preferred alternatives that have similar effectiveness, quality and safety. When pharmacies fill prescriptions with preferred alternatives, the generic equivalents are dispensed, if available. Additional coverage requirements may apply for preferred alternatives.
Brand-name drugs with a generic copay that won’t be covered on the Preferred Drug List On some of our drug lists, select brand-name drugs are covered at a generic copay and the generic equivalent drug isn’t covered. These brand-name drugs will no longer be covered at the generic copay. Members can fill prescriptions with the generic equivalent, and the brand-name drug will no longer be covered.
Changes coming to preferred drug designations under medical benefit for most commercial membersFor dates of service on or after Jan. 1, 2024, Blue Cross Blue Shield of Michigan and Blue Care Network are making changes to preferred drug designations for some products. In addition, providers will need to submit prior authorization requests through different systems for some preferred and nonpreferred drugs. These changes will affect:
Changes to preferred drug designations We’re changing preferred drug designations as shown in the following table. Changes are in bold text.
How existing prior authorizations are affected by these changes Existing prior authorizations are affected as follows:
Changes to prior authorization processes The following table outlines prior authorization requirements for the drugs listed above for dates of service on or after Jan. 1, 2024. To determine which Blue Cross commercial groups have opted in to the Carelon medical oncology program, see the Carelon medical oncology prior authorization program opt-in list for Blue Cross commercial self-funded groups.
Additional information For additional information on requirements related to drugs covered under the medical benefit, refer to the following drug lists:
For additional information about medical benefit drugs, see the following pages of our ereferrals.bcbsm.com website:
We’ve updated how we calculate MME measurements for certain opioidsBlue Cross Blue Shield of Michigan and Blue Care Network have updated how we calculate morphine milligram equivalents, or MME, measurements for certain opioids. The update, based on changes recommended by the Centers for Disease Control and Prevention, was effective Oct. 1. MMEs are calculations used to measure and compare different opioids, using morphine as the standard. Blue Cross requires a prior authorization for opioid dosages that exceed 90 MMEs per day. This change will only affect the opioids listed in the table below:
Members who fill hydromorphone, methadone or tramadol prescriptions may experience a claim rejection when their total daily MME exceeds the plan threshold level of 90 MME, even if the member hasn’t changed doses. The total MME of all opioids remains at 90 MME per day and won’t change. If the pharmacy receives a rejected claim due to this change, the provider will need to submit a prior authorization request attesting that the dose is medically necessary. If we don’t provide a prior authorization, members may not be able to fill the prescribed dose. For more information related to this change, refer to the Opioid National Drug Code and Oral MME Conversion File Update** on the CDC website. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Lumoxiti no longer requires prior authorizationLumoxiti™ (moxetumomab pasudotox-tdfk), HCPCS code J9313, no longer requires prior authorization through Carelon Medical Benefits Management (formerly known as AIM Specialty Health®). This change applies to the following members for dates of service on or after Sept. 30, 2023:
This drug is covered under members’ medical benefits, not their pharmacy benefits. More about prior authorization requirements For information on requirements related to drugs covered under the medical benefit, refer to the following drug lists:
Blue Cross commercial and BCN commercial: URMBT members with Blue Cross non-Medicare plans: Medicare Plus Blue and BCN Advantage members: Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services.
Beyfortus to have quantity limits for commercial members, starting Jan. 1Starting Jan. 1, 2024, Beyfortus™ (nirsevimab-alip), procedure codes *90380 and *90381, will have quantity limits when billed under the pharmacy benefit. There won’t be quantity limits when Beyfortus is billed under the medical benefit. Note: For the administration of Beyfortus, use procedure codes *96380 and *96381. Administration site and coverage details Beyfortus is covered as follows.
Blue Cross commercial groups that may have cost sharing or may not have vaccine coverage For members who have coverage through Blue Cross Blue Shield of Michigan commercial groups that are exempt from the Patient Protection and Affordable Care Act, members may have cost sharing or they may not have vaccine coverage. Here’s how to check member eligibility and benefits for vaccines:
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Zynyz to require prior authorization for most members, starting Dec. 10For dates of service on or after Dec. 10, 2023, Zynyz™ (retifanlimab-dlwr), HCPCS code J9345, will require prior authorization through Carelon Medical Benefits Management (formerly known as AIM Specialty Health®). The drug is covered under the members’ medical benefits, not their pharmacy benefits. Prior authorization requirements apply when the drug is administered in outpatient settings for:
How to submit authorization requests Submit authorization requests to Carelon using one of the following methods:
More about the prior authorization requirements For additional information on requirements related to drugs covered under the medical benefit, refer to the following drug lists:
We’ll update the pertinent drug lists to reflect the information in this message prior to the effective date. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Starting Jan.1, prior authorization no longer required for some proceduresFor dates of service on or after Jan. 1, 2024, the following procedures will no longer require prior authorization. Note: For dates of service before Jan. 1, these procedures require prior authorization by Medicare Plus Blue℠ and BCN Utilization Management.
Prior to Jan. 1, we’ll update lists of procedure codes that require prior authorization. Prior to Jan. 1, we’ll update lists of procedure codes that require prior authorization.
Here’s an update on high-intensity in-home care program through LandmarkWe’ve communicated extensively about the Landmark high-intensity in-home health care program in The Record over the past two years. This month, we want to bring you a quick overview of the program, along with a look at some of our program outcomes and what members are saying about the program. Background Blue Cross Blue Shield of Michigan and Blue Care Network launched the Landmark high-intensity in-home care program in late 2021 for eligible members in Southeast Michigan with coverage through a group customer. The program was expanded in phases and, since January 2023, it’s available to all eligible Medicare Plus Blue℠ and BCN Advantage℠ members who reside in Michigan’s Lower Peninsula. Blue Cross and BCN offer this program as a benefit for our most at-risk members. This additional in-home support is also something employer groups have requested to help improve quality of life and health outcomes. To be eligible for the Landmark program, members must have multiple chronic conditions and take a high number of prescription medications. Currently, approximately 15% of Blue Cross and BCN’s Medicare Advantage members are eligible. How the Landmark program works Using a physician-led, interdisciplinary team, the Landmark program complements office-based primary care by:
The Landmark program provides supplemental support and reinforces the primary care provider’s plan of care for chronic condition management. It doesn’t replace a member’s primary care provider, and members don’t become attributed or assigned to Landmark. Because the Landmark program is part of members’ benefits, eligible members can choose whether they want to participate. Program outcomes We’re beginning to see the benefits of the Landmark program on this vulnerable member population. Early data from the initial phase of the program has shown the following for engaged members:
Collaborating with physician organizations Landmark has built collaborative relationships with a number of physician organizations and is willing to adapt processes and communication methods to best meet the unique needs of each physician organization. At a recent Physician Group Incentive Program meeting, Sparrow Care Network shared details of how they’re working with Landmark to build a successful collaboration, despite initial concerns from Sparrow providers about the program. The working relationship is being customized to fit into Sparrow’s overall Population Health Service Organization and requires engagement from clinical and operational teams from both organizations. Sparrow care managers also play a significant role in ensuring communication flows appropriately in both directions. Sparrow has expressed appreciation for Landmark’s flexibility and responsiveness and continues to collaborate on achieving the best care outcomes for patients. What members are saying about the Landmark program Here are several comments from Blue Cross and BCN members who are engaged in the Landmark program: “I was in need of some help. My doctor wasn't available. Erica (nurse practitioner) arrived within a few hours. Erica was very friendly and professional. I am grateful for her help.” “Wonderful experience. Very professional, but very caring. Very nice to have medical service at home.” “The nurses have been very good about responding to me when I get sick or fall. I'm grateful they're included in my insurance plan.” “My father received excellent and immediate care in his home when his cold became more serious with shortness of breath, fever and productive cough. I was able to talk with the clinician by phone during the visit and all our concerns were addressed. Follow-up care was also excellent.” “Great program for keeping my health at its best.” How to learn more To learn more about our program with Landmark, see the High-intensity in-home care program: Frequently asked questions for providers document. If you have questions about the program, email the Blue Cross Care Delivery Solutions team at CareDeliverySolutionsProgramMtg@bcbsm.com. To coordinate directly with Landmark regarding patient care, call Landmark at 313-241-5242. Landmark Health LLC is an independent company that provides in-home care services for Blue Cross Blue Shield of Michigan and Blue Care Network members who have Medicare Advantage plans.
Newly enrolled PAs and NPs required to identify their work settings to help avoid payment issuesWhat you need to know This requirement applies to newly enrolled physician assistants and nurse practitioners only. Work setting information for PAs and NPs enrolled prior to Nov. 10 will be updated automatically — there’s no action required. Starting Nov. 10, 2023, newly enrolled physician assistants and nurse practitioners will be required to identify their work settings (primary care or specialty care) on our provider enrollment and change forms. This information is necessary to help ensure that withholds can be accurately applied and that payment issues can be resolved for PAs and NPs covering for physician specialists or primary care physicians. The following provider enrollment and change forms have been updated to include work setting:
Provider enrollment and change forms can be found in the Enrollment section of bcbsm.com/providers.
Update: TurningPoint medical policies for musculoskeletal and pain management proceduresIn an article in the September Record and the September-October BCN Provider News, we reported that Blue Cross Blue Shield of Michigan, Blue Care Network and TurningPoint Healthcare Solutions LLC added and updated TurningPoint medical policies for musculoskeletal and pain management procedures. The newsletter articles linked to a provider alert for details. We’re letting you know that we updated the provider alert to:
View the updated provider alert for full details. TurningPoint Healthcare Solutions LLC is an independent company that manages authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Reminder: Independent labs must provide advance notice to Blue Cross commercial members before providing noncovered servicesHere’s information you need to know about providing noncovered services to Blue Cross Blue Shield of Michigan commercial members at outpatient laboratories. Independent laboratories Before receiving noncovered services at independent laboratories, Blue Cross commercial members must sign the Advance Notice of Member Responsibility form. Prior to having members sign the form, be sure to familiarize yourself with the requirements under our Clinical Laboratory Agreement. The language in this agreement states that independent laboratories may bill members for services that Blue Cross has deemed to be not medically necessary only when all of the following are true:
To access the Advance Notice of Member Responsibility form:
Hospital laboratories The Advance Notice of Member Responsibility form isn’t approved for use by hospital labs at this time. We’re currently reviewing the processes for hospital labs. Watch for an upcoming provider alert and Record article with more information. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Here’s information and resources to share with patients about flu vaccineThis is part of an ongoing series of articles focusing on the tools and resources available to help FEP members manage their health. With flu season in full swing, we wanted to make sure you have the resources you need to help encourage your patients to get the flu shot. Here are some resources from the Centers for Disease Control and Prevention:
Encouraging patients with chronic conditions to get the flu vaccine is especially important but can sometimes be challenging. The following are flyers you can share with patients:
For more information on Blue Cross and Blue Shield Federal Employee Program® benefits and resources, members and health care providers can call Customer Service at 1-800-482-3600 or go to fepblue.org. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
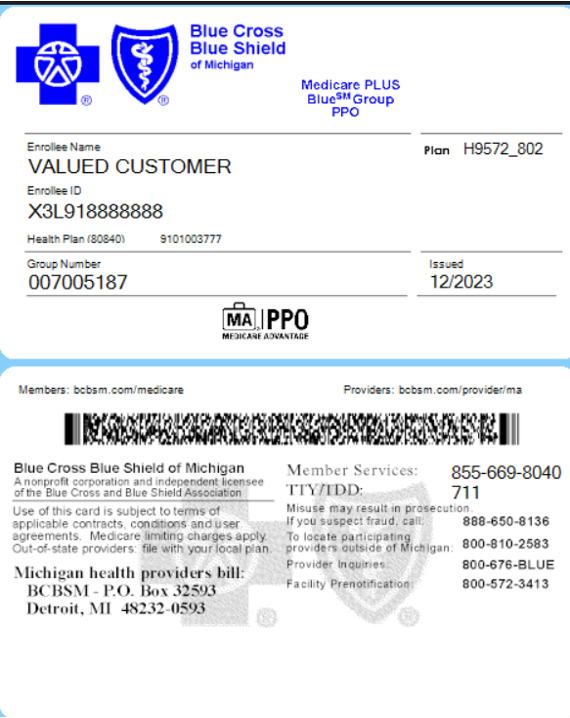
University of Michigan retirees can join our Medicare Advantage plans, effective Jan. 1University of Michigan retirees can choose either our Medicare Plus Blue℠ or BCN Advantage℠ plan, effective Jan. 1, 2024. These plans provide coverage for medical and surgical benefits. Magellan Rx, an independent company, administers the group’s prescription drug benefits. How to recognize a U-M Medicare Advantage member U-M retirees with Medicare Plus Blue plans will have Blue Cross Blue Shield of Michigan identification cards that indicate “Medicare Plus Blue Group PPO.” The group number is 007005187 and the alphanumeric prefix of the enrollee ID is X3L See sample ID card below:
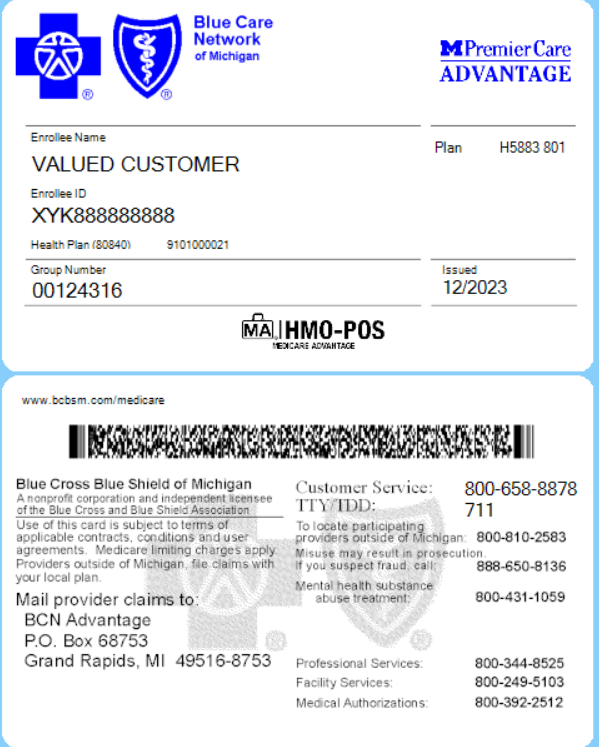
The U-M BCN Advantage plan is called U-M PremierCare Advantage, and the logo will be displayed at the top right. The ID card will indicate Blue Care Network of Michigan at the top left. The group number is 00124316, and the enrollee ID number will have an alpha prefix of XYK. The HMO-POS logo next to the MA suitcase image at the bottom center shows that members have a point-of-service option. See sample ID card below:
Note: Providers should verify eligibility and coverage at every visit. To verify eligibility and check coverage, log in to our provider portal, Availity Essentials, at availity.com.** Enhanced benefits U-M Medicare Advantage members have some additional enhanced benefits not available to other groups. Visit Medicare Plus Blue PPO Enhanced Benefits Policies or BCN Advantage Enhanced Benefits Policies for more information. What to know about prior authorization Like our other Medicare Advantage plans, U-M Medicare Advantage benefits require prior authorization for all acute inpatient admissions and specified high-tech radiology services. Prior authorization is also required for skilled nursing, long-term acute care and inpatient rehabilitation admissions. For information about prior authorization requirements, refer to the appropriate provider manual listed below: Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Updated on-demand training available: e-referral, risk adjustment, ICD-10-CM codingAction item Visit our provider training site to find updated resources on topics that are important to your role. Provider Experience continues to offer training resources for health care providers and staff. Our on-demand courses are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network. We recently updated the following learning opportunities:
The goal of our provider training site is to enhance the training experience for health care providers and staff. Check out the dashboard regularly for announcements as we add more courses, including those with CME offerings. To request access to the training site, complete the following steps:
If you need assistance creating your login ID or navigating the site, contact ProviderTraining@bcbsm.com.
Lunch and learn webinars for physicians and coders focus on risk adjustment, codingAs a reminder, we’re offering live, 30-minute educational webinars that provide updated information on documentation and coding for common challenging diagnoses. Webinars also include an opportunity to ask questions. Here’s our upcoming schedule and tentative topics for the webinars. Each session starts at noon Eastern time. Log in to the provider training website to register for sessions that work with your schedule.
Registering for the provider training website If you haven’t already registered for the provider training website, follow these steps:
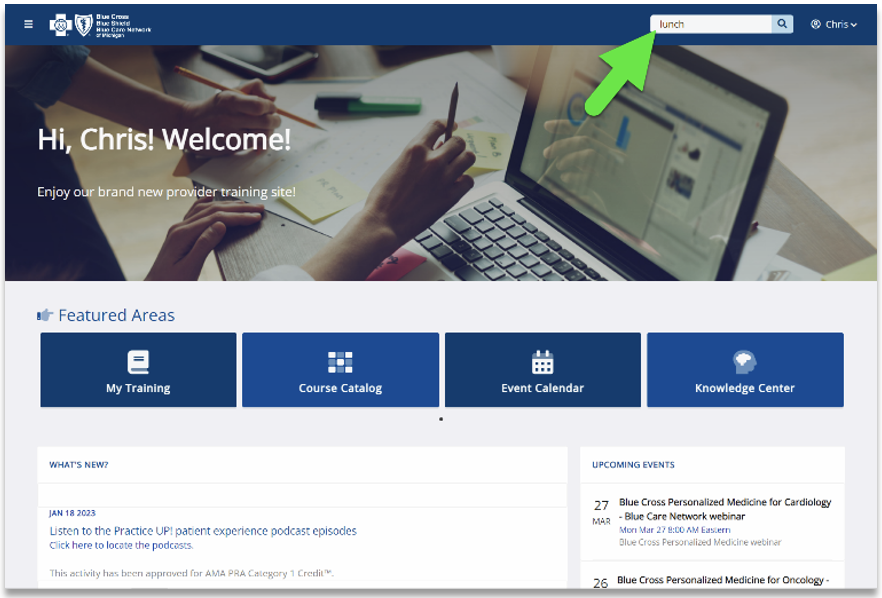
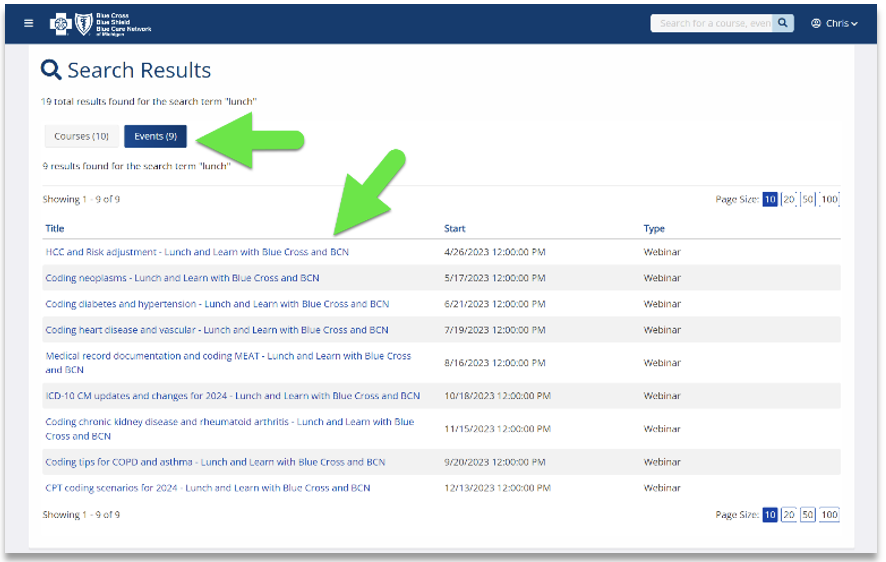
Locating a session Click here if you’re already registered for the provider training website. On the provider training website, look in the Event Calendar or use the search feature using the keyword “lunch” to quickly locate all 2023 sessions. See the screenshots below for more details.
Previous sessions You can also listen to previously recorded sessions. Check out the following:
For more information If you have any questions about the sessions, contact April Boyce at aboyce@bcbsm.com. If you have questions regarding a session or website registration, email ProviderTraining@bcbsm.com.
New enhanced benefits will be available to Medicare Advantage members in 2024Medicare Plus Blue℠ and BCN Advantage℠ are adding three new enhanced benefits to their comprehensive Medicare Advantage plans for the 2024 plan year. Beginning Jan. 1, 2024, members can capitalize on the following new benefits:
Note: Check your patient’s eligibility and benefits in our provider portal (availity.com)** to verify coverage for these new benefits. Details on new enhanced benefits Ambulance services without transport: Currently, if a member or another person calls for an ambulance for a member’s health emergency, and the member isn’t transported, the service isn’t covered. Beginning Jan. 1, 2024, if the ambulance providers are able to stabilize the member at the current location without transporting to a facility, the plan covers the services with the applicable cost sharing. This service isn’t covered outside of the U.S. or its territories. Enhanced annual wellness visit: After having Medicare Part B for longer than 12 months, members can get an annual wellness visit every 12 months. The annual wellness visit:
No cost sharing applies for this benefit. Mobile crisis and crisis stabilization for behavioral health: This benefit offers improved care for people experiencing a behavioral health crisis. Services include mobile crisis intervention by eligible providers through telehealth or face-to-face, on-site services and crisis stabilization. Members can be treated at their home or another location, and at participating outpatient psychiatric centers available in certain counties in Michigan. Cost sharing applies for these services. For more information on crisis care services and locations, visit our crisis care webpage. Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Know guidelines for trauma activation billing and reimbursementBlue Cross Blue Shield of Michigan and Blue Care Network follow the National Uniform Billing Committee rules for billing and reimbursing trauma activation charges. Effective immediately, Blue Cross and BCN won’t reimburse providers for trauma activation charges when they’re billed outside of the NUBC guidelines on inpatient facility claims. This rule applies to all claims submitted for Blue Cross commercial and BCN commercial members. This reimbursement policy isn’t intended to affect patient care. Health care providers are expected to apply medical judgment when caring for all members. Here’s how to bill trauma activation under NUBC guidelines:
In addition to NUBC guidance for appropriately billing trauma activation, there’s also trauma activation criteria set forth by the American College of Surgeons. Apply the ACS criteria in the prehospital setting to identify trauma patients who would benefit most from the highest level of trauma activation. The minimum criteria to activate the highest level of trauma activation is based on ACS 2022 updates to Resources for Optimal Care of the Injured Patient.** It includes one or more of the following:
Revenue code 068X is only permitted for reporting trauma activation charges, and trauma centers and hospitals must be licensed, designated or authorized by the state. The revenue code a facility may bill is determined by the ACS designation. See table below for details:
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
We’re making some changes in behavioral health processes beginning Jan. 1What you need to know New Directions, now known as Lucet, won’t handle requests for Blue Cross Blue Shield of Michigan commercial members related to dates of service before Jan. 1, 2024, a change from what was originally published. Submit requests for prior authorization, continued stay reviews and appeals related to dates of service before Jan. 1, 2024, using one of these methods:
When contacting Blue Cross by email or phone, you’ll need to provide the following:
We communicated in previous articles that starting Jan. 1, 2024, Blue Cross Blue Shield of Michigan and Blue Care Network will consolidate the prior authorization and case management functions for behavioral health services, including treatment for autism. This will affect all members covered by Blue Cross commercial, Medicare Plus Blue℠, BCN commercial and BCN Advantage℠ plans, except those in certain employer groups. Refer to the Mental Health and Substance Use Disorder Carve-Out List for more information. The programs are called:
These programs will align and standardize prior authorization and case management functions for Blue Cross and BCN members. We expect this consistency across lines of business to simplify processes for health care providers. Consistent processes The main benefit for providers is consistency across all lines of business. For example, for dates of service on or after Jan. 1, 2024:
FAQ document We’ve published the Blue Cross Behavioral Health: Frequently asked questions for providers document, which contains many details you’ll need to know. In the FAQ document, you’ll find important information that will help you navigate this change, including how to submit requests for prior authorization, continued stay reviews and appeals for all dates of service. We’ll update the FAQ document with additional information as it becomes available. Key change for Blue Cross commercial prior authorization requests Starting Jan. 1, 2024, New Directions, now known as Lucet, won’t handle requests for Blue Cross commercial members with dates of service on or after Jan. 1, 2024. Also, Lucet won’t handle requests related to dates of service before Jan. 1, 2024, a change from what was originally published. For Blue Cross commercial members, submit requests for prior authorization, continued stay reviews and appeals related to dates of service before Jan. 1, 2024, using one of these methods:
When you email or call, provide:
Medical necessity criteria For dates of service on or after Jan. 1, 2024, Blue Cross Behavioral Health will use the following to make determinations on prior authorization requests:
Later in 2023, you’ll be able to access these criteria on our Services That Need Prior Authorization webpage at bcbsm.com. Appeals process Starting in 2024, the addresses for submitting appeals of prior authorization requests that aren’t approved will change. Refer to the determination letters for the addresses. Training We’ll offer training for providers to learn how to access and use the new provider portal to submit prior authorization requests. Watch for more information.
Washtenaw County Community Mental Health joins crisis services programWashtenaw County Community Mental Health is the newest organization to join Blue Cross Blue Shield of Michigan’s crisis services program. It offers both mobile crisis and residential crisis services. For mobile crisis services or to determine the location of the appropriate facility for the member, call 734-544-3050. Our crisis services program was designed to offer our members (and their family members) a wider array of care options if they’re experiencing a mental health crisis. To learn more about the program and to see a list of other participating facilities, visit the Crisis Care section of our behavioral health website. Reminder: Signature required on medical recordsWhat you need to know Medical records require a provider’s signature. This article reviews what constitutes acceptable electronic and handwritten signatures.
A signature is mandatory on medical records to identify who provided services for the patient. It also validates the services were documented, reviewed and authenticated by the provider. Requirements for an acceptable signature depend on whether the medical record is generated by an electronic health record or is handwritten. Services performed by nonphysician practitioners who require physician supervision must be signed by the overseeing provider. Examples of services requiring a supervising physician signature include therapeutic and behavioral health. This includes providers supervising licensed social workers, behavioral health therapists, massage therapists and registered nurses performing administration of drugs. Electronic signatures Electronic signatures must be generated by encrypted or password-protected software and used solely by the author of the report or record. The Medicare Integrity Manual (Ch. 3, 3.3.2.4) states: “Providers using electronic systems need to recognize that there is a potential for misuse or abuse with alternate signature methods. For example, providers need a system and software products that are protected against modification, etc., and should apply adequate administrative procedures that correspond to recognized standards and laws. The individual whose name is on the alternate signature method and the provider bear the responsibility for the authenticity of the information for which an attestation has been provided. Physicians are encouraged to check with their attorneys and malpractice insurers concerning the use of alternative signature methods.” Electronic signatures must contain the following key elements:
Acceptable attestation statements include the following:
Example (electronic signature and attestation statement):
Unacceptable electronic signatures include the following:
Examples:
Handwritten signatures Handwritten signatures may only be used on handwritten, transcribed or dictated reports. Handwritten signatures aren’t valid on reports generated from an electronic health records system.
The Medicare Program Integrity Manual (Chapter 3) requires a handwritten signature be legible and include the provider’s credentials. An illegible signature is allowed when the letterhead or other information on the page indicates the identity and credential of the signer. For additional guidance, refer to the Medicare Program Integrity Manual** and the June 2018 Record article, “Medical Record Signatures: What’s acceptable?” **Blue Cross Blue Shield of Michigan doesn’t own or control this website. Update: Starting Jan. 1, 2024, all DME codes will be removed from the CareCentrix HIT and AIS programThis is an update to previous newsletter articles on this topic that ran in The Record and BCN Provider News. The articles contained three incorrect HCPCS codes. Use the following article as your reference going forward. For dates of service on or after Jan. 1, 2024, the durable medical equipment codes listed in the table below will be removed from the CareCentrix network management program for home infusion therapy and ambulatory infusion suite providers.
This change applies to:
These codes are still part of the DME benefit. Providers who participate in Blue Cross’ or BCN’s DME network can bill them in accordance with existing Blue Cross or BCN billing guidelines. Prior to Jan. 1, 2024, we’ll update the Home infusion therapy and ambulatory infusion suite provider network management: Frequently asked questions document to reflect this change. CareCentrix is an independent company that manages the in-state, independent home infusion services and ambulatory infusion center provider network for Blue Cross Blue Shield of Michigan and Blue Care Network members who have commercial plans. Northwood to manage outpatient diabetes supplies for some members, starting Jan. 1Starting Jan. 1, 2024, Northwood Inc., an independent company, will manage outpatient diabetes supplies that are covered under the medical benefit for members with:
For these members, Northwood will:
Outpatient diabetes supplies include items such as continuous glucose monitors, insulin pumps and supplies, and testing supplies. Contact Northwood starting Jan. 1 Starting Jan. 1, for diabetes supplies for Medicare Plus Blue, BCN commercial and BCN Advantage members, health care providers can call Northwood's Customer Service department at 1 800-393-6432 to locate the nearest supplier contracted with Northwood. The contracted supplier will:
Providers who currently submit orders directly to J&B Medical may continue to do so. J&B Medical is an independent company that participates in the Northwood network. Some diabetes drugs to require prior authorization for Blue Cross and BCN members, starting Jan. 1Beginning Jan. 1, 2024, the presence of prior pharmacy claims for insulin alone will no longer qualify Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members for coverage of the medications in the table listed below. We’ll require a prior authorization to confirm that the medications listed below are being used for Type 2 diabetes for members who don’t have a supporting prescription or medical record with a diabetes diagnosis. The full-coverage requirements are listed in the table below.
**Effective Jan. 1, 2024, previous trial of only insulin will no longer qualify members for coverage without prior authorization if they don’t have a medical diagnosis of Type 2 diabetes. For more information on how to submit an authorization electronically:
A complete list of included drugs and coverage requirements for all drug lists is available at bcbsm.com/druglists. Updated COVID-19 vaccines approved by FDAThe U.S. Food and Drug Administration recently amended the emergency use authorization of COVID-19 vaccines from Moderna,** Novavax** and Pfizer-BioNTech** to include the 2023-24 formula. Use the following procedure codes for COVID-19 monovalent vaccine administration and products: *90480, *91304, *91318, *91319, *91320, *91321 and *91322. For more information, see the following:
The vaccine administration and products are part of members’ preventive benefits. For most health plans, there’s no member cost sharing. See below for information about checking vaccine benefits for Blue Cross Blue Shield of Michigan commercial groups that may have cost sharing or may not have vaccine coverage. Blue Cross commercial groups that may have cost sharing or may not have vaccine coverage For members who have coverage through Blue Cross commercial groups that are exempt from the Patient Protection and Affordable Care Act, members may have cost sharing or they may not have vaccine coverage. Here’s how to check member eligibility and benefits for vaccines:
For more information on our vaccines, see the article “Blue Cross and BCN covering additional vaccines,” also in this issue. None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **Blue Cross Blue Shield of Michigan doesn’t own or control this website. Requirements and codes changed for some medical benefit drugsAs part of our efforts to encourage appropriate use of high-cost medications covered under the medical benefit, we recently added requirements for some medical benefit drugs. Also, the Centers for Medicare & Medicaid Services assigned some drugs new HCPCS codes. The changes went into effect on various dates in July, August and September. Changes in requirements For Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members, we added prior authorization requirements for the following:
For Medicare Plus Blue℠ and BCN Advantage℠ members, we added prior authorization requirements for the following:
Code changes The table below shows HCPCS code changes that were effective July 1, 2023, (unless otherwise noted) for medical benefit drugs we manage.
Drug lists For additional details, see the following drug lists:
These lists are also available on the following pages of the ereferrals.bcbsm.com website: More information about these requirements We communicated these changes previously through provider alerts. Those alerts contain additional details. You can view the provider alerts on ereferrals.bcbsm.com and on our Provider Resources site, which is accessible through our provider portal (availity.com).*** More information for Blue Cross commercial groups For Blue Cross commercial groups, authorization requirements apply only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. A link to this list is also available on the Blue Cross Medical Benefit Drugs page of the ereferrals.bcbsm.com website. Note: Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don't participate in the standard prior authorization program Reminder An authorization approval isn’t a guarantee of payment. As always, health care providers need to verify eligibility and benefits for members. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **May be assigned a unique code in the future. ***Blue Cross Blue Shield of Michigan and Blue Care Network doesn’t own or control this website. ***Blue Cross Blue Shield of Michigan and Blue Care Network doesn’t own or control this website. Starting Jan. 1, we’ll change how we cover some drugs on Clinical, Custom, Custom Select and Preferred drug listsOur goal at Blue Cross Blue Shield of Michigan and Blue Care Network is to provide our members with safe, high-quality prescription drug therapies. We continually review prescription drugs so we can provide the best value for our members, control costs and make sure our members are using the right drugs for the right situations. Starting Jan. 1, 2024, we’ll change how we cover some medications on the Clinical, Custom, Custom Select and Preferred drug lists. We’ll send letters to notify affected members, their groups and their health care providers about these changes. Drugs that won’t be covered on the Clinical, Custom and Custom Select Drug lists The drugs that won’t be covered are listed along with suggested covered preferred alternatives that have similar effectiveness, quality and safety. When pharmacies fill prescriptions with preferred alternatives, the generic equivalents are dispensed, if available. Additional coverage requirements may apply for preferred alternatives, such as prior authorization.
Drugs that will have a higher copayment on Clinical, Custom and Custom Select drug lists The brand-name drugs that will have a higher copayment are listed in the table below along with suggested covered preferred alternatives that have similar effectiveness, quality and safety. When pharmacies fill prescriptions with preferred alternatives, the generic equivalents are dispensed, if available. Additional coverage requirements may apply for preferred alternatives.
**Nonpreferred brand drugs aren’t covered for members with a closed benefit. Brand-name drugs no longer covered with generic copay on HMO Custom Drug List On some of our drug lists, select brand-name drugs are covered at a generic copay and the generic equivalent drug isn’t covered. These brand-name drugs will no longer be covered at the generic copay. Members can fill prescriptions with the generic equivalent.
Drugs that won’t be covered on the Preferred Drug List We’ll no longer cover the drugs in the table below. Unless noted, both the brand name and available generic equivalents won’t be covered. If a member fills a prescription for one of these drugs on or after Jan.1, 2024, they’ll be responsible for the full cost. The drugs that won’t be covered are listed in the table below along with suggested covered preferred alternatives that have similar effectiveness, quality and safety. When pharmacies fill prescriptions with preferred alternatives, the generic equivalents are dispensed, if available. Additional coverage requirements may apply for preferred alternatives, such as prior authorization.
Drugs that will have a higher copayment on the Preferred Drug List The brand-name drugs that will have a higher copayment are listed along with suggested covered preferred alternatives that have similar effectiveness, quality and safety. When pharmacies fill prescriptions with preferred alternatives, the generic equivalents are dispensed, if available. Additional coverage requirements may apply for preferred alternatives.
Brand-name drugs with a generic copay that won’t be covered on the Preferred Drug List On some of our drug lists, select brand-name drugs are covered at a generic copay and the generic equivalent drug isn’t covered. These brand-name drugs will no longer be covered at the generic copay. Members can fill prescriptions with the generic equivalent, and the brand-name drug will no longer be covered.
Changes coming to preferred drug designations under medical benefit for most commercial membersFor dates of service on or after Jan. 1, 2024, Blue Cross Blue Shield of Michigan and Blue Care Network are making changes to preferred drug designations for some products. In addition, providers will need to submit prior authorization requests through different systems for some preferred and nonpreferred drugs. These changes will affect:
Changes to preferred drug designations We’re changing preferred drug designations as shown in the following table. Changes are in bold text.
How existing prior authorizations are affected by these changes Existing prior authorizations are affected as follows:
Changes to prior authorization processes The following table outlines prior authorization requirements for the drugs listed above for dates of service on or after Jan. 1, 2024. To determine which Blue Cross commercial groups have opted in to the Carelon medical oncology program, see the Carelon medical oncology prior authorization program opt-in list for Blue Cross commercial self-funded groups.
Additional information For additional information on requirements related to drugs covered under the medical benefit, refer to the following drug lists:
For additional information about medical benefit drugs, see the following pages of our ereferrals.bcbsm.com website:
Lumoxiti no longer requires prior authorizationLumoxiti™ (moxetumomab pasudotox-tdfk), HCPCS code J9313, no longer requires prior authorization through Carelon Medical Benefits Management (formerly known as AIM Specialty Health®). This change applies to the following members for dates of service on or after Sept. 30, 2023:
This drug is covered under members’ medical benefits, not their pharmacy benefits. More about prior authorization requirements For information on requirements related to drugs covered under the medical benefit, refer to the following drug lists:
Blue Cross commercial and BCN commercial: URMBT members with Blue Cross non-Medicare plans: Medicare Plus Blue and BCN Advantage members: Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services.
Beyfortus to have quantity limits for commercial members, starting Jan. 1Starting Jan. 1, 2024, Beyfortus™ (nirsevimab-alip), procedure codes *90380 and *90381, will have quantity limits when billed under the pharmacy benefit. There won’t be quantity limits when Beyfortus is billed under the medical benefit. Note: For the administration of Beyfortus, use procedure codes *96380 and *96381. Administration site and coverage details Beyfortus is covered as follows.
Blue Cross commercial groups that may have cost sharing or may not have vaccine coverage For members who have coverage through Blue Cross Blue Shield of Michigan commercial groups that are exempt from the Patient Protection and Affordable Care Act, members may have cost sharing or they may not have vaccine coverage. Here’s how to check member eligibility and benefits for vaccines:
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Zynyz to require prior authorization for most members, starting Dec. 10For dates of service on or after Dec. 10, 2023, Zynyz™ (retifanlimab-dlwr), HCPCS code J9345, will require prior authorization through Carelon Medical Benefits Management (formerly known as AIM Specialty Health®). The drug is covered under the members’ medical benefits, not their pharmacy benefits. Prior authorization requirements apply when the drug is administered in outpatient settings for:
How to submit authorization requests Submit authorization requests to Carelon using one of the following methods:
More about the prior authorization requirements For additional information on requirements related to drugs covered under the medical benefit, refer to the following drug lists:
We’ll update the pertinent drug lists to reflect the information in this message prior to the effective date. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Facilities must submit appeals within required time framesWhat you need to know
Facilities must submit appeals of nonapproved inpatient medical and surgical (non-behavioral health) prior authorization requests within the time frames stated in the denial letters. We reinstated the usual appeals time frames on July 1 During the COVID-19 public health emergency, Blue Cross Blue Shield of Michigan and Blue Care Network waived the time frames for submitting appeals. We reinstated the time frames for submitting appeals, starting July 1, 2023. This was communicated in a May 1, 2023, provider alert. Time frames for submitting appeals Here are the time frames for submitting appeals of inpatient medical and surgical (non‑behavioral health) prior authorization requests that we’ve denied:
Where to find additional information For additional information about submitting appeals of prior authorization requests that aren’t approved, refer to the pertinent provider manual:
To access the provider manuals:
Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Update: TurningPoint medical policies for musculoskeletal and pain management proceduresIn an article in the September Record and the September-October BCN Provider News, we reported that Blue Cross Blue Shield of Michigan, Blue Care Network and TurningPoint Healthcare Solutions LLC added and updated TurningPoint medical policies for musculoskeletal and pain management procedures. The newsletter articles linked to a provider alert for details. We’re letting you know that we updated the provider alert to:
View the updated provider alert for full details. TurningPoint Healthcare Solutions LLC is an independent company that manages authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Reminder: Independent labs must provide advance notice to Blue Cross commercial members before providing noncovered servicesHere’s information you need to know about providing noncovered services to Blue Cross Blue Shield of Michigan commercial members at outpatient laboratories. Independent laboratories Before receiving noncovered services at independent laboratories, Blue Cross commercial members must sign the Advance Notice of Member Responsibility form. Prior to having members sign the form, be sure to familiarize yourself with the requirements under our Clinical Laboratory Agreement. The language in this agreement states that independent laboratories may bill members for services that Blue Cross has deemed to be not medically necessary only when all of the following are true:
To access the Advance Notice of Member Responsibility form:
Hospital laboratories The Advance Notice of Member Responsibility form isn’t approved for use by hospital labs at this time. We’re currently reviewing the processes for hospital labs. Watch for an upcoming provider alert and Record article with more information. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Update: Starting Jan. 1, 2024, all DME codes will be removed from the CareCentrix HIT and AIS programThis is an update to previous newsletter articles on this topic that ran in The Record and BCN Provider News. The articles contained three incorrect HCPCS codes. Use the following article as your reference going forward. For dates of service on or after Jan. 1, 2024, the durable medical equipment codes listed in the table below will be removed from the CareCentrix network management program for home infusion therapy and ambulatory infusion suite providers.
This change applies to:
These codes are still part of the DME benefit. Providers who participate in Blue Cross’ or BCN’s DME network can bill them in accordance with existing Blue Cross or BCN billing guidelines. Prior to Jan. 1, 2024, we’ll update the Home infusion therapy and ambulatory infusion suite provider network management: Frequently asked questions document to reflect this change. CareCentrix is an independent company that manages the in-state, independent home infusion services and ambulatory infusion center provider network for Blue Cross Blue Shield of Michigan and Blue Care Network members who have commercial plans. Northwood to manage outpatient diabetes supplies for some members, starting Jan. 1Starting Jan. 1, 2024, Northwood Inc., an independent company, will manage outpatient diabetes supplies that are covered under the medical benefit for members with:
For these members, Northwood will:
Outpatient diabetes supplies include items such as continuous glucose monitors, insulin pumps and supplies, and testing supplies. Contact Northwood starting Jan. 1 Starting Jan. 1, for diabetes supplies for Medicare Plus Blue, BCN commercial and BCN Advantage members, health care providers can call Northwood's Customer Service department at 1 800-393-6432 to locate the nearest supplier contracted with Northwood. The contracted supplier will:
Providers who currently submit orders directly to J&B Medical may continue to do so. J&B Medical is an independent company that participates in the Northwood network. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||