Subscribe | The Record Archive | Contacts | bcbsm.com
|
January 2023
Follow these tips for checking claim status and viewing remittance advices and vouchers in Availity
Checking claim status Click on Claims & Payments and then click on Claim Status. If you have more than one organization, select the appropriate one, then select BCBS MICHIGAN AND BLUE CARE NETWORK as the payer. Next, follow these steps:
Tip: Allow at least 72 hours for the claim to be processed before checking its status. Tip: For Federal Employee Program® contracts or contracts from non-Michigan Blue plans, start with the HIPAA Standard tab. Using the Remittance Viewer in Availity Click on Claims & Payments and then click on Remittance Viewer twice. Tip: When you open the Remittance Viewer, you’ll see a pop-up screen titled Welcome to Remittance Viewer with a link at the bottom to a demo for using the tool. The Remittance Viewer screen has two tabs:
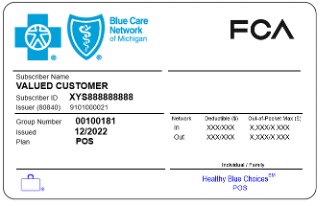
Tip: Make sure the date span is correct for the search option you use. With the Check/EFT tab, it’s best to search for a couple of days before and after the check date. Tip: When you find results, you’ll see a row of data. On the right, there will be an Actions column. One of the items is labeled EOP/EOB when you hover your mouse over it. This is the voucher you’re used to seeing in Provider Secured Services/web-DENIS. Another item is labeled Download when you hover your mouse over it. This is the electronic remittance advice that you can download as a PDF. Submitting claims through the Availity Claim Submission tool If you use Availity’s Claims Submission tool to submit claims to Blue Cross Blue Shield of Michigan and Blue Care Network, you need to make sure the member prefix is included with the member contract number on your claim. The prefix is usually three alpha characters preceding the nine-digit contract number. Federal Employee Program contract numbers are an exception, with an R followed by an eight-digit contract number. In some cases, when you search for a Blue Cross or BCN member within Availity, the results don’t display the contract prefix. If you submit a claim that doesn’t include the prefix, the claim will reject due to an incomplete or invalid contract number. To find the prefix, look up the patient in Availity’s Eligibility and Benefits Inquiry tool (found under the Patient Registration dropdown) and click on View Member ID Card near the top of the results page. The ID card image will include the complete contract number (called the Subscriber ID), including the prefix. Training assistance Here’s where you can learn more.
Troubleshooting If you’re having problems checking claim status or using the Remittance Viewer, ask your Availity administrator to make sure you have the claim status role assigned to you. Contact Availity Client Services for one-on-one assistance by calling 1-800-AVAILITY (282-4548) from 8 a.m. to 8 p.m. Eastern time, Monday through Friday (excluding holidays). Request an ACS ticket number for reference in case this call doesn’t resolve your problem and you need follow-up assistance. Still need to register? Find out how at Register for Availity Essentials.** Learn more at Get Started with Availity Essentials.** Have you been surprised by a paper check when you expected electronic payment? If you submit a claim with a tax ID that doesn’t match what we have in our system for electronic funds transfer, or EFT, the claim will pay by paper check instead of EFT. Review your recent vouchers that were paid via EFT to note the tax ID. If you need to revise your EFT information, check out EFT training within the Availity Learning Center or in the Get Up to Speed with Training** website, or call 1-800-AVAILITY (282-4548), from 8 a.m. to 8 p.m. Eastern time, Monday through Friday (excluding holidays). Request an ACS ticket number for reference in case this call doesn’t resolve your problem and you need follow-up assistance. Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
We’re updating Benefit Explainer to include Medicare Plus Blue benefit informationWe’re making updates to Benefit Explainer to improve the information available to you online and make it easier for you to do business with us. These changes will give you access to the same medical and benefit policy information for our Medicare Plus Blue℠ members as you already have for our commercial plan members. Benefit Explainer will continue to have Blue Cross Blue Shield of Michigan benefit information only; Blue Care Network benefit information isn’t included. What you need to know As of Nov. 7, we added a new link and tab for Medicare Plus Blue benefits. The new tab and link are labeled “Medicare Advantage Policy.” Although the new link and tab are visible to you now, the data won’t be loaded until a later date. Once the Medicare information is loaded, the new tab and link will be available for use. We’ll share more information with you as we get closer to the data launch. The tab and link previously titled “Medical/Payment Policy” are now labeled “Commercial Policy.” These tabs and links, along with others, will continue to function as usual. Other changes
The Communications tab has a new field called “Commercial/Medicare Advantage Identifier.” If you have any questions or need additional information, call Provider Inquiry.
We’re making a change to Record article categoriesAs part of our ongoing efforts to streamline The Record, we’re eliminating the Pharmacy category. Record articles related to prescription drugs will typically appear in the Professional or Facility categories, or both, depending on which types of health care providers require the information. Prescription drugs include those covered under pharmacy benefits as well as those covered under medical benefits. We’re doing this because most pharmacies don’t receive The Record, and we want the Record categories to better reflect the types of providers who need to read these articles. In addition, articles that previously appeared in the Pharmacy category tend to focus on prescription drugs and how professional and facility health care providers prescribe and administer those drugs. Beginning with this issue, following are the categories that will be used:
If you have any questions, send an email to provcomm@bcbsm.com.
Members enrolled in Healthy Blue Choices POS don’t need referrals to specialistsWhat you need to know We want to let specialists who participate with Blue Cross Blue Shield of Michigan know that members enrolled in Healthy Blue Choices℠ POS don’t need a referral to see them for covered services. However, some services are covered only from in-network providers, including office visits. Healthy Blue Choices℠ POS is a new point-of-service plan, effective Jan. 1, 2023, for FCA non-bargaining employees and retirees** that allows the flexibility to receive covered health care services in or out of network without a referral. It’s administered by Blue Care Network and works similarly to our popular Blue Elect Plus℠ POS plan. Members enrolled in Healthy Blue Choices POS or Blue Elect Plus POS don't need a referral for any covered service. They can refer themselves to any provider — even to providers who are considered out of network for this product. The member ID card prefix for both plans is the same one that’s on the member ID card for HMO coverage. The difference is that the front of the ID card shows the name of the plan. (See image below.) In addition, there is wording on the back of the card noting that referrals aren’t required. Healthy Blue Choices POS for employees
Requirements for selecting a primary care provider Healthy Blue Choices POS members with a Michigan address must select a BCN primary care physician; however, they also have the option to receive covered health care services in or out of network without a referral. Members who live outside of Michigan, with a non-Michigan address, don’t need an assigned primary care physician. They also don’t need a referral — they just need to see a BlueCard-participating provider if they want to pay the lower in-network out-of-pocket costs. More key information
For more information Refer to the Healthy Blue Choices℠ POS webpage for more information. If you have questions about Healthy Blue Choices POS, call Provider Inquiry as follows:
**FCA bargaining employees are covered under a separate health plan administered by Blue Care Network.
2023 early-release CPT Category III code update: New codes addedCategory III codes
Category III codes
Category III codes
Category III codes
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations. Billing chart: Blue Cross highlights medical, benefit policy changesYou’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart. This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures. You will also see that descriptions for the codes are no longer included. This is a result of recent negotiations with the AMA on use of the codes. We will publish information about new BCBS groups or changes to group benefits under the Group Benefit Changes heading. For more detailed descriptions of the BCBSM policies for these procedures, please check under the Medical/Payment Policy tab in Explainer on web-DENIS. To access this online information:
None of the information included in this billing chart is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
New radiology-focused initiative aims to improve quality of care and patient outcomesBlue Cross Blue Shield of Michigan and Blue Care Network are engaging Covera Health to launch a radiology-focused quality improvement program to help us better support radiologists and referring providers in their efforts to improve diagnostic quality, overall care and patient outcomes. Covera’s quality improvement programs support radiology facilities and radiologists in their efforts to:
Participating practices and radiologists will:
Program participation and quality assurance insights
Program availability Starting in April 2023, the program will be available for the following groups and members:
Designations for quality and value On prior authorization requests approved by AIM Specialty Health®, Covera designations will display as follows:
Providers that are designated as high quality and are also cost effective will receive an additional “high-value” designation on prior authorization requests approved by AIM. Cost efficiency is determined through cost factors including (but not limited to):
Only radiology centers that have been designated as high-quality are eligible to receive the high-value designation. Register for webinars to learn more Blue Cross, BCN and Covera Health will host webinars throughout the program, starting in January 2023. The webinars will provide an overview of the Covera programs, how they improved outcomes for members and providers, and how they can enhance peer learning opportunities. For more information on dates and clinical areas covered, go to coverahealth.com/webinar.** Questions? If you have questions about this program, contact Covera Health by calling 1-855-211-2272 or by sending an email message to bcbsmsupport@coverahealth.com. Our commitment to quality Blue Cross and BCN are proud to be leaders in advancing collaborative partnerships with our provider community to improve the quality, outcomes and value of care delivered to our members. This new radiology-focused initiative represents a significant step in fulfilling our commitment to our providers, our members and the communities we serve. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. AIM Specialty Health is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services. For more information, go to our ereferrals.bcbsm.com website. Covera Health is an independent company that supports Blue Cross Blue Shield of Michigan and Blue Care Network by providing programs to help improve the diagnostic quality, quality of care and member outcomes related to radiology.
Billing changes coming for COVID-19 treatment productsSince the development of COVID-19 treatment products, the U.S. government has provided these products at no cost to health care providers. Because of this, providers submitted claims to Blue Cross Blue Shield of Michigan or Blue Care Network only for the administration of the products. As the remaining federal supply runs out, these products are transitioning to the commercial marketplace.After a product transitions, providers will need to purchase it and submit a claim to Blue Cross or BCN for both the product and the administration of the product. For Blue Cross commercial and BCN commercial members, out-of-pocket costs may apply for commercialized treatment products. Notes:
Expected time frame for additional products to transition to commercial marketplace According to the Administration for Strategic Preparedness & Response,** following is the expected time frame for these products to transition to the commercial marketplace:
Additional information For more information on COVID-19 vaccines, treatment, billing, etc., refer to our Coronavirus webpage. To access this page, log in to our provider portal (availity.com**) and follow these steps:
You can also view these documents on our public coronavirus webpage. Note: The U.S. Department of Health and Human Services is assisting providers who treat uninsured or underinsured patients with commercially purchased bebtelovimab by offering to replace the dose for free. HHS expects the supply for this initiative** to last through September 2023. Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Here’s what you need to know about COVID-19 vaccinesWhen the government-purchased supply of COVID-19 vaccines runs out, health care providers should bill members’ health plans for both administration and the vaccine. We’ll process claims based on members’ immunization benefits. As a reminder, you can view our COVID-19 provider communications as follows:
You can also access these communications on our public COVID-19 webpage for health care providers. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services.
User guide created to assist providers with importing medical recordsEXL Health has created a user guide to assist health care providers with importing medical records into their portal. EXL is an independent company that contracts with Blue Cross Blue Shield of Michigan to conduct medical claim audits for Medicare Plus Blue℠ and Blue Cross commercial members. No need to register Providers, hospitals and facilities don’t need to register for an account to use the portal. They can use their facility name, letter reference key or email address to begin importing the requested medical records at exlhealthproviderportal.exlservice.com.** Some features of EXL provider portal:
Training Providers can get instructions needed for training staff on using the portal at exlservice.com/how-to-send-medical-records.** Questions? EXL is available to assist during any step of the process. Contact EXL by calling 1‑833-717-0378 and pressing “0” from 8 a.m. to 5 p.m. Eastern time Monday through Friday. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Here are the 2023 FEP benefit changesBlue Cross and Blue Shield Federal Employee Program® 2023 benefit changes will take effect Jan. 1, 2023. Below is an overview of the changes. Acupuncture
Bariatric surgery
Diagnostic services
Facility
Infertility
Maternity
Medical food
Pharmacy
Preventive care
New prior approval requirements
Transplants
For complete 2023 Blue Cross and Blue Shield Service Benefit Plan benefit information, go to fepblue.org/brochure or call Customer Service at 1-800-482-3600.
Know how to access and use RC Claim Assist through Availity EssentialsWhat you need to know RC Claim Assist is available to Blue Cross Blue Shield of Michigan and Blue Care Network contracted health care providers through Availity® Essentials to help them bill for drugs covered under the medical benefit. This article was developed to provide information on how to access and use RC Claim Assist, a free web‑based resource. RC Claim Assist provides:
How to access RC Claim Assist Here’s how to find RC Claim Assist within Availity Essentials:
Tips to help you use RC Claim Assist You can use any of the following starting points to retrieve the conversion between HCPCS or CPT and NDC:
Refer to the tool only as a general reference and in conjunction with other resources, such as applicable fee schedules. Note: Average wholesale price displayed is for reference only and doesn’t reflect the actual reimbursement in claims processing. Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Pemfexy to require prior authorization for most members starting Feb. 9For dates of service on or after Feb. 9, 2023, we’ll require prior authorization for Pemfexy® (pemetrexed), HCPCS code J9304, through AIM Specialty Health®. This drug is part of members’ medical benefits, not their pharmacy benefits. Prior authorization requirements apply when this drug is administered in outpatient settings for:
How to submit authorization requests Submit authorization requests to AIM using one of the following methods:
More about the authorization requirements Authorization isn’t a guarantee of payment. As always, health care providers need to verify eligibility and benefits for members. For additional information on requirements related to drugs covered under the medical benefit, refer to the following drug lists:
We’ll update the pertinent drug lists to reflect the information in this message prior to the effective date. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Xenpozyme and Spevigo to have site-of-care requirements for most commercial members, starting in MarchFor dates of service on or after March 1, 2023, we’re adding site-of-care requirements for Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members for the following drugs covered under the medical benefit:
The NovoLogix® online tool will prompt you to select a site of care when you submit prior authorization requests for these drugs. If the request meets clinical criteria for the drug, it will be approved automatically if it’s for one of the following sites of care:
Additional information or documentation may be required for requests to administer Xenpozyme or Spevigo in an outpatient hospital setting. As a reminder, these drugs already require prior authorization; providers can submit prior authorization requests using NovoLogix. The new site-of-care requirements are in addition to the current prior authorization requirements. Members who start courses of treatment with Xenpozyme or Spevigo before March 1, 2023, will be able to continue receiving the drug in their current location until their existing authorization expires. If those members then continue treatment under a new prior authorization, the site-of-care requirements outlined above will apply. Some Blue Cross commercial groups not subject to these requirements For Blue Cross commercial groups, the prior authorization and site-of-care requirements apply only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. Note: Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don’t participate in the standard prior authorization program. List of requirements For a full list of requirements related to drugs covered under the medical benefit, see the Blue Cross and BCN utilization management medical drug list for Blue Cross commercial and BCN commercial members. We’ll update this list prior to March 1, 2023. You can access this list and other information about requesting prior authorization on ereferrals.bcbsm.com at these locations: As a reminder, authorization isn't a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members.
Fylnetra now requires prior authorization for Medicare Advantage membersFor dates of service on or after Dec. 19, 2022, we require prior authorization for Fylnetra® (pegfilgrastim-pbbk), HCPCS code J3590, for our Medicare Advantage members (both Medicare Plus Blue℠ and BCN Advantage℠ members). This drug is part of members’ medical benefits, not their pharmacy benefits. Submit prior authorization requests through the NovoLogix® online tool. When prior authorization is required This medication requires prior authorization when it’s administered by a health care provider in sites of care such as outpatient facilities or physicians’ offices, and is billed in one of the following ways:
Submit prior authorization requests through the NovoLogix tool To access NovoLogix, log in to our provider portal (availity.com**), click on Payer Spaces in the menu bar and then click on the BCBSM and BCN logo. You’ll find links to the NovoLogix tools on the Applications tab. Note: If you need to request access to our provider portal, follow the instructions on the Register for web tools webpage on bcbsm.com/providers. List of requirements For a list of requirements related to drugs covered under the medical benefit, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue PPO and BCN Advantage members. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services.
Hemgenix and Tzield require prior authorization for Medicare Advantage membersFor dates of service on or after Dec. 2, 2022, we require prior authorization for Medicare Plus Blue℠ and BCN Advantage℠ members for the following drugs covered under the medical benefit:
A prior authorization requirement also applies to most Blue Cross Blue Shield of Michigan and Blue Care Network commercial members. See this provider alert for more information. Submit prior authorization requests through NovoLogix® Submit prior authorization requests for Hemgenix and Tzield through the NovoLogix online tool. It offers real-time status checks and immediate approvals for certain medications. To access NovoLogix, log in to our provider portal (availity.com**), click on Payer Spaces in the menu bar and then click on the BCBSM and BCN logo. You’ll find links to the NovoLogix tools on the Applications tab. To request access to our provider portal, follow the instructions on the Register for web tools webpage at bcbsm.com/providers. When prior authorization is required These medications require prior authorization when they’re administered by a health care provider in sites of care such as outpatient facilities or physicians’ offices and are billed in one of the following ways:
List of requirements For a full outline of requirements related to drugs covered under the medical benefit for our Medicare Advantage members, refer to the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue PPO and BCN Advantage members. We’ve updated this list to reflect the change for Hemgenix and Tzield. You can access this list and other information about requesting prior authorization at ereferrals.bcbsm.com on these pages: Authorization isn't a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Reminder: What you need to know about billing specialty pharmacy drugsWe want to remind you that specialty pharmacy drugs shouldn’t be billed by both the specialty pharmacy and physician. When physician-administered drugs are ordered from the specialty pharmacy and shipped to the physician for administration, the specialty pharmacy submits the claim for the drug under the medical benefit. The physician should only bill for the administration of the drug. If the specialty drug is billed by both the specialty pharmacy and physician, the physician’s claim may be denied.
We’re expanding specialty pharmacy claim editing for Medicare Plus BlueIn support of correct coding and payment accuracy, we’ll begin applying additional edits for specialty pharmacy claims in March 2023 for our Medicare Plus Blue℠ members. These edits apply to claims processed under the medical benefit, not the pharmacy benefit. They’ll address various coding inaccuracies, including, but not limited to:
These edits are supported by guidelines as approved by the Centers for Medicare & Medicaid Services and other nationally recognized governing bodies. We’ve updated fax forms for submitting prior authorization requests to TurningPointOn Nov. 22, 2022, Blue Cross Blue Shield of Michigan and Blue Care Network posted updated fax forms on ereferrals.bcbsm.com for use when submitting prior authorization requests to TurningPoint Healthcare Solutions, LLC, for musculoskeletal procedures. We updated the forms as follows:
If you use fax forms to submit prior authorization requests to TurningPoint, be sure to incorporate the updated forms into your process. You can find these forms and other useful resources on these pages of our ereferrals.bcbsm.com website: TurningPoint Healthcare Solutions LLC is an independent company that manages authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
New, engaging patient experience e-learning course now availableAction item Visit our provider training site to learn how to improve the overall experience of your patients. Many of you have been asking for a self-directed, virtual approach to learning best practice tips, tools and techniques for improving the patient experience in personal and office interactions with patients. We’ve responded by developing a patient experience e-learning course, consisting of four modules. The four modules include:
The series is informative, engaging, fun and respectful of your busy schedules. It takes on average about 15 minutes to complete a module. The modules have been reviewed and enthusiastically endorsed by a variety of our stakeholders, including physicians, physician organization staff and provider office staff. They’re available for clinical and non-clinical staff on our provider training site. We encourage you to go through the modules individually or as part of a team in the office. To register for and access provider training site To request access to the site (if you haven’t already registered) or to link to the site, follow these steps:
If you need assistance creating your login ID or navigating the site, contact ProviderTraining@bcbsm.com. Continuing education credits The Minnesota Medical Association designates this activity for a maximum of 2 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. Patient experience podcast series As a reminder, be sure to check out our patient experience podcasts. For complete details, see the December Record article.
New on-demand training availableAction item Visit our provider training site to find new resources on topics that are important to your role. Provider Experience continues to offer new training resources for health care providers and staff. Our on-demand courses can help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network. We recently added the following learning opportunities:
As a reminder, we also have courses available to physicians for continuing education credit. These include:
Check the dashboard on our provider training site for announcements of what’s available as we add more CME offerings to enhance the training experience for health care providers and staff. Complete the following steps to request access to the training site:
If you need assistance creating your login ID or navigating the site, contact ProviderTraining@bcbsm.com.
Gastric stimulation questionnaire updatedOn Nov. 14, 2022, we updated the Gastric stimulation questionnaire in the e-referral system for adult Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members. We also updated the corresponding preview questionnaire on the ereferrals.bcbsm.com website. As a reminder, we use our prior authorization criteria, our medical policies and your answers to the questionnaires in the e-referral system when making utilization management determinations on your prior authorization requests. Preview questionnaires You can access preview questionnaires at ereferrals.bcbsm.com. They show the questions you'll need to answer in the questionnaires that open in the e-referral system so you can prepare your answers ahead of time. To find the preview questionnaires:
Authorization criteria and medical policies The pertinent prior authorization criteria and medical policies are also available on the Authorization Requirements & Criteria page.
We won’t be bundling testing codes for sexually transmitted infections at this timeIn an article in the October Record, we wrote that we planned to bundle STI testing codes in the near future. However, after additional consideration, we’ve decided not to move forward with this initiative at this time. If a determination is made to pursue this initiative further, we’ll communicate about it in a future issue of The Record.
New radiology-focused initiative aims to improve quality of care and patient outcomesBlue Cross Blue Shield of Michigan and Blue Care Network are engaging Covera Health to launch a radiology-focused quality improvement program to help us better support radiologists and referring providers in their efforts to improve diagnostic quality, overall care and patient outcomes. Covera’s quality improvement programs support radiology facilities and radiologists in their efforts to:
Participating practices and radiologists will:
Program participation and quality assurance insights
Program availability Starting in April 2023, the program will be available for the following groups and members:
Designations for quality and value On prior authorization requests approved by AIM Specialty Health®, Covera designations will display as follows:
Providers that are designated as high quality and are also cost effective will receive an additional “high-value” designation on prior authorization requests approved by AIM. Cost efficiency is determined through cost factors including (but not limited to):
Only radiology centers that have been designated as high-quality are eligible to receive the high-value designation. Register for webinars to learn more Blue Cross, BCN and Covera Health will host webinars throughout the program, starting in January 2023. The webinars will provide an overview of the Covera programs, how they improved outcomes for members and providers, and how they can enhance peer learning opportunities. For more information on dates and clinical areas covered, go to coverahealth.com/webinar.** Questions? If you have questions about this program, contact Covera Health by calling 1-855-211-2272 or by sending an email message to bcbsmsupport@coverahealth.com. Our commitment to quality Blue Cross and BCN are proud to be leaders in advancing collaborative partnerships with our provider community to improve the quality, outcomes and value of care delivered to our members. This new radiology-focused initiative represents a significant step in fulfilling our commitment to our providers, our members and the communities we serve. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. AIM Specialty Health is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services. For more information, go to our ereferrals.bcbsm.com website. Covera Health is an independent company that supports Blue Cross Blue Shield of Michigan and Blue Care Network by providing programs to help improve the diagnostic quality, quality of care and member outcomes related to radiology.
Here’s what you need to know about COVID-19 vaccinesWhen the government-purchased supply of COVID-19 vaccines runs out, health care providers should bill members’ health plans for both administration and the vaccine. We’ll process claims based on members’ immunization benefits. As a reminder, you can view our COVID-19 provider communications as follows:
You can also access these communications on our public COVID-19 webpage for health care providers. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services.
User guide created to assist providers with importing medical recordsEXL Health has created a user guide to assist health care providers with importing medical records into their portal. EXL is an independent company that contracts with Blue Cross Blue Shield of Michigan to conduct medical claim audits for Medicare Plus Blue℠ and Blue Cross commercial members. No need to register Providers, hospitals and facilities don’t need to register for an account to use the portal. They can use their facility name, letter reference key or email address to begin importing the requested medical records at exlhealthproviderportal.exlservice.com.** Some features of EXL provider portal:
Training Providers can get instructions needed for training staff on using the portal at exlservice.com/how-to-send-medical-records.** Questions? EXL is available to assist during any step of the process. Contact EXL by calling 1‑833-717-0378 and pressing “0” from 8 a.m. to 5 p.m. Eastern time Monday through Friday. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Here are the 2023 FEP benefit changesBlue Cross and Blue Shield Federal Employee Program® 2023 benefit changes will take effect Jan. 1, 2023. Below is an overview of the changes. Acupuncture
Bariatric surgery
Diagnostic services
Facility
Infertility
Maternity
Medical food
Pharmacy
Preventive care
New prior approval requirements
Transplants
For complete 2023 Blue Cross and Blue Shield Service Benefit Plan benefit information, go to fepblue.org/brochure or call Customer Service at 1-800-482-3600.
Pemfexy to require prior authorization for most members starting Feb. 9For dates of service on or after Feb. 9, 2023, we’ll require prior authorization for Pemfexy® (pemetrexed), HCPCS code J9304, through AIM Specialty Health®. This drug is part of members’ medical benefits, not their pharmacy benefits. Prior authorization requirements apply when this drug is administered in outpatient settings for:
How to submit authorization requests Submit authorization requests to AIM using one of the following methods:
More about the authorization requirements Authorization isn’t a guarantee of payment. As always, health care providers need to verify eligibility and benefits for members. For additional information on requirements related to drugs covered under the medical benefit, refer to the following drug lists:
We’ll update the pertinent drug lists to reflect the information in this message prior to the effective date. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Xenpozyme and Spevigo to have site-of-care requirements for most commercial members, starting in MarchFor dates of service on or after March 1, 2023, we’re adding site-of-care requirements for Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members for the following drugs covered under the medical benefit:
The NovoLogix® online tool will prompt you to select a site of care when you submit prior authorization requests for these drugs. If the request meets clinical criteria for the drug, it will be approved automatically if it’s for one of the following sites of care:
Additional information or documentation may be required for requests to administer Xenpozyme or Spevigo in an outpatient hospital setting. As a reminder, these drugs already require prior authorization; providers can submit prior authorization requests using NovoLogix. The new site-of-care requirements are in addition to the current prior authorization requirements. Members who start courses of treatment with Xenpozyme or Spevigo before March 1, 2023, will be able to continue receiving the drug in their current location until their existing authorization expires. If those members then continue treatment under a new prior authorization, the site-of-care requirements outlined above will apply. Some Blue Cross commercial groups not subject to these requirements For Blue Cross commercial groups, the prior authorization and site-of-care requirements apply only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. Note: Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don’t participate in the standard prior authorization program. List of requirements For a full list of requirements related to drugs covered under the medical benefit, see the Blue Cross and BCN utilization management medical drug list for Blue Cross commercial and BCN commercial members. We’ll update this list prior to March 1, 2023. You can access this list and other information about requesting prior authorization on ereferrals.bcbsm.com at these locations: As a reminder, authorization isn't a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members.
Fylnetra now requires prior authorization for Medicare Advantage membersFor dates of service on or after Dec. 19, 2022, we require prior authorization for Fylnetra® (pegfilgrastim-pbbk), HCPCS code J3590, for our Medicare Advantage members (both Medicare Plus Blue℠ and BCN Advantage℠ members). This drug is part of members’ medical benefits, not their pharmacy benefits. Submit prior authorization requests through the NovoLogix® online tool. When prior authorization is required This medication requires prior authorization when it’s administered by a health care provider in sites of care such as outpatient facilities or physicians’ offices, and is billed in one of the following ways:
Submit prior authorization requests through the NovoLogix tool To access NovoLogix, log in to our provider portal (availity.com**), click on Payer Spaces in the menu bar and then click on the BCBSM and BCN logo. You’ll find links to the NovoLogix tools on the Applications tab. Note: If you need to request access to our provider portal, follow the instructions on the Register for web tools webpage on bcbsm.com/providers. List of requirements For a list of requirements related to drugs covered under the medical benefit, see the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue PPO and BCN Advantage members. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services.
Hemgenix and Tzield require prior authorization for Medicare Advantage membersFor dates of service on or after Dec. 2, 2022, we require prior authorization for Medicare Plus Blue℠ and BCN Advantage℠ members for the following drugs covered under the medical benefit:
A prior authorization requirement also applies to most Blue Cross Blue Shield of Michigan and Blue Care Network commercial members. See this provider alert for more information. Submit prior authorization requests through NovoLogix® Submit prior authorization requests for Hemgenix and Tzield through the NovoLogix online tool. It offers real-time status checks and immediate approvals for certain medications. To access NovoLogix, log in to our provider portal (availity.com**), click on Payer Spaces in the menu bar and then click on the BCBSM and BCN logo. You’ll find links to the NovoLogix tools on the Applications tab. To request access to our provider portal, follow the instructions on the Register for web tools webpage at bcbsm.com/providers. When prior authorization is required These medications require prior authorization when they’re administered by a health care provider in sites of care such as outpatient facilities or physicians’ offices and are billed in one of the following ways:
List of requirements For a full outline of requirements related to drugs covered under the medical benefit for our Medicare Advantage members, refer to the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue PPO and BCN Advantage members. We’ve updated this list to reflect the change for Hemgenix and Tzield. You can access this list and other information about requesting prior authorization at ereferrals.bcbsm.com on these pages: Authorization isn't a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. We’ve updated fax forms for submitting prior authorization requests to TurningPointOn Nov. 22, 2022, Blue Cross Blue Shield of Michigan and Blue Care Network posted updated fax forms on ereferrals.bcbsm.com for use when submitting prior authorization requests to TurningPoint Healthcare Solutions, LLC, for musculoskeletal procedures. We updated the forms as follows:
If you use fax forms to submit prior authorization requests to TurningPoint, be sure to incorporate the updated forms into your process. You can find these forms and other useful resources on these pages of our ereferrals.bcbsm.com website: TurningPoint Healthcare Solutions LLC is an independent company that manages authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
New on-demand training availableAction item Visit our provider training site to find new resources on topics that are important to your role. Provider Experience continues to offer new training resources for health care providers and staff. Our on-demand courses can help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network. We recently added the following learning opportunities:
As a reminder, we also have courses available to physicians for continuing education credit. These include:
Check the dashboard on our provider training site for announcements of what’s available as we add more CME offerings to enhance the training experience for health care providers and staff. Complete the following steps to request access to the training site:
If you need assistance creating your login ID or navigating the site, contact ProviderTraining@bcbsm.com. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 If you’re still getting accustomed to using our new provider portal, Availity® Essentials, here are some tips that can help with claims-related activities.
If you’re still getting accustomed to using our new provider portal, Availity® Essentials, here are some tips that can help with claims-related activities.