|
July 2022

Program provides mobile crisis assessment and stabilization for mental health and substance use
As you may have read last September in The Record, Blue Cross Blue Shield of Michigan began offering a new method of obtaining crisis assessment and stabilization services for mental health and substance use, effective Oct. 1, 2021. This article provides additional details.
Our mobile crisis and crisis stabilization services help ensure that our Blue Cross and Blue Care Network commercial members who are in crisis get prompt and appropriate behavioral health treatment. These services can also help members avoid emergency room visits for mental health issues and substance use disorder, as well as unnecessary hospitalizations.
Central to the success of the program has been the establishment of facilities that provide high-quality mobile crisis and crisis stabilization services. Currently two facilities in Southeast Michigan meet the criteria to provide these services as part of our program: Common Ground Resources and Crisis Center, and Hegira Health’s COPE, which stands for Community Outreach for Psychiatric Emergencies.
Here’s additional information about these centers:
Common Ground Resources and Crisis Center
Phone: 1-800-231-1127
Primary geographic areas covered: Oakland County, Macomb County, west of Macomb County
Hegira Health’s COPE
Phone: 1-734-721-0200
Primary geographic areas covered: Livonia, Wayne County
Currently, Blue Cross is in discussion with other facilities that are interested in providing such services. We also hope to expand these services to our Medicare Advantage members in the future.
“The beauty of these services is they can meet the member where they are and be accessed any way you need to access them,” said Dr. William Beecroft, medical director of behavioral health for Blue Cross.
They can be accessed by a health care provider, the member or other individuals. For example:
- A physician with a patient in crisis can contact one of these centers directly to have the patient be evaluated by a member of the mobile crisis team, either in person or by phone.
- An emergency department at a hospital can contact one of the centers to request assistance in evaluating the patient and determining the best course of treatment, placement and referrals.
- A member can call the number on the back of their ID card to connect with a Blue Cross case manager who can direct them to a crisis counselor at one of the participating facilities.
- Members can call one of the participating centers directly or simply walk into one of the crisis stabilization units.
- A law enforcement officer can call one of the centers for a behavioral health evaluation for a citizen in crisis.
“These services help ensure our members get treated at the right place at the right time and that they’re linked to the appropriate level of care and available community resources,” Beecroft said. “However, as part of the evaluation and treatment process, some members may still require psychiatric hospitalization as part of their treatment plan.”
Mobile crisis services
The mobile crisis mental health team may stay involved for two to four weeks after the initial encounter to ensure patients are connected to the right level of care for mental health or substance use issues.
Following the initial encounter, crisis stabilization services (formerly called psychiatric observation) may take place and include:
- Behavioral health evaluation to initiate appropriate treatment (similar to medical observation services)
- Physical site-based services that are necessary to support the mobile crisis team
- Services include intake assessment, psychiatric evaluation, crisis intervention, psychotherapy, medication administration, therapeutic injection, laboratory and imaging diagnostics, observation and peer support
- Linkages and “warm handoffs” to the appropriate level of care and community resources
Additional benefits
Here are some additional benefits of mobile crisis and crisis stabilization services:
- A speedy, specialty-focused and confidential assessment of their immediate behavioral health (mental health and substance use disorder) needs
- A multidisciplinary evaluation, including the services of a psychiatrist, which leads to a plan of care and placement in the appropriate level of care
- A positive, less stigmatizing experience than with some other systems of care.
- Rapid access to behavioral interventions, including medication, nursing care, psychotherapy and psychoeducation
- Alleviation of a sense of crisis, encouraging feelings of hope
Facilities that offer mobile crisis and crisis stabilization services must meet certain criteria. For example, they must be open 24/7 and incorporate the services of a multidisciplinary staff, including physicians, registered nurses, licensed master social workers, psychologists, clinical supervisors and additional support staff.
For more information
To learn more — or if you’re interested in joining the program as a facility offering these services — contact one of the following:
Blue Cross recognized as No. 1 in customer satisfaction among commercial health plans in Michigan
 For the second time in three years, Blue Cross Blue Shield of Michigan and Blue Care Network received the J.D. Power Award for ranking first overall with highest member satisfaction among commercial health plans in Michigan. Achieving the top ranking was largely driven by strong scores in coverage and benefits, provider choice and information and communication. For the second time in three years, Blue Cross Blue Shield of Michigan and Blue Care Network received the J.D. Power Award for ranking first overall with highest member satisfaction among commercial health plans in Michigan. Achieving the top ranking was largely driven by strong scores in coverage and benefits, provider choice and information and communication.
You can view our recent news release about this announcement here. For more details on the J.D. Power 2022 Commercial Health Plan Study℠, visit jdpower.com.**
J.D. Power is a global leader in consumer insights, advisory services and data and analytics. A pioneer in the use of “big data,” artificial intelligence and algorithmic modeling capabilities to understand consumer behavior, J.D. Power has been delivering incisive industry intelligence on customer interactions with brands and products for more than 50 years. The world's leading businesses across major industries rely on J.D. Power to guide their customer-facing strategies.
J.D. Power has offices in North America, Europe and Asia Pacific. To learn more about the company’s business offerings, visit JDPower.com/business. The J.D. Power auto shopping tool can be found at JDPower.com.
About the study
The U.S. Commercial Member Health Plan Study, now in its 16th year, measures satisfaction among members of 147 health plans in 22 regions throughout the United States by examining six factors (in alphabetical order):
- Billing and payment
- Cost
- Coverage and benefits
- Customer service
- Information and communication
- Provider choice
The study also measures several other key aspects of the experience and member engagement.
The study is based on responses from 36,366 commercial health plan members and was fielded from January through April 2022.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Provider Secured Services, including web-DENIS, end date extended for some functions
Blue Cross Blue Shield of Michigan and Blue Care Network are extending the original June 21, 2022, retirement date for some core functions within Provider Secured Services, including web-DENIS.
We encourage you to continue to learn and use the new provider portal, Availity Essentials. Some functions will remain on Provider Secured Services for a limited time, but many links and resource information will only be accessible through Availity®.
See the provider alert for more details.
Here are resources for learning about our new provider portal
 If you’re looking for training or have questions about the new Blue Cross Blue Shield of Michigan and Blue Care Network provider portal, Availity Essentials, take advantage of the following resources. If you’re looking for training or have questions about the new Blue Cross Blue Shield of Michigan and Blue Care Network provider portal, Availity Essentials, take advantage of the following resources.
View recorded trainings
You can view recorded trainings on how to use Availity Essentials for your Blue Cross and BCN business. You must have an Availity® account to access these recordings. See the section on registration below if you’re not yet registered.
There are two ways to find recorded trainings:
- Within the provider portal, you can find the training sessions by following these steps:
- Log in to our provider portal (availity.com**).
- Choose Help & Training and then click on Get Trained.
- In the search field at the top of the screen, enter BCBSM.
Find answers to your questions
Here’s where you can find answers to your questions:
Still need to register?
If you haven’t yet registered for an Availity Essentials account, you no longer have access to some Blue Cross Blue Shield of Michigan and Blue Care Network online tools. For information about registering with Availity, go to the Blue Cross and BCN Welcome to Availity** webpage, scroll down the page and click on Register for Availity Essentials.
After registering, your Availity administrator will need to take additional steps for users to access e-referral and Health e-Blue℠. For more information, go to our Register for web tools page and scroll down to Getting access to Blue Cross and BCN tools through our provider portal.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services.
Clarification: At-home COVID-19 testing policy revised for Blue Cross, BCN commercial plans
We ran an article in March Record and March-April BCN Provider News about our revised at-home COVID-19 testing policy. On May 19, we posted a provider alert clarifying how frequently members can obtain at-home rapid diagnostic COVID-19 tests, changing the wording from “monthly” to “every 30 days.” Currently, commercial members with pharmacy coverage through Blue Cross Blue Shield of Michigan or Blue Care Network have coverage for up to eight FDA-approved, over-the-counter at-home rapid diagnostic COVID-19 tests every 30 days.
The federal government’s website has also been updated and the quantity and timing on shipping has been removed as this continues to change.
See the May 19 provider alert and the articles in the March Record and March-April BCN Provider News for additional details.
Amendments made to Trading Partner Agreement
Effective Sept. 1, the Blue Cross Blue Shield of Michigan Trading Partner Agreement will be amended to include Blue Care Network of Michigan when Blue Cross is functioning as a health plan. All terms of paragraph 14 of the TPA, which governs Blue Cross’ relationship with non-participating providers, will also include Blue Care Network.
The TPA is the document that governs how electronic data interchange and electronic transactions, including electronic claims, will be conducted between Blue Cross and its trading partner — typically health care providers, billing agents and other health plans.
No action is needed on your part for this change to occur.
Chippewa County War Memorial Hospital changed its name
On April 1, 2022, Chippewa County War Memorial Hospital officially changed its name to MyMichigan Medical Center Sault. The hospital is located in Sault Ste Marie, Michigan. You’ll want to make a note of this for your files and for billing purposes.
Billing chart: Blue Cross highlights medical, benefit policy changes
You’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart.
This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures.
You will also see that descriptions for the codes are no longer included. This is a result of recent negotiations with the AMA on use of the codes.
We will publish information about new BCBS groups or changes to group benefits under the Group Benefit Changes heading.
For more detailed descriptions of the BCBSM policies for these procedures, please check under the Medical/Payment Policy tab in Explainer on web-DENIS. To access this online information:
- Log in to web-DENIS.
- Click on BCBSM Provider Publications & Resources.
- Click on Benefit Policy for a Code.
- Click on Topic.
- Under Topic Criteria, click on the drop-down arrow next to Choose Identifier Type and then click on HCPCS Code.
- Enter the procedure code.
- Click on Finish.
- Click on Search.
| Code* |
BCBSM changes to:
Basic Benefit and Medical Policy, Group
Variations Payment Policy, Guidelines
|
| NEW PAYABLE PROCEDURES |
E0118 |
Basic benefit and medical policy
Knee scooters or crutch substitute
The knee scooter or crutch substitute is established for individuals with below-the-knee injuries as an alternative to standard crutches.
The policy is effective May 1, 2022. |
| POLICY CLARIFICATIONS |
36482, 36483
Experimental:
36473, 36474
|
Basic benefit and medical policy
Endovenous ablation of varicose veins (ClariVein, VeniSeal Closure System)
Endovenous ablation of varicose veins by mechanochemical (ClariVein®) is experimental. This procedure hasn’t been scientifically demonstrated to be as safe and effective as conventional treatment.
Endovenous ablation of varicose veins by chemical adhesive (Cyanoacrylate, VenaSeal™) is established in patients with symptomatic varicose veins/venous insufficiency when the below criteria are met.
Coverage criteria has been updated, effective July 1, 2022
Inclusions:
Great or small saphenous veins
Cyanoacrylate adhesive may be considered established for symptomatic varicose veins/venous insufficiency when all the following criteria have been met:
- There is demonstrated saphenous reflux and CEAP, or Clinical, Etiology, Anatomy, Pathophysiology, class C2 or greater.
- There is documentation of one or more of the following indications:
- Ulceration secondary to venous stasis
- Recurrent superficial thrombophlebitis
- Hemorrhage or recurrent bleeding episodes from a ruptured superficial varicosity
- Persistent pain, swelling, itching, burning or other symptoms are associated with saphenous reflux and the symptoms significantly interfere with activities of daily living and conservative management therapy, including compression therapy for at least three consecutive months prior to surgical interventionhasn’t improved the symptoms:
- Conservative management must include a trial of compression therapy garments or medical reason for compression therapy exemption is documented (e.g., existing chronic limb ischemia, severe musculoskeletal disability, morbid obesity, unusual leg anatomy)
Accessory saphenous veins
All the following criteria must be met:
- Incompetence of the accessory saphenous vein is isolated or the great or small saphenous veins had been previously eliminated (at least three months).
- There is demonstrated accessory saphenous reflux.
- There is documentation of one or more of the following indications:
- Ulceration secondary to venous stasis
- Recurrent superficial thrombophlebitis
- Hemorrhage or recurrent bleeding episodes from a ruptured superficial varicosity
- Persistent pain, swelling, itching, burning or other symptoms are associated with saphenous reflux and the symptoms significantly interfere with activities of daily living and conservative management therapy, including compression therapy for at least three consecutive months prior to surgical intervention, hasn’t improved the symptoms:
- Conservative management must include a trial of compression therapy garments or medical reason for compression therapy exemption is documented (e.g., existing chronic limb ischemia, severe musculoskeletal disability, morbid obesity, unusual leg anatomy)
|
76390
Experimental
0609T, 0610T, 0611T, 0612T
|
Basic benefit and medical policy
Magnetic resonance spectroscopy
The safety and effectiveness of magnetic resonance spectroscopy have been established for patients meeting specific patient selection criteria.
Exclusionary criteria have been updated, effective July 1, 2022.
Inclusions:
Magnetic resonance spectroscopy, or MRS, is an appropriate clinical tool for diagnosing:
- Disorders of creatine metabolism
- Presence of mitochondrial disease
- MRS may be used to assist in distinguishing tissue necrosis from persistent or recurrent brain tumor as an alternative to invasive brain biopsy
Exclusions:
- MRS for discogenic pain (cervical, thoracic or lumbar)
- MRS for any condition other than those listed in the Inclusions section
|
78072, 78830,** 78832**
**Payable effective Jan. 1, 2022 |
Basic benefit and medical policy
SPECT/CT fusion imaging
The safety and effectiveness of SPECT/CT fusion imaging have been established. It may be considered a useful imaging option when indicated.
Payment policy:
May be subject to prior authorization through the PPO Radiology Management Program. Check member benefits.
Inclusions:
- Preoperative evaluation to further localize a lesion identified on planar scintigraphy or SPECT when additional anatomic information is needed to direct surgery and that information hasn’t already been provided by CT or MRI
- Radiation therapy for planning of selective internal radiation therapy, or SIRT
- Bone imaging:
- Avascular necrosis when MRI can’t be performed or is nondiagnostic in either of the following scenarios:
- Diagnosis following negative or inconclusive radiographs
- Preoperative planning for osteonecrosis with femoral head collapse
- Fracture, including occult or stress fracture in any of the following scenarios:
- Suspected spinal fracture when other imaging (radiographs, CT or MRI) is nondiagnostic
- Suspected skeletal injury in non-accidental trauma when MRI can’t be performed or is nondiagnostic
- Suspected fracture, when MRI cannot be performed or is nondiagnostic at the following high-risk/weight bearing sites:
- Femoral neck; proximal femur
- Tibia (anterior/lateral/plateau)
- Great toe sesamoid
- Patella
- Scaphoid
- Lunate
- Talus
- Navicular
- Metatarsal base (second and fifth digits)
- Bone lesions for further characterization of indeterminate bone lesions when MRI, CT or planar scintigraphy is equivocal
- Osseous metastatic disease: osseous metastatic disease, not otherwise specified in either of the following scenarios:
- Diagnostic workup and management when both of the following apply:
- Patient has a documented malignancy and signs or symptoms concerning for bony metastatic disease
- Suspicious findings on CT, MRI or planar bone scintigraphy require further clarification
- To determine bone invasion prior to surgical resection of head and neck malignancies when CT, PET/CT or MRI is nondiagnostic
- Postoperative joint or spine pain when other imaging (radiographs, CT or MRI) is nondiagnostic
- Spondylolysis/spondylolisthesis when radiographs provide insufficient information to direct management
- Sentinel node localization when clinical evaluation is negative nodal involvement in the following scenarios:
- Stage I-III invasive breast cancer
- Cervical cancer that is stage IA1 with lymphovascular invasion (LVI), IA2, IB1, or IIA1
- Head and neck cancer when decisions are being made regarding mandibular resection
- Melanoma that is stage IA with adverse features, IB, stage II, in-transit or locally recurrent
- Penile cancer
- Uterine cancer confined to the uterus
- Vulvar cancer (T1 or T2)
- Neuroendocrine cancer diagnostic workup and management of documented neuroendocrine cancer as clinically indicated for neuroblastoma or tumors of the autonomic nervous system (pheochromocytoma, paraganglioma, ganglioneuroma)
- Parathyroid/thyroid cancer to identify tumor for surgical planning, localization of residual tissue in patients with recurrent or persistent disease following surgery and surveillance for intermediate or high-risk differentiated cancer six to 12 months after therapy has been completed
- Pulmonary embolism when CT/CTA can’t be performed or is nondiagnostic
- Infection/inflammation not otherwise specified, for functional anatomic mapping of infections
- Back pain when all other diagnostic workup is inconclusive
Exclusions:
SPECT/CT fusion imaging for any other condition than listed above. |
78608, 78609, 788112, 78812, 78813, 78814, 78815, 78816, A9552
Experimental
Q9982, Q9983
|
Basic benefit and medical policy
Positron emission tomography for miscellaneous applications
The safety and effectiveness of positron emission tomography, or PET, scanning have been established. It’s a useful diagnostic option for patients meeting patient selection criteria.
Inclusionary and exclusionary criteria have been updated, effective July 1, 2022.
Inclusions:
PET using 2-[fluorine-18]-fluoro-2-deoxy-D-glucose, or FDG, may be considered established when one of the following are met:
- The assessment of select patients with epileptic seizures who are candidates for surgery
- The diagnosis of chronic osteomyelitis
- One-time evaluation to differentiate between frontotemporal dementia and Alzheimer’s disease when substantial diagnostic uncertainty remains after all the following have been completed:
- Neuropsychological testing
- Evaluation by a physician experienced in neurodegenerative disease
- Structural imaging (CT or MRI)
Exclusions:
The use of FDG-PET is experimental for all other miscellaneous indications not listed in inclusion criteria above including, but not limited to:
CNS diseases
- Autoimmune disorders with CNS manifestations, including:
- Behçet syndrome
- Lupus erythematosus
- Cerebrovascular diseases, including:
- Arterial occlusive disease (arteriosclerosis, atherosclerosis)
- Carotid artery disease
- Cerebral aneurysm
- Cerebrovascular malformations (AVM and Moya-Moya disease)
- Hemorrhage
- Infarct
- Ischemia
- Degenerative motor neuron diseases, including:
- Amyotrophic lateral sclerosis
- Friedreich ataxia
- Olivopontocerebellar atrophy
- Parkinson's disease
- Progressive Supranuclear Palsy
- Shy-Drager syndrome
- Spinocerebellar degeneration
- Steele-Richardson-Olszewski disease
- Tourette syndrome
- Dementias, including:
- Alzheimer disease
- Multi-infarct dementia
- Pick disease
- Dementia with Lewy-Bodies
- Presenile dementia
- Demyelinating diseases, such as multiple sclerosis
- Developmental, congenital, or inherited disorders, including:
- Adrenoleukodystrophy
- Down syndrome
- Huntington chorea
- Kinky-hair disease (Menkes’ syndrome)
- Sturge-Weber syndrome (encephalofacial angiomatosis) and the phakomatoses
- Miscellaneous:
- Chronic fatigue syndrome
- Sick building syndrome
- Post-traumatic stress disorder
- Nutritional or metabolic diseases and disorders, including:
- Acanthocytosis
- Hepatic encephalopathy
- Hepatolenticular degeneration
- Metachromatic leukodystrophy
- Mitochondrial disease
- Subacute necrotizing encephalomyelopathy
- Psychiatric diseases and disorders, including:
- Affective disorders
- Depression
- Obsessive-compulsive disorder
- Psychomotor disorders
- Schizophrenia
- Pyogenic infections, including:
- Aspergillosis
- Encephalitis
- Substance abuse, including the CNS effects of alcohol, cocaine and heroin
- Trauma, including brain injury and carbon monoxide poisoning
- Viral infections, including:
- HIV/AIDS
- AIDS dementia complex
- Creutzfeldt-Jakob syndrome
- Progressive multifocal leukoencephalopathy
- Progressive rubella encephalopathy
- Subacute sclerosing panencephalitis
- Mycobacterium infection
- Migraine
- Anorexia nervosa
- Assessment of cerebral blood flow in newborns:
- Vegetative versus "locked-in" state
Pulmonary diseases
- Adult respiratory distress syndrome
- Diffuse panbronchiolitis
- Emphysema
- Obstructive lung disease
- Pneumonia
Musculoskeletal diseases
- Spondylodiscitis
- Joint replacement follow-up
Other
- Fever of unknown origin
- Giant cell arteritis
- Inflammation of unknown origin
- Inflammatory bowel disease
- Sarcoidosis
- Vascular prosthetic graft infection
- Vasculitis
|
90750 |
Basic benefit and medical policy
Shingrix (zoster vaccine recombinant, adjuvanted)
Shingrix (zoster vaccine recombinant, adjuvanted) is payable for the following updated indications, effective July 29, 2021:
In adults ages 18 and older who are or will be at increased risk of HZ due to immunodeficiency or immunosuppression caused by known disease or therapy. |
95782, 95783, 95800, 95805, 95806, 95807, 95808, 95810, 95811, E0486, G0398, G0399
Experimental
95801, A7047, E0485, E1399, G0400, K1028, K1029
|
Basic benefit and medical policy
Sleep disorders
Polysomnography, or PSG, is an attended (supervised) sleep study (sleep apnea test) performed in a hospital or freestanding sleep laboratory. The safety and effectiveness of PSG, including a split-night PSG, have been established. It may be considered a useful diagnostic option when indicated.
The safety and effectiveness of an unattended sleep study/sleep apnea test with a minimum of three recording channels (using, at a minimum, the following sensors: nasal pressure with chest and abdominal respiratory inductance plethysmography and oximetry; or using Peripheral Arterial Tone, known as PAT, with oximetry and actigraphy) in a home setting (home sleep study/home sleep apnea test) have been established. It may be considered a useful diagnostic option when indicated.
The safety and effectiveness of multiple sleep latency testing, or MSLT, have been established. It may be a useful tool in diagnosing narcolepsy.
Noninvasive pulse oximetry as a sole test (as an alternative to polysomnography or as a cardiorespiratory study for diagnosing sleep related breathing disorders) is considered experimental. Its effectiveness hasn’t been established.
Medical management:
The safety and effectiveness of oral appliances to reduce upper airway collapsibility in the treatment of OSA have been established. An oral appliance may be considered a useful therapeutic option when indicated.
Palate and mandible expansion devices are considered experimental for the treatment of OSA. There is insufficient evidence in the current medical literature to support their efficacy and use in clinical practice.
Nasal expiratory positive airway pressure, known as nasal EPAP, for the treatment of OSA is considered experimental. There is insufficient evidence in the current medical literature to support its efficacy and use in clinical practice.
Oral pressure therapy for the treatment of OSA is considered experimental. There is insufficient medical literature found to support its efficacy.
Positional therapy devices, such as the NightBalance Lunoa SPT system, are considered experimental. They haven’t been proven to be more effective than standard care.
Exclusionary criteria have been updated, effective July 1, 2022.
Inclusionary and exclusionary guidelines:
Diagnosis
Unattended (unsupervised) home sleep study, with a minimum of three recording channels (using, at a minimum, the following sensors: nasal pressure with chest and abdominal respiratory inductance plethysmography and oximetry; or using peripheral arterial tone, known as PAT, with oximetry and actigraphy)
Inclusions:
- Adult patients ages 18 or older with high pretest probability for moderate to severe OSA:
- Observed apneas during sleep, or
- A combination of at least two of the following:
- Excessive daytime sleepiness evidenced by an Epworth sleepiness >10, inappropriate daytime napping (e.g., during driving, conversation or eating), or sleepiness that interferes with daily activities and isn’t explained by other conditions
- Habitual snoring or gasping/choking episodes associated with awakenings
- Treatment-resistant hypertension (persistent hypertension in a patient taking three or more antihypertensive medications)
- Obesity, defined as a body mass index > 35 kg/m2 or neck circumference defined as >17 inches in men or >16 inches in women
- Craniofacial or upper airway soft tissue abnormalities
- Unexplained nocturia
- No exclusions/contraindications to a home sleep study
Exclusions/contraindications:
- Younger than 18 years of age
- Morbid obesity, defined as a body mass index >40 kg/m2 or the patient is 100 pounds over the ideal body weight for their height
- Obesity hypoventilation syndrome
- Narcolepsy
- Periodic limb disorder during sleep
- Central sleep disorder
- Parasomnias
- Nocturnal seizures
- REM behavior disorder
- Moderate or severe congestive heart failure – New York Heart Association class III or IV
- Congestive heart failure with a history of ventricular fibrillation or sustained ventricular tachycardia in a patient who doesn’t have an implanted defibrillator
- Moderate or severe chronic pulmonary disease – forced expiratory volume in 1 second/forced vital capacity (FEV1/FVC) less than or equal to 0.7 and FEV1 less than 80% of predicted
- Documented neuromuscular disease (e.g., Parkinson’s, myotonic dystrophy, ALS)
- History of stroke, severe insomnia or chronic opioid use
- Impairment that results in inability to apply the home sleep testing equipment
- Oxygen dependence
- History of seizures with use of anticonvulsants
- Cardiac conditions
- Restless leg syndrome
Repeat unattended (unsupervised) home sleep study, with a minimum of three recording channels using, at a minimum, the following sensors: nasal pressure with chest and abdominal respiratory inductance plethysmography and oximetry; or using peripheral arterial tone, known as PAT, with oximetry and actigraphy)
Inclusions (one of the following):
- To assess efficacy of surgery or oral appliances or devices
- To re-evaluate the diagnosis of OSA and need for continued continuous positive airway pressure, or CPAP, e.g., if there is a significant change in weight or change in symptoms suggesting that CPAP should be retitrated or possibly discontinued.
Attended (supervised) sleep study performed in a sleep lab
Note: Check our prior authorization program for in-lab sleep testing. All procedures/codes may not be covered by all contracts or certificates.
Adults (ages 18 or older):
Inclusions:
- Adult patients age 18 or older with a moderate to high pretest probability for OSA
- Observed apneas during sleep, or
- A combination of at least two of the following:
- Excessive daytime sleepiness evidenced by an Epworth sleepiness >10, inappropriate daytime napping (e.g., during driving, conversation or eating), or sleepiness that interferes with daily activities and is not explained by other conditions
- Habitual snoring or gasping/choking episodes associated with awakenings
- Treatment-resistant hypertension (persistent hypertension in a patient taking three or more antihypertensive medications)
- Obesity, defined as a body mass index (BMI) >35 kg/m2 or neck circumference > 17 inches in men or >16 inches in women
- Craniofacial or upper airway soft tissue abnormalities
- Unexplained nocturia
- When unattended (unsupervised) home sleep study is contraindicated (see exclusions/contraindications to unattended home sleep study above)
- When the initial unattended (unsupervised) study was negative, inadequate, equivocal or non-diagnostic and clinical suspicion for OSA remains
Children (younger than age 18)
Inclusions:
- Pediatric patients younger than age 18 with a moderate to high probability of OSA and one of the following:
- Habitual snoring in association with one or more of criteria below:
- Restless or disturbed sleep
- Behavioral disturbance or learning disorders including deterioration in academic performance, attention deficit disorder, hyperactivity
- Frequent awakenings
- Enuresis (bedwetting)
- Growth retardation or failure to thrive; OR
- Excessive daytime somnolence or altered mental status not explained by other conditions
- Polycythemia not explained by other conditions
- Cor pulmonale not explained by other conditions
- Witnessed apnea with duration greater than two respiratory cycles
- Labored breathing during sleep
- Hypertrophy of the tonsils or adenoids in patients at significant surgical risk such that the exclusion of OSA would allow avoidance of surgery
- Suspected congenital central alveolar hypoventilation syndrome or sleep-related hypoventilation due to neuromuscular disease or chest wall deformities
- Clinical evidence of a sleep-related breathing disorder in infants who have experienced an apparent life-threatening event
- For exclusion of OSA in a patient who’s undergone adenotonsillectomy for suspected OSA more than eight weeks previously
Repeated (attended) sleep study performed in a sleep lab:
Inclusions:
- Equipment failure or less than six hours of recording
- Initial PSG is negative and a clinical suspicion of OSA remains
- To initiate and titrate CPAP in adult patients who have one of the following:
- An AHI or RDI of at least 15 events per hour
- An AHI or RDI of at least five events per hour in a patient with excessive daytime sleepiness or unexplained hypertension.
Note: A split-night study, in which moderate to severe OSA is documented during the first portion of the study using PSG, followed by CPAP during the second portion of the study, can eliminate the need for a second study to titrate CPAP.
- To initiate and titrate CPAP in children:
- In pediatric patients, an AHI greater than 1.5 is considered abnormal, and an AHI of 10 or more may be considered severe.
- To re-evaluate the diagnosis of OSA and need for continued CPAP (e.g., if there is a significant change in weight or change in symptoms suggesting that CPAP should be retitrated or possibly discontinued).
Note: This statement doesn’t imply that supervised studies are needed routinely following unattended studies. This statement means a re-evaluation based on a substantial change in symptoms or in the clinical situation.
- To assess efficacy of surgery (including adenotonsillectomy) or oral appliances/devices
- For patients younger than age 18 and initial study was inadequate, equivocal or non-diagnostic and the child’s parents or caregiver report that the breathing patterns observed at home were different from those during testing.
Mutliple sleep latency testing, or MSLT
MSLT is considered experimental to diagnose obstructive sleep apnea except to exclude or confirm narcolepsy in the diagnostic workup of OSA syndrome.
Nonivasive pulse oximetry
The effectiveness of noninvasive pulse oximetry as a sole test (as an alternative to polysomnography or as a cardiorespiratory study for diagnosing sleep related breathing disorders) is considered experimental. Its effectiveness hasn’t been established.
Medical management
Pap therapies, i.e., continuous positive airway pressure, known as CPAP; automatic positive airway pressure, or APAP; bilevel positive airway pressure, or BiPAP; and variable positive airway pressure, or VPAP, may be considered medically necessary for the management of OSA, central sleep apnea or mixed apnea. These devices for treatment are addressed in policy titled “Positive Pressure Airway Devices.”
Oral appliances for OSA (e.g., tongue-retaining devices or mandibular orthopedic positioning devices), may be considered established in adult patients with clinically significant OSA. (Verify coverage of intraoral appliances under the DME benefit.)
Definition of an oral appliance for OSA
- A custom-fabricated appliance, using digital or physical impressions and models of an individual patient’s oral structures and physical needs
- Not a prefabricated item that is modified. Prefabricated components may be included in the final appliance.
- Includes all appliances, including titration appliances
- Made of biocompatible materials
- Engages the maxillary and mandibular arches
- Includes a mechanism that advances the mandible in increments of 1 mm or less with a protrusive adjustment range of at least 5 mm. This mechanism may or may not include fixed mechanical hinges or metallic materials.
- Reversal of the advancement is possible
- The protrusive setting must be verifiable
An appropriate oral appliance will allow for optimal protrusion of the mandible (e.g., less than 5 mm) to produce the desired relative opening of the airway, without contributing to an increased risk of temporal mandibular joint dysfunction.
Inclusions (all of the following):
- OSA, as defined by one of the following:
- An AHI, RDI or REI of at least 15 events per hour
- An AHI, RDI or REI of at least five events per hour in a patient with excessive daytime sleepiness, impaired cognition, mood disorders, insomnia, hypertension, ischemic heart disease or history of stroke
- A trial of CPAP has failed, isn’t tolerated by the patient or is contraindicated.
- The device is prescribed by the treating physician.
- The device is custom-fitted by a dentist (preferably a dentist with certification/additional training in dental sleep medicine).
- There is a dental evaluation that documents the absence of both temporomandibular dysfunction and periodontal disease.
- Impressions, models, fabrication, materials, insertion/fitting, training, subsequent adjustments/modifications of the appliance, repairs and ancillary appliances are included with the OSA appliance and aren’t separately billable for the first 90 days after provision of the oral appliance.
Replacement of an oral appliance may be considered at the end of the five-year reasonable useful lifetime, or RUL, or prior, if there;s a change in the patient’s condition.
Exclusions:
- Prefabricated (not custom-fit) devices (e.g., sport mouth guards, mouth guards that can be purchased in a retail store or pharmacy)
- Screening tests (e.g., questionnaire, pulse oximetry, rhinometry, and laryngometry, etc.) performed by a dentist
The use of an abbreviated daytime sleep session for acclimation to CPAP (PAP-NAP) is considered experimental.
The use of daytime electrical stimulation of the tongue is considered experimental for the treatment of OSA.
Palate and mandible expansion devices are considered experimental.
Nasal expiratory positive airway pressure and oral pressure therapy devices are considered experimental.
Positional therapy devices, such as the NightBalance Lunoa SPT system, are considered experimental. They haven’t been proven to be more effective than standard care.
Policy guidelines:
Polysomnography or home sleep apnea testing is ordered by a physician or qualified health care provider who has evaluated the patient and is managing the medical care of the patient, i.e., either a primary care physician or a specialist. Following the review of the sleep study results, recommendations for the most appropriate medical treatment may be made by the treating physician or qualified health care provider, or may be a collaborative effort between the treating physician or qualified health care provider and the board-certified sleep medicine physician who interprets the results of the testing.
Facility/provider requirements:
If an attended sleep study is performed in a non-hospital-based sleep laboratory, the laboratory must be accredited by the American Academy of Sleep Medicine.
An attended sleep study in a hospital-based sleep testing center must be accredited by AASM or an accreditation organization accepted under the Participating Hospital Agreement.
To perform and receive reimbursement for in-center and out-of-center sleep testing, a physician must be board-certified in sleep medicine by the American Board of Medical Specialties or the American Board of Sleep Medicine. Any M.D. or D.O. may order a sleep test; however, it must be performed and interpreted by a physician who is board-certified in sleep medicine.
The technician performing the sleep testing must have one of the following certifications:
- American Board of Sleep Medicine, Registered Sleep Technologist
- Board of Registered Polysomnographic Technologists, Registered Polysomnographic Technologist
- National Board for Respiratory Care (any of the following):
- Certified pulmonary function technologist
- Registered pulmonary function technologist
- Certified respiratory therapist
- Registered respiratory therapist
Treatment of patients diagnosed with OSA should be initiated and monitored by a physician who is board-certified in sleep medicine. It’s important to monitor symptoms and adherence to positive airway pressure, or PAP, treatment (e.g., review of symptoms and device utilization at 90 days with a minimum of four hours per night for at least five nights per week).
Risk factors for OSA:
Although not an exclusive list, patients with all four of the following symptoms are considered to be at high risk for obstructive sleep apnea:
- Habitual snoring
- Observed apneas
- Excessive daytime sleepiness
- A body mass index greater than 35 kg/m2
If no bed partner is available to report snoring or observed apneas, other signs and symptoms suggestive of OSA (e.g., age of the patient, male gender, thick neck, craniofacial or upper airway soft tissue abnormalities or unexplained hypertension) may be considered. Objective clinical prediction rules are being developed; however, at present, risk assessment is based primarily on clinical judgment.
The STOP-BANG questionnaire is a method developed for non-sleep specialists to assess the signs and symptoms of OSA (Snore, Tired, Observed apnea, blood Pressure, BMI, Age, Neck, Gender) and has been shown to have 97% sensitivity and 96% negative predictive value (specificity, 33%) for the identification of patients with severe OSA (Apnea/Hypopnea Index score >30 events per hour). Overnight oximetry has been used by some sleep specialists as a component of the risk assessment but isn’t adequate for the diagnosis of OSA. Therefore, a follow-up polysomnography, or PSG, or home sleep study/home sleep apnea test would still be required to confirm or exclude a diagnosis of OSA.
OSA in children:
The presentation of OSA in children may differ from that of adults. Children frequently exhibit behavioral problems or hyperactivity rather than daytime sleepiness. Obesity is defined as a body mass index greater than the 90th percentile for the weight/height ratio. Although the definition of severe OSA in children isn’t well established, an AHI or RDI greater than 1.5 events per hour is considered abnormal (an AHI or RDI of >10 events per hour may be considered severe). In addition, the first-line treatment in children is usually adenotonsillectomy. Continuous positive airway pressure is an option for children who aren’t candidates for surgery or who have an inadequate response to surgery.
Bariatric surgery patients:
Screening for OSA should be performed routinely in patients scheduled for bariatric surgery, due to the high prevalence of OSA in this population. The optimal screening approach isn’t certain. An in-laboratory PSG or home sleep study/home sleep apnea test is the most accurate screening method. Some experts recommend a symptom-based screening instrument, followed by PSG in patients who exceed a certain threshold, as an alternative to performing PSG in all patients. It should be noted that there is a high prevalence of obesity hypoventilation syndrome in patients who are candidates for bariatric surgery. Therefore, obesity hypoventilation syndrome should be ruled out prior to home sleep testing in this population.
Significant weight change:
There’s no established threshold for significant change in weight. Studies have reported improvements in OSA with an average weight loss of 20 kg or 20% of body weight.
Multiple sleep latency test:
The multiple sleep latency test, or MSLT, is an objective measure of the tendency to fall asleep in the absence of alerting factors, while the maintenance of wakefulness test, or MWT, is an objective measure of the ability to stay awake under soporific conditions (used to assess occupational safety). The MSLT and MWT aren’t routinely indicated in the evaluation and diagnosis of OSA or in assessment of change following treatment with CPAP. The MSLT may be indicated as part of the evaluation of patients with suspected narcolepsy to confirm the diagnosis (often characterized by cataplexy, sleep paralysis, and hypnagogic/hypnopompic hallucinations) or to differentiate between suspected idiopathic hypersomnia and narcolepsy. Narcolepsy and OSA can co-occur. Because it’s not possible to differentiate the excessive sleepiness caused by OSA and narcolepsy, OSA should be treated before confirming a diagnosis of narcolepsy with the MSLT.
Split-night studies:
American Academy of Sleep Medicine practice parameters indicate that a split-night study (initial diagnostic PSG followed by CPAP titration during PSG on the same night) is an alternative to one full night of diagnostic PSG followed by a second night of titration if the following four criteria are met:
- An AHI of at least 40 is documented during a minimum of two hours of diagnostic PSG. Split-night studies may sometimes be considered at an AHI of 20 to 40 events per hour, based on clinical judgment (e.g., if there are also repetitive long obstructions and major desaturations). However, at AHI values below 40, determination of CPAP-level requirements, based on split-night studies, may be less accurate than in full-night calibrations.
- CPAP titration is carried out for more than three hours (because respiratory events can worsen as the night progresses).
- PSG documents that CPAP eliminates or nearly eliminates the respiratory events during rapid eye movement and non-REM sleep, including REM sleep with the patient in the supine position.
- A second full night of PSG for CPAP titration is performed if the diagnosis of a sleep-related breathing disorder, or SRBD, is confirmed, but criteria b and c aren’t met.
|
97810, 97811, 97813, 97814
Experimental:
20560, 20561
|
Basic benefit and medical policy
Acupuncture
The safety and effectiveness of acupuncture have been established for a narrow range of medical conditions. It may be considered a useful therapeutic option when specific indications are met.
Other uses of acupuncture are considered experimental. While acupuncture may be considered safe, it hasn’t been demonstrated to be more effective than conventional treatment for these other (multiple) proposed uses. This policy is effective July 1, 2022.
Basic benefit policy group variations:
Acupuncture isn’t covered for most groups. Reference member benefits prior to service.
Inclusions:
Acupuncture (manual or electroacupuncture) may be considered medically necessary when an individual has been referred by their treating physician to a licensed acupuncturist for the treatment of any of the following:
- Chronica non-specific low back pain
- Chronica neck pain
- Episodic migraines
- Tension-type headaches
- Prevention of chemotherapy associated nausea and vomiting
- Pregnancy induced nausea or vomiting
aUnresolved pain that has been persistent for at least 12 weeks
Exclusions:
- Acupuncture point injection
- Dry needling
- Acupuncture for/when:
- Opioid reduction or cessation in opiate users
- Maintenance care (therapeutic goals of the treatment program have been reached)
- No further significant progress has been achieved or is reasonably expected to occur
- Other uses not mentioned in inclusions
|
99281, 99282, 99283, 99284, 99285 |
Basic benefit and medical policy
Emergency medical services
The provision of emergency medical services as defined by the Emergency Medical Treatment and Labor Act and American College of Emergency Physicians are considered established. This policy is effective July 1, 2022.
Inclusions:
Visits for a medical condition with acute symptoms of sufficient severity (including severe pain) that could cause a prudent layperson with average knowledge of health and medicine to reasonably expect that the absence of immediate medical attention would result in one of the following:
- Health of the patient (or with respect to a pregnant woman, the health of the woman or her unborn child) to be in serious jeopardy
- Serious impairment to bodily function
- Serious dysfunction of any bodily organ or part
- Visits for a psychiatric (behavioral health) condition of sufficient severity where the patient is at immediate risk of self-harm or immediate risk of harm to another person.
Exclusions:
- Routine follow-up of previous emergency room visit.
- Visits where signs and symptoms haven’t worsened to a level that emergent care is required.
- Visit for evaluation of signs, symptoms where appropriate care could have been provided in a setting of lower acuity than an emergency room (e.g., primary care provider’s office or urgent care center).
|
A7030-A7039, A7046, E0470, E0471, E0472, E0561, E0562, E0601 |
Basic benefit and medical policy
Positive pressure airway devices
Positive pressure airway devices are considered safe, effective and useful therapeutic options for the management of obstructive sleep apnea, central sleep apnea or mixed apnea.
Inclusionary and exclusionary criteria have been updated, effective July 1, 2022.
Inclusions:
Auto-adjusting positive airway pressure, or APAP, is considered established for the titration of pressure in adults with clinically significant OSA defined as those who have one of the following:
- An AHI, RDI or Respiratory Event Index, or REI, of at least 15 events per hour
- An AHI, RDI or REI of at least five events per hour in a patient with one or more signs or symptoms associated with OSA (e.g., excessive daytime sleepiness, hypertension, cardiovascular heart disease, or stroke)
- If there’s a significant change in weight or change in symptoms suggesting that CPAP should be re-titrated or possibly discontinued.
Continuous positive airway pressure, or CPAP, is considered established in adult or pediatric patients with clinically significant OSA.
Clinically significant OSA in adults is (one of the following):
- An AHI, RDI or REI ≥15
- An AHI, RDI, or REI ≥5 in a patient with one or more signs or symptoms associated with OSA (e.g., excessive daytime sleepiness, hypertension, cardiovascular heart disease, or stroke)
In pediatric patients (ages 1-17), one of the following:
- An AHI or RDI ≥5
- An AHI or RDI ≥1.5 in a patient with excessive daytime sleepiness, behavioral problems or hyperactivity
Bilevel positive airway pressure, or BiPAP/variable Positive Airway Pressure, or VPAP, or APAP is considered established in both pediatric and adult patients with clinically significant OSA who have failed a prior trial of CPAP or for whom bilevel positive airway pressure is found to be more effective in the sleep lab.
Central sleep apnea:
- Polysomnogram with more than five central apneas per hour of sleep lasting 10 seconds or longer
- Polysomnogram with the presence of at least 10 central events per hour of sleep in the crescendo-decrescendo pattern
Note: CPAP has been shown to have greater effectiveness than oral appliances in general. This difference in efficacy is more pronounced for patients with severe OSA, because oral appliances have been shown to be less efficacious in patients with severe OSA than in patients with mild-to-moderate OSA. Therefore, it’s particularly important that patients with severe OSA have an initial trial of CPAP and that all reasonable attempts are made to continue treatment with CPAP prior to the decision to switch to an oral appliance.
Exclusions:
- Diagnosis of snoring without sleep apnea
- The use of CPAP, BiPAP/VPAP and APAP that don’t meet the above criteria is considered investigational for the treatment of OSA.
|
C9399, J3490, J3590, J9999 |
Basic benefit and medical policy
Opdualag (nivolumab and relatlimab-rmbw)
Opdualag (nivolumab and relatlimab-rmbw) is payable for the FDA-approved indications, effective March 18, 2022.
Opdualag is a combination of nivolumab, a programmed death receptor-1 (PD-1) blocking antibody, and relatlimab, a lymphocyte activation gene-3 (LAG-3) blocking antibody, indicated for the treatment of adult and pediatric patients ages 12 or older with unresectable or metastatic melanoma.
Dosage and administration:
- Adult patients and pediatric patients 12 years of age or older who weigh at least 40 kg: 480 mg nivolumab and 160 mg relatlimab intravenously every four weeks.
- Administer Opdualag as an intravenous infusion over 30 minutes.
Dosage forms and strengths:
- Injection: 240 mg of nivolumab and 80 mg of relatlimab per 20 mL (12 mg and 4 mg per mL) in a single-dose vial.
Opdualag (nivolumab and relatlimab-rmbw) isn’t a benefit for URMBT. |
J0875 |
Basic benefit and medical policy
Dalvance (dalbavancin)
Effective July 22, 2021, Dalvance (dalbavancin) is covered for the following FDA-approved indications:
Dalvance is a lipoglycopeptide antibacterial indicated for the treatment of adult and pediatric patients with acute bacterial skin and skin structure infections, or ABSSSI, caused by designated susceptible strains of gram-positive microorganisms.
Dosage and administration:
Dosage in pediatric patients with CLcr 30 mL/min/1.73m2 and above:
- Age range: Birth to less than 6 years. Dosage (single dose regimen): 22.5 mg/kg (maximum of 1500 mg)
- Age range: 6 to less than 18 years. Dosage (single dose regimen): 18 mg/kg (maximum of 1500 mg)
Dosage adjustment in pediatric patients with CLcr less than 30 mL/min hasn’t been studied. |
J1599 |
Basic benefit and medical policy
Cutaquig (immune globulin subcutaneous [human]-hipp)
Effective Nov. 1, 2021, Cutaquig (immune globulin subcutaneous [human]-hipp) is covered for the following FDA-approved indications:
Cutaquig (immune globulin subcutaneous [human]-hipp) is a 16.5% immune globulin solution for subcutaneous infusion indicated for treatment of primary humoral immunodeficiency in adults and pediatric patients ages 2 and older.
Dosage information:
For subcutaneous use only.
Before switching to Cutaquig, obtain the patient’s serum IgG trough level to guide subsequent dose adjustments.
Dose:
- Switching from immune globulin intravenous, or IGIV, to Cutaquig: Calculate the dosing by using a dose conversion factor (1.30).
- Switching from other immune globulin subcutaneous, or IGSC: Dosing should be the same as for previous IGSC.
- Weekly: Start Cutaquig one week after last IGIV infusion
Initial weekly dose = Previous IGIV dose (in grams) x 1.30
Number of weeks between IGIV doses
- Every other week: Start Cutaquig one or two weeks after the last IGIV dosing or one week after the last IGSC administration. Infuse twice the calculated weekly dose.
- More frequent than weekly (two to seven times a week): Start Cutaquig one week after last IGIV or IGSC administration. Divide the calculated weekly dose by the desired number of infusions per week.
- Adjust dosing according to patient’s pharmacokinetics and clinical response
Administration:
Administer at regular interval from daily up to every other week. Infusion rate and infusion volume per site may gradually be increased every two to four weeks as tolerated by patients.
Infusion parameters:*
Volume (mL/site):
- For ages 7-17 – Initial two infusions are ≤ 15. Subsequent infusions gradually increase by approximately 5-10 mL/site every two to four weeks up to a maximum of 29
- For ages 2-6 years – Initial two infusions are ≤ 10. Subsequent infusions gradually increase by approximately 5-10 mL/site every two to four eeks up to a maximum of 15.5
Rate (mL/hr/site):
- For children ages 2-17 – Initial two infusions are ≤ 15. Subsequent infusions gradually increase by approximately 10 mL/hr/site every two to four weeks up to a maximum of 25
*As tolerated
Infusion sites: Up to six infusion sites simultaneously, with at least two inches between sites. Rotate sites for each administration. |
J3490, J3590 |
Basic benefit and medical policy
Apretude (cabotegravir)
Effective Dec. 20, 2021, Apretude (cabotegravir) is covered for the following FDA-approved indications:
Apretude (cabotegravir) is an HIV-1 integrase strand transfer inhibitor, or INSTI, indicated in at-risk adults and adolescents weighing at least 35 kg for PrEP to reduce the risk of sexually acquired HIV-1 infection. Individuals must have a negative HIV-1 test prior to initiating Apretude (with or without an oral lead-in with oral cabotegravir) for HIV-1 PrEP.
Dosage and administration:
- HIV-1 screening: Screen all individuals for HIV-1 infection immediately prior to initiating Apretude for HIV-1 PrEP and prior to each injection while taking Apretude.
- Prior to initiating Apretude, an oral lead-in dosing may be used for approximately one month with the recommended dosage to assess the tolerability of Apretude.
- For gluteal intramuscular injection only.
- Recommended dosing schedule: Initiate Apretude with a single 600 mg (3 mL) injection given one month apart for two consecutive months on the last day of an oral lead-in if used or within three days and continue with the injections every two months thereafter.
Dosage forms and strengths:
Injection: Single-dose vial of 600 mg/3 mL (200 mg/mL) of cabotegravir extended-release injectable suspension.
This drug isn’t a benefit for URMBT. |
J3490
J3590 |
Basic benefit and medical policy
Dapzura RT (daptomycin)
Effective Jan. 25, 2022, Dapzura RT (daptomycin) is covered for the following FDA-approved indications:
Dapzura RT is a lipopeptide antibacterial indicated for the treatment of:
- Complicated skin and skin structure infections (cSSSI) in adult and pediatric patients (ages 1 to 17)
- Staphylococcus aureus bloodstream infections (bacteremia), in adult patients including those with right-sided infective endocarditis
- Staphylococcus aureus bloodstream infections (bacteremia) in pediatric patients (ages 1 to 17 years)
Limitations of use:
- Dapzura RT isn’t indicated for the treatment of pneumonia.
- Dapzura RT isn’t indicated for the treatment of left-sided infective endocarditis due to S. aureus.
- Dapzura RT isn’t recommended in pediatric patients younger than age 1 due to the risk of potential effects on muscular, neuromuscular, and/or nervous systems (either peripheral and/or central) observed in neonatal dogs.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Dapzura RT and other antibacterial drugs, Dapzura RT should be used to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
Dosage information:
Adult patients
- Administer to adult patients intravenously in 0.9% sodium chloride, either by injection over a 2-minute period or by infusion over a 30-minute period.
- Recommended dosage regimen for adult patients:
- Creatinine clearance, or CLCR: ≥30 mL/min
- Dosage regimen for cSSSI: For seven to 14 days, 4 mg/kg once every 24 hours
- Dosage regimen for S. aureus bacteremia: For two to six weeks, 6 mg/kg once every 24 hours
- Creatinine clearance, or CLCR: <30 mL/min, including hemodialysis and CAPD
- Dosage regimen: 4 mg/kg once every 48 hours**
- Dosage regimen for S. aureus bacteremia: For two to six weeks, 6 mg/kg once every 48 hours**
**Administered following hemodialysis on hemodialysis days.
Pediatric patients
- Unlike in adults, don’t administer by injection over a two minute period to pediatric patients.
- Administer to pediatric patients intravenously in 0.9% sodium chloride, by infusion over a 30- or 60-minute period, based on age.
- Recommended dosage regimen for pediatric patients (ages 1 to 17) with cSSSI, based on age:
- Age group 12 to 17 years: Dosage is 5 mg/kg once every 24 hours infused over 30 minutes.** Duration of therapy is up to 14 days.
- Age group 7 to 11 years: Dosage is 7 mg/kg once every 24 hours infused over 30 minutes.** Duration of therapy is up to 14 days.
- Age group 2 to 6 years: Dosage is 9 mg/kg once every 24 hours infused over 60 minutes.** Duration of therapy is up to 14 days.
- Age group 1 to less than 2 years: Dosage is 10 mg/kg once every 24 hours infused over 60 minutes.** Duration of therapy is up to 14 days.
**Recommended dosage is for pediatric patients (ages 1 to 17) with normal renal function. Dosage adjustment for pediatric patients with renal impairment hasn’t been established.
- Recommended dosage regimen for pediatric patients (ages 1 to 17) with S. aureus bacteremia, based on age:
- Age group 12 to 17 years: Dosage is 7 mg/kg once every 24 hours infused over 30 minutes.** Duration of therapy is up to 42 days
- Age group 7 to 11 years: Dosage is 9 mg/kg once every 24 hours infused over 30 minutes.** Duration of therapy is up to 42 days
- Age group 1 to 6 years: Dosage is 12 mg/kg once every 24 hours infused over 60 minutes.** Duration of therapy is up to 42 days
**Recommended dosage is for pediatric patients (1 to 17 years of age) with normal renal function. Dosage adjustment for pediatric patients with renal impairment hasn’t been established.
- There are other formulations of daptomycin that have differences concerning storage and reconstitution.
- Don’t use in conjunction with ReadyMED® elastomeric infusion pumps in adult and pediatric patients.
Dosage forms and strengths:
For injection: 500 mg lyophilized powder for reconstitution in a single-dose vial
Dapzura RT (daptomycin) isn’t a benefit for URMBT. |
J3490, J3590, J9999 |
Basic benefit and medical policy
Kimmtrak (tebentafusp-tebn)
Effective Jan. 25, 2022, Kimmtrak (tebentafusp-tebn) is covered for the following FDA-approved indications:
Kimmtrak is a bispecific gp100 peptide-HLA-directed CD3 T cell engager indicated for the treatment of
HLA-A 02:01-positive adult patients with unresectable or metastatic uveal melanoma.
Dosage and administration:
- Recommended dosage: 20 mcg intravenously on Day 1, 30 mcg intravenously on Day 8, 68 mcg intravenously on Day 15, and 68 mcg intravenously once every week thereafter.
- Dilute and administer by intravenous infusion over 15 to 20 minutes.
- Dosage interruption or permanent discontinuation may be required based on individual safety and tolerability.
Dosage forms and strengths:
Injection: 100 mcg/0.5 mL solution in a single-dose vial
This drug isn’t a benefit for URMBT. |
J3490, J3590 |
Basic benefit and medical policy
Leqvio (inclisiran)
Effective Dec. 22, 2021, Leqvio (inclisiran) is covered for the following FDA-approved indications:
Leqvio is a small interfering RNA, or siRNA, directed to PCSK9, known as proprotein convertase subtilisin kexin type 9, mRNA indicated as an adjunct to diet and maximally tolerated statin therapy for the treatment of adults with heterozygous familial hypercholesterolemia, or HeFH, or clinical atherosclerotic cardiovascular disease, or ASCVD, who require additional lowering of low-density lipoprotein cholesterol, or LDL-C.
Limitations of use:
The effect of Leqvio on cardiovascular morbidity and mortality hasn’t been determined.
Dosage and administration:
- The recommended dosage of Leqvio, in combination with maximally tolerated statin therapy, is 284 mg administered as a single subcutaneous injection initially, again at three months and then every six months.
- Leqvio should be administered by a health care professional.
- Inject Leqvio subcutaneously into the abdomen, upper arm or thigh.
Dosage forms and strengths:
Injection: 284 mg/1.5 mL (189 mg/mL) in a single-dose prefilled syringe
This drug is not a benefit for URMBT. |
J3490, J3590 |
Basic benefit and medical policy
PreHevbrio hepatitis B vaccine (recombinant)
Effective Nov. 1, 2021, PreHevbrio hepatitis B vaccine (recombinant) is covered for the following FDA-approved indications:
PreHevbrio hepatitis B vaccine (recombinant) is indicated for prevention of infection caused by all known subtypes of hepatitis B virus. PreHevbrio is approved for use in adults 18 years of age and older.
Dosage and administration:
For intramuscular injection.
Administer a series of three doses (1.0 mL each) of PreHevbrio on a 0-, 1- and 6-month schedule.
Dosage forms and strengths:
PreHevbrio is an injectable suspension, for intramuscular use supplied as a single-dose vial. A single dose of PreHevbrio is 1.0 mL. |
J3490, J3590 |
Basic benefit and medical policy
Tezspire (tezepelumab-ekko)
Effective Dec. 17, 2021, Tezspire (tezepelumab-ekko) is covered for the following FDA-approved indications:
Tezspire is a thymic stromal lymphopoietin, or TSLP, blocker, human monoclonal antibody (IgG2λ), indicated for the add-on maintenance treatment of adult and pediatric patients ages 12 years and older with severe asthma.
Limitations of use:
Not for relief of acute bronchospasm or status asthmaticus.
Dosage information:
- Administer by subcutaneous injection.
- Recommended dosage is 210 mg administered once every four weeks.
Dosage forms and strengths:
- 210 mg/1.91 mL (110 mg/mL) solution in a single-dose glass vial
- 210 mg/1.91 mL (110 mg/mL) solution in a single-dose pre-filled syringe
Tezspire (tezepelumab-ekko) isn’t a benefit for URMBT.
|
J3490, J3590 |
Basic benefit and medical policy
Vyvgart (efgartigimod alfa-fcab)
Effective Dec. 17, 2021, Vyvgart (efgartigimod alfa-fcab) is covered for the following FDA-approved indications:
- Vyvgart is a neonatal Fc receptor blocker indicated for the treatment of generalized myasthenia gravis, or gMG, in adult patients who are anti-acetylcholine receptor, or AChR, antibody positive.
Dosage and administration:
- Evaluate the need to administer age-appropriate vaccines according to immunization guidelines before initiation of a new treatment cycle with Vyvgart.
- The recommended dosage is 10 mg/kg administered as an intravenous infusion over one hour once weekly for four weeks.
- In patients weighing 120 kg or more, the recommended dose is 1200 mg per infusion.
- Administer subsequent treatment cycles based on clinical evaluation, the safety of initiating subsequent cycles sooner than 50 days from the start of the previous treatment cycle hasn’t been established.
- Must be diluted with 0.9% sodium chloride injection, USP prior to administration.
- Administer as an intravenous infusion over one hour via a 0.2 micron in-line filter.
Dosage forms and strengths:
- Injection: 400 mg in 20 mL (20 mg/mL) single-dose vial.
This drug isn’t a benefit for URMBT.
|
J9144 |
Basic benefit and medical policy
Darzalex Faspro (daratumumab and hyaluronidase-fihj)
Effective Nov. 30, 2021, Darzalex Faspro (daratumumab and hyaluronidase-fihj) is covered for the following FDA-approved indications:
Darzalex Faspro is a combination of daratumumab, a CD38-directed cytolytic antibody, and hyaluronidase, an endoglycosidase, indicated for the treatment of adult patients with:
- Multiple myeloma in combination with carfilzomib and dexamethasone in patients with relapsed or refractory multiple myeloma who have received one to three prior lines of therapy
Dosage information:
For subcutaneous use only.
- Pre-medicate with a corticosteroid, acetaminophen and a histamine-1 receptor antagonist
- The recommended dosage of Darzalex Faspro is (1,800 mg daratumumab and 30,000 units hyaluronidase) administered subcutaneously into the abdomen over approximately three to five minutes according to recommended schedule.
- Administer post-medications as recommended.
|
J9145 |
Basic benefit and medical policy
Darzalex (daratumumab)
Darzalex (daratumumab) is payable for the
following updated FDA-approved indications:
Darzalex is a CD38-directed cytolytic antibody indicated for the treatment of adult patients with multiple myeloma:
- Treatment of adult patients with light chain amyloidosis in combination with bortezomib, cyclophosphamide and dexamethasone in newly diagnosed patients
Dosage information:
- Pre-medicate with corticosteroids, antipyretics and antihistamines.
- Dilute and administer as an intravenous infusion.
- Recommended dose is 16 mg/kg actual body weight.
- Administer post-infusion medications.
|
J9271 |
Basic benefit and medical policy
Keytruda (pembrolizumab)
Effective Dec. 3, 2021, Keytruda (pembrolizumab) is covered for the following updated FDA-approved indications:
Keytruda (pembrolizumab) is a programmed death receptor-1 (PD-1)-blocking antibody indicated for:
Urothelial carcinoma
- For the treatment of patients with locally advanced or metastatic urothelial carcinoma who meet one of the following:
- Aren’t eligible for any platinum-containing chemotherapy
- Who have disease progression during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy
- Or the treatment of patients with Bacillus Calmette-Guerin, or BCG, unresponsive, high-risk, non-muscle invasive bladder cancer, or NMIBC, with carcinoma in situ, or CIS, with or without papillary tumors who are ineligible for or have elected not to undergo cystectomy
Cervical cancer
- In combination with chemotherapy, with or without bevacizumab, for the treatment of patients with persistent, recurrent, or metastatic cervical cancer whose tumors express PD-L1 (CPS ≥1) as determined by an FDA-approved test
- As a single agent for the treatment of patients with recurrent or metastatic cervical cancer with disease progression on or after chemotherapy whose tumors express PD-L1 (CPS ≥1) as determined by an FDA-approved test. (Clarified indication underlined.)
Renal cell carcinoma, or RCC
- In combination with axitinib, for the first-line treatment of patients with advanced RCC
- In combination with lenvatinib, for the first-line treatment of adult patients with advanced RCC
- For the adjuvant treatment of patients with RCC at intermediate-high or high risk of recurrence following nephrectomy, or following nephrectomy and resection of metastatic lesions
Melanoma
- For the treatment of patients with unresectable or metastatic melanoma
- For the adjuvant treatment of adult and pediatric (12 years and older) patients with Stage IIB, IIC, or III melanoma following complete resection
Dosage and administration:
- Urothelial carcinoma: 200 mg every three weeks or 400 mg every six weeks
- Cervical cancer: 200 mg every three weeks or 400 mg every six weeks
- Renal cell carcinoma: 200 mg every three weeks or 400 mg every six weeks as a single agent in the adjuvant setting, or in the advanced setting with one of the following:
- Axitinib 5 mg orally twice daily
- Lenvatinib 20 mg orally once daily
- Melanoma: 200 mg every three weeks or 400 mg every six weeks.
|
J9299 |
Basic benefit and medical policy
Opdivo (nivolumab)
Effective July 23, 2021, Opdivo (nivolumab) is payable for the following updated FDA-approved indications:
Opdivo (nivolumab) is a programmed death receptor-1 (PD-1)-blocking antibody indicated for the treatment of:
- Hepatocellular carcinoma: Patients with hepatocellular carcinoma who have been previously treated with sorafenib in combination with ipilimumab.
Dosage and administration:
Hepatocellular carcinoma: 1 mg/kg followed by ipilimumab 3 mg/kg on the same day every three weeks for four doses, then 240 mg every two weeks or 480 mg every four weeks. |
J9312, Q5115, Q5119, Q5123 |
Basic benefit and medical policy
Rituxan (rituximab), Truxima (rituximab-abbs), Ruxience (rituximab-pvvr) and Riabni (rituximab-arrx)
Effective Dec. 2, 2021, Rituxan (rituximab), Truxima (rituximab-abbs), Ruxience (rituximab-pvvr) and Riabni (rituximab-arrx) are payable for the following updated FDA-approved indications:
- Pediatric patients ages 6 months and older with mature B-cell NHL and mature B-cell acute leukemia (B-AL):
- Previously untreated, advanced stage, CD20-positive, diffuse large B-cell lymphoma, Burkitt lymphoma, Burkitt-like lymphoma or mature B-cell acute leukemia in combination with chemotherapy.
|
Q5119 |
Basic benefit and medical policy
Ruxience (rituximab-pvvr)
Effective Nov. 15, 2021, Ruxience (rituximab-pvvr) is covered for the following FDA-approved indications:
Ruxience (rituximab-pvvr) is a CD20-directed cytolytic antibody indicated for the treatment of:
- Adult patients with non-Hodgkin lymphoma, or NHL
- Adult patients with chronic lymphocytic leukemia, or CLL
- Rheumatoid arthritis, or RA, in combination with methotrexate in adult patients with moderately to severely active RA who have inadequate response to one or more TNF antagonist therapies.
Dosage and administration:
- The dose for NHL is 375 mg/m2.
- The dose for CLL is 375 mg/m2 in the first cycle and 500 mg/m2 in cycles 2-6, in combination with FC, administered every 28 days.
- The dose for RA in combination with methotrexate is two 1,000 mg intravenous infusions separated by two weeks (one course) every 24 weeks or based on clinical evaluation, but not sooner than every 16 weeks. Methylprednisolone 100 mg intravenous or equivalent glucocorticoid is recommended 30 minutes prior to each infusion.
|
| GROUP BENEFIT CHANGES |
Ford Motor Company hourly employees |
Retroactive to Jan. 1, 2022, allergy serum is covered under the medical plan for Ford Motor Company hourly employees, group numbers 87950 and 87951.
Group numbers: 87950 and 87951
Alpha prefix: FGP and FBP
Platform: NASCO |
Valeo |
Valeo, group number 75418, is adding three plans.
Group number: 75418
Alpha prefix: LEO (PPO), LEC (CMM), LEC (Medicare)
Platform: NASCO
Plans offered:
Medical
Prescription drugs
Vision |
None of the information included in this billing chart is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.

Blue Cross and BCN add new virtual option for behavioral health care
Blue Cross Blue Shield of Michigan and Blue Care Network are providing members with expanded access to behavioral health providers by offering a new virtual option for anxiety and depression treatment, effective July 15, 2022.
We’ve contracted with AbleTo, an independent company with a network of more than 2,000 therapists serving adults 18 and older, to offer virtual mental health services in all 50 states. This option is available for members with Blue Cross commercial, Medicare Plus Blue℠, BCN commercial and BCN Advantage℠ coverage.
AbleTo provides adult members with a structured and evidence-based eight-week cognitive behavioral treatment program for anxiety and depression, the most common behavioral health conditions. The program includes access to weekly sessions with a licensed master’s level clinician and access to digital tools, resources and relaxation activities for practice between sessions.
If you have a patient struggling to find a behavioral health therapist in their area or get an appointment as quickly as they want it, you may want to refer them to AbleTo, ableto.com/bcbsm,** beginning July 15. Note: Website may not be operational until July 15.
AbleTo intends to also refer patients to other in-network health care providers as needed.
Members can find an AbleTo provider by calling the number on the back of their member ID card or going to the AbleTo website.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Clinical quality corner: Coordination of care
This new column by Dr. William Beecroft, medical director of behavioral health, will feature topics recommended by the Clinical Quality Committee.
Blue Cross Blue Shield of Michigan promotes the importance of coordination of care among contracted providers, including the primary care provider and behavioral health specialist. Coordination of care is crucial to ensuring that everyone on the treatment team is aware of others who may be involved in the care of the patient. This helps eliminate so-called silos of care and leads, ultimately, to optimal patient outcomes.
We’ve added language to our insurance certificates that provides our members with information about this key component of their care. The certificates indicate that the primary care physician is the participating provider a member chooses to provide or coordinate all their medical health care, including specialty and hospital care. The primary care physician is licensed in one of the following medical fields:
- Family Practice
- General Practice
- Internal Medicine
- Pediatrics
We encourage you to explain to your patients why coordination of care is so important and ask them to let you know if they’re seeing other health care providers.
The Michigan Department of Health and Human Services has made available a standard consent form** that providers can use for sharing mental health and substance use disorder treatment information.
For more information, see the Coordination of care section of the “Behavioral Health chapter” in your online provider manual.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Landmark Health high-intensity in-home care program expands Oct. 1
On July 1, 2022, Blue Cross Blue Shield of Michigan and Blue Care Network expanded the high-intensity in-home care program by Landmark Health to include all Medicare Advantage members with multiple chronic conditions who reside in Southeast Michigan counties, as well as in the Lansing and Flint areas.
Starting Oct. 1, 2022, the program will be available to members in the following additional counties:
- Arenac
- Bay
- Calhoun
- Gladwin
- Gratiot
- Huron
- Jackson
- Kalamazoo
- Lenawee
- Midland
- Sanilac
- Tuscola
For high-level information about the program, see this provider alert.
For detailed information about the program, see the document titled High-intensity in-home care program: Frequently asked questions for providers.
Landmark Health, L.L.C., is an independent company that provides select services for Blue Cross Blue Shield of Michigan and Blue Care Network members who have Medicare Advantage plans.
We’re removing age limits for autism spectrum disorder services
We’re removing age limits for autism spectrum disorder services, including applied behavior analysis, or ABA. This change is retroactive to Jan. 1, 2022, to ensure continued access to treatment for Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members whose plan benefits include ABA treatment, other autism services or both.
For dates of service on or after Jan. 1, 2022, we’ll reprocess claims for ASD services that were rejected due to age limits. You don’t need to resubmit the claims.
Members who aged out of eligibility for ASD services in 2022 will remain eligible to continue receiving ASD services that are medically necessary.
Background
Previously, following state of Michigan legal guidelines, children aged out of eligibility for certain ASD services when they turned 19. We’re updating our benefits to allow members over the age of 19 to receive these ASD services when medically necessary.
We’re making this change because recent medical evidence indicates that age limits are no longer an appropriate method for determining whether ABA treatment is medically necessary.
This change is consistent with recent guidance from the Michigan Department of Insurance and Financial Services, and the federal government.
Additional information
We’re updating our Autism Spectrum Disorder Services medical policy and provider communications — including provider manuals — to reflect this change.
We’ll update our certificate and benefit documents to reflect this change by Jan. 1, 2023.
Reminder: Members can’t receive prescriptions for DME/P&O items through telehealth visits
As we told you in an October 2018 Record article, effective Nov. 1, 2018, health care providers aren’t able to prescribe or issue durable medical equipment and prosthetic and orthotic supplies during telehealth visits. A telehealth visit doesn’t meet the medical necessity requirements for prescribing these items. Prescription and issuance resulting from a telehealth visit may be subject to audit review and recovery.
A telehealth visit includes:
- Phone call
- Both email and postal mail
- Video chat
All telehealth formats are excluded from issuing DME and prosthetic and orthotic items.
All behavioral health practitioner specialty changes require new enrollment
A new mental health practitioner enrollment application is required when you’re making changes to your specialty or licensure. Any groups you currently practice with will need to update their records to reflect your change.
For information on enrollment and credentialing with Blue Cross Blue Shield of Michigan, visit the Join Our Provider Network section of bcbsm.com. The credentialing process verifies the licenses and qualifications of a health care provider and ensures that they meet the state requirements for health care.
Additionally, you’ll want to make sure you’re reviewing and submitting all required documents for your new specialty or license. See the Provider Enrollment and Change Process Required Document Checklist, which is also on our website.
Examples:
- If you’re a limited licensed psychologist, or LLP, who has recently become a fully licensed psychologist, a new mental health enrollment application is required. After your new enrollment application is processed, you must submit a request to terminate the LLP profile.
- If you’re a clinical licensed master’s social worker, or LMSW, who has recently become a licensed professional counselor, a new mental health enrollment application is required. After new mental enrollment application is processed you must submit a request to terminate the LMSW profile.
Note: You can terminate the previous profile by filling out and faxing the “Terminate Practitioner” paperwork in the Provider Enrollment section of our website.
If you have any questions or need additional information, contact Provider Enrollment Data Management at 1-800-822-2761.
2022 InterQual criteria to be implemented Aug. 1
Blue Cross Blue Shield of Michigan and Blue Care Network will start using 2022 InterQual® criteria on Aug. 1, 2022, to make utilization management determinations.
Keep in mind that there are InterQual criteria for behavioral health services, as well as non-behavioral health services. However, New Directions® Behavioral Health, an independent company that managers authorizations for behavioral health and autism services for most Blue Cross commercial members, uses its own criteria for making determinations on behavioral health authorization requests.
Additional information about behavioral health services is at the end of this article.
Non-behavioral health services
We’ll use updated criteria for all levels of care to make utilization management determinations for requests to authorize non-behavioral health services, subject to review, for the following members:
- Blue Cross commercial
- Medicare Plus Blue℠
- BCN commercial
- BCN Advantage℠
When clinical information is requested for a medical or surgical admission or for other services, we require submission of the specific components of the medical record that validate that the request meets the criteria.
Blue Cross and BCN also use local rules — modifications of InterQual criteria — in making utilization management determinations. The 2022 local rules for acute care inpatient medical admissions were implemented on March 1, 2022. The 2022 local rules for post-acute care will be announced at a later date.
You can access the modifications (local rules), as applicable, for:
- Blue Cross — on the Authorization Requirements & Criteria page in the Blue Cross section of our ereferrals.bcbsm.com website. You’ll see links to the criteria in both the Blue Cross commercial and Medicare Plus Blue sections of that page.
- BCN — on the Authorization Requirements & Criteria page in the BCN section of our ereferrals.bcbsm.com website. Look under the Referral and authorization information heading.
Refer to the table below for more specific information about which criteria are used in making determinations for various types of non-behavioral health authorization requests.
|
Criteria
|
Application |
|
- Inpatient admissions
- Continued stay discharge readiness
|
|
- Subacute and skilled nursing facility admissions
- Continued stay discharge readiness
|
|
- Inpatient admissions
- Continued stay and discharge readiness
|
|
- Long-term acute care facility admissions
- Continued stay discharge readiness
|
|
- Imaging studies and X-rays
|
|
- Surgery and invasive procedures
|
|
- Services that require clinical review for medical necessity and benefit determinations
|
|
- Services that require clinical review for medical necessity
|
|
- Exceptions to the application of InterQual criteria that reflect the accepted practice standards for Blue Cross and BCN
|
Local rules for post-acute care (applies to inpatient rehabilitation, skilled nursing facility and long-term acute care admissions for Blue Cross commercial and BCN commercial)
|
- Exceptions to the application of InterQual criteria that reflect the accepted practice standards for Blue Cross and BCN
|
Note: The information in the table above applies to lines of business and members whose authorizations are managed by Blue Cross or BCN directly and not by an independent company that provides services to Blue Cross Blue Shield of Michigan.
Behavioral health services
On Aug. 1, 2022, we’ll begin using the 2022 InterQual criteria to make utilization management determinations for behavioral health services for these members:
- Medicare Plus Blue
- BCN commercial
- BCN Advantage
In addition, certain types of determinations will be based on modifications to InterQual criteria or on local rules or medical policies, as shown in the table below.
Health plans |
Modified InterQual criteria for:
|
Local rules or medical policies for:
|
BCN commercial and BCN Advantage |
- Substance use disorders: partial hospital program and intensive outpatient program
- Mental health disorders: partial hospital program and intensive outpatient program
- Residential mental health treatment (adult, geriatric, child and adolescent members)
Note: Neither BCN commercial members with BCN1, BCN5 and BCN10 plans nor BCN Advantage members have residential mental health treatment benefits. |
- Applied behavior analysis for autism spectrum disorder — for BCN commercial members only
- Neurofeedback for attention deficit disorder and attention deficit hyperactivity disorder
- Transcranial magnetic stimulation, or TMS
- Telemedicine (telepsychiatry and teletherapy)
|
Medicare Plus Blue |
- Substance use disorders: partial hospital program and intensive outpatient program
- Mental health disorders: partial hospital program and intensive outpatient program
Note: Only State of Michigan Medicare Plus Blue members have intensive outpatient program benefits. |
- Telemedicine (telepsychiatry and teletherapy)
Note: Medicare Plus Blue members don’t have neurofeedback or TMS benefits. |
For more information on telemedicine, refer to the Blue Cross and BCN: Telehealth for behavioral health providers document.
In early July, we’ll have links to the updated versions of the modified behavioral health and autism local rules and to the medical policies. Those links will be located on these pages on our ereferrals.bcbsm.com website:
As noted earlier in the article, determinations on Blue Cross commercial behavioral health authorization requests are handled by New Directions. New Directions uses its own Medical Necessity Criteria.**
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Coding Advisor outreach to educate providers about appropriate use of procedure codes
What you need to know
In July, Change Healthcare will reach out by phone or letter to health care providers who submit claims to Blue Cross Blue Shield of Michigan and Blue Care Network. Coding Advisor will compare the billing of CPT codes to the codes used by a provider’s peers through a physician profile. (An example of a physician profile is at the end of this article.)
It can be challenging for health care providers and their office staff to select the Current Procedural Terminology, or CPT®, code that best reflects the complexity of a patient visit. That’s why Blue Cross Blue Shield of Michigan contracted with Change Healthcare, an independent company, to implement our Coding Advisor program in 2019.
Change Healthcare reviews evaluation and management codes billed and other scenarios — such as use of modifier 25, observation care and nursing facility care — on claims submitted to Blue Cross. While Change Healthcare won’t review Evaluation and Management services for BCN and BCN Advantage℠ because they use a repricing program that’s already in place, the company will review other modules that include services provided by BCN and BCN Advantage. The program provides useful data insights to the provider community and works to maximize coding efficiency and accuracy through up-front education, rather than taking a traditional post-claim review process.
Effective July 1, 2022, the Coding Advisor program will expand to include the review of the Global Surgical Package. The GSP review is meant to help ensure the surgeon is using global service modifiers appropriately, based on modifier definitions. Global surgery applies in any setting, including an inpatient hospital, outpatient hospital, outpatient surgical center and physician’s office.
Throughout the course of this program, Coding Advisor will continue to monitor billing practices and send updated reports periodically. Coding Advisor may contact your practice to discuss coding variances and to offer one-on-one coding education. You’ll receive all correspondence from Change Healthcare.
If you have any questions, call the Coding Advisor Customer Support line at
1-844-592-7009 and select option 3.
For reference, here’s an example of a physician profile:
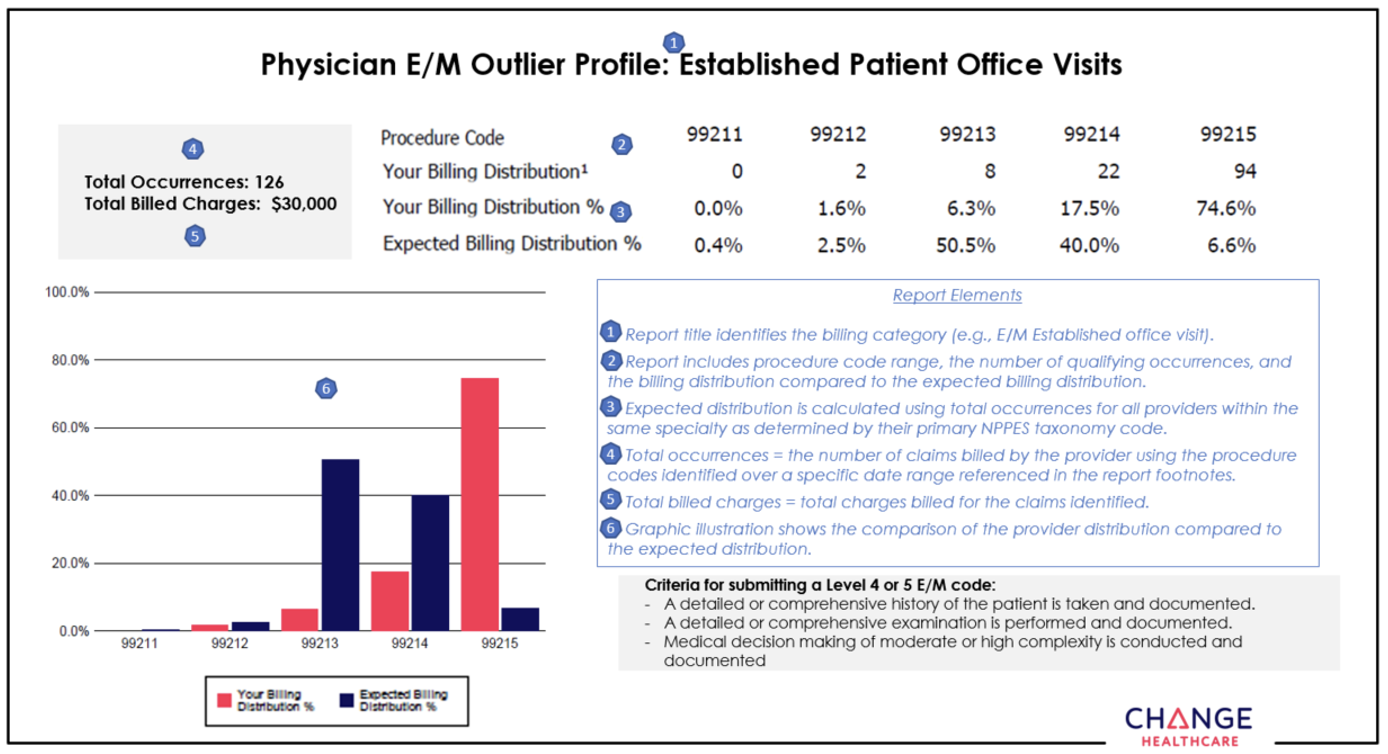
Update: Reminder of appropriate use of modifier 59 and related X modifiers for Medicare Plus Blue claims
In the June Record, we communicated about the appropriate use of modifier 59 for Medicare Plus Blue℠ claims. We’ve updated the article to indicate that the guidelines that apply when appending modifier 59 also apply to related X modifiers. Use the revised article below as your reference going forward.
As a reminder, you’ll want to continue to follow the guidelines communicated in the September 2021 Record article when appending modifier 59 Medicare Plus Blue℠ claims — and keep in mind that the guidelines also apply to related X modifiers. We’ve begun editing claim lines when modifier 59 and related X modifiers are appended on Medicare Plus Blue claims.
This change aligns with the Centers for Medicare & Medicaid National Correct Coding Initiative, or NCCI, program to ensure the correct coding of services. Modifier 59 and related X modifiers are used to indicate that a procedure or service was distinct or independent from other services that aren’t normally reported together but are performed on the same day.
We no longer automatically allow payment for certain procedures billed with modifier 59 and related X modifiers when billed with a procedure code on the CMS Procedure to Procedure NCCI List. Only select codes allow modifier 59 and related X modifiers to automatically bypass the NCCI code-pair edits.
The X modifiers are defined below:
- XE — Separate Encounter, a service that is distinct because it occurred during a separate encounter (Only use XE to describe separate encounters on the same date of service.)
- XS — Separate Structure, a service that is distinct because it was performed on a separate organ/ structure
- XP — Separate Practitioner, a service that is distinct because it was performed by a different practitioner”
- XU — Unusual Non-Overlapping Service, the use of a service that is distinct because it doesn’t overlap usual components of the main service
The additional review assures claims have been coded correctly for more complex situations where an overriding modifier has been appended. Health care providers should code claims to the level of specificity for the services rendered and appropriately append diagnosis codes and modifiers following the guidelines published by the American Medical Association and CMS. The reported services should be supported in the patient’s medical record.
Note: The appeal process won’t change. Continue to submit appeals on the Clinical Editing Appeal Form with the necessary documentation. Also, continue to fax one appeal at a time to avoid processing delays.
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Follow these billing guidelines for removal of impacted cerumen
The removal of cerumen is a procedure that’s different from routine earwax removal. Routine earwax removal is performed to facilitate the ear examination portion of a physical examination.
Blue Cross Blue Shield of Michigan requires that procedure codes *69209, *69210 and G0268 should only be reported for removal of cerumen when all of these statements apply:
- Impacted cerumen, an immovable collection of compressed or hardened earwax in the external ear canal, is symptomatic and can’t be dislodged.
- Treatment requires extensive use of a spoon, loop, suction device or an agent that degrades the earwax for irrigation.
- The procedure requires the personal attention of the physician.
- The removal of the impacted cerumen is the major part of the encounter.
Note: Cleaning earwax from the external ear canal involves removing the soft, brownish, yellow, wax-like secretion of the ceruminous glands of the external auditory canal. It can easily be removed using a spoon, loop or bulb syringe. For this service, the physician typically takes one to two minutes, and the service shouldn’t be reported separately.
Removal of impacted cerumen (*69209, *69210, G0268) will only be considered as medically necessary when reported with a diagnosis of impacted cerumen (ICD-10 H61.20-H61.23) in accordance with the AMA CPT and HCPCS Level II manuals.
Therefore, CPT codes *69209, *69210 or G0268 billed with any other diagnosis will be denied or recovered.
Leqvio to have site-of-care requirement for commercial members, starting Aug. 1
Leqvio® (inclisiran), HCPCS code J3590, will have a site-of-care requirement, in addition to its current prior authorization requirement for Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members, starting Aug. 1, 2022.
When the site-of-care requirement goes into effect, this drug may be covered only when administered at the following sites of care:
- Doctor’s or other health care provider’s office
- Ambulatory infusion center
- The member's home, from a home infusion therapy provider
Members who start treatment in a location other than those outlined above prior to Aug. 1, 2022, will be able to continue receiving the drug in that location until their current authorization expires. Providers should then transition members to one of the above sites of care.
Notes:
- Starting July 1, 2022, the HCPCS code for this drug will be J1306.
- This drug is part of members’ medical benefits, not their pharmacy benefits.
- As a reminder, prior authorization requests are submitted using the NovoLogix® online tool.
Some Blue Cross commercial groups not subject to these requirements
For Blue Cross commercial groups, this authorization requirement applies only to groups that currently participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list.
Note: Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don't participate in the standard prior authorization program.
List of requirements
For a full list of requirements related to drugs covered under the medical benefit, see the Blue Cross and BCN utilization management medical drug list for Blue Cross commercial and BCN commercial members. We’ll update this list prior to Aug. 1.
You can access this list and other information about requesting prior authorization at ereferrals.bcbsm.com, at these locations:
Authorization isn't a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members.
Fyarro to require prior authorization for most members, starting Aug. 16
For dates of service on or after Aug. 16, 2022, Fyarro™ (sirolimus protein-bound particles), HCPCS code J9331, will require prior authorization through AIM Specialty Health®. This drug is part of members’ medical benefits, not their pharmacy benefits.
Prior authorization requirements apply when this drug is administered in outpatient settings for:
- Blue Cross Blue Shield of Michigan commercial — Members who have coverage through fully insured groups and members with individual coverage
Note: This requirement doesn’t apply to members who have coverage through Blue Cross commercial self-funded groups, including the Blue Cross and Blue Shield Federal Employee Program® and UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans.
- Medicare Plus Blue℠ members
- Blue Care Network commercial members
- BCN Advantage℠ members
How to submit authorization requests
Submit authorization requests to AIM using one of the following methods:
More about the authorization requirements
Authorization isn’t a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members.
For additional information on requirements related to drugs covered under the medical benefit, see:
- Blue Cross commercial and BCN commercial:
- Medicare Advantage:
We’ll update the pertinent drug lists to reflect the information in this message prior to the effective date.
AIM Specialty Health is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services. For more information, go to our ereferrals.bcbsm.com website.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Fyarro and Tivdak will have requirements for URMBT members with Blue Cross non-Medicare plans
For dates of service on or after Aug. 16, 2022, the drugs listed below will require prior authorization through AIM Specialty Health® and may also have site-of-care requirements, quantity limit requirements or both. These requirements will apply to UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans. These drugs are part of members’ medical benefits, not their pharmacy benefits.
See the table for more information. When a cell is blank, the drug doesn’t have that requirement.
Brand name |
Generic name |
HCPCS code |
Requirements |
Prior authorization |
Site of care |
Quantity limits |
Fyarro™ |
sirolimus protein-bound particles |
J9331 |
✓ |
|
|
Tivdak® |
tisotumab vedotin-tftv |
J9273 |
✓ |
|
|
These requirements apply only when these drugs are administered in an outpatient setting.
Note: These requirements don’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714).
How to submit authorization requests
Submit prior authorization requests to AIM using one of the following methods:
More about the authorization requirements Authorization isn’t a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members.
For additional information on requirements related to drugs covered under the medical benefit for URMBT members with Blue Cross non-Medicare plans, see:
We’ll update the pertinent drug lists to reflect the information in this article prior to the effective date.
Note: Accredo manages prior authorization requests for additional medical benefit drugs for these members.
AIM Specialty Health is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services. For more information, go to our ereferrals.bcbsm.com website.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Fusilev no longer requires prior authorization
Because Spectrum Pharmaceuticals has stopped manufacturing Fusilev® (levoleucovorin), HCPCS code J0641, we no longer require prior authorization through AIM Specialty Health® for dates of service on or after May 31, 2022. The drug was part of members’ medical benefits, not their pharmacy benefits.
This change applies to:
- Blue Cross Blue Shield of Michigan commercial:
- Members who have coverage through fully insured groups
- Members with individual coverage
- UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans
- Medicare Plus Blue℠ members
- Blue Care Network commercial members
- BCN Advantage℠ members
For additional information on requirements related to drugs covered under the medical benefit, refer to the following drug lists:
- Medicare Plus Blue and BCN Advantage members:
What you need to know about submitting medical benefit drug prior authorization requests for Medicare Advantage members
Blue Cross Blue Shield of Michigan and Blue Care Network recently transitioned to a new provider portal, Availity Essentials. You should continue to submit prior authorization requests for most medical benefit drugs, including CAR-T cell therapy drugs, for Medicare Plus Blue℠ and BCN Advantage℠ members in one of the following ways:
- Preferred method: Through the NovoLogix® online tool. See the next section for the steps you need to take to access NovoLogix through Availity®.
- For providers who aren’t able to submit requests through NovoLogix: You have two options:
Preferred method for submitting prior authorization requests
The preferred method continues to be submitting requests through NovoLogix.
Note: If you haven’t already done so, be sure to register for Availity so you can continue to submit requests through NovoLogix.
If you have an Availity account, you have access to NovoLogix.
To submit requests through Availity:
- Log in to our provider portal (availity.com**).
- Click on Payer Spaces on the Availity menu bar.
- Click on the BCBSM and BCN logo.
- In the Applications tab, click on the appropriate tile:
- NovoLogix MAPPO
- NovoLogix BCN/BCN Advantage
Additional information
You can access the Medication Authorization Request Form (for any medication) on the For Providers: How do I Submit a Drug Prior Authorization Request for Medicare Plus Blue PPO and BCN Advantage? page of the bcbsm.com website. Later this year, we’ll remove the medical drug prior authorization request forms for specific medications.
For more information about submitting requests and to view the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members, see the following pages of ereferrals.bcbsm.com website:
**Blue Cross and Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Cortrophin and Ryplazim to have requirements for URMBT members with Blue Cross non-Medicare plans
For dates of service on or after Sept. 1, 2022, the following drugs will require prior authorization through the NovoLogix® online tool and may also have site-of-care requirements, quantity limit requirements or both. These requirements will apply to UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans. These drugs are part of members’ medical benefits, not their pharmacy benefits.
See the table for more information. When a cell is blank, the drug doesn’t have that requirement.
Brand name |
Generic name |
HCPCS code |
Requirements |
Prior authorization |
Site of care |
Quantity limits |
Cortrophin® |
corticotropin |
J3490/J3590 |
✓ |
|
|
Ryplazim® |
plasminogen, human-tvmh |
J3590/C9090 |
✓ |
|
✓ |
These requirements apply only when these drugs are administered in an outpatient setting.
Note: These requirements don’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714).
How to submit authorization requests
Submit prior authorization requests through NovoLogix. It offers real-time status checks and immediate approvals for certain medications.
To learn how to submit requests through NovoLogix, go to our Blue Cross Medical Benefit Drugs page, scroll to the Blue Cross commercial column and review the information in the How to submit authorization requests electronically using NovoLogix section.
More about the authorization requirements
Authorization isn’t a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members.
For additional information on requirements related to drugs covered under the medical benefit for URMBT members with Blue Cross non-Medicare plans, see:
We’ll update the pertinent drug lists to reflect the information in this message prior to the effective date.
Note: Accredo manages prior authorization requests for additional medical benefit drugs for these members.
AllianceRx Walgreens Prime is now AllianceRx Walgreens Pharmacy
Effective June 24, 2022, AllianceRx Walgreens Prime, a provider of specialty pharmacy services, changed its name to AllianceRx Walgreens Pharmacy.
AllianceRx Walgreens Pharmacy will continue to provide Blue Cross Blue Shield of Michigan members with specialty medications used to treat chronic, complex or rare conditions.
Blue Cross introducing payment policy for multiple therapy services
Starting in October, Blue Cross Blue Shield of Michigan will use a new payment reduction procedure for physical, occupational and speech therapy.
This policy will reduce reimbursement for the practice expense portions of therapy procedures when those services are the secondary or subsequent procedures provided on a single date of service by the same physician or other qualified health care professional. The change is being made to align with the Centers for Medicare & Medicaid Services’ Multiple Therapy Policy.
The service with the highest Relative Value Unit, or RVU, is considered the primary service. The practice expense RVU includes the nonphysician clinical and nonclinical labor of the practice, as well as expenses for building space, equipment and office supplies. Such expenses are considered duplicative for each subsequent therapy service and therefore will be reduced by 50% accordingly.
This practice expense reduction will result in an approximate average reimbursement of 83% of the allowed amount for all subsequent therapy services rendered on the same day.
In the Facility section of this issue of the newsletter, we provide details on how facilities can provide input on this new procedure.
Reminder: 2% Medicare sequestration reduction slated to resume July 1
We’re reminding health care providers that Medicare sequestration reduction is scheduled to resume July 1, 2022, at 2%. Blue Cross Blue Shield of Michigan and Blue Care Network are aligned with the Centers for Medicare & Medicaid Services’ guidance regarding Medicare sequestration reductions.
You may recall that the U.S. Congress and Biden administration suspended the mandatory Medicare 2% sequestration reduction through March 31, 2022, and reduced the sequestration cuts to 1% from April through June 2022.
The suspension was made to offset the decrease in payments to health care providers because of the COVID-19 public health emergency. If the suspension is extended after June 30, we’ll update you with a provider alert.
Note: The 2% reimbursement adjustment is applied after determining any applicable member deductible, copayment or other required member out-of-pocket costs. The change won’t affect reimbursements to providers who haven’t been affected by sequestration previously.
New on-demand training available
Action item
Visit our provider training site to find new resources on topics that are important to your role.
Provider Experience continues to offer training resources for health care providers and staff. On-demand courses are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network.
We recently added the following new learning opportunity:
- Avalon laboratory services overview — This recorded webinar discusses the laboratory benefits management program supported by Avalon Healthcare Solutions, lab policy administration and the trial claim advice tool.
Our provider training site is available to enhance the training experience for health care providers and staff. To request access, complete the following steps:
- Open the registration page.
- Complete the registration. We recommend using the same email you use to communicate with Blue Cross for other provider-related needs. This will become your login ID.
- Follow the link to log in.
If you need assistance creating your login ID or navigating the site, contact ProviderTraining@bcbsm.com.
Lunch and learn webinars focus on risk adjustment, coding
Action item
Register now for webinars that can improve your coding processes.
Physicians and coders are invited to attend webinars that provide new information on documentation and coding of common and challenging diagnoses. These live lunchtime educational sessions will include an opportunity to ask questions.
Current schedule
All sessions start at noon Eastern time and generally run for 30 minutes. Click on a link below to sign up.
You can watch previously hosted sessions on our provider training website. Use the keyword “Lunch” to search for the courses. You’ll also find them listed in the Quality management section of the course catalog.
Click here if you are already registered for the site.
To request access to the provider training website:
- Click here to register.
- Complete the registration. We recommend using the same email you use to communicate with Blue Cross Blue Shield of Michigan for other provider-related needs. This will become your login ID.
Previously recorded |
Topic |
April 19 |
Coding and Documentation for HCC Capture and Risk Adjustment |
May 5 |
Coding for Cancer and Neoplasms |
June 16 |
Coding for Heart Disease and Heart Arrythmias |
If you have any questions about the sessions, contact April Boyce at aboyce@bcbsm.com. If you have questions about registration, email Patricia Scarlett at pscarlett@bcbsm.com.
Do we have your medical records request address?
As a reminder, please ensure that we have your correct medical records request address on file. In the April 2022 Record, we let you know we’ll be working with Optum to implement some new edits. Optum is an independent company that contracts with Blue Cross Blue Shield of Michigan to identify professional and facility claims that require additional review.
One component of our relationship with Optum involves medical records requests.
To prevent claim processing delays, we need to keep your medical records request address on file. If you haven’t provided it yet or need to make changes, use the Enrollment and Change Self-Service Tool, located on the Applications tab of our payer space on the provider portal.
Here are the step-by-step directions:
- Log in to our provider portal (availity.com**).
- Click on Payer Spaces on the Availity menu bar.
- Click on the BCBSM and BCN logo.
- Click on Provider Enrollment and Change Self-Service on the Applications tab.
If we don’t have a medical record request address on file, the request will be sent to the mailing address. If there’s no mailing address on file, the request will be sent to the billing address. And if there’s no billing address on file, the request will be sent to the address shown on the claim.
Help us streamline the claim processing process by making sure we have your correct medical records request address on file.
**Blue Cross Blue Shield of Michigan doesn't own or control this website.
Learn what you can do to better manage osteoporosis and limit disability
Musculoskeletal conditions are the second largest contributor to disability, according to the World Health Organization.
Osteoporosis Management in Women who had a Fracture (OMW), a HEDIS® Star measure, assesses women 67 to 85 years of age who suffered a fracture and had either a bone mineral density test or received a prescription to treat osteoporosis within six months of the fracture.
Read this tip sheet to learn more about the measure and find out what information to include in medical records.
HEDIS®, which stands for Healthcare Effectiveness Data Information Set, is a registered trademark of the National Committee for Quality Assurance, or NCQA.
Remember to discuss fall risk, urinary incontinence and physical activity with Medicare patients
According to the National Committee for Quality Assurance, or NCQA:
- Falls are the leading cause of death by injury in people 65 and older. Every year, 1 in 4 older adults fall.
- Urinary incontinence is significantly underreported and underdiagnosed.
- Any amount of physical activity reduces the risk of developing certain chronic conditions and increases quality of life.
Due to the risks posed by falls and urinary incontinence, the Medicare Health Outcomes Survey, or HOS, measures patient-reported outcomes for three HEDIS® Effectiveness of Care measures:
- Fall Risk Management
- Management of Urinary Incontinence in Older Adults
- Physical Activity in Older Adults
The survey, which runs from August through November, asks randomly selected Medicare Advantage members questions about how their health care providers talk with them about these important topics.
Read the HOS tip sheet to learn more, including what questions are members are being asked and how you can address care opportunities with your patients.
HEDIS®, which stands for Healthcare Effectiveness Data Information Set, is a registered trademark of the National Committee for Quality Assurance, or NCQA.
Prenatal, well-child support for FEP members with growing families
This is part of an ongoing series of articles focusing on the tools and resources available to help FEP members manage their health.
The Blue Cross and Blue Shield Federal Employee Program® recognizes the importance of preventive care for pregnant women and growing families. Pregnant women should be seen regularly for prenatal care, especially in the first trimester. Parents are also encouraged to schedule regular well-child visits for their children, particularly in the first 15 months of life.
Here are some resources to share with FEP patients:
- Online information at fepblue.org/maternity:
- Tips for a healthy pregnancy
- Breastfeeding support
- The Pregnancy Care Incentive Program is available to members with the Standard and Basic Option. The program encourages early and ongoing prenatal care. Pregnant members can earn a Pregnancy Care Box that includes pregnancy gifts, information and $75 toward a health account for members who complete all requirements.
- The Summer Health Checklist For Families has reminders for families about well-child visits, immunizations and more.
- Bright Futures,** led by the American Academy of Pediatrics, provides guidance for all preventive care screenings and well-child visits.
If you or FEP members have questions about benefits, call Customer Service at 1-800-482-3600.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Additional procedures codes payable to OPC providers for Blue Cross commercial members, starting July 1
For members with Blue Cross Blue Shield of Michigan commercial plans, we’ve updated our systems to make additional services payable to providers at outpatient psychiatric care facilities.
For dates of service on or after July 1, 2022, the following procedure codes will be payable to the OPC providers specified below for Blue Cross commercial members:
Procedure code |
Payable to |
*98966 |
Clinical psychologists, clinical social workers, limited licensed psychologists, licensed marriage and family therapists, and licensed professional counselors |
*98967 |
*98968 |
*98970 |
*98971 |
*98972 |
*99484 |
Psychiatrists (M.D.s or D.O.s) and certified nurse practitioners |
*99487 |
*99489 |
*99491 |
G2086 |
G2087 |
This change brings the list of procedure codes that are payable to OPC providers for Blue Cross commercial members more in line with those that are payable to OPC providers for Blue Care Network members.
Billing instructions
When billing these procedure codes, include the following in the order specified below:
- The modifier that indicates the licensure level (level of care) for the rendering provider (such as: AH, AJ, HO)
- If the service was delivered via telemedicine: The telemedicine modifier (either GT or 95)
- The place of service:
- If the service was delivered in person: Include place of service 11.
- If the service was delivered via telemedicine: Include place of service code 11, 02 or 10.
To view detailed billing instructions for services delivered via telemedicine, see the “Billing telehealth visits” section of the Telehealth for behavioral health providers document. Refer to the “Outpatient psychiatric care facilities” subsection.
By July 1, we’ll update the Telehealth for behavioral health providers document to reflect the additional codes that are payable for Blue Cross commercial members.
Blue Cross commercial OPC fee schedule
By July 1, we’ll update the OPC fee schedule to reflect this change. You can access the fee schedule as follows:
- Log in to our provider portal (availity.com**).
- Click on Payer Spaces on the Availity menu bar.
- Click on the BCBSM and BCN logo.
- Click on Secure Provider Resources (Blue Cross and BCN) on the Resources tab.
- Choose Fee Schedules > Blue Cross Facility Fee Schedules.
- If prompted, accept the End User License Agreement.
- Click on Outpatient Psychiatric Care on the left.
- Click on the link to open the 2022 fee schedule.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.

2022 InterQual criteria to be implemented Aug. 1
Blue Cross Blue Shield of Michigan and Blue Care Network will start using 2022 InterQual® criteria on Aug. 1, 2022, to make utilization management determinations.
Keep in mind that there are InterQual criteria for behavioral health services, as well as non-behavioral health services. However, New Directions® Behavioral Health, an independent company that managers authorizations for behavioral health and autism services for most Blue Cross commercial members, uses its own criteria for making determinations on behavioral health authorization requests.
Additional information about behavioral health services is at the end of this article.
Non-behavioral health services
We’ll use updated criteria for all levels of care to make utilization management determinations for requests to authorize non-behavioral health services, subject to review, for the following members:
- Blue Cross commercial
- Medicare Plus Blue℠
- BCN commercial
- BCN Advantage℠
When clinical information is requested for a medical or surgical admission or for other services, we require submission of the specific components of the medical record that validate that the request meets the criteria.
Blue Cross and BCN also use local rules — modifications of InterQual criteria — in making utilization management determinations. The 2022 local rules for acute care inpatient medical admissions were implemented on March 1, 2022. The 2022 local rules for post-acute care will be announced at a later date.
You can access the modifications (local rules), as applicable, for:
- Blue Cross — on the Authorization Requirements & Criteria page in the Blue Cross section of our ereferrals.bcbsm.com website. You’ll see links to the criteria in both the Blue Cross commercial and Medicare Plus Blue sections of that page.
- BCN — on the Authorization Requirements & Criteria page in the BCN section of our ereferrals.bcbsm.com website. Look under the Referral and authorization information heading.
Refer to the table below for more specific information about which criteria are used in making determinations for various types of non-behavioral health authorization requests.
|
Criteria
|
Application |
|
- Inpatient admissions
- Continued stay discharge readiness
|
|
- Subacute and skilled nursing facility admissions
- Continued stay discharge readiness
|
|
- Inpatient admissions
- Continued stay and discharge readiness
|
|
- Long-term acute care facility admissions
- Continued stay discharge readiness
|
|
- Imaging studies and X-rays
|
|
- Surgery and invasive procedures
|
|
- Services that require clinical review for medical necessity and benefit determinations
|
|
- Services that require clinical review for medical necessity
|
|
- Exceptions to the application of InterQual criteria that reflect the accepted practice standards for Blue Cross and BCN
|
Local rules for post-acute care (applies to inpatient rehabilitation, skilled nursing facility and long-term acute care admissions for Blue Cross commercial and BCN commercial)
|
- Exceptions to the application of InterQual criteria that reflect the accepted practice standards for Blue Cross and BCN
|
Note: The information in the table above applies to lines of business and members whose authorizations are managed by Blue Cross or BCN directly and not by an independent company that provides services to Blue Cross Blue Shield of Michigan.
Behavioral health services
On Aug. 1, 2022, we’ll begin using the 2022 InterQual criteria to make utilization management determinations for behavioral health services for these members:
- Medicare Plus Blue
- BCN commercial
- BCN Advantage
In addition, certain types of determinations will be based on modifications to InterQual criteria or on local rules or medical policies, as shown in the table below.
Health plans |
Modified InterQual criteria for:
|
Local rules or medical policies for:
|
BCN commercial and BCN Advantage |
- Substance use disorders: partial hospital program and intensive outpatient program
- Mental health disorders: partial hospital program and intensive outpatient program
- Residential mental health treatment (adult, geriatric, child and adolescent members)
Note: Neither BCN commercial members with BCN1, BCN5 and BCN10 plans nor BCN Advantage members have residential mental health treatment benefits. |
- Applied behavior analysis for autism spectrum disorder — for BCN commercial members only
- Neurofeedback for attention deficit disorder and attention deficit hyperactivity disorder
- Transcranial magnetic stimulation, or TMS
- Telemedicine (telepsychiatry and teletherapy)
|
Medicare Plus Blue |
- Substance use disorders: partial hospital program and intensive outpatient program
- Mental health disorders: partial hospital program and intensive outpatient program
Note: Only State of Michigan Medicare Plus Blue members have intensive outpatient program benefits. |
- Telemedicine (telepsychiatry and teletherapy)
Note: Medicare Plus Blue members don’t have neurofeedback or TMS benefits. |
For more information on telemedicine, refer to the Blue Cross and BCN: Telehealth for behavioral health providers document.
In early July, we’ll have links to the updated versions of the modified behavioral health and autism local rules and to the medical policies. Those links will be located on these pages on our ereferrals.bcbsm.com website:
As noted earlier in the article, determinations on Blue Cross commercial behavioral health authorization requests are handled by New Directions. New Directions uses its own Medical Necessity Criteria.**
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Coding Advisor outreach to educate providers about appropriate use of procedure codes
What you need to know
In July, Change Healthcare will reach out by phone or letter to health care providers who submit claims to Blue Cross Blue Shield of Michigan and Blue Care Network. Coding Advisor will compare the billing of CPT codes to the codes used by a provider’s peers through a physician profile. (An example of a physician profile is at the end of this article.)
It can be challenging for health care providers and their office staff to select the Current Procedural Terminology, or CPT®, code that best reflects the complexity of a patient visit. That’s why Blue Cross Blue Shield of Michigan contracted with Change Healthcare, an independent company, to implement our Coding Advisor program in 2019.
Change Healthcare reviews evaluation and management codes billed and other scenarios — such as use of modifier 25, observation care and nursing facility care — on claims submitted to Blue Cross. While Change Healthcare won’t review Evaluation and Management services for BCN and BCN Advantage℠ because they use a repricing program that’s already in place, the company will review other modules that include services provided by BCN and BCN Advantage. The program provides useful data insights to the provider community and works to maximize coding efficiency and accuracy through up-front education, rather than taking a traditional post-claim review process.
Effective July 1, 2022, the Coding Advisor program will expand to include the review of the Global Surgical Package. The GSP review is meant to help ensure the surgeon is using global service modifiers appropriately, based on modifier definitions. Global surgery applies in any setting, including an inpatient hospital, outpatient hospital, outpatient surgical center and physician’s office.
Throughout the course of this program, Coding Advisor will continue to monitor billing practices and send updated reports periodically. Coding Advisor may contact your practice to discuss coding variances and to offer one-on-one coding education. You’ll receive all correspondence from Change Healthcare.
If you have any questions, call the Coding Advisor Customer Support line at
1-844-592-7009 and select option 3.
For reference, here’s an example of a physician profile:
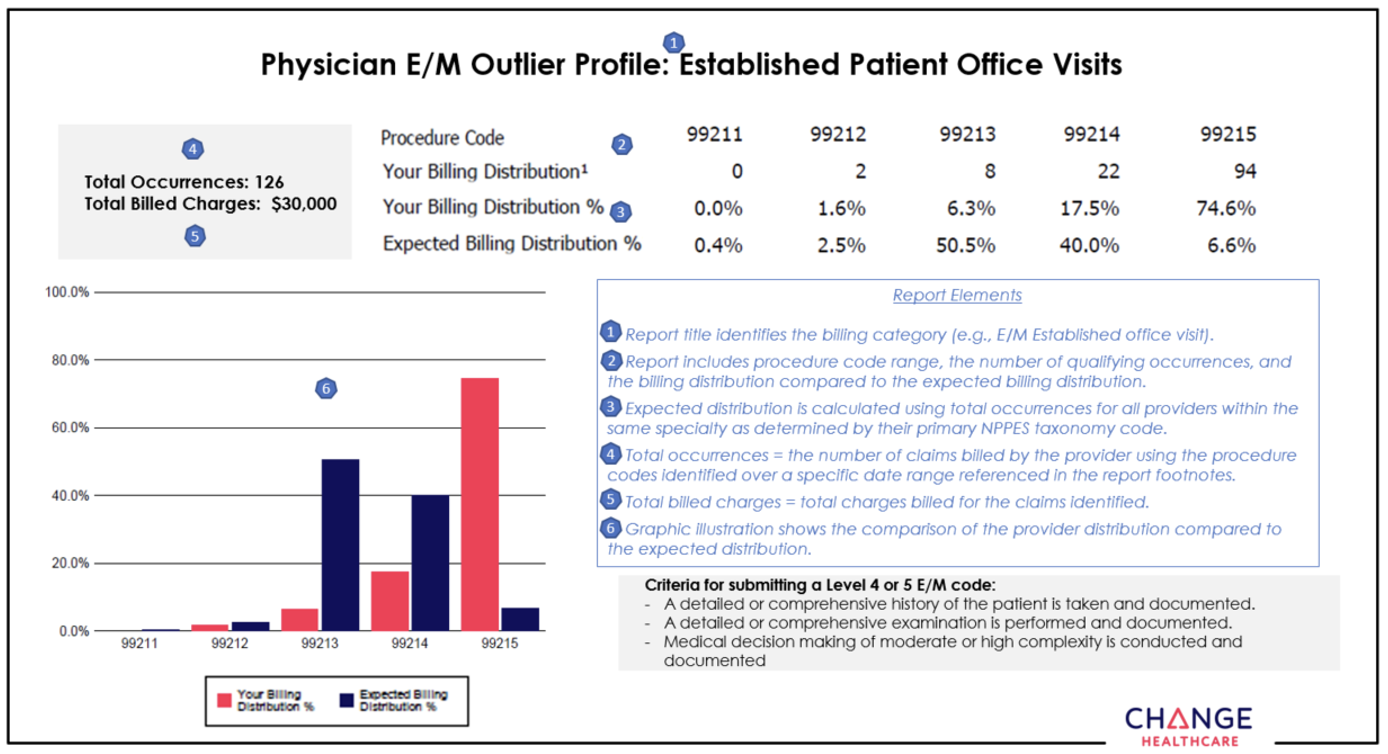
Here’s what you need to know about Prepayment Laboratory Claim Edits and how to provide input
Blue Cross Blue Shield of Michigan is proposing fourth-quarter implementation of a laboratory benefits management program through Avalon Healthcare Solutions. This program will affect independent and facility outpatient lab services for our commercial Blue Cross members.
Avalon is an independent company that contracts with Blue Cross to provide laboratory benefits management.
Avalon’s automated policy enforcement (post-service) edits will be applied to claims reporting laboratory services performed in office, hospital outpatient and independent laboratory locations. Laboratory services, tests and procedures provided in emergency department, hospital observation and hospital inpatient settings are excluded from this program.
This program will:
- Promote consistency of routine testing across all patients and places of service.
- Reduce fraud, waste and abuse.
- Enhance the patient health care experience, ensuring it’s aligned with scientific evidence-based guidelines.
- Deliver value-driven care by improving quality and appropriateness of lab services.
- Increase payment accuracy as it relates to allowable provider reimbursement associated with lab claims.
What this means to facilities
The lab claim edits will support our medical policy in cases where there’s fixed criteria, specificity and no risk of a different interpretation that would require a medical review. Edit types include:
- History
- Quantity
- Frequency
- Procedure code-diagnosis code comparison
- Incompatibility
- Age
The claim edits will focus on high-volume, low-cost tests, such as vitamin D, thyroid, cholesterol and A1c. They will identify unnecessary units (excessive units, unnecessary testing and over-frequency).
Facilities need to be aware of the new and revised laboratory medical policies and guidelines, as these polices and guidelines affect certain laboratory services, tests and procedures. Facility and independent lab reimbursement may be reduced if the lab tests ordered by the physician and provided by the labs don’t meet these policies, which became effective June 1, 2022.
To review laboratory medical policies, click on this link.** The following polices are expected to have the most significant effect on facilities:
- Prescription Medication and Illicit Drug Testing in the Outpatient Setting
- Vitamin D Testing — variance
- Vitamin B12 and Methylmalonic Acid Testing
- Cardiovascular Disease Risk Assessment
- Thyroid Disease Testing
- Testosterone Testing
Policy |
Edit Type |
Rule |
Vitamin D |
Procedure and diagnosis code compatibility |
Always allowed or never allowed |
Frequency |
2 units per year |
Vitamin B12 |
Procedure and diagnosis code compatibility |
Always allowed or never allowed |
Frequency |
1 unit every 3 months |
HbA1c |
Procedure and diagnosis code compatibility |
- Diabetic or pregnant
- Diabetic
- Not diabetic for members 18 years and older
- Not diabetic for members under 18 years
|
Frequency |
1 unit every 3 months |
Cervical Cancer Screening |
Procedure and diagnosis code compatibility |
Always allowed or never allowed |
Age |
Units/period of time/age range |
Trial Claim Advice Tool
Before ordering a test, health care providers can use the Trial Claim Advice Tool to simulate a trial claim by inputting codes for services, along with patients’ diagnoses, to determine possible edits in advance of submitting claims. To access the tool, follow these steps:
- Log in to our provider portal (availity.com).**
- Click on Payer Spaces on the Availity menu bar.
- Click on the BCBSM and BCN logo.
- Click on Avalon Lab Claim Editing on the Applications tab.
This tool will review claims with laboratory services for adherence and consistency with our laboratory policies, such as:
- Meeting policy coverage criteria
- Appropriateness for patient’s age
- Frequency of services
- Whether a procedure is considered experimental or investigational
- Whether it’s appropriate for the clinical situation
Notes:
- This is a simulation tool and doesn’t guarantee approval or reimbursement of a claim.
- It’s expected that health care providers who order lab tests are doing so appropriately, according to medical necessity and relevant guidelines.
- Blue Cross and Avalon will offer health care provider education seminars prior to implementation. Ongoing support tools will also be available through provider portals.
Input requested
According to the Contract Administration Process — part of the Participating Hospital Agreement that went into effect July 1, 2021 — we allow nonbinding input from participating facilities about such proposals.
Input from facilities is requested by July 31, 2022. Send any input you may have to Liz Bowman at ebowman@bcbsm.com.
After input is received, Blue Cross has 30 calendar days to respond.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
What facilities need to know about proposed new policy for multiple therapy services and how to provide input
Blue Cross Blue Shield of Michigan is proposing implementation of a new payment reduction policy for physical, occupational and speech therapy. Program implementation is scheduled for the fourth quarter of 2022 for Blue Cross commercial members.
This policy will reduce reimbursement for the practice expense portions of therapy procedures when those services are the secondary or subsequent procedures provided on a single date of service by the same physician or other qualified health care professional. This change is being made to align with the Centers for Medicare & Medicaid Services’ Multiple Therapy Policy.
The policy doesn’t interfere with benefit limits. Blue Cross allows 90 therapy visits per calendar year, and these rules won’t affect those limits.
What this means to facilities
When multiple therapy services are rendered on the same day, we’ll apply a “therapy pay percent edit.” The primary service will be reimbursed at 100% of the allowed amount, while secondary procedures performed on the same day will be reduced by 50% of the practice expense relative value unit, or RVU.
The service with the highest RVU is considered the primary service. The practice expense RVU includes the nonphysician clinical and nonclinical labor of the practice, as well as expenses for building space, equipment and office supplies. Such expenses are considered duplicative for each subsequent therapy service and therefore will be reduced accordingly.
This practice expense reduction will result in an approximate average reimbursement of 83% of the allowed amount for all subsequent therapy services rendered on the same day.
The top five procedure codes that would receive the facility edit (reduced payment) include:
- *97140 – MANUAL THERAPY 1/> REGIONS
- *97110 – THERAPEUTIC EXERCISES
- *97530 – THERAPEUTIC ACTIVITIES
- *97112 – NEUROMUSCULAR REEDUCATION
- *97116 – GAIT TRAINING THERAPY
Input requested
According to the Contract Administration Process — part of the Participating Hospital Agreement that went into effect July 1, 2021 — we allow non-binding input from participating facilities about such proposals.
Input from facilities is requested by July 31, 2022. Send any input you may have to Liz Bowman at ebowman@bcbsm.com.
After input is received, Blue Cross has 30 calendar days to respond.
Update: DRG Clinical Validation Audit implementation
In a February Record article, we wrote about the proposed implementation of the Diagnosis-related Group Clinical Validation Audits and asked for facility input. Based on that input, we’re providing some additional information below:
- Change Healthcare** clinical review of the physician documentation will determine if the patient diagnosis is consistent with the clinical documentation in the medical record. These claim rules align with Blue Cross Blue Shield of Michigan policy.
- According to guidelines from the Centers for Medicare & Medicaid Services, DRG clinical validation is a separate process from DRG coding validation. DRG coding validation involves a clinical review of a case to determine whether the patient has the conditions that were documented. Because this is a clinical DRG validation audit, it should be performed by a clinician or a clinician with approved coding credentials and doesn’t require a certified coder.
- Adding this type of audit won’t increase the number of audits a hospital is subject to as we have established inpatient audit limits. Since we aren’t auditing additional claims, there shouldn’t be an increased administrative burden.
- As DRG clinical validation is a separate process from DRG coding validation, it’s possible to have a claim that is correctly coded based on national coding guidelines, but where the clinical indicators aren’t met.
- DRG clinical validation audits will exclude hospitals who have prospective rate agreements.
Following Blue Cross Blue Shield of Michigan’s review of facility input, we’ll be moving forward with this program, effective Aug. 1, 2022. Details about the DRG Clinical Validation Audits were presented at the May 16 Staff Liaison Group meeting, which included leadership from the Michigan Health and Hospital Association and Blue Cross, and the PHA Advisory Committee on June 21.
**Change Healthcare is an independent company that contracts with Blue Cross Blue Shield of Michigan to provide audit services.
Update: Emergency Department Claims Analyzer implementation
In a February Record article, we wrote about the proposed expansion of Blue Cross Blue Shield of Michigan’s claim editing process, aimed at promoting correct coding through the Optum Emergency Department Claim Analyzer tool, and asked for input from our facilities. Based on that input, we’re providing some additional information below:
- Currently, the EDC Analyzer only recodes from a higher-level Evaluation and Management, or E/M code, to a lower-level code.
- To appeal an EDC Analyzer claim, follow the current clinical editing appeals process.
- EDC Analyzer is now the Blue Cross payment policy, and claims can be modeled at EDSAnalyzer.com.**
- Blue Cross recognizes that there are different methodologies that can be used to arrive at the appropriate CPT code. However, we’ll adhere to the EDC Analyzer tool, which uses ICD-10 and CPT codes as the basis for E/M selection.
- This is how EDC Analyzer claims will be processed:
- Hospitals that are reimbursed through a fee schedule for outpatient services won’t have their claims denied, but instead will be reimbursed using the EDC Analyzer recommended code.
- Hospitals that are reimbursed a percentage of the charge for outpatient services will have their claims denied if submitted with an incorrect code and the recommended E/M code will be reflected on the voucher. Hospitals should rebill with the EDC Analyzer recommended code.
Following Blue Cross Blue Shield of Michigan’s review of facility input, we’ll be moving forward with this program, effective early October 2022. Details about the EDC Analyzer were also presented at the May 16 Staff Liaison Group meeting, which included leadership from the Michigan Health and Hospital Association and Blue Cross, and the PHA Advisory Committee, which was held on June 21.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
We’ve updated Addendum C of Blue Cross’ Ambulatory Surgical Facility Traditional Participation Agreement
Blue Cross Blue Shield of Michigan has made changes to the participating agreement for ambulatory surgical facilities. The changes are to Addendum C, Reimbursement Methodology, and are effective Oct. 1, 2022.
The new participating agreement is accessible from the Ambulatory Surgical Facilities section of Provider Enrollment on bcbsm.com/providers.
Leqvio to have site-of-care requirement for commercial members, starting Aug. 1
Leqvio® (inclisiran), HCPCS code J3590, will have a site-of-care requirement, in addition to its current prior authorization requirement for Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members, starting Aug. 1, 2022.
When the site-of-care requirement goes into effect, this drug may be covered only when administered at the following sites of care:
- Doctor’s or other health care provider’s office
- Ambulatory infusion center
- The member's home, from a home infusion therapy provider
Members who start treatment in a location other than those outlined above prior to Aug. 1, 2022, will be able to continue receiving the drug in that location until their current authorization expires. Providers should then transition members to one of the above sites of care.
Notes:
- Starting July 1, 2022, the HCPCS code for this drug will be J1306.
- This drug is part of members’ medical benefits, not their pharmacy benefits.
- As a reminder, prior authorization requests are submitted using the NovoLogix® online tool.
Some Blue Cross commercial groups not subject to these requirements
For Blue Cross commercial groups, this authorization requirement applies only to groups that currently participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list.
Note: Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don't participate in the standard prior authorization program.
List of requirements
For a full list of requirements related to drugs covered under the medical benefit, see the Blue Cross and BCN utilization management medical drug list for Blue Cross commercial and BCN commercial members. We’ll update this list prior to Aug. 1.
You can access this list and other information about requesting prior authorization at ereferrals.bcbsm.com, at these locations:
Authorization isn't a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members.
Fyarro to require prior authorization for most members, starting Aug. 16
For dates of service on or after Aug. 16, 2022, Fyarro™ (sirolimus protein-bound particles), HCPCS code J9331, will require prior authorization through AIM Specialty Health®. This drug is part of members’ medical benefits, not their pharmacy benefits.
Prior authorization requirements apply when this drug is administered in outpatient settings for:
- Blue Cross Blue Shield of Michigan commercial — Members who have coverage through fully insured groups and members with individual coverage
Note: This requirement doesn’t apply to members who have coverage through Blue Cross commercial self-funded groups, including the Blue Cross and Blue Shield Federal Employee Program® and UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans.
- Medicare Plus Blue℠ members
- Blue Care Network commercial members
- BCN Advantage℠ members
How to submit authorization requests
Submit authorization requests to AIM using one of the following methods:
More about the authorization requirements
Authorization isn’t a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members.
For additional information on requirements related to drugs covered under the medical benefit, see:
- Blue Cross commercial and BCN commercial:
- Medicare Advantage:
We’ll update the pertinent drug lists to reflect the information in this message prior to the effective date.
AIM Specialty Health is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services. For more information, go to our ereferrals.bcbsm.com website.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Fyarro and Tivdak will have requirements for URMBT members with Blue Cross non-Medicare plans
For dates of service on or after Aug. 16, 2022, the drugs listed below will require prior authorization through AIM Specialty Health® and may also have site-of-care requirements, quantity limit requirements or both. These requirements will apply to UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans. These drugs are part of members’ medical benefits, not their pharmacy benefits.
See the table for more information. When a cell is blank, the drug doesn’t have that requirement.
Brand name |
Generic name |
HCPCS code |
Requirements |
Prior authorization |
Site of care |
Quantity limits |
Fyarro™ |
sirolimus protein-bound particles |
J9331 |
✓ |
|
|
Tivdak® |
tisotumab vedotin-tftv |
J9273 |
✓ |
|
|
These requirements apply only when these drugs are administered in an outpatient setting.
Note: These requirements don’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714).
How to submit authorization requests
Submit prior authorization requests to AIM using one of the following methods:
More about the authorization requirements Authorization isn’t a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members.
For additional information on requirements related to drugs covered under the medical benefit for URMBT members with Blue Cross non-Medicare plans, see:
We’ll update the pertinent drug lists to reflect the information in this article prior to the effective date.
Note: Accredo manages prior authorization requests for additional medical benefit drugs for these members.
AIM Specialty Health is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services. For more information, go to our ereferrals.bcbsm.com website.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Fusilev no longer requires prior authorization
Because Spectrum Pharmaceuticals has stopped manufacturing Fusilev® (levoleucovorin), HCPCS code J0641, we no longer require prior authorization through AIM Specialty Health® for dates of service on or after May 31, 2022. The drug was part of members’ medical benefits, not their pharmacy benefits.
This change applies to:
- Blue Cross Blue Shield of Michigan commercial:
- Members who have coverage through fully insured groups
- Members with individual coverage
- UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans
- Medicare Plus Blue℠ members
- Blue Care Network commercial members
- BCN Advantage℠ members
For additional information on requirements related to drugs covered under the medical benefit, refer to the following drug lists:
- Medicare Plus Blue and BCN Advantage members:
What you need to know about submitting medical benefit drug prior authorization requests for Medicare Advantage members
Blue Cross Blue Shield of Michigan and Blue Care Network recently transitioned to a new provider portal, Availity Essentials. You should continue to submit prior authorization requests for most medical benefit drugs, including CAR-T cell therapy drugs, for Medicare Plus Blue℠ and BCN Advantage℠ members in one of the following ways:
- Preferred method: Through the NovoLogix® online tool. See the next section for the steps you need to take to access NovoLogix through Availity®.
- For providers who aren’t able to submit requests through NovoLogix: You have two options:
Preferred method for submitting prior authorization requests
The preferred method continues to be submitting requests through NovoLogix.
Note: If you haven’t already done so, be sure to register for Availity so you can continue to submit requests through NovoLogix.
If you have an Availity account, you have access to NovoLogix.
To submit requests through Availity:
- Log in to our provider portal (availity.com**).
- Click on Payer Spaces on the Availity menu bar.
- Click on the BCBSM and BCN logo.
- In the Applications tab, click on the appropriate tile:
- NovoLogix MAPPO
- NovoLogix BCN/BCN Advantage
Additional information
You can access the Medication Authorization Request Form (for any medication) on the For Providers: How do I Submit a Drug Prior Authorization Request for Medicare Plus Blue PPO and BCN Advantage? page of the bcbsm.com website. Later this year, we’ll remove the medical drug prior authorization request forms for specific medications.
For more information about submitting requests and to view the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members, see the following pages of ereferrals.bcbsm.com website:
**Blue Cross and Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Cortrophin and Ryplazim to have requirements for URMBT members with Blue Cross non-Medicare plans
For dates of service on or after Sept. 1, 2022, the following drugs will require prior authorization through the NovoLogix® online tool and may also have site-of-care requirements, quantity limit requirements or both. These requirements will apply to UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans. These drugs are part of members’ medical benefits, not their pharmacy benefits.
See the table for more information. When a cell is blank, the drug doesn’t have that requirement.
Brand name |
Generic name |
HCPCS code |
Requirements |
Prior authorization |
Site of care |
Quantity limits |
Cortrophin® |
corticotropin |
J3490/J3590 |
✓ |
|
|
Ryplazim® |
plasminogen, human-tvmh |
J3590/C9090 |
✓ |
|
✓ |
These requirements apply only when these drugs are administered in an outpatient setting.
Note: These requirements don’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714).
How to submit authorization requests
Submit prior authorization requests through NovoLogix. It offers real-time status checks and immediate approvals for certain medications.
To learn how to submit requests through NovoLogix, go to our Blue Cross Medical Benefit Drugs page, scroll to the Blue Cross commercial column and review the information in the How to submit authorization requests electronically using NovoLogix section.
More about the authorization requirements
Authorization isn’t a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members.
For additional information on requirements related to drugs covered under the medical benefit for URMBT members with Blue Cross non-Medicare plans, see:
We’ll update the pertinent drug lists to reflect the information in this message prior to the effective date.
Note: Accredo manages prior authorization requests for additional medical benefit drugs for these members.
We’re sharing skilled nursing facilities’ performance reporting for Medicare Advantage members
In late June, Blue Cross Blue Shield of Michigan and Blue Care Network began sharing skilled nursing facility performance data for Medicare Advantage members with providers in risk-based contracts. Information being shared includes member volumes at each facility and specific performance metrics.
This is part of an effort to foster increased collaboration between our health care providers in risk contracts and the skilled nursing facilities that provide services to their patients. “We hope this additional reporting will continue to help build relationships between skilled nursing facilities and the hospital providers sending patients to these facilities,” said Karolina Skrzypek, M.D., medical director with Provider Engagement.
Lunch and learn webinars focus on risk adjustment, coding
Action item
Register now for webinars that can improve your coding processes.
Physicians and coders are invited to attend webinars that provide new information on documentation and coding of common and challenging diagnoses. These live lunchtime educational sessions will include an opportunity to ask questions.
Current schedule
All sessions start at noon Eastern time and generally run for 30 minutes. Click on a link below to sign up.
You can watch previously hosted sessions on our provider training website. Use the keyword “Lunch” to search for the courses. You’ll also find them listed in the Quality management section of the course catalog.
Click here if you are already registered for the site.
To request access to the provider training website:
- Click here to register.
- Complete the registration. We recommend using the same email you use to communicate with Blue Cross Blue Shield of Michigan for other provider-related needs. This will become your login ID.
Previously recorded |
Topic |
April 19 |
Coding and Documentation for HCC Capture and Risk Adjustment |
May 5 |
Coding for Cancer and Neoplasms |
June 16 |
Coding for Heart Disease and Heart Arrythmias |
If you have any questions about the sessions, contact April Boyce at aboyce@bcbsm.com. If you have questions about registration, email Patricia Scarlett at pscarlett@bcbsm.com.
Do we have your medical records request address?
As a reminder, please ensure that we have your correct medical records request address on file. In the April 2022 Record, we let you know we’ll be working with Optum to implement some new edits. Optum is an independent company that contracts with Blue Cross Blue Shield of Michigan to identify professional and facility claims that require additional review.
One component of our relationship with Optum involves medical records requests.
To prevent claim processing delays, we need to keep your medical records request address on file. If you haven’t provided it yet or need to make changes, use the Enrollment and Change Self-Service Tool, located on the Applications tab of our payer space on the provider portal.
Here are the step-by-step directions:
- Log in to our provider portal (availity.com**).
- Click on Payer Spaces on the Availity menu bar.
- Click on the BCBSM and BCN logo.
- Click on Provider Enrollment and Change Self-Service on the Applications tab.
If we don’t have a medical record request address on file, the request will be sent to the mailing address. If there’s no mailing address on file, the request will be sent to the billing address. And if there’s no billing address on file, the request will be sent to the address shown on the claim.
Help us streamline the claim processing process by making sure we have your correct medical records request address on file.
**Blue Cross Blue Shield of Michigan doesn't own or control this website.
Additional procedures codes payable to OPC providers for Blue Cross commercial members, starting July 1
For members with Blue Cross Blue Shield of Michigan commercial plans, we’ve updated our systems to make additional services payable to providers at outpatient psychiatric care facilities.
For dates of service on or after July 1, 2022, the following procedure codes will be payable to the OPC providers specified below for Blue Cross commercial members:
Procedure code |
Payable to |
*98966 |
Clinical psychologists, clinical social workers, limited licensed psychologists, licensed marriage and family therapists, and licensed professional counselors |
*98967 |
*98968 |
*98970 |
*98971 |
*98972 |
*99484 |
Psychiatrists (M.D.s or D.O.s) and certified nurse practitioners |
*99487 |
*99489 |
*99491 |
G2086 |
G2087 |
This change brings the list of procedure codes that are payable to OPC providers for Blue Cross commercial members more in line with those that are payable to OPC providers for Blue Care Network members.
Billing instructions
When billing these procedure codes, include the following in the order specified below:
- The modifier that indicates the licensure level (level of care) for the rendering provider (such as: AH, AJ, HO)
- If the service was delivered via telemedicine: The telemedicine modifier (either GT or 95)
- The place of service:
- If the service was delivered in person: Include place of service 11.
- If the service was delivered via telemedicine: Include place of service code 11, 02 or 10.
To view detailed billing instructions for services delivered via telemedicine, see the “Billing telehealth visits” section of the Telehealth for behavioral health providers document. Refer to the “Outpatient psychiatric care facilities” subsection.
By July 1, we’ll update the Telehealth for behavioral health providers document to reflect the additional codes that are payable for Blue Cross commercial members.
Blue Cross commercial OPC fee schedule
By July 1, we’ll update the OPC fee schedule to reflect this change. You can access the fee schedule as follows:
- Log in to our provider portal (availity.com**).
- Click on Payer Spaces on the Availity menu bar.
- Click on the BCBSM and BCN logo.
- Click on Secure Provider Resources (Blue Cross and BCN) on the Resources tab.
- Choose Fee Schedules > Blue Cross Facility Fee Schedules.
- If prompted, accept the End User License Agreement.
- Click on Outpatient Psychiatric Care on the left.
- Click on the link to open the 2022 fee schedule.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.

Leqvio to have site-of-care requirement for commercial members, starting Aug. 1
Leqvio® (inclisiran), HCPCS code J3590, will have a site-of-care requirement, in addition to its current prior authorization requirement for Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members, starting Aug. 1, 2022.
When the site-of-care requirement goes into effect, this drug may be covered only when administered at the following sites of care:
- Doctor’s or other health care provider’s office
- Ambulatory infusion center
- The member's home, from a home infusion therapy provider
Members who start treatment in a location other than those outlined above prior to Aug. 1, 2022, will be able to continue receiving the drug in that location until their current authorization expires. Providers should then transition members to one of the above sites of care.
Notes:
- Starting July 1, 2022, the HCPCS code for this drug will be J1306.
- This drug is part of members’ medical benefits, not their pharmacy benefits.
- As a reminder, prior authorization requests are submitted using the NovoLogix® online tool.
Some Blue Cross commercial groups not subject to these requirements
For Blue Cross commercial groups, this authorization requirement applies only to groups that currently participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list.
Note: Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don't participate in the standard prior authorization program.
List of requirements
For a full list of requirements related to drugs covered under the medical benefit, see the Blue Cross and BCN utilization management medical drug list for Blue Cross commercial and BCN commercial members. We’ll update this list prior to Aug. 1.
You can access this list and other information about requesting prior authorization at ereferrals.bcbsm.com, at these locations:
Authorization isn't a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members.
Fyarro to require prior authorization for most members, starting Aug. 16
For dates of service on or after Aug. 16, 2022, Fyarro™ (sirolimus protein-bound particles), HCPCS code J9331, will require prior authorization through AIM Specialty Health®. This drug is part of members’ medical benefits, not their pharmacy benefits.
Prior authorization requirements apply when this drug is administered in outpatient settings for:
- Blue Cross Blue Shield of Michigan commercial — Members who have coverage through fully insured groups and members with individual coverage
Note: This requirement doesn’t apply to members who have coverage through Blue Cross commercial self-funded groups, including the Blue Cross and Blue Shield Federal Employee Program® and UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans.
- Medicare Plus Blue℠ members
- Blue Care Network commercial members
- BCN Advantage℠ members
How to submit authorization requests
Submit authorization requests to AIM using one of the following methods:
More about the authorization requirements
Authorization isn’t a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members.
For additional information on requirements related to drugs covered under the medical benefit, see:
- Blue Cross commercial and BCN commercial:
- Medicare Advantage:
We’ll update the pertinent drug lists to reflect the information in this message prior to the effective date.
AIM Specialty Health is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services. For more information, go to our ereferrals.bcbsm.com website.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Fyarro and Tivdak will have requirements for URMBT members with Blue Cross non-Medicare plans
For dates of service on or after Aug. 16, 2022, the drugs listed below will require prior authorization through AIM Specialty Health® and may also have site-of-care requirements, quantity limit requirements or both. These requirements will apply to UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans. These drugs are part of members’ medical benefits, not their pharmacy benefits.
See the table for more information. When a cell is blank, the drug doesn’t have that requirement.
Brand name |
Generic name |
HCPCS code |
Requirements |
Prior authorization |
Site of care |
Quantity limits |
Fyarro™ |
sirolimus protein-bound particles |
J9331 |
✓ |
|
|
Tivdak® |
tisotumab vedotin-tftv |
J9273 |
✓ |
|
|
These requirements apply only when these drugs are administered in an outpatient setting.
Note: These requirements don’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714).
How to submit authorization requests
Submit prior authorization requests to AIM using one of the following methods:
More about the authorization requirements Authorization isn’t a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members.
For additional information on requirements related to drugs covered under the medical benefit for URMBT members with Blue Cross non-Medicare plans, see:
We’ll update the pertinent drug lists to reflect the information in this article prior to the effective date.
Note: Accredo manages prior authorization requests for additional medical benefit drugs for these members.
AIM Specialty Health is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services. For more information, go to our ereferrals.bcbsm.com website.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Fusilev no longer requires prior authorization
Because Spectrum Pharmaceuticals has stopped manufacturing Fusilev® (levoleucovorin), HCPCS code J0641, we no longer require prior authorization through AIM Specialty Health® for dates of service on or after May 31, 2022. The drug was part of members’ medical benefits, not their pharmacy benefits.
This change applies to:
- Blue Cross Blue Shield of Michigan commercial:
- Members who have coverage through fully insured groups
- Members with individual coverage
- UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans
- Medicare Plus Blue℠ members
- Blue Care Network commercial members
- BCN Advantage℠ members
For additional information on requirements related to drugs covered under the medical benefit, refer to the following drug lists:
- Medicare Plus Blue and BCN Advantage members:
What you need to know about submitting medical benefit drug prior authorization requests for Medicare Advantage members
Blue Cross Blue Shield of Michigan and Blue Care Network recently transitioned to a new provider portal, Availity Essentials. You should continue to submit prior authorization requests for most medical benefit drugs, including CAR-T cell therapy drugs, for Medicare Plus Blue℠ and BCN Advantage℠ members in one of the following ways:
- Preferred method: Through the NovoLogix® online tool. See the next section for the steps you need to take to access NovoLogix through Availity®.
- For providers who aren’t able to submit requests through NovoLogix: You have two options:
Preferred method for submitting prior authorization requests
The preferred method continues to be submitting requests through NovoLogix.
Note: If you haven’t already done so, be sure to register for Availity so you can continue to submit requests through NovoLogix.
If you have an Availity account, you have access to NovoLogix.
To submit requests through Availity:
- Log in to our provider portal (availity.com**).
- Click on Payer Spaces on the Availity menu bar.
- Click on the BCBSM and BCN logo.
- In the Applications tab, click on the appropriate tile:
- NovoLogix MAPPO
- NovoLogix BCN/BCN Advantage
Additional information
You can access the Medication Authorization Request Form (for any medication) on the For Providers: How do I Submit a Drug Prior Authorization Request for Medicare Plus Blue PPO and BCN Advantage? page of the bcbsm.com website. Later this year, we’ll remove the medical drug prior authorization request forms for specific medications.
For more information about submitting requests and to view the Medical Drug and Step Therapy Prior Authorization List for Medicare Plus Blue and BCN Advantage members, see the following pages of ereferrals.bcbsm.com website:
**Blue Cross and Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Cortrophin and Ryplazim to have requirements for URMBT members with Blue Cross non-Medicare plans
For dates of service on or after Sept. 1, 2022, the following drugs will require prior authorization through the NovoLogix® online tool and may also have site-of-care requirements, quantity limit requirements or both. These requirements will apply to UAW Retiree Medical Benefits Trust members with Blue Cross non-Medicare plans. These drugs are part of members’ medical benefits, not their pharmacy benefits.
See the table for more information. When a cell is blank, the drug doesn’t have that requirement.
Brand name |
Generic name |
HCPCS code |
Requirements |
Prior authorization |
Site of care |
Quantity limits |
Cortrophin® |
corticotropin |
J3490/J3590 |
✓ |
|
|
Ryplazim® |
plasminogen, human-tvmh |
J3590/C9090 |
✓ |
|
✓ |
These requirements apply only when these drugs are administered in an outpatient setting.
Note: These requirements don’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714).
How to submit authorization requests
Submit prior authorization requests through NovoLogix. It offers real-time status checks and immediate approvals for certain medications.
To learn how to submit requests through NovoLogix, go to our Blue Cross Medical Benefit Drugs page, scroll to the Blue Cross commercial column and review the information in the How to submit authorization requests electronically using NovoLogix section.
More about the authorization requirements
Authorization isn’t a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members.
For additional information on requirements related to drugs covered under the medical benefit for URMBT members with Blue Cross non-Medicare plans, see:
We’ll update the pertinent drug lists to reflect the information in this message prior to the effective date.
Note: Accredo manages prior authorization requests for additional medical benefit drugs for these members.
AllianceRx Walgreens Prime is now AllianceRx Walgreens Pharmacy
Effective June 24, 2022, AllianceRx Walgreens Prime, a provider of specialty pharmacy services, changed its name to AllianceRx Walgreens Pharmacy.
AllianceRx Walgreens Pharmacy will continue to provide Blue Cross Blue Shield of Michigan members with specialty medications used to treat chronic, complex or rare conditions.

Reminder: Members can’t receive prescriptions for DME/P&O items through telehealth visits
As we told you in an October 2018 Record article, effective Nov. 1, 2018, health care providers aren’t able to prescribe or issue durable medical equipment and prosthetic and orthotic supplies during telehealth visits. A telehealth visit doesn’t meet the medical necessity requirements for prescribing these items. Prescription and issuance resulting from a telehealth visit may be subject to audit review and recovery.
A telehealth visit includes:
- Phone call
- Both email and postal mail
- Video chat
All telehealth formats are excluded from issuing DME and prosthetic and orthotic items.
|

 For the second time in three years, Blue Cross Blue Shield of Michigan and Blue Care Network received the J.D. Power Award for ranking first overall with highest member satisfaction among commercial health plans in Michigan. Achieving the top ranking was largely driven by strong scores in coverage and benefits, provider choice and information and communication.
For the second time in three years, Blue Cross Blue Shield of Michigan and Blue Care Network received the J.D. Power Award for ranking first overall with highest member satisfaction among commercial health plans in Michigan. Achieving the top ranking was largely driven by strong scores in coverage and benefits, provider choice and information and communication. If you’re looking for training or have questions about the new Blue Cross Blue Shield of Michigan and Blue Care Network provider portal, Availity Essentials, take advantage of the following resources.
If you’re looking for training or have questions about the new Blue Cross Blue Shield of Michigan and Blue Care Network provider portal, Availity Essentials, take advantage of the following resources.