
Subscribe | The Record Archive | Contacts | bcbsm.com
|
January 2021
No-cost COVID-19 treatment extended through March 31, 2021As the pandemic continues, Blue Cross Blue Shield of Michigan and Blue Care Network want to ensure that members can get the care they need during these difficult times. We are extending the time frame for waiving the member cost share for COVID-19 treatment through March 31, 2021. The coverage applies to Blue Cross, BCN, Medicare Plus Blue℠, BCN Advantage℠ and Medigap plans. We’ll also continue to cover physician-approved testing and associated services for the duration of the public health emergency, as required by federal guidelines. For more information, see our news release. You can read about changes we’ve implemented for COVID-19 at bcbsm.com/coronavirus or log in to Provider Secured Services and click on Coronavirus (COVID-19). Note: Some commercial self-funded groups are extending the waiver of member cost share. In addition, the Michigan Education Special Services Association, known as MESSA, and some Medicare Advantage groups have a different end date for the waiver of member cost share. Providers are encouraged to submit claims to Blue Cross and BCN and wait for the voucher before charging member cost share, if applicable.
Get ready for Availity: How to select an administratorPrevious articles about Availity
Choose a primary administrator Select someone who knows each team member’s access needs, or create an internal process for the primary administrator to review and confirm access needs. The goal is to make sure team members have access only to the roles and permissions they need to do their jobs. A primary administrator who controls access helps safeguard patient information, maintain compliance with federal privacy and security laws, and reduce opportunities for fraud and abuse. This ensures that:
Also, your primary administrator will be able to add team members or change access needs with just a few keystrokes. This will replace having to fax a form for every change. The primary administrator can have help
Start thinking about the administrator structure that will work best for your organization, so you’ll be able to register in the coming months. Availity will make the administration tasks easy with training, forums and reports. Questions? If you need immediate assistance or have a question specific to a certain member or situation, use our website resources or contact Provider Inquiry. Web resources:
Provider Inquiry numbers are available at bcbsm.com/providers.
Call the Blue Cross Web Support Help Desk at 1-877-258-3932 if you have problems with the current Blue Cross Provider Secured Services site.
Blue Cross amends procedures eligible for pilot program to promote pain control through limiting post-operative opioid dispensing
The following surgical groupings will be eligible for the modifier 22 billing, effective Jan. 1, 2021, and will remain eligible through Dec. 31, 2022:
The following surgical groupings will be extended until Dec. 31, 2021
The following surgical groupings will no longer be eligible for modifier 22, effective April 1, 2021:
Using modifier 22 To submit your attestation statement indicating that appropriate protocols were included as part of the surgery, follow the process for submitting medical records and other claim attachments when appending modifier 22 to a qualifying procedure. For details, see the “Claims” chapter of the provider manual. Also, to bill modifier 22 for adherence with the Pain Control Optimization Pathway, the physician agrees to follow the prescribing recommendations of the Michigan Opioid Prescribing Engagement Network, or Michigan-OPEN. For information, click here.** The physician also agrees to the following guidelines:
Background In 2018, the payment policy was modified to allow surgeons to report modifier 22 for an additional 35% reimbursement when pain control optimization protocols are used to support the surgery. The initial period of the pilot program included the following surgical categories:
Due to the success of the pilot program, we expanded the program to also include the following surgical groupings in July 2019:
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Blue Cross doesn’t reimburse providers for experimental drugsBlue Cross Blue Shield of Michigan and Blue Care Network won’t reimburse providers for experimental drugs, effective Jan. 1, 2021. This applies to all claims submitted for Blue Cross commercial, Medicare Plus Blue℠, BCN commercial and BCN Advantage℠ members. When you bill these types of drugs on a UB-04 for inpatient services, use the correct revenue code and modifiers for experimental drug usage. Use revenue code 0256 – experimental drugs, along with the appropriate Advance Beneficiary Notice of Noncoverage modifier (GA, GX, GY, GZ). Health care providers may not bill members for such services unless, prior to the services, all these requirements are met:
The member understands that Blue Cross won’t reimburse the provider for the service.
New ICD-10-CM/PCS COVID-19 diagnosis and procedure codes now availableThe Centers for Medicare & Medicaid Services, in conjunction with the Centers for Disease Control and Prevention and the National Center for Health Statistics, has released a January ICD-10-CM/PCS code update, which will be effective with dates of service on or after Jan. 1, 2021. The update was released in response to the national emergency that was declared due to the COVID-19 outbreak. It includes six new ICD-10-CM (diagnosis) codes and 21 ICD-10-PCS (inpatient procedure) codes to capture COVID-19 diagnoses and inpatient procedures for COVID-19. We’ve created a document listing the new codes. For more information, visit the ICD-10 section** of the CMS website:
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
2021 HCPCS codes delayed, CPT Update document publishedAs you may have read in a web-DENIS message posted Nov. 18, the Centers for Medicare & Medicaid Services delayed release of its 2021 HCPCS codes. Due to the delay in publishing the codes and the final rules, Blue Cross Blue Shield of Michigan anticipates a delay in updating its claims processing systems. We’re preparing a contingency plan to ensure that the codes are accepted and implemented as soon as possible. 2021 CPT codes Each year, we publish our HCPCS Update document, containing new and deleted HCPCS and CPT codes, and post it on web-DENIS. But this year, because of the delay, we’re publishing a CPT codes-only document. Once the HCPCS codes are received and go through the appropriate Blue Cross review and implementation process, we’ll update the document to include both the CPT and the HCPCS codes for 2021. To access the 2021 CPT Update from web-DENIS, follow these steps:
We’ll provide updates via web-DENIS or The Record as soon as the document is updated to include HCPCS codes for 2021.
Learn to conduct a physical exam using telemedicineGretchen C. Goltz, D.O., a Blue Cross Blue Shield of Michigan medical director, has created a training video to help health care providers conduct thorough physical exams using audio and visual telemedicine. It covers the following aspects of the exam:
Click here to see the video. None of the information included in the video is intended to be medical advice.
Mi-COVID19 registry earns national recognitionBlue Cross Blue Shield of Michigan’s Collaborative Quality Initiative program was recently awarded the Blue Cross and Blue Shield Association’s Fast Network Best Practice Prize. We won the prize for the rapid development and implementation efforts of the Mi-COVID19 registry through the Hospital Medicine Safety, or HMS, Collaborative Quality Initiative. The 2020 Fast Network Best Practice Prize recognized plans demonstrating innovations for improving health equity and addressing the effects of the COVID-19 pandemic. Blue Cross Blue Shield of Michigan was a finalist among 12 other Blue plans demonstrating the effectiveness of CQI programs in rapidly bringing together providers across the state to implement quality improvement initiatives, particularly in times of crisis. The goal of HMS has been to improve the quality of care for hospitalized medical patients who are at risk for adverse events. In April 2020, within weeks of the pandemic hitting Michigan, HMS launched a clinical registry focused on Michigan patients hospitalized with COVID-19. The purpose of this initiative was to quickly obtain data to understand this patient population and help support clinical decision-making across Michigan. The Mi-COVID19 initiative consisted of 40-plus hospitals and health systems across the state of Michigan. They worked together to share and learn best practices to improve care for patients with COVID-19. Participating hospitals in the Mi-COVID19 clinical data registry have performed rigorous chart abstractions of patients hospitalized with COVID-19. Here are the goals of collecting data from the patients’ medical records:
A recent study conducted through the COVID-19 initiative uncovered widespread unnecessary prescribing of antibiotics for early patients. When COVID-19 cases were peaking in the spring, more than half of hospitalized patients suspected of having the virus received antibiotics, just in case they had a bacterial infection. Yet testing showed that more than 96% of them only had the coronavirus — which isn’t affected by antibiotics. Based on the study findings, inpatient COVID-19 treatment guidelines have been updated and can help providers across the country supply better care for patients. The rapid speed in which the COVID-19 CQI could be pulled together is further proof that the platform and support provided by Blue Cross Blue Shield of Michigan can make a big difference when emerging health crises develop. As the pandemic continues, HMS is launching a sepsis initiative across 15 pilot hospitals starting in first-quarter 2021. The initiative will incorporate key elements from the COVID-19 data collection into the quality improvement efforts for sepsis care. About CQIs The award-winning CQI model is the first of its kind nationally and is internationally recognized as an innovative approach to improving health care quality and value. CQI findings are routinely published in peer-reviewed literature, and best practices discovered in Michigan are widely implemented across the globe. The CQI platform has been profiled in presentations in more than 30 countries on five continents. Click here for more information about the award-winning CQI model. Billing chart: Blues highlight medical, benefit policy changesYou’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart. This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures. You will also see that descriptions for the codes are no longer included. This is a result of recent negotiations with the AMA on use of the codes. We will publish information about new BCBS groups or changes to group benefits under the Group Benefit Changes heading. For more detailed descriptions of the BCBSM policies for these procedures, please check under the Medical/Payment Policy tab in Explainer on web-DENIS. To access this online information:
Starting Jan. 1, Northwood is Blue Cross’ DME/POS program benefits managerStarting Jan. 1, 2021, Northwood Inc. will administer and manage all aspects of durable medical equipment, prosthetics, orthotics and medical supply benefits for Blue Cross Blue Shield of Michigan commercial fully insured and individual members who reside in the state of Michigan. Only members in groups enrolled in the program are required to participate. Blue Care Network, BCN Advantage℠, and Medicare Plus Blue℠ are already part of the tailored network arrangement with Northwood. Northwood will administer:
DME/POS program categories and examples of services include: Standard equipment
Labor-intensive equipment
Body supports and limbs
Medical or surgical supplies
Prior authorization
Participation
If you have additional questions about the DME/POS management program, contact Northwood Provider Relations at 1-800-447-9599 between 8:30 a.m. and 5 p.m. Eastern time Monday through Friday. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
We’re expanding access to diabetes monitoring products for commercial members, starting in JanuaryStarting Jan. 1, 2021, diabetes monitoring products, such as glucometers and test strips, lancets, continuous glucose monitors and insulin delivery devices, will be added to the pharmacy benefit for Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members. Members will be able to obtain diabetes monitoring products or supplies through participating pharmacies or through durable medical equipment providers, as outlined below. Participating pharmacies Select glucometers and continuous glucose monitors will be available through members’ pharmacy benefit with no cost sharing. Other diabetes supplies will be covered according to the drug list for the member’s plan. The appropriate pharmacy cost sharing or copayment will apply. Glucometers and continuous glucose monitoring products that are available with no cost sharing include:
Durable medical equipment providers Members can also obtain diabetes monitoring products through a DME provider. The process to locate DME providers varies depending on a member’s plan:
A Northwood icon appears next to each Northwood network provider.
What this change means This change effects members as follows:
Reminder: We’re expanding our cardiology services authorization program with AIM for some membersStarting Jan. 1, 2021, we’re adding some cardiology services that will require authorization by AIM Specialty Health® for Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members. The services include cardiac implantable devices and arterial ultrasound for dates of service on or after Jan. 1, 2021. Please refer to the November 2020 Record article for more information.
We’re making a professional payment policy change for select procedures done in ambulatory surgical facilitiesBlue Cross Blue Shield of Michigan recognizes that for certain procedures, additional effort is required and additional costs are incurred when performed outside of a hospital setting. Starting Feb. 1, 2021, the PPO physician reimbursement policy will increase allowed amounts by 15% for select procedures when done in an ambulatory surgical facility. For a preliminary list of the CPT codes for these procedures, click here. Note: This is in addition to the procedures identified in the May 2020 Record article, with payment policy that was adjusted in July 2020. We’ll continue to closely monitor our list of eligible procedures and adjust it based on provider input and other factors, including the effectiveness of the policy. Any other procedures not listed will be paid at the published rate.
AIM to handle prior authorization for some high-tech radiology services for Michigan FEP membersStarting Feb. 1, 2021, AIM Specialty Health® will handle select high-tech radiology services for Michigan Blue Cross and Blue Shield Federal Employee Program® members receiving services in Michigan. AIM is an independent company that manages authorizations of select services for Blue Cross Blue Shield of Michigan. Providers must request authorization from AIM prior to the services being performed. Authorization requests for these services can be submitted on and after Jan. 18, 2021, for services performed on or after Feb. 1, 2021. Note: For dates of service prior to Feb. 1, 2021, prior authorization for high-tech radiology from AIM isn’t required for high-technology radiology services covered under the medical benefit for FEP Blue Cross and Blue Shield Service Benefit Plan members.
AIM will review prior authorizations for the following — MRI, MRA, CT and PET. For a list of the procedure codes that require prior authorization through AIM, click here. How to submit authorization requests Submit authorization requests using one of the following methods:
As a reminder, requests should be submitted before the services are provided. Questions? If you have questions, call AIM at 1-800-728-8008 or visit the AIM website.** You can also contact your provider consultant. Additional information For requirements related to high-tech radiology services covered under the medical benefit for Blue Cross Blue Shield of Michigan commercial members and for Blue Care Network commercial members, refer to the ereferrals.bcbsm.com website. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Starting March 1, changes coming to site-of-care requirements for Blue Cross commercial and BCN commercial pediatric membersBeginning March 1, 2021, site-of-care exemptions will no longer apply to pediatric Blue Cross Blue Shield of Michigan commercial members and pediatric Blue Care Network commercial members for some drugs covered under the medical benefit. This means all drugs that have site-of-care requirements for adult commercial members will have the same site-of-care requirements for pediatric commercial members. For these drugs:
Notes
Definition of pediatric members Pediatric members are defined as one of the following:
More about the authorization requirements
How to submit authorization requests Submit authorization requests through the NovoLogix® online tool. It offers real-time status checks and immediate approvals for certain medications. To learn how to submit requests through NovoLogix, go to ereferrals.bcbsm.com and do the following:
Lists of requirements
Update: Oncology management program for Blue Cross fully insured commercial members doesn’t include codes S0353, S0354We wrote in the September edition of The Record that Blue Cross Blue Shield of Michigan expanded its medical oncology management program to include all fully insured commercial members starting Dec. 1, 2020. The program is administered by AIM Specialty Health®. However, because of an update to the program, providers can’t bill or receive the enhanced reimbursement for codes S0353 or S0354 for Blue Cross commercial fully insured members. This change doesn’t apply to Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members or to UAW Retiree Medical Benefits Trust non-Medicare members. For those members, providers can bill and be reimbursed for codes S0353 and S0354. The Oncology management program: Frequently asked questions for providers document has been updated to reflect this change. Look in the section titled “About enhanced reimbursement.” Find the FAQ at ereferrals.bcbsm.com on the Blue Cross AIM-Managed Procedures page.
Authorization for IOP treatment no longer required for State of Michigan enrollees starting in JanuaryProviders will no longer need to obtain authorization for intensive outpatient services from New Directions Behavioral Health for State of Michigan enrollees (group number 007000562), starting Jan. 1, 2021. Previously, the State of Michigan was one of the few groups that required authorization for IOP services. Authorization will continue to be required for all higher level of behavioral health care admissions for which State of Michigan enrollees have a benefit, including acute inpatient psychiatric, substance use disorder acute detox and residential care, psychiatric and SUD partial hospitalization, and outpatient applied behavioral analysis treatment for autism. Providers and office staff can log in to WebPass** to request prior authorizations for State of Michigan members. Providers who’ve never utilized WebPass before can visit the website** to review a training tutorial on how WebPass works. Reminder
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Reminder: Providers must submit authorization requests to TurningPoint for musculoskeletal procedures for most membersAs we reported in the November issue of The Record and the November-December issue of BCN Provider News (Page 46), TurningPoint Healthcare Solutions LLC has expanded its surgical quality and safety management program for dates of service on or after Jan. 1, 2021. You now need to submit authorization requests for orthopedic, pain management and spinal procedures to TurningPoint for the following groups and members:
Some important reminders
Webinar training Professional provider training includes information about TurningPoint’s clinical model, operational changes and provider portal.
Facility training includes information about TurningPoint’s clinical model and operational changes and the facility verification process.
Portal training includes information about using the TurningPoint provider portal.
Where to find more information To view the lists of codes for which TurningPoint manages authorizations, see Musculoskeletal procedure codes that require authorization by TurningPoint. For detailed information, see Musculoskeletal procedure authorizations: Frequently asked questions for providers.
Medical specialty drug prior authorization list will change in January for Blue Cross commercial fully insured groupsFor dates of service on or after Jan. 18, 2021, we’re adding prior authorization requirements for the following specialty drugs covered under the medical benefit for Blue Cross Blue Shield of Michigan commercial fully insured groups, with the exception of the Michigan Education Special Services Association and the Blue Cross and Blue Shield Federal Employee Program®:
Providers must request prior authorization for these drugs through AIM Specialty Health®. How to submit authorization requests Submit authorization requests to AIM using one of the following methods:
For information about registering for and accessing the AIM ProviderPortal℠, see the Frequently asked questions page** on the AIM website. Authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. For additional information on requirements related to drugs covered under the medical benefit, see the Blue Cross and BCN utilization management medical drug list and the Medical oncology prior authorization list. We’ll update these lists to reflect these changes prior to the effective dates. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Changes coming Jan. 1 for preferred, clinical, custom and custom select drug listsWe recently published an article that detailed changes to the Preferred Drug List, starting Jan. 1, 2021. We’re making an update to the exclusion information: Cimzia® and Kevzara® will remain on the Preferred Drug List. These drugs won’t be excluded. 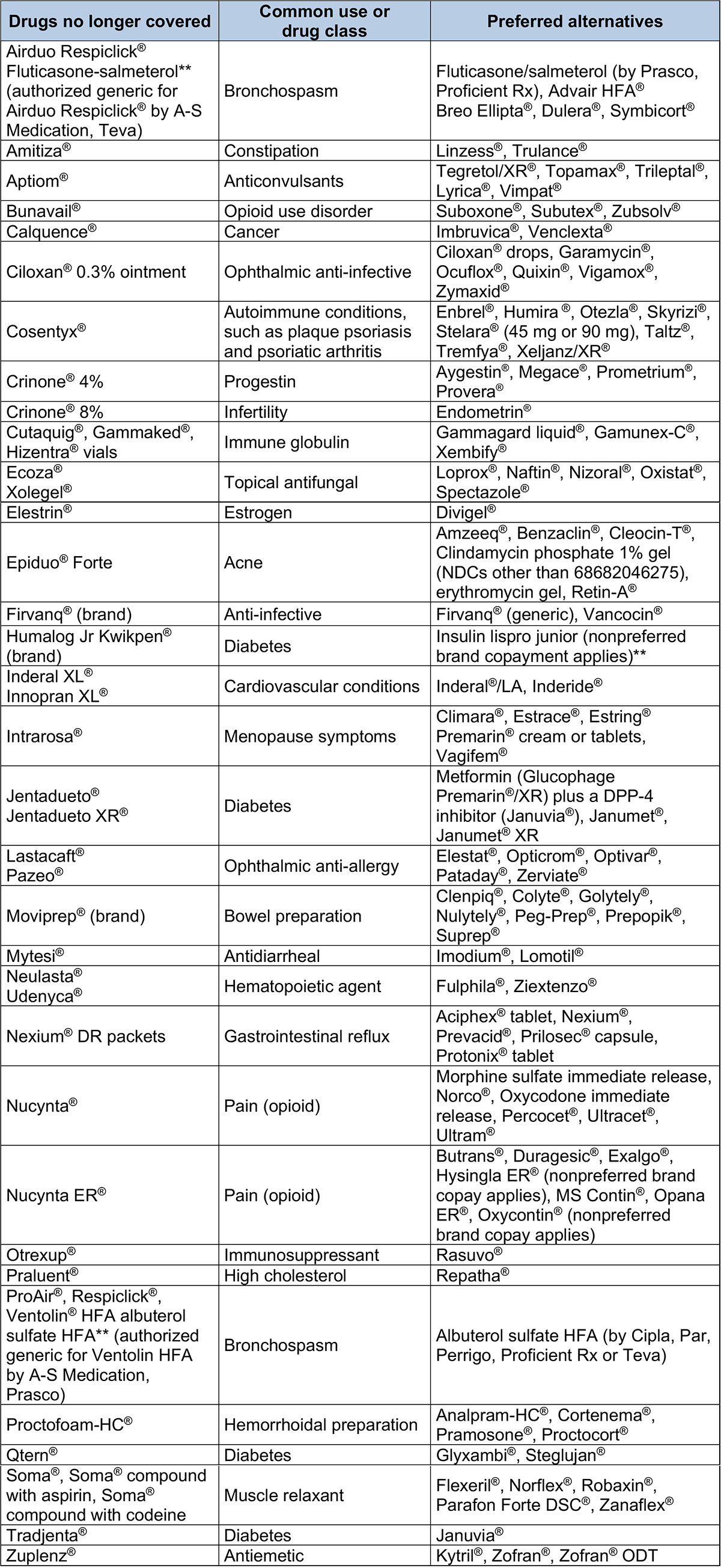 Drugs with a higher copayment – Preferred Drug List 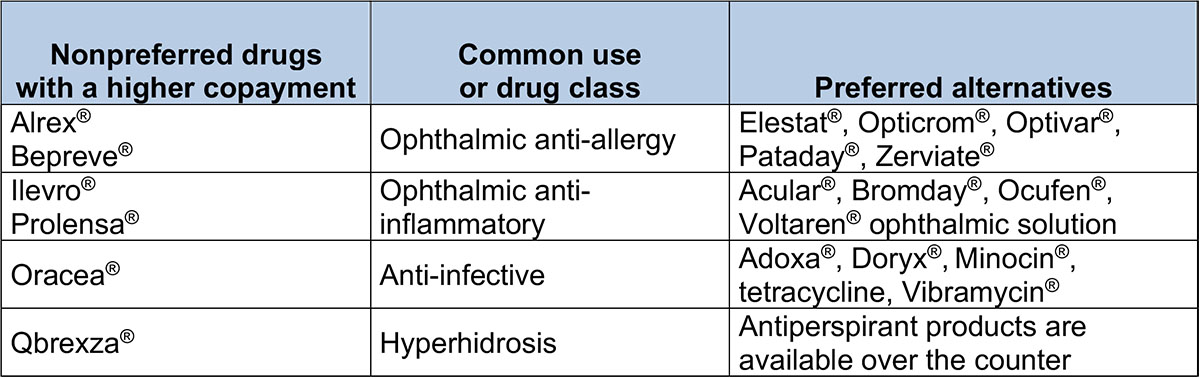 Drugs with quantity limits – Preferred Drug List 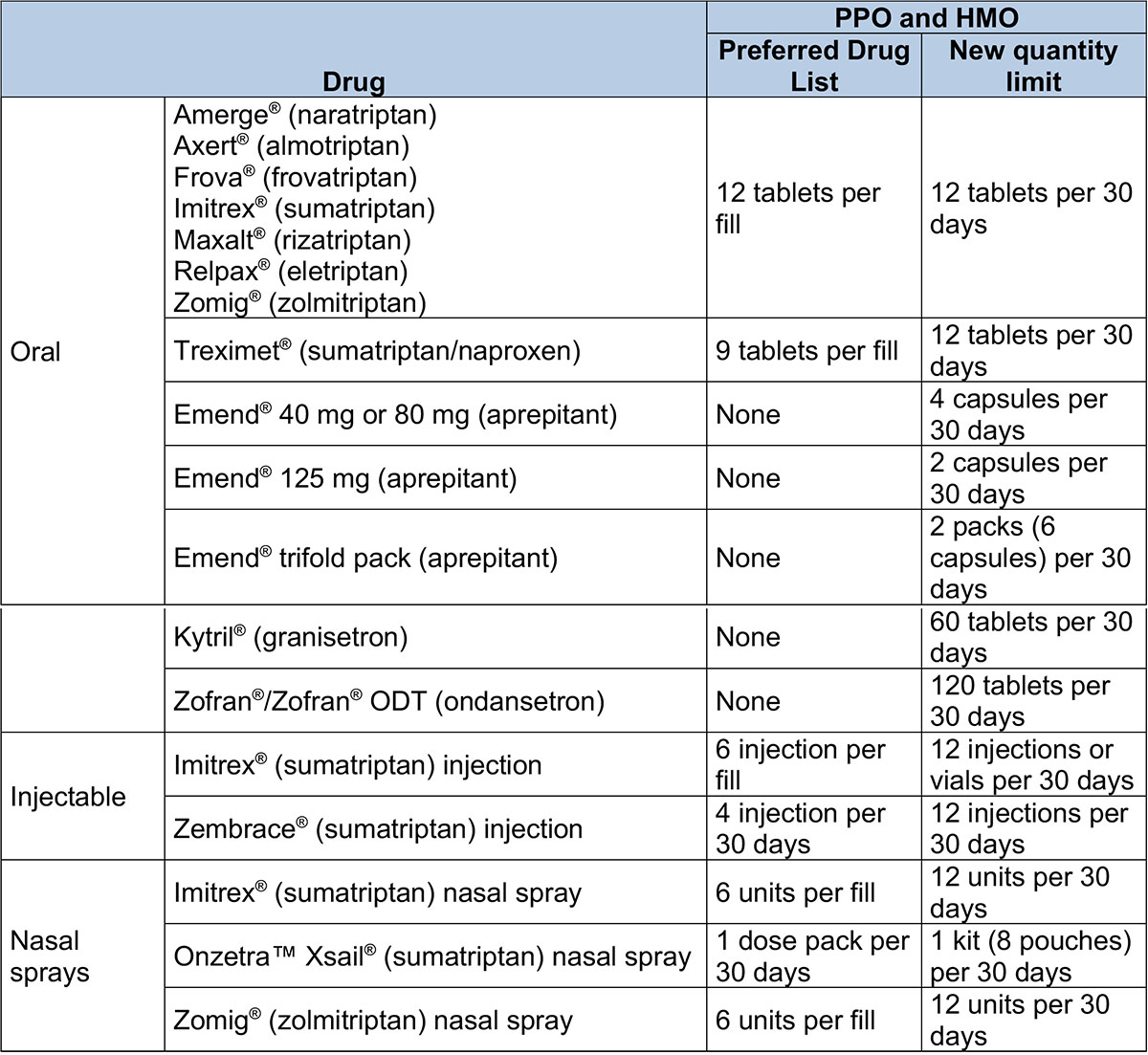 Clinical, Custom and Custom Select Drug List changes Drugs no longer covered – Clinical and Custom Drug lists 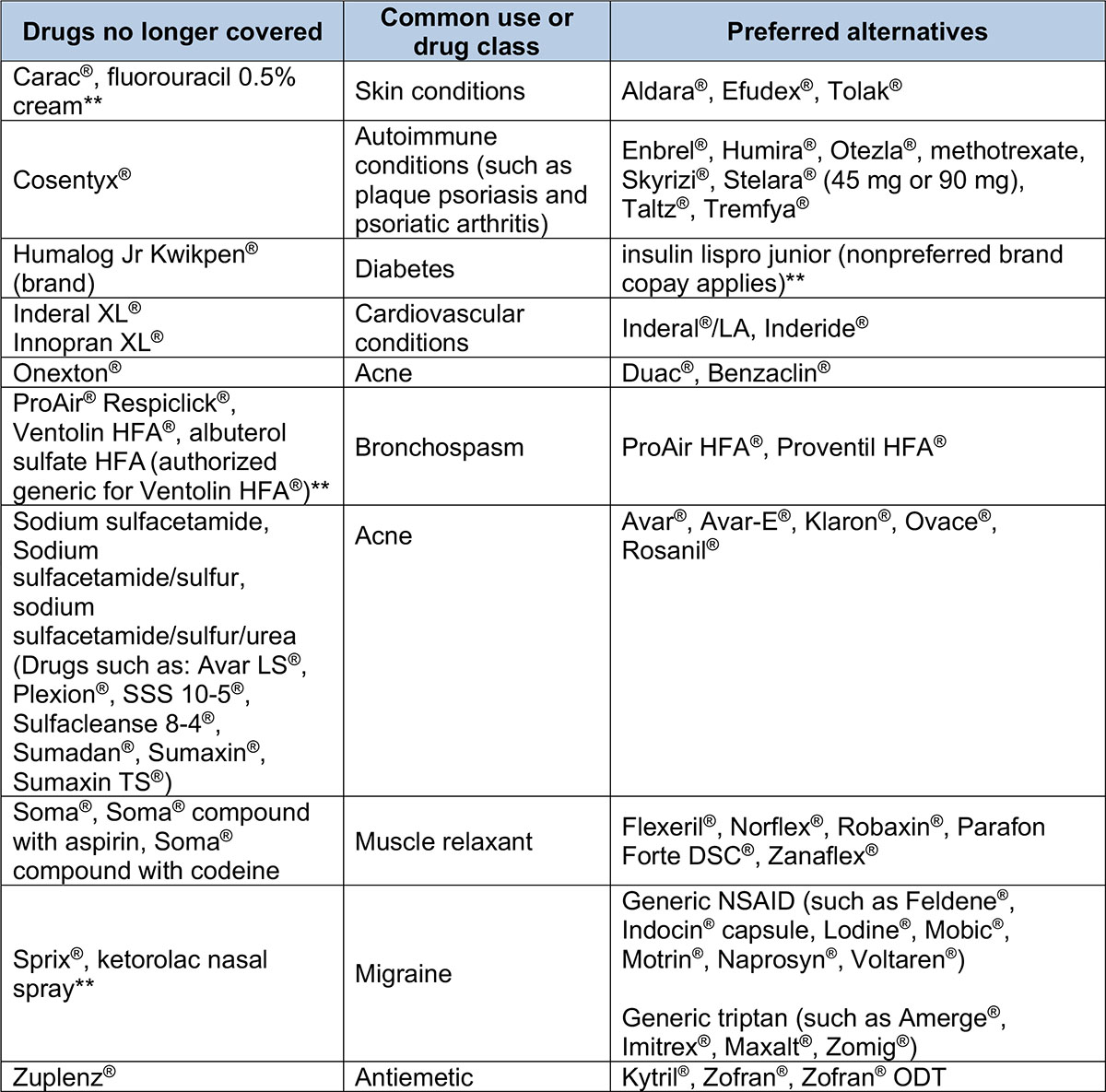 Drugs with a higher copayment – Custom Drug List 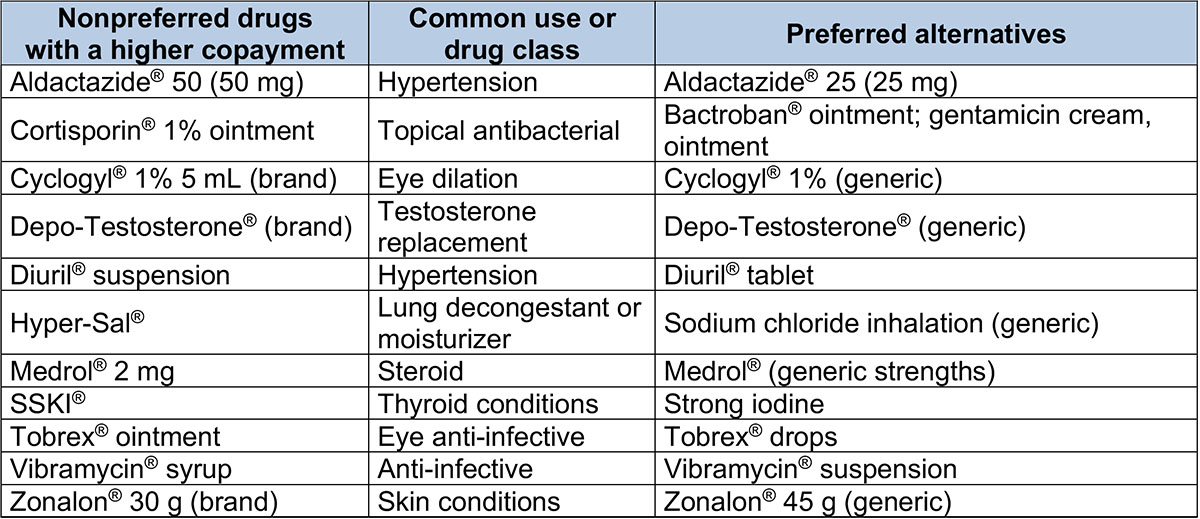 Drugs no longer covered – Custom Select Drug List 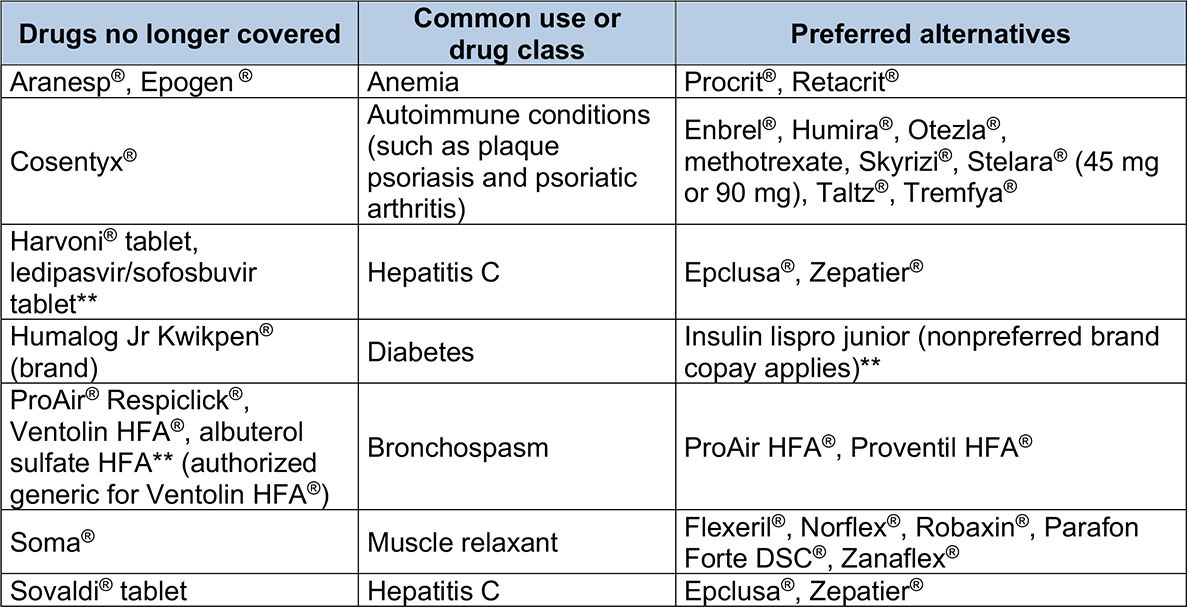 Drugs with quantity limits – Clinical, Custom and Custom Select Drug lists 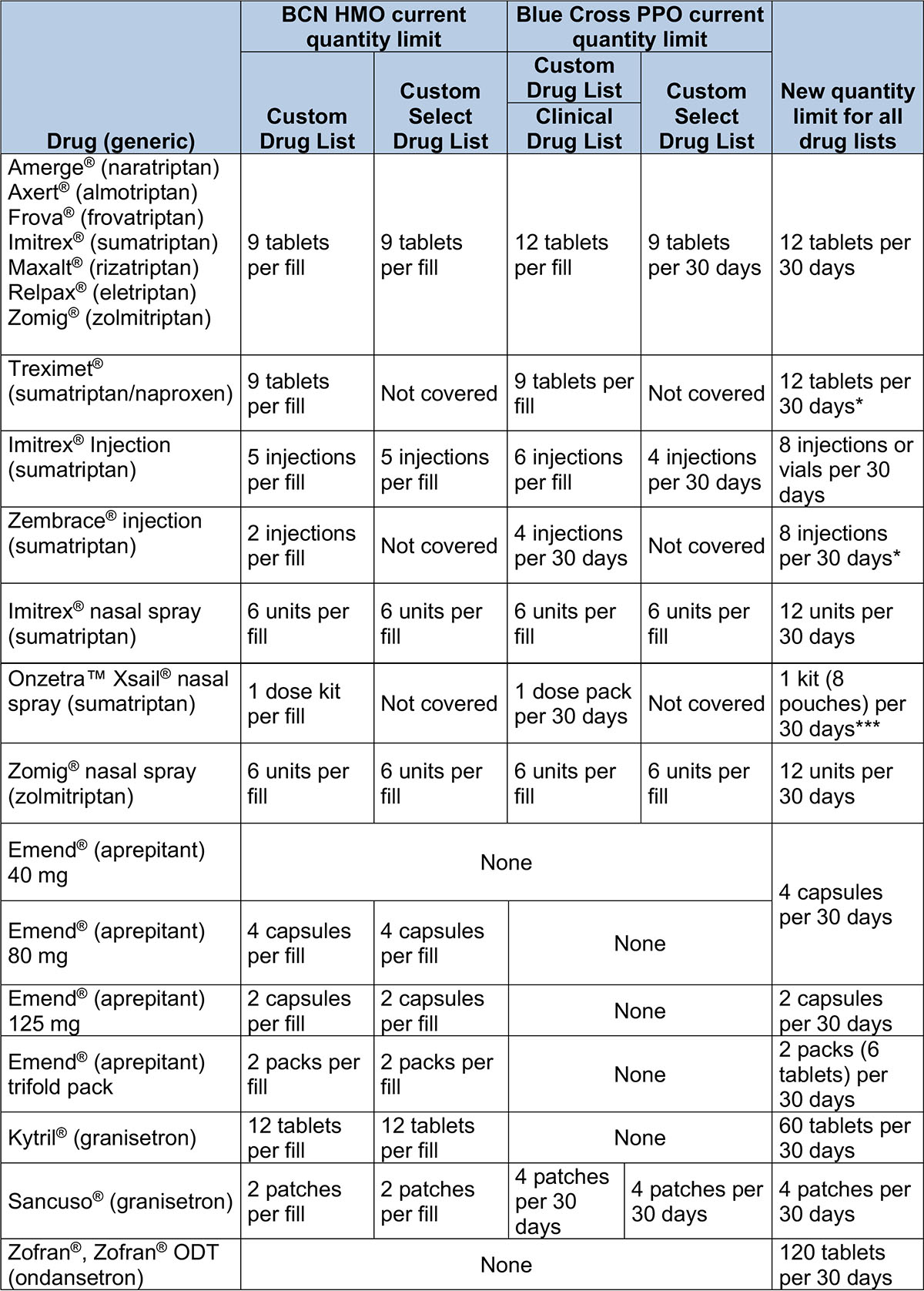 **Represents drugs that have brand names without generic equivalents. These may be considered “authorized generics,” which are the same as brand-name drugs but aren’t true generic drugs. ***Doesn’t apply to members whose plans use the Custom Select Drug List.
Manufacturer discontinues Zostavax shingles vaccinePharmaceutical company Merck announced it has discontinued the Zostavax® vaccine, a vaccine for the prevention of shingles in adults age 60 and older. All remaining product had an expiration date of November 2020, and Zostavax is no longer available for use in the United States. On Dec. 1, 2020, Blue Cross Blue Shield of Michigan and Blue Care Network commercial pharmacy stopped covering the Zostavax vaccine. Pharmacy claims for Zostavax will reject at the point of sale as of Dec. 1, 2020. Blue Cross and BCN will continue to offer the Shingrix® shingles prevention vaccine for adults age 50 and older.
Expansion of drug waste avoidance program starts March 1To minimize drug waste, reduce unnecessary drug exposure and decrease the risk of adverse events, we’re expanding our waste avoidance program to include additional drugs, effective March 1, 2021. This change affects Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members who receive these drugs:
When this change takes effect, dosing for these therapies will be based on weight and will be specific to:
This change will apply to members who start therapy and members whose authorizations are renewed on or after March 1. Members whose current authorizations for these drugs extend past March 1, 2021, can continue at their current dose until their authorization expires. Members not affected by this change This change doesn’t apply to:
Lists of requirements To view the requirements for these drugs, see the following drug lists:
We’ll update these drug lists with this information about the change in dosing strategy before March 1. **In addition to Blue Cross commercial and BCN commercial members, the dosing strategy change for this drug applies to UAW Retiree Medical Benefits Trust non-Medicare members.
Revision to Medicare Plus Blue payment policy for transvaginal and pelvic ultrasoundsBeginning April 1, 2021, for Medicare Plus Blue℠ members, we won’t pay for both a transvaginal ultrasound and a pelvic ultrasound if they’re both performed in the same session. A transvaginal ultrasound (CPT code *76830) is a diagnostic test providing a look at the female reproductive organs. A pelvic ultrasound (CPT code *76856 or *76857) typically evaluates the same organs and represents a redundancy in services. In extenuating circumstances, a provider may submit medical records on the clinical editing appeal form supporting the medical need for both procedures. Indications that may result in payment of both ultrasounds may include the inability to visualize all the structures or a finding of some pathology extending outside the pelvis. These should be clearly documented in the medical record and should be unique to the individual member.
Sign up for additional training webinarsProvider Experience is continuing its series of training webinars for health care providers and staff. The webinars are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network. Here’s information on the upcoming training webinars:
The Blue Cross 201 webinar series provides an in-depth learning opportunity and builds on information shared in our Blue Cross 101: Understanding the Basics webinar. This new webinar reviews the processes and tools available when submitting claims. The Autism Overview webinar reviews current processes related to providing services to members with autism. Recordings of previous webinars are available on web-DENIS via the Blue Cross Provider Publications and Resources or BCN Provider Publications and Resources pages as follows. Blue Cross Provider Publications and Resources
You can also get more information about online training, presentations and videos by clicking on the E‑Learning icon at the top of the page. BCN Provider Publications and Resources
As additional training webinars become available, we’ll provide notices through
Here are 2021 FEP benefit changesBlue Cross and Blue Shield Federal Employee Program® 2021 benefit changes will take effect Jan. 1, 2021. Below is an overview of the benefit changes. Complete information on benefit changes for Standard Option, Basic Option and FEP Blue Focus plans are available at www.fepblue.org/brochure. Catastrophic out-of-pocket maximum
Hearing aids
Hepatitis C screening
HIV screening
Hospice
Nutritional counseling
Outpatient emergency room facility
Pharmacy
Telemedicine
X-rays
If you have any questions about benefit changes, contact Customer Service at 1-800-482-3600.
Reminder: Peer-to-peer review request process to change for inpatient medical hospital admissionsAs you may have read in a web-DENIS message posted Nov. 23 and a December Record article, the process for requesting peer-to-peer reviews for inpatient medical hospital admissions is changing. Please use the following information as your reference on this matter. Effective Jan. 4, 2021, the process for requesting peer-to-peer reviews for inpatient medical hospital admissions will change. Here are the changes that go into effect on that date:
We're updating documents We're updating the document titled How to request a peer-to-peer review with a Blue Cross or BCN medical director to reflect the changes in the process for all lines of business. The updated document will be available starting Jan. 4 on our ereferrals.bcbsm.com website on these webpages:
We’re also updating the provider manuals to reflect the changes related to peer-to-peer-review request. Guidelines for submitting clinical information Follow these guidelines when submitting prior authorization requests for inpatient hospital admissions:
If a request is pended for clinical review, our clinicians will use the clinical information you’ve submitted to support a medical necessity determination. How to expedite review of the authorization request Here are some things you can do to expedite review of the authorization request and possibly avoid the need to request a peer-to-peer review:
Facilities required to prorate respiratory therapy servicesBlue Cross Blue Shield of Michigan and Blue Care Network will require facilities to prorate daily respiratory therapy services by hours used, not to exceed 24 hours in a single day. This billing rule is effective Jan. 1, 2021, for Blue Cross commercial, Medicare Plus Blue℠, BCN commercial and BCN Advantage℠ members. It applies to an inpatient setting only. The following is a list of general respiratory therapy services applicable to this billing policy:
Billing example On a single day of service, a patient is on the ventilator for five hours and then weaned to CPAP for the remaining 19 hours of the day. Previously, services were billed at a daily rate, regardless of hours used. New billing should reflect only those hours used for each modality. Background Respiratory therapy services are prescribed by a physician or non-physician practitioner for the assessment and diagnostic evaluation, treatment, management and monitoring of patients with deficiencies and abnormalities of cardiopulmonary function. This billing policy isn’t intended to affect physician decision-making; providers are expected to apply medical judgment when caring for all members.
Facilities can’t bill for separate labs when using point-of-care testing for blood gas analysisWhen blood analysis is completed by point-of-care testing in an inpatient hospital setting, Blue Cross Blue Shield of Michigan and Blue Care Network will only pay for the primary charge (per time and date of service) that the blood was analyzed — not for other associated or separately billed labs. Separate labs should be zero-priced when billed and will be considered a provider write-off. This policy is effective Jan. 1, 2021, for Blue Cross commercial, Medicare Plus Blue℠, BCN commercial and BCN Advantage℠ members. Background Blood gas analysis performed by point-of-care testing, or utilization of a blood gas analyzer, is prescribed by a physician, or a non-physician practitioner, to provide quick laboratory testing using one sample of blood to achieve multiple test results within minutes. It can affect the treatment and management of the patient. This billing policy isn’t intended to affect provider decision-making or patient care. Providers are expected to apply medical judgment when caring for all members. The following is a list of common point-of-care testing or blood gas analyzer devices that are covered by this billing policy:
The following is a list of commonly associated, but separately billed labs. These include, but aren’t limited to:
We’re expanding access to diabetes monitoring products for commercial members, starting in JanuaryStarting Jan. 1, 2021, diabetes monitoring products, such as glucometers and test strips, lancets, continuous glucose monitors and insulin delivery devices, will be added to the pharmacy benefit for Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members. Members will be able to obtain diabetes monitoring products or supplies through participating pharmacies or through durable medical equipment providers, as outlined below. Participating pharmacies Select glucometers and continuous glucose monitors will be available through members’ pharmacy benefit with no cost sharing. Other diabetes supplies will be covered according to the drug list for the member’s plan. The appropriate pharmacy cost sharing or copayment will apply. Glucometers and continuous glucose monitoring products that are available with no cost sharing include:
Durable medical equipment providers Members can also obtain diabetes monitoring products through a DME provider. The process to locate DME providers varies depending on a member’s plan:
A Northwood icon appears next to each Northwood network provider.
What this change means This change effects members as follows:
Reminder: We’re expanding our cardiology services authorization program with AIM for some membersStarting Jan. 1, 2021, we’re adding some cardiology services that will require authorization by AIM Specialty Health® for Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members. The services include cardiac implantable devices and arterial ultrasound for dates of service on or after Jan. 1, 2021. Please refer to the November 2020 Record article for more information.
We’re making a professional payment policy change for select procedures done in ambulatory surgical facilitiesBlue Cross Blue Shield of Michigan recognizes that for certain procedures, additional effort is required and additional costs are incurred when performed outside of a hospital setting. Starting Feb. 1, 2021, the PPO physician reimbursement policy will increase allowed amounts by 15% for select procedures when done in an ambulatory surgical facility. For a preliminary list of the CPT codes for these procedures, click here. Note: This is in addition to the procedures identified in the May 2020 Record article, with payment policy that was adjusted in July 2020. We’ll continue to closely monitor our list of eligible procedures and adjust it based on provider input and other factors, including the effectiveness of the policy. Any other procedures not listed will be paid at the published rate.
Starting March 1, changes coming to site-of-care requirements for Blue Cross commercial and BCN commercial pediatric membersBeginning March 1, 2021, site-of-care exemptions will no longer apply to pediatric Blue Cross Blue Shield of Michigan commercial members and pediatric Blue Care Network commercial members for some drugs covered under the medical benefit. This means all drugs that have site-of-care requirements for adult commercial members will have the same site-of-care requirements for pediatric commercial members. For these drugs:
Notes
Definition of pediatric members Pediatric members are defined as one of the following:
More about the authorization requirements
How to submit authorization requests Submit authorization requests through the NovoLogix® online tool. It offers real-time status checks and immediate approvals for certain medications. To learn how to submit requests through NovoLogix, go to ereferrals.bcbsm.com and do the following:
Lists of requirements
Update: Oncology management program for Blue Cross fully insured commercial members doesn’t include codes S0353, S0354We wrote in the September edition of The Record that Blue Cross Blue Shield of Michigan expanded its medical oncology management program to include all fully insured commercial members starting Dec. 1, 2020. The program is administered by AIM Specialty Health®. However, because of an update to the program, providers can’t bill or receive the enhanced reimbursement for codes S0353 or S0354 for Blue Cross commercial fully insured members. This change doesn’t apply to Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members or to UAW Retiree Medical Benefits Trust non-Medicare members. For those members, providers can bill and be reimbursed for codes S0353 and S0354. The Oncology management program: Frequently asked questions for providers document has been updated to reflect this change. Look in the section titled “About enhanced reimbursement.” Find the FAQ at ereferrals.bcbsm.com on the Blue Cross AIM-Managed Procedures page.
Authorization for IOP treatment no longer required for State of Michigan enrollees starting in JanuaryProviders will no longer need to obtain authorization for intensive outpatient services from New Directions Behavioral Health for State of Michigan enrollees (group number 007000562), starting Jan. 1, 2021. Previously, the State of Michigan was one of the few groups that required authorization for IOP services. Authorization will continue to be required for all higher level of behavioral health care admissions for which State of Michigan enrollees have a benefit, including acute inpatient psychiatric, substance use disorder acute detox and residential care, psychiatric and SUD partial hospitalization, and outpatient applied behavioral analysis treatment for autism. Providers and office staff can log in to WebPass** to request prior authorizations for State of Michigan members. Providers who’ve never utilized WebPass before can visit the website** to review a training tutorial on how WebPass works. Reminder
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Reminder: Providers must submit authorization requests to TurningPoint for musculoskeletal procedures for most membersAs we reported in the November issue of The Record and the November-December issue of BCN Provider News (Page 46), TurningPoint Healthcare Solutions LLC has expanded its surgical quality and safety management program for dates of service on or after Jan. 1, 2021. You now need to submit authorization requests for orthopedic, pain management and spinal procedures to TurningPoint for the following groups and members:
Some important reminders
Webinar training Professional provider training includes information about TurningPoint’s clinical model, operational changes and provider portal.
Facility training includes information about TurningPoint’s clinical model and operational changes and the facility verification process.
Portal training includes information about using the TurningPoint provider portal.
Where to find more information To view the lists of codes for which TurningPoint manages authorizations, see Musculoskeletal procedure codes that require authorization by TurningPoint. For detailed information, see Musculoskeletal procedure authorizations: Frequently asked questions for providers.
Medical specialty drug prior authorization list will change in January for Blue Cross commercial fully insured groupsFor dates of service on or after Jan. 18, 2021, we’re adding prior authorization requirements for the following specialty drugs covered under the medical benefit for Blue Cross Blue Shield of Michigan commercial fully insured groups, with the exception of the Michigan Education Special Services Association and the Blue Cross and Blue Shield Federal Employee Program®:
Providers must request prior authorization for these drugs through AIM Specialty Health®. How to submit authorization requests Submit authorization requests to AIM using one of the following methods:
For information about registering for and accessing the AIM ProviderPortal℠, see the Frequently asked questions page** on the AIM website. Authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. For additional information on requirements related to drugs covered under the medical benefit, see the Blue Cross and BCN utilization management medical drug list and the Medical oncology prior authorization list. We’ll update these lists to reflect these changes prior to the effective dates. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Expansion of drug waste avoidance program starts March 1To minimize drug waste, reduce unnecessary drug exposure and decrease the risk of adverse events, we’re expanding our waste avoidance program to include additional drugs, effective March 1, 2021. This change affects Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members who receive these drugs:
When this change takes effect, dosing for these therapies will be based on weight and will be specific to:
This change will apply to members who start therapy and members whose authorizations are renewed on or after March 1. Members whose current authorizations for these drugs extend past March 1, 2021, can continue at their current dose until their authorization expires. Members not affected by this change This change doesn’t apply to:
Lists of requirements To view the requirements for these drugs, see the following drug lists:
We’ll update these drug lists with this information about the change in dosing strategy before March 1. **In addition to Blue Cross commercial and BCN commercial members, the dosing strategy change for this drug applies to UAW Retiree Medical Benefits Trust non-Medicare members.
Sign up for additional training webinarsProvider Experience is continuing its series of training webinars for health care providers and staff. The webinars are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network. Here’s information on the upcoming training webinars:
The Blue Cross 201 webinar series provides an in-depth learning opportunity and builds on information shared in our Blue Cross 101: Understanding the Basics webinar. This new webinar reviews the processes and tools available when submitting claims. The Autism Overview webinar reviews current processes related to providing services to members with autism. Recordings of previous webinars are available on web-DENIS via the Blue Cross Provider Publications and Resources or BCN Provider Publications and Resources pages as follows. Blue Cross Provider Publications and Resources
You can also get more information about online training, presentations and videos by clicking on the E‑Learning icon at the top of the page. BCN Provider Publications and Resources
As additional training webinars become available, we’ll provide notices through
Here are billing guidelines for home health care servicesBlue Cross Blue Shield of Michigan requires home health care services to be billed using the number of visits (rather than hours or incremental hours) as a unit of service. Visits should be reported individually on separate lines to correctly reflect if multiple visits were performed on the same date of service. Note: Some services, such as therapy services (revenue codes 0421, 0431 and 0441), are only payable once per day. Only the required and appropriate number of visits should be billed for reimbursement for home health care services. Private duty nursing shouldn’t be billed as a home health care visit. For accurate processing and reimbursement, it should be billed according to billing guidelines for private duty nursing. Additional guidelines for reference:
Claims not billed according to these guidelines will be denied or reimbursed at the rate for one visit. None of the information included herein is intended to be legal advice and as such it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Blue Cross implements post-pay audits related to inpatient readmissionsIn 2019, Blue Cross Blue Shield of Michigan implemented post-pay audits related to inpatient readmissions for all Medicare Plus Blue℠ members. Blue Cross contracted with HMS® to conduct audits for readmissions to the same facility occurring up to 30 days from the date the patient was released from the hospital if the readmission is related to the prior medical condition. This applies to both contracted and non-contracted hospitals that are reimbursed at a diagnosis-related group case rate. Hospitals can no longer rebill Medicare Part B services from the denied admission. HMS’ initial letter will contain findings that medical conditions causing the readmission appear to be related to the prior medical condition. If the hospitals disagree with HMS’ decision, hospitals can submit a reconsideration request and submit medical records on appeal for all listed claims on the HMS letter (including the reference claim). If no medical records are submitted, we will recoup payment on the readmitted claim on the HMS letter. How to request a reconsideration review:
Hospitals are responsible for all costs pertaining to readmissions denied under the Medicare Plus Blue Readmissions Reimbursement Policy. They aren’t allowed to charge or balance bill Medicare Plus Blue members for the denied stay. The following are exclusions to this policy:
Questions? If you need to speak to an HMS representative during an audit, call 1-866-875-1749 from 9 a.m. to 7:30 p.m. Eastern time Monday through Friday.
We’re expanding access to diabetes monitoring products for commercial members, starting in JanuaryStarting Jan. 1, 2021, diabetes monitoring products, such as glucometers and test strips, lancets, continuous glucose monitors and insulin delivery devices, will be added to the pharmacy benefit for Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members. Members will be able to obtain diabetes monitoring products or supplies through participating pharmacies or through durable medical equipment providers, as outlined below. Participating pharmacies Select glucometers and continuous glucose monitors will be available through members’ pharmacy benefit with no cost sharing. Other diabetes supplies will be covered according to the drug list for the member’s plan. The appropriate pharmacy cost sharing or copayment will apply. Glucometers and continuous glucose monitoring products that are available with no cost sharing include:
Durable medical equipment providers Members can also obtain diabetes monitoring products through a DME provider. The process to locate DME providers varies depending on a member’s plan:
A Northwood icon appears next to each Northwood network provider.
What this change means This change effects members as follows:
Starting March 1, changes coming to site-of-care requirements for Blue Cross commercial and BCN commercial pediatric membersBeginning March 1, 2021, site-of-care exemptions will no longer apply to pediatric Blue Cross Blue Shield of Michigan commercial members and pediatric Blue Care Network commercial members for some drugs covered under the medical benefit. This means all drugs that have site-of-care requirements for adult commercial members will have the same site-of-care requirements for pediatric commercial members. For these drugs:
Notes
Definition of pediatric members Pediatric members are defined as one of the following:
More about the authorization requirements
How to submit authorization requests Submit authorization requests through the NovoLogix® online tool. It offers real-time status checks and immediate approvals for certain medications. To learn how to submit requests through NovoLogix, go to ereferrals.bcbsm.com and do the following:
Lists of requirements
Update: Oncology management program for Blue Cross fully insured commercial members doesn’t include codes S0353, S0354We wrote in the September edition of The Record that Blue Cross Blue Shield of Michigan expanded its medical oncology management program to include all fully insured commercial members starting Dec. 1, 2020. The program is administered by AIM Specialty Health®. However, because of an update to the program, providers can’t bill or receive the enhanced reimbursement for codes S0353 or S0354 for Blue Cross commercial fully insured members. This change doesn’t apply to Medicare Plus Blue℠, Blue Care Network commercial and BCN Advantage℠ members or to UAW Retiree Medical Benefits Trust non-Medicare members. For those members, providers can bill and be reimbursed for codes S0353 and S0354. The Oncology management program: Frequently asked questions for providers document has been updated to reflect this change. Look in the section titled “About enhanced reimbursement.” Find the FAQ at ereferrals.bcbsm.com on the Blue Cross AIM-Managed Procedures page.
Medical specialty drug prior authorization list will change in January for Blue Cross commercial fully insured groupsFor dates of service on or after Jan. 18, 2021, we’re adding prior authorization requirements for the following specialty drugs covered under the medical benefit for Blue Cross Blue Shield of Michigan commercial fully insured groups, with the exception of the Michigan Education Special Services Association and the Blue Cross and Blue Shield Federal Employee Program®:
Providers must request prior authorization for these drugs through AIM Specialty Health®. How to submit authorization requests Submit authorization requests to AIM using one of the following methods:
For information about registering for and accessing the AIM ProviderPortal℠, see the Frequently asked questions page** on the AIM website. Authorization isn’t a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members. For additional information on requirements related to drugs covered under the medical benefit, see the Blue Cross and BCN utilization management medical drug list and the Medical oncology prior authorization list. We’ll update these lists to reflect these changes prior to the effective dates. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Changes coming Jan. 1 for preferred, clinical, custom and custom select drug listsWe recently published an article that detailed changes to the Preferred Drug List, starting Jan. 1, 2021. We’re making an update to the exclusion information: Cimzia® and Kevzara® will remain on the Preferred Drug List. These drugs won’t be excluded. 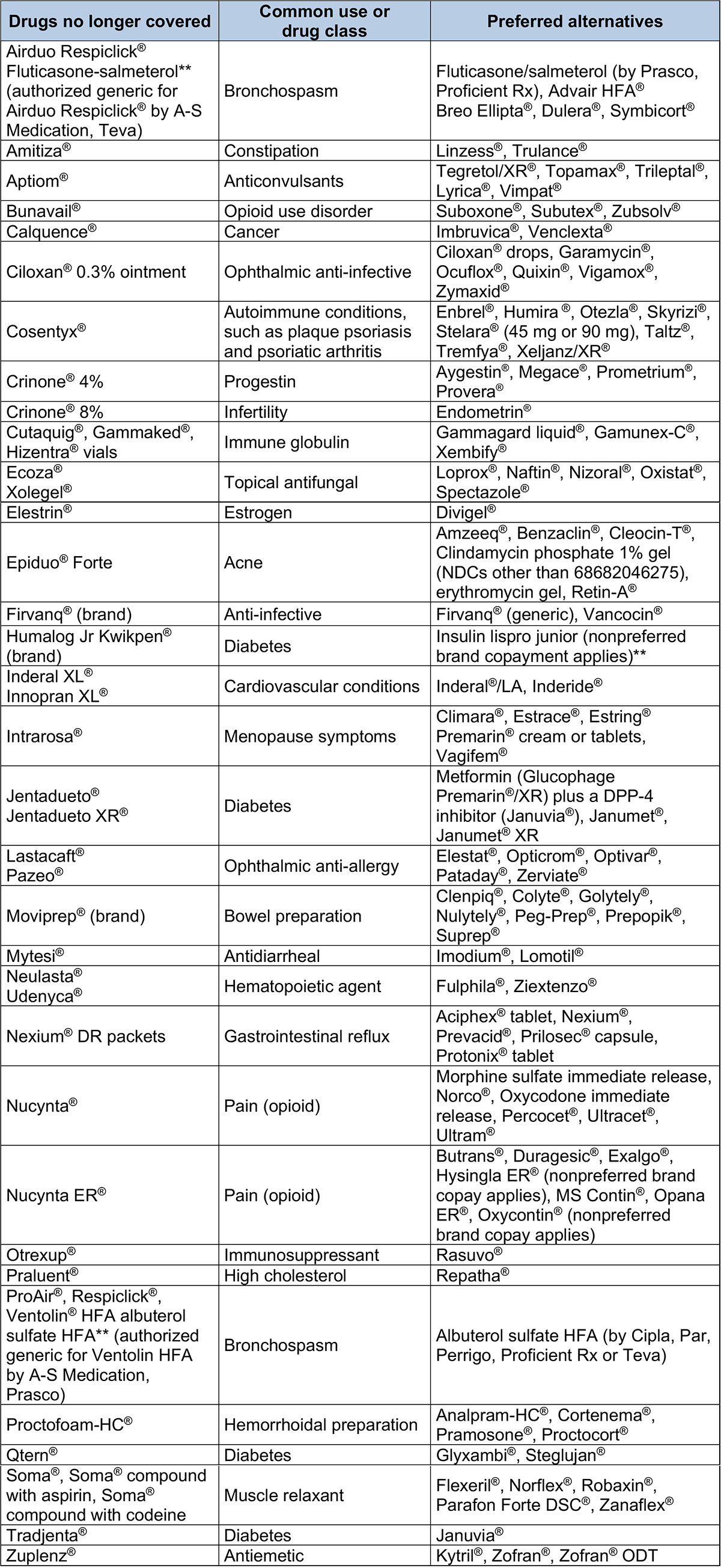 Drugs with a higher copayment – Preferred Drug List 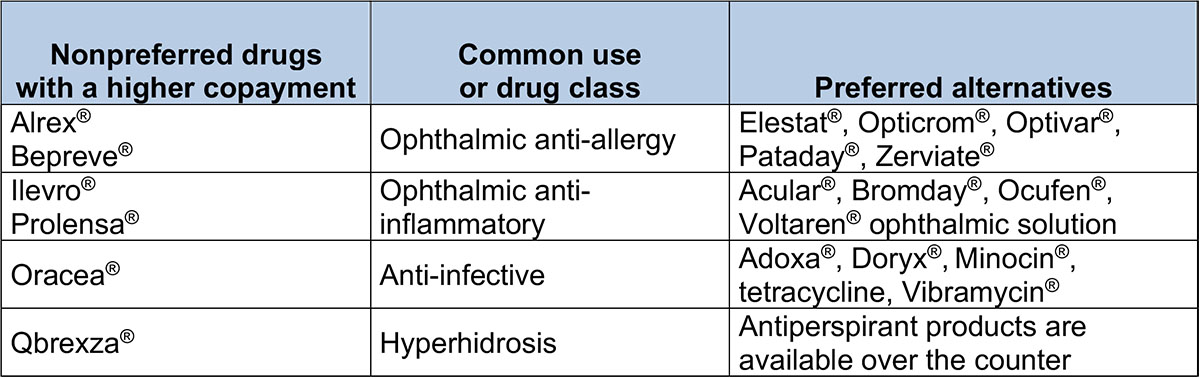 Drugs with quantity limits – Preferred Drug List 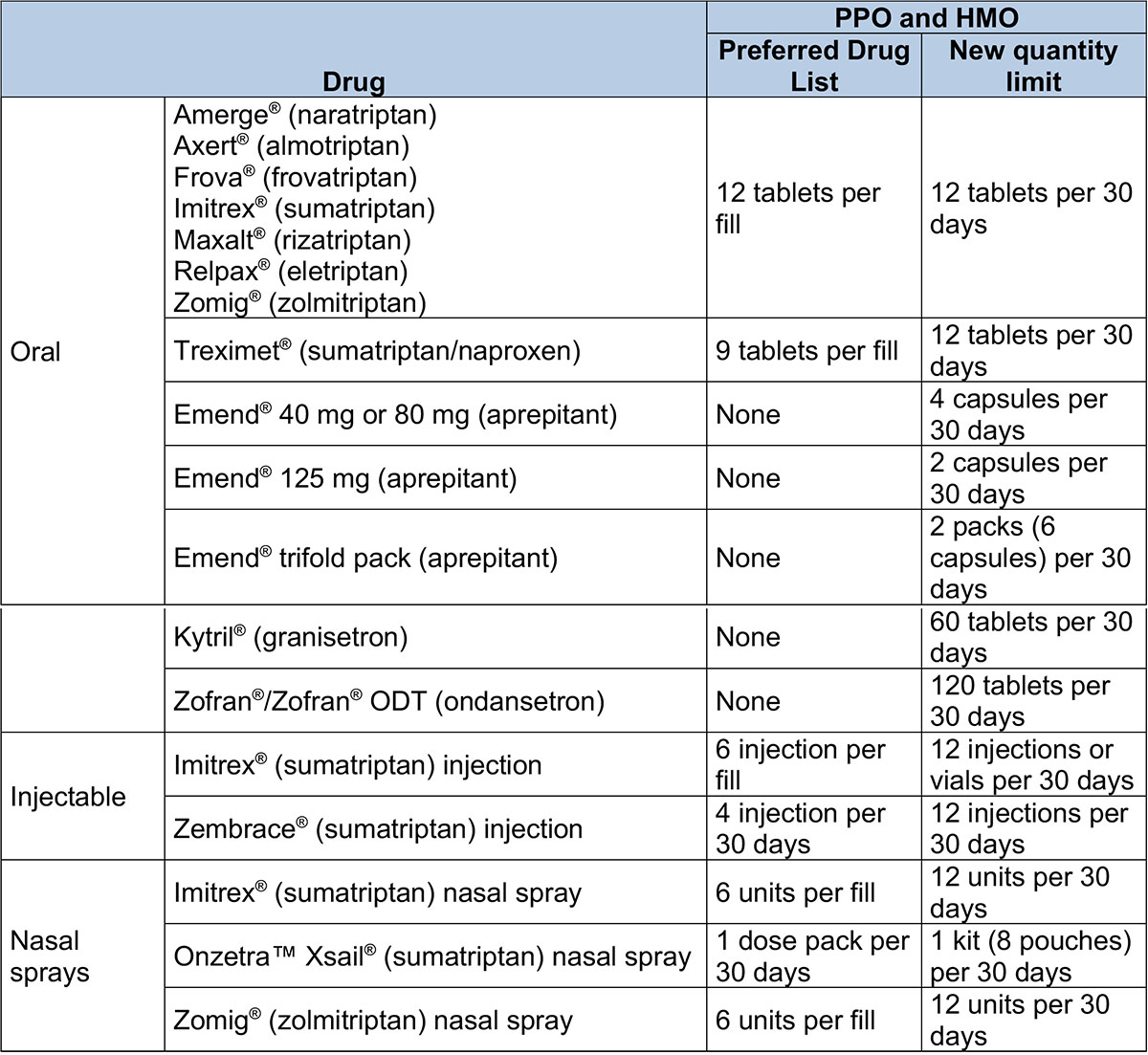 Clinical, Custom and Custom Select Drug List changes Drugs no longer covered – Clinical and Custom Drug lists 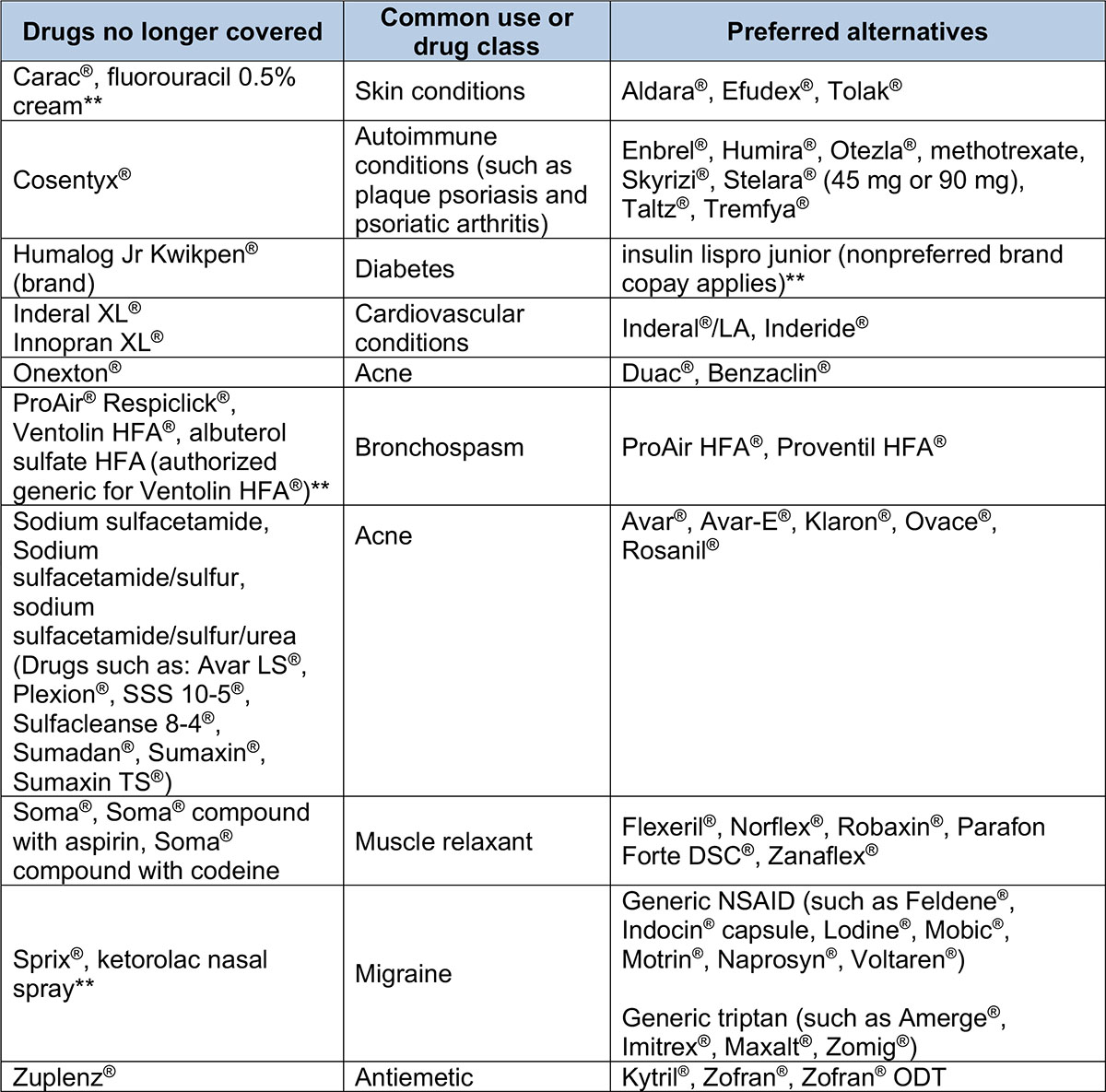 Drugs with a higher copayment – Custom Drug List 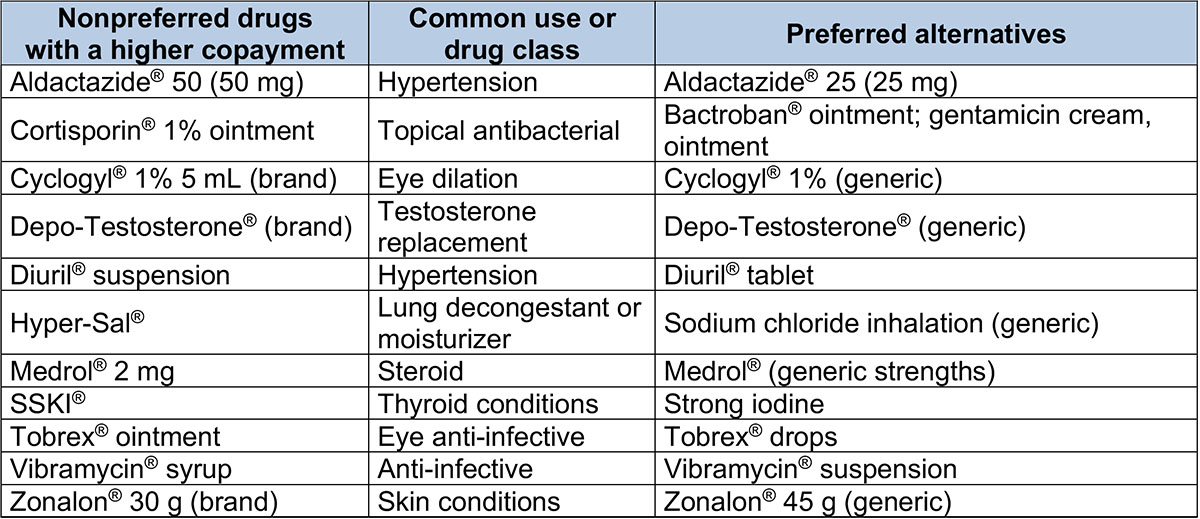 Drugs no longer covered – Custom Select Drug List 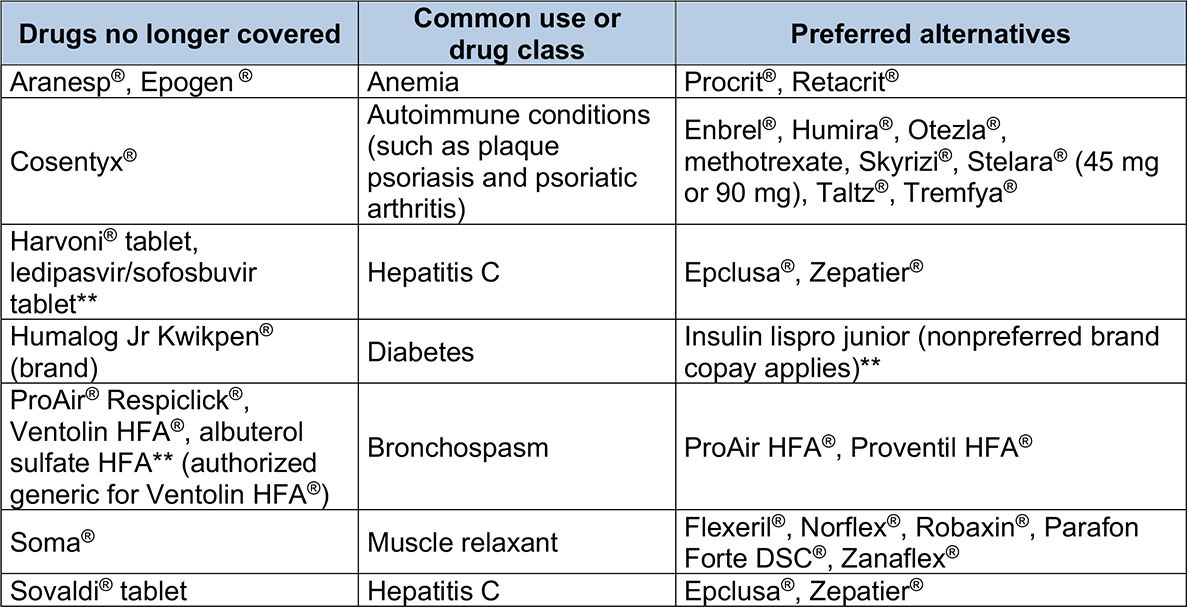 Drugs with quantity limits – Clinical, Custom and Custom Select Drug lists 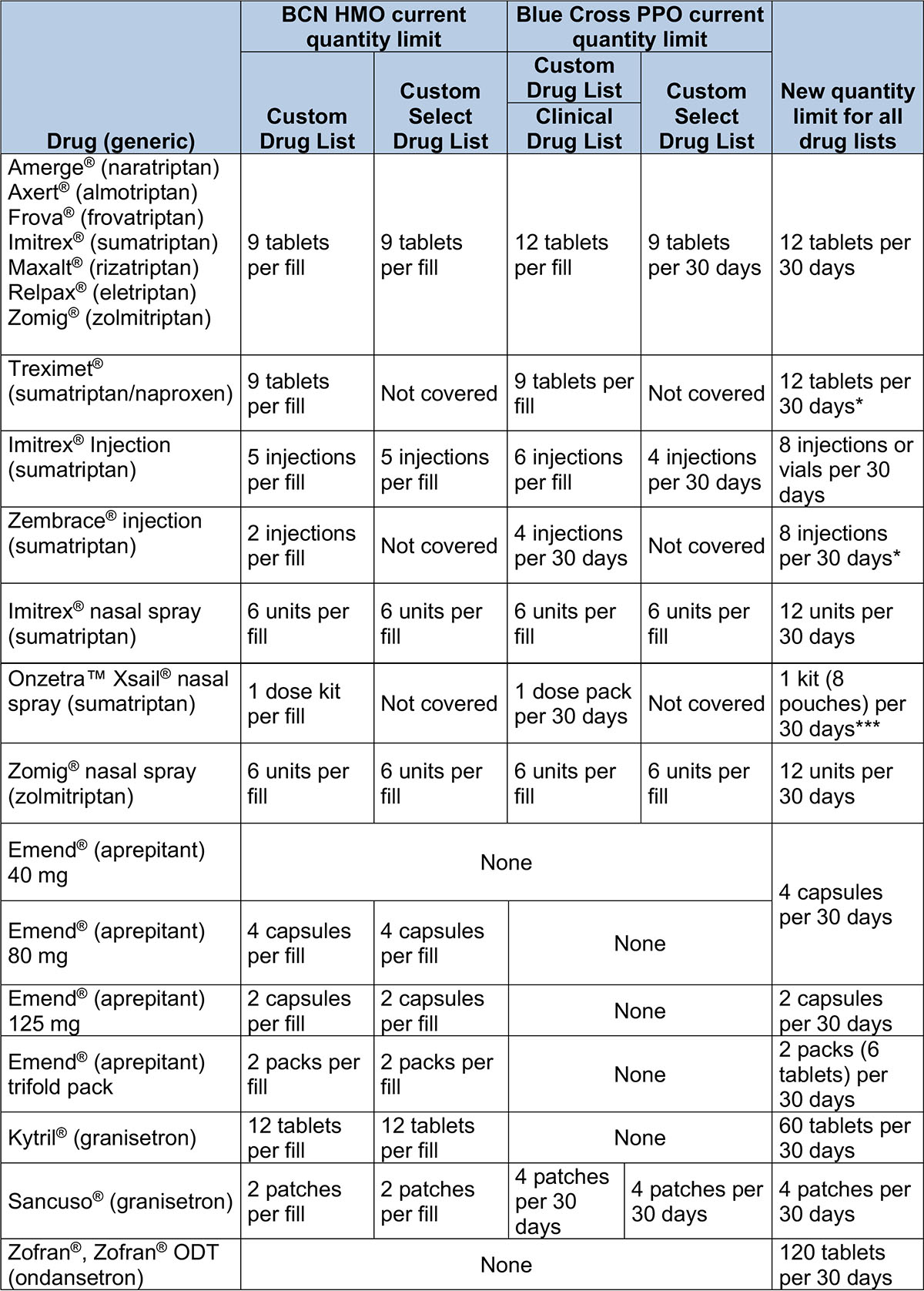 **Represents drugs that have brand names without generic equivalents. These may be considered “authorized generics,” which are the same as brand-name drugs but aren’t true generic drugs. ***Doesn’t apply to members whose plans use the Custom Select Drug List.
Manufacturer discontinues Zostavax shingles vaccinePharmaceutical company Merck announced it has discontinued the Zostavax® vaccine, a vaccine for the prevention of shingles in adults age 60 and older. All remaining product had an expiration date of November 2020, and Zostavax is no longer available for use in the United States. On Dec. 1, 2020, Blue Cross Blue Shield of Michigan and Blue Care Network commercial pharmacy stopped covering the Zostavax vaccine. Pharmacy claims for Zostavax will reject at the point of sale as of Dec. 1, 2020. Blue Cross and BCN will continue to offer the Shingrix® shingles prevention vaccine for adults age 50 and older.
Expansion of drug waste avoidance program starts March 1To minimize drug waste, reduce unnecessary drug exposure and decrease the risk of adverse events, we’re expanding our waste avoidance program to include additional drugs, effective March 1, 2021. This change affects Blue Cross Blue Shield of Michigan commercial and Blue Care Network commercial members who receive these drugs:
When this change takes effect, dosing for these therapies will be based on weight and will be specific to:
This change will apply to members who start therapy and members whose authorizations are renewed on or after March 1. Members whose current authorizations for these drugs extend past March 1, 2021, can continue at their current dose until their authorization expires. Members not affected by this change This change doesn’t apply to:
Lists of requirements To view the requirements for these drugs, see the following drug lists:
We’ll update these drug lists with this information about the change in dosing strategy before March 1. **In addition to Blue Cross commercial and BCN commercial members, the dosing strategy change for this drug applies to UAW Retiree Medical Benefits Trust non-Medicare members.
Starting Jan. 1, Northwood is Blue Cross’ DME/POS program benefits managerStarting Jan. 1, 2021, Northwood Inc. will administer and manage all aspects of durable medical equipment, prosthetics, orthotics and medical supply benefits for Blue Cross Blue Shield of Michigan commercial fully insured and individual members who reside in the state of Michigan. Only members in groups enrolled in the program are required to participate. Blue Care Network, BCN Advantage℠, and Medicare Plus Blue℠ are already part of the tailored network arrangement with Northwood. Northwood will administer:
DME/POS program categories and examples of services include: Standard equipment
Labor-intensive equipment
Body supports and limbs
Medical or surgical supplies
Prior authorization
Participation
If you have additional questions about the DME/POS management program, contact Northwood Provider Relations at 1-800-447-9599 between 8:30 a.m. and 5 p.m. Eastern time Monday through Friday. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Blue Cross Blue Shield of Michigan and Blue Care Network will move to the Availity® Provider Portal later in 2021. If you’re already an Availity user, you don’t need to do anything to access Blue Cross and BCN information once it’s available. If you’re not currently using Availity, here’s some information to help you prepare for the transition.
Blue Cross Blue Shield of Michigan and Blue Care Network will move to the Availity® Provider Portal later in 2021. If you’re already an Availity user, you don’t need to do anything to access Blue Cross and BCN information once it’s available. If you’re not currently using Availity, here’s some information to help you prepare for the transition. In August 2018, Blue Cross Blue Shield of Michigan announced an initiative for select surgeries aimed at promoting effective pain control through care processes that limit opioid dispensing. In 2021, modifications will be made to the eligible surgical groupings by adding some groupings, extending some and retiring others.
In August 2018, Blue Cross Blue Shield of Michigan announced an initiative for select surgeries aimed at promoting effective pain control through care processes that limit opioid dispensing. In 2021, modifications will be made to the eligible surgical groupings by adding some groupings, extending some and retiring others.