Subscribe | The Record Archive | Contacts | bcbsm.com
|
May 2025
Dr. Beecroft: Presenting a synopsis of the current thinking around autism etiology and treatmentThe science behind an autism diagnosis and its treatment is changing very rapidly, which is a good thing for our members, according to Dr. William Beecroft, medical director of behavioral health at Blue Cross Blue Shield of Michigan. Based on collateral research on precision psychiatry and neuroscience, this column explores the current, predominant hypothesis of the etiology of autism. We’ve known for many years that neonates, when born, have an overabundance of neurons and neural junctions in the brain — the most that they will ever have in their lives. Autistic children have even more, although the reason is currently unknown. We also know that the major neural pathways that link parts of the brain start out with a variable density of these neurons and junctions. When mapped to areas of the brain that mitigate and drive the symptoms of autism we see, they directly relate to those symptoms. For example, the pathway to the Fusiform Gyrus (occipital lobe), which is related to facial recognition, is hypoactive in some autistic individuals, contributing to social difficulties interacting with others, especially strangers. Other connections and pathways such as the pathway to the temporal parietal lobe (which is linked to social cognition) is dysfunctional with many individuals as well as the path to the orbital frontal cortex, which has a role in social behavioral as well. Having poor function in these areas at the same time then drives the social difficulties many individuals exhibit. These pathways may have either too many or not enough neurons and neural connections. If the pathway has too many, the behaviors mitigated by that pathway are accentuated. Those with not enough are deficit in the behaviors controlled by those areas of the brain. I have only provided three pathways involved in common behavioral symptomology, but there are other pathways involved as well. The observed behaviors and symptoms are a combination of the variable factors in multiple pathways and modify each other due to feedback loops in the brain. The way the brain works then is to naturally “prune” the excess neurons in pathways where there is too much activity and not change or modestly “grow” additional neurons and junctions in pathways that do not have enough activity. This process is referred to as the brain being “plastic” and having over time the ability to strengthen weak pathways and slow down ones that are too active. This “plasticity” is more pronounced in younger children and decreases over the lifespan. This is where Applied Behavior Analysis, known as ABA, comes in. As a combination of learning theory and behavior modification, ABA works by increasing the strength of the pathways, which will then improve (as much as possible) the behavior that are a deficit for the individual. The other pathways that are too active can be slowed by not giving positive reinforcement for the negative behaviors that are desired to be “extinguished” or “mitigated.” Both processes are a natural occurrence of pruning of the excess neurons and not decreasing or slightly increasing the neurons in the hypoactive pathways. This is like habit modification and learning in general. You practice things you want to remember, which results in having faster recall. Those things you want to forget or habits you want to lose aren’t rewarded. It takes much longer to extinguish a habit or behavior than learn a new one. The key to successful change, though, is consistent and repetitive reward for positive change and no reward for negative attributes. This is where working in a team with clear communication of even minute changes is important for all people who interact with the individual. Once the behaviors have been brought to their best ability, there needs to be a period of trial and error with less frequent rewards to capitalize on the gains made to the process outlined above. This combination of the science behind the process and improving the consistency in the process offers significant hope for improvement in function to the best of that individual’s capacity. References:
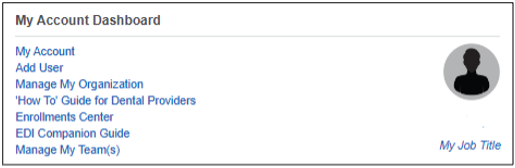
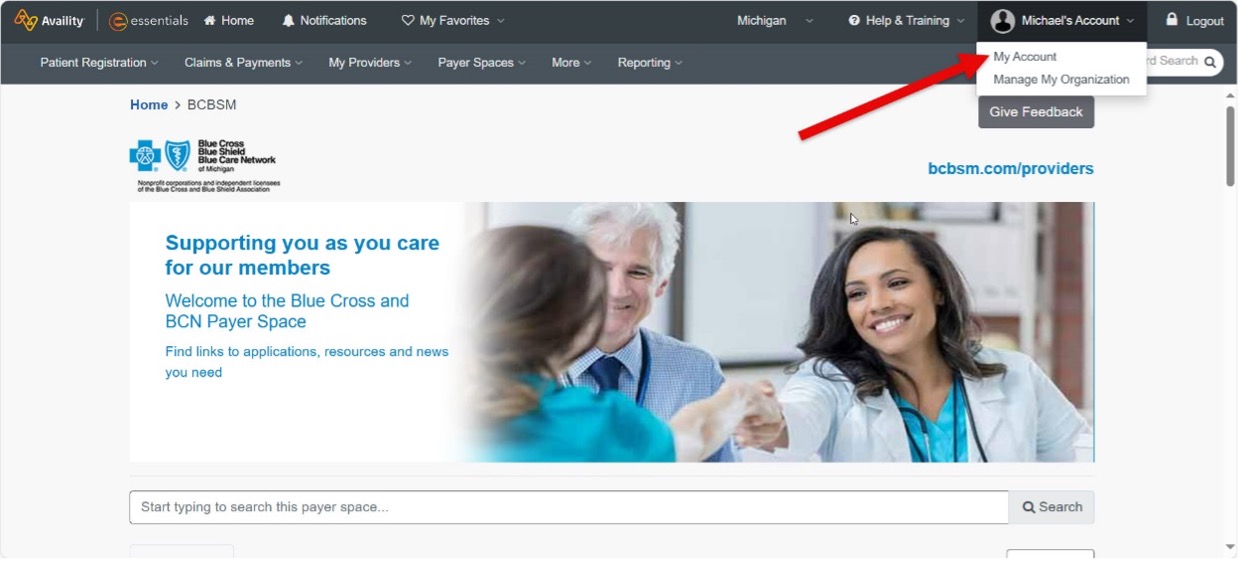
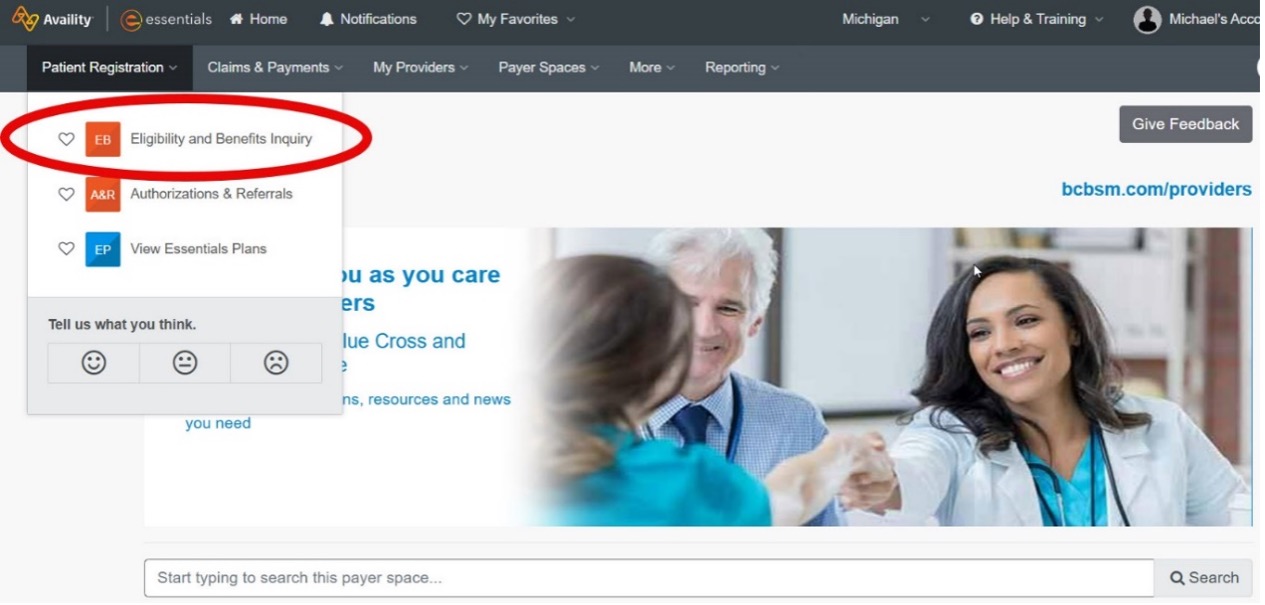
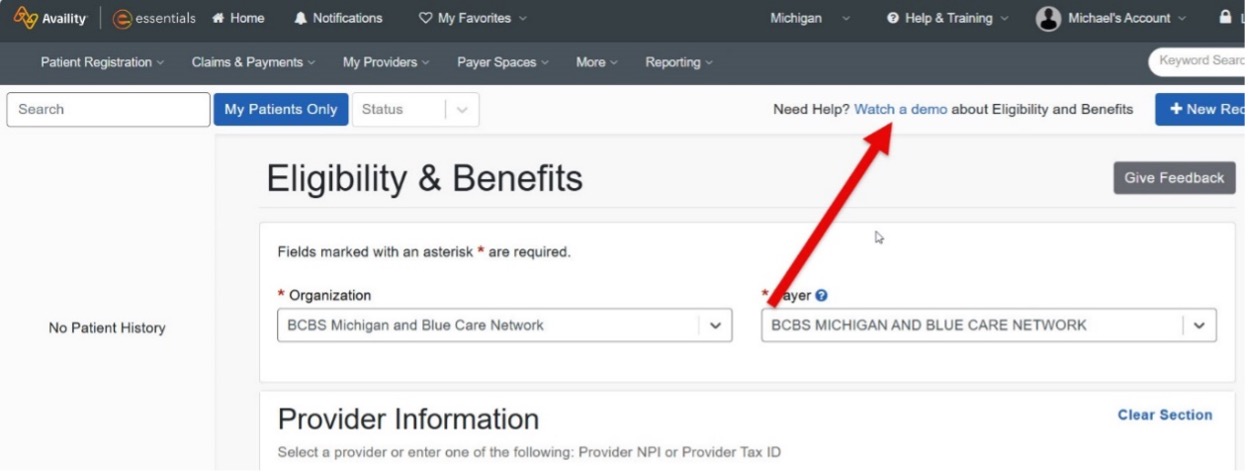
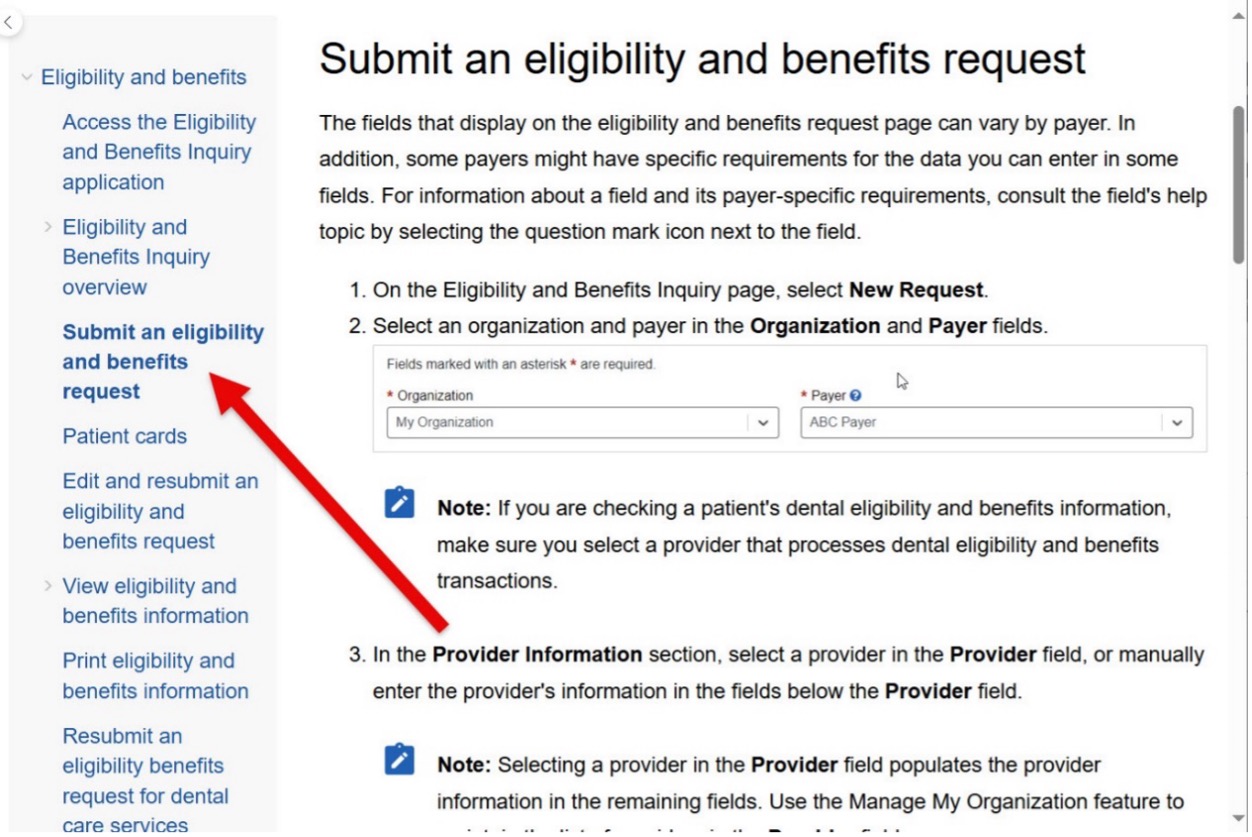
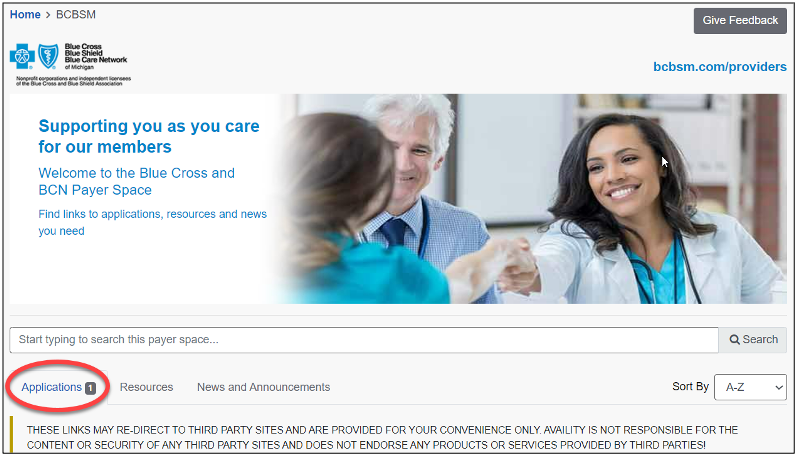
Provider portal pointers: Submitting an eligibility and benefits requestThis is a new ongoing series of tips and tricks designed to help you do your job more efficiently by getting the most out of the applications and tools available on our provider portal. Using our provider portal, availity.com,** to determine patient eligibility and benefits helps you more quickly get the information you need to service your patients. However, if you’re new to our provider portal, or only need to access patient benefits and eligibility infrequently, you may have questions.The Eligibility & Benefits page has two useful tools to help you complete your request: Watch a demo and Find Help. To get to them, let’s first look at the My Account Dashboard. The My Account Dashboard lets users:
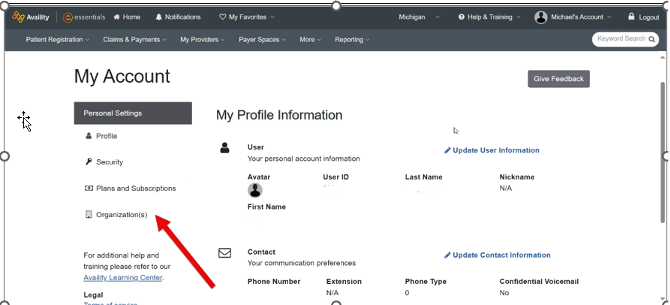
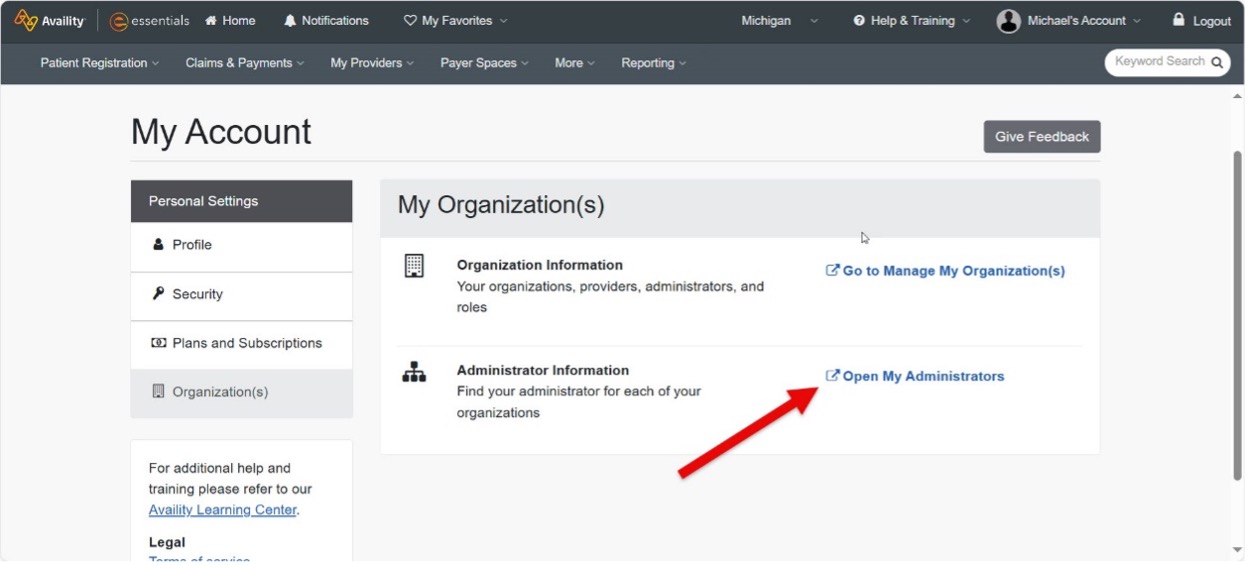
How to gain access to Eligibility & Benefits Your organization administrator must grant you access to the Eligibility and Benefits role under Manage My Team(s). To locate your administrator, hover over Manage My Team(s) and then click on I need access. This will display who controls your access. Or do the following:
How to get to the Eligibility & Benefits page
Lines of business include Blue Cross Blue Shield of Michigan (PPO) and Blue Care Network (HMO) commercial, BCN Advantage℠ and Medicare Plus Blue℠ (Medicare Advantage), Flexlink, out of state Blue Cross Blue Shield of Michigan plans and Blue Cross and Blue Shield Federal Employee Program® (FEP) contracts.
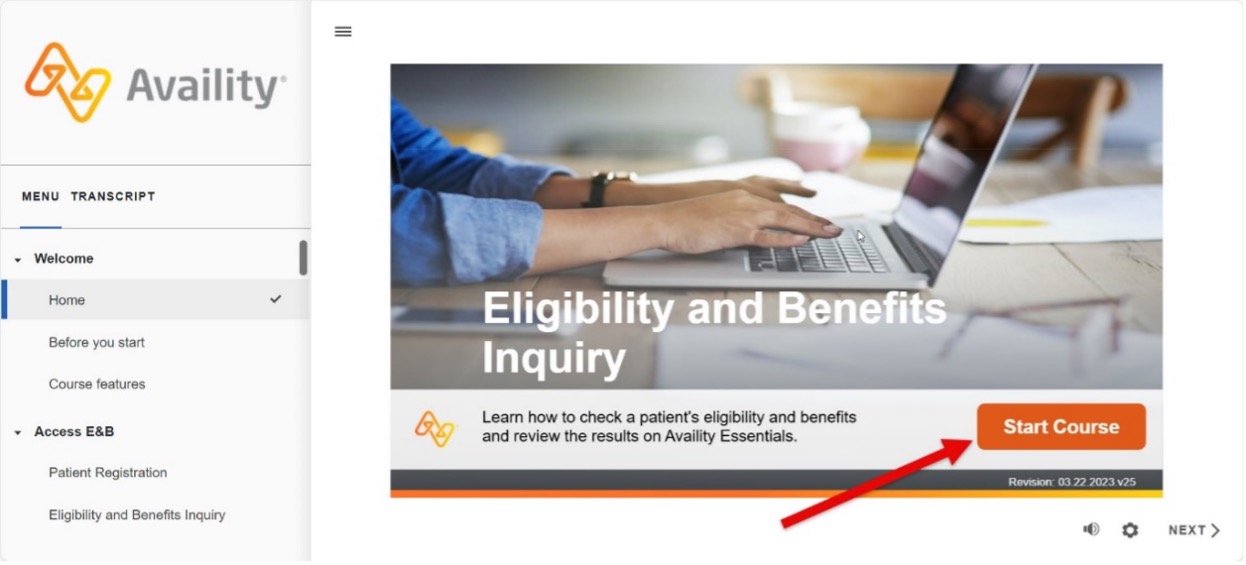
On the Eligibility & Benefits page you can choose to either watch a training video or access detailed step-by-step instructions on how to submit a request. How to view the training video
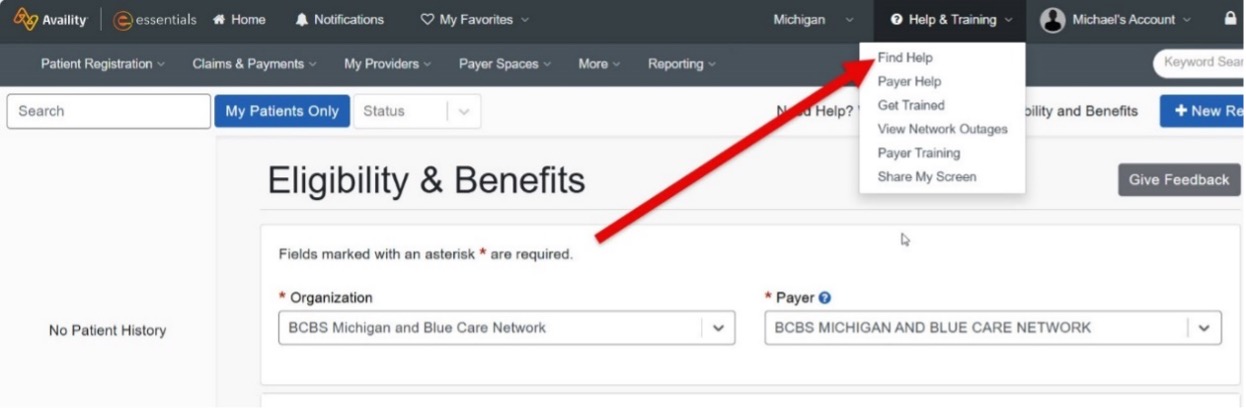
How to view detailed step-by-step instructions
Eligibility and benefits request tips and tricks Be sure to look for more provider portal pointers in future issues of this newsletter. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Billing chart: Blue Cross highlights medical, benefit policy changesYou’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the “Billing chart.” The billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures. We’ll publish information about new Blue Cross groups or changes to group benefits under the Group Benefit Changes heading. For more detailed descriptions of Blue Cross’ policies for these procedures, check under the Commercial Policy tab in Benefit Explainer on Availity Essentials™. To access this online information: To view the “May 2025 Billing chart,” click here. **Blue Cross Blue Shield of Michigan doesn’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Behavioral health providers shouldn’t submit claims for behavioral health collaborative care servicesAs a reminder, behavioral health providers shouldn’t bill Blue Cross Blue Shield of Michigan or Blue Care Network for collaborative care services performed in a primary care or specialty setting. These services are associated with: Claims submitted by behavioral health providers for these services will deny. These codes aren’t payable for behavioral health providers. Collaborative care services are covered under the member’s medical benefits and must be billed by the member’s treating medical provider.
HCPCS replacement codes established, effective April 1, 2025J9038 replaces C9399, J3490, J3590, J9999 when billing for Niktimvo™ (axatilimab-csfr) Effective April 1, 2025, the Centers for Medicare & Medicaid Services, or CMS, has established a new procedure code for the specialty medical drug Niktimvo (axatilimab-csfr). All services through March 31, 2025, will continue to be reported with codes C9399, J3490, J3590 and J9999. All services performed on and after April 1, 2025, must be reported with J9038. Prior authorization is required through the medical benefit drug program for J9038 for all groups unless they are opted out of this program. Reference the Prior Authorization Opt-In/Out Group list on availity.com.** For groups that have opted out of the prior authorization program, this code is covered for its FDA-approved indications. Q5147 replaces C9399, J3490, J3590, J9999 when billing for PAVBLU™ (aflibercept-ayyh) Effective April 1, 2025, CMS has established a new procedure code for the specialty medical drug PAVBLU (aflibercept-ayyh). All services through March 31, 2025, will continue to be reported with codes C9399, J3490, J3590 and J9999. All services performed on and after April 1, 2025, must be reported with Q5147. Prior authorization is required through the medical benefit drug program for Q5147 for all groups unless they are opted out of this program. Reference the Prior Authorization Opt-In/Out Group list on availity.com.** For groups that have opted out of the prior authorization program, this code is covered for its FDA-approved indications. Q5148 replaces C9399, J3490, J3590, J9999 when billing for Nypozi® (filgrastim-txid) Effective April 1, 2025, CMS has established a new procedure code for the specialty medical drug Nypozi (filgrastim-txid). All services through March 31, 2025, will continue to be reported with codes C9399, J3490, J3590 and J9999. All services performed on and after April 1, 2025, must be reported with Q5148. Prior authorization is required through the medical benefit drug program for Q5148 for all groups unless they are opted out of this program. Reference the Prior Authorization Opt-In/Out Group list on availity.com.** For groups that have opted out of the prior authorization program, this code is covered for its FDA-approved indications. Q5149 replaces C9399, J3490, J3590, J9999 when billing for Enzeevu™ (aflibercept-abzv) Effective April 1, 2025, CMS has established a new procedure code for the specialty medical drug Enzeevu (aflibercept-abzv). All services through March 31, 2025, will continue to be reported with codes C9399, J3490, J3590 and J9999. All services performed on and after April 1, 2025, must be reported with Q5149. Prior authorization is required through the medical benefit drug program for Q5149 for all groups unless they are opted out of this program. Reference the Prior Authorization Opt-In/Out Group list on availity.com.** For groups that have opted out of the prior authorization program, this code is covered for its FDA-approved indications. Q5152 replaces C9399, J3490, J3590, J9999 when billing for Bkemv™ (eculizumab-aeeb) Effective April 1, 2025, CMS has established a new procedure code for the specialty medical drug Bkemv (eculizumab-aeeb). All services through March 31, 2025, will continue to be reported with codes C9399, J3490, J3590 and J9999. All services performed on and after April 1, 2025, must be reported with Q5152. Prior authorization is required through the medical benefit drug program for Q5152 for all groups unless they are opted out of this program. Reference the Prior Authorization Opt-In/Out Group list on availity.com.** For groups that have opted out of the prior authorization program, this code is covered for its FDA-approved indications. Q9999 replaces C9399, J3490, J3590, J9999 when billing for Otulfi™ (ustekinumab-aauz) Effective April 1, 2025, CMS has established a new procedure code for the specialty medical drug Otulfi (ustekinumab-aauz). All services through March 31, 2025, will continue to be reported with codes C9399, J3490, J3590 and J9999. All services performed on and after April 1, 2025, must be reported with Q9999. Prior authorization is required through the medical benefit drug program for Q9999 for all groups unless they are opted out of this program. Reference the Prior Authorization Opt-In/Out Group at availity.com.** For groups that have opted out of the prior authorization program, this code is covered for its FDA-approved indications. **Blue Cross Blue Shield of Michigan doesn’t own or control this website. Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
2025 HCPCS 1st-quarter update: New, deleted codesThe Centers for Medicare & Medicaid Services has added several new codes as part of its quarterly Healthcare Common Procedure Coding System updates. The codes, effective dates and Blue Cross Blue Shield of Michigan’s coverage decisions are below. Outpatient prospective payment system, or OPPS/radiology
OPPS/surgery
Surgery/skin substitute
Medical/surgical supplies
Medical and surgical supplies/radiopharmaceuticals
Durable medical equipment
Temporary national codes (non-Medicare)/durable medical equipment
Prosthetic procedures
Orthotic procedures
Injections/chemotherapy
Injections
Procedures/professional services (temporary)/pathology and laboratory
Procedures/professional services (temporary)/radiology
Procedures/professional services (temporary)/surgery
Radiology procedures
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Reminder: How to check the status of prior authorization requests to share with your patientsIf a patient who has coverage through Blue Cross Blue Shield of Michigan or Blue Care Network asks about the status of a prior authorization request, you can check it for them by following these steps:
Additional information available for providers Providers can also find a summary of services that require prior authorization through our Summary of utilization management programs for Michigan providers document on ereferrals.bcbsm.com. Note: For help using the e-referral tool, go to ereferrals.bcbsm.com, then under Access & Training, click on Training Tools. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Do you have time for a Quality Minute about patient care?An ongoing series of quick tips designed to be read in 60 seconds or less and provide your practice with information about performance in key areas. Establishing patient care Members are required to select a primary care physician when joining health maintenance organization plans. In cases when our BCN commercial and BCN Advantage℠ members don’t select a PCP, we assign them one. If a patient hasn’t established care with their assigned PCP, that patient won’t be visible in Active Care Relationship Service or Admit, Discharge, and Transfer files. This can make managing their care more challenging and can affect the provider’s quality measure performance. What you can do What we’re doing as a health plan We recognize that care coordination is not solely the provider’s responsibility. Internally, we are working with our membership area to identify where members who haven’t visited their PCP are receiving care. Through targeted outreach, we aim to connect these members with their PCPs and support their health care needs.
Here’s an overview of Identification of Microorganisms Using Nucleic Acid Probes policyThe use of nucleic acid testing using either single pathogens or panel testing is established in specified situations for Blue Cross Blue Shield of Michigan and Blue Care Network commercial. It may be considered a useful diagnostic tool when indicated. The updated criteria effective Jan. 1, 2025, is outlined below. Inclusionary and exclusionary guidelines: The status of nucleic acid identification (using either direct probe, amplified probe or quantification) for certain microorganisms are summarized in the table below by CPT code (if applies) and status of the procedure (established or investigational). Note: In the table, EST is an abbreviation for established and INV for investigational. Determination table for microorganism by test, CPT code (if applies) and efficacy
aConsidered established when criteria below are met. Panel testing using nucleic acid probes for central nervous system pathogens are considered established when one of the following criteria is met: Repeat panel testing for the same clinical indication will only be covered when all the following are met: Single nucleic acid probe testing for urinary tract pathogens to diagnose an infection (for example, prostatitis, urinary tract infection) is considered established when all the following are met: Note: Criteria for single nucleic acid probe testing for urinary tract pathogens is established for covered organisms without a specific CPT code and up to 10 units/pathogens in infection diagnoses (for example, prostatitis, UTI) Polymerase chain reaction, or PCR, testing for the following microorganisms that don’t have specific CPT codes are considered established: aImmunocompromised individuals consist of those with weakened immune systems including human immunodeficiency virus or acquired immunodeficiency syndrome, individuals who are taking immunosuppressive medications (such as chemotherapy, biologics, transplant-related immunosuppressive drugs, high-dose systemic corticosteroids) and those with inherited diseases that affect the immune system (such as congenital immunoglobulin deficiencies). Exclusions: None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
We invite you to join PGIP as a physician organizationBlue Cross Blue Shield of Michigan will accept applications for the Physician Group Incentive Program from any physician organizations from May 1 through June 30, 2025. PGIP offers incentives to participating physician organizations for transforming health care delivery and improving the overall value of health care. To request application materials, send an email to valuepartnerships@bcbsm.com, and we’ll send you information on PGIP and PO eligibility requirements. About PGIP PGIP was developed with input from providers across Michigan to help improve the quality and efficiency of health care in the state. PGIP facilitates change through a wide range of initiatives, including our nationally recognized Patient-Centered Medical Home program. Through PGIP, we reward physician organizations for improving health care delivery to their attributed patient population. PGIP-participating physicians are eligible for value-based reimbursement consideration as a result of program efforts. A PGIP physician organization consists of physicians participating in our PPO or Traditional network, working together to: Learn more If you’re an individual practitioner and interested in participating in PGIP, click here to learn more about PGIP physician organizations. For more information on PGIP and its initiatives, visit valuepartnerships.com.
Webinars for physicians, coders focus on documentation, codingAction item Register for our 2025 monthly Lunch & Learn webinars focusing on coding and documentation. In 2025, we’ll continue to offer webinars about documentation and coding of common challenging diagnoses. These live, lunchtime educational sessions will also include an opportunity to ask questions. Below is our schedule and topics for the sessions. All sessions start at noon Eastern time and should last for 30 minutes. Register for the sessions on the provider training website.
If you have an Availity Essentials™ account can access the provider training website this way: Existing users who used the same email address as their provider portal profile email will be directed to the training site. If you used a different email address, contact ProviderTraining@bcbsm.com to update your profile You can also directly access the training website if you don’t have a provider portal account by clicking here. After logging in to the provider training website, look in Event Calendar to sign up for your desired session. You can also quickly search for all the sessions with the keyword “lunchtime” and then look under the results for Events. You can listen to the previously recorded sessions, too. Check out the following:
Questions? **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
On-demand opportunities are available for provider trainingAction item Visit our provider training site to register for a June webinar and find resources on topics that are important to your role. Provider Experience continues to offer training resources for health care providers and staff. On-demand courses are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network. The following learning opportunities are available: e-referral mini module: Submitting an inpatient authorization: This is a revised interactive mini module in the series on using e-referral to submit prior authorization requests. The new format is based on an interactive system simulation, where you will learn the basics of submitting an inpatient authorization. The hands-on module only takes about 6 minutes to complete. CMS Star and HEDIS® measures mini modules: Prior eLearning courses on Star and HEDIS measures are now broken down into mini modules. You can learn about the measures in just a few minutes each. Search star or HEDIS to see the list of available topics. The mini modules have all the updates from the 2025 technical specifications. Prior authorization best practices — for requests managed by Carelon Medical Benefits Management: Register now for the webinar on June 17 from 1 to 2 p.m. Topics include important program updates for 2025 and case studies with Carelon provider portal walk-throughs. The goal is to help providers be successful when handling requests for prior authorization. How to access provider training resources To access the training site, follow these steps: Existing users who used the same email address as their provider portal profile email will be directed to the training site. If you used a different email address, contact ProviderTraining@bcbsm.com to update your profile. Those who don’t have a provider portal account can directly access the training through the provider training website. Questions? For more information about using the provider training website, contact the provider training team at ProviderTraining@bcbsm.com. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. HEDIS is also known as the Healthcare Effectiveness Data and Information Set. HEDIS® is a registered trademark of the National Committee for Quality Assurance. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Register now for 2025 virtual provider symposium sessionsThis year’s virtual health care provider symposiums start in May. They’ll focus on quality measures and review of evaluation and management guidelines. Registration is now open on the provider training website. Physicians, physician assistants, nurse practitioners, nurses and coders can receive continuing education credits for attending. Once logged in to the provider training site, open the event calendar to sign up for any of the sessions listed below. All times are Eastern time. All Star Performance-HEDIS®/Star Rating Measure Overview: The Golden Star Awards For physicians and office staff responsible for closing gaps in care related to quality measures for adults
Conducting an Internal Chart Audit: Livestreaming with April For physicians, coders, billers and administrative staff
How to register on the provider training website Provider portal users with an Availity Essentials™ account can access the provider training website: You can also directly access the training website if you don’t have a provider portal account. Questions? **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. HEDIS® is a registered trademark of the National Committee for Quality Assurance. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. Accreditation statement: This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of the Minnesota Medical Association and Blue Cross Blue Shield of Michigan. The Minnesota Medical Association (MMA) is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. CME statement: The Minnesota Medical Association designates this internet live activity for a maximum of 2 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Check out resources for heart health, antibiotic use, immunizationsThis is part of an ongoing series of articles focusing on the tools and resources available to help FEP® members manage their health. When patients understand the importance of heart health, antibiotic use and immunizations it will help keep them healthy and will also help providers meet HEDIS® requirements. Heart health Hypertension, clinical atherosclerotic cardiovascular disease and diabetes can all affect a patient’s heart health. Here are some flyers to share with patients to help them understand the importance of treatment compliance: Blue Cross Blue Shield of Michigan created tip sheets to help health care providers meet HEDIS requirements: Antibiotics The CDC flyer Antibiotics Aren’t Always the Answer** may help patients with acute bronchitis or bronchiolitis understand why antibiotics aren’t recommended tor treatment. The flyer explains that antibiotics don’t work on viruses and discusses the danger of antibiotic resistance. Blue Cross developed a HEDIS tip sheet for Avoidance of Antibiotic Treatment for Acute Bronchitis/Bronchiolitis (AAB) to help inform providers of the measure requirements, including coding tips and patient education. Immunizations The CDC has age-specific flyers to help patients understand the importance of immunizations. These flyers show when immunizations should be received and the symptoms and disease complications each virus can cause: Blue Cross also created HEDIS tip sheets for providers to help meet coding and patient education requirements for immunizations: FEP benefit information For information on Blue Cross and Blue Shield Federal Employee Program® benefits, providers and members can visit fepblue.org or call Customer Service at 1-800-482-3600 for Federal Employee Health Benefits information or 1-877-760-8574 for Postal Service Health Benefits information. **Blue Cross Blue Shield of Michigan doesn’t own or control this website. HEDIS®, which stands for Healthcare Effectiveness Data and Information Set, is a registered trademark of the National Committee for Quality Assurance or NCQA.
Reminder: Chiropractors invited to join new quality reward programBlue Cross Blue Shield of Michigan is offering all participating chiropractors the opportunity to join our new low back pain quality reward program. As part of the program, engaged chiropractors can earn a value-based reimbursement of 5% on eligible PPO professional claims for the pay period of Sept. 1, 2026, through Aug. 31, 2027. Participating chiropractors need to sign up by June 30, 2025, to be eligible. For more information about the program, see the January issue of The Record and the chiropractic quality rewards website.
Reminder: Prior authorization won’t be required for pain management procedures for Medicare Advantage members, starting May 1For dates of service on or after May 1, 2025, Blue Cross Blue Shield of Michigan and Blue Care Network will no longer require prior authorization for pain management procedures for Medicare Plus Blue℠ and BCN Advantage℠ members. We previously announced this change in a Jan. 31, 2025, provider alert. For pain management procedures with dates of service on or before April 30, 2025, health care providers can submit retroactive authorization requests to TurningPoint Healthcare Solutions through July 31, 2025. TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Tyenne will be preferred tocilizumab biosimilar product for most commercial members, starting June 1We will change how we manage Actemra® and Actemra biosimilar products, starting June 1, 2025. This change will affect most Blue Cross Blue Shield of Michigan and Blue Care Network commercial members covered under pharmacy and medical benefits. How this will affect members under pharmacy benefits Actemra (tocilizumab) subcutaneous, or SC, injection will no longer be covered for all commercial fully insured and self-funded groups using the Custom, Custom Select and Clinical drug lists. Tyenne® (tocilizumab-aazg) will be the preferred (tocilizumab) biosimilar product. Authorizations for Actemra will remain in effect until May 31, 2025. If members decide to use Actemra on or after June 1, they’ll be responsible for the full cost. New authorizations for Tyenne SC will be approved June 1, 2025, and active through May 31, 2026, so members can continue therapy without interruption. Filling the prescription We’ll only pay for Tyenne when filled through Walgreens Specialty Pharmacy, an independent company that provides specialty pharmacy services to Blue Cross and BCN. Members who currently fill their Actemra SC prescriptions at the Michigan Medicine Specialty Pharmacy may continue filling there. If members are currently filling Actemra SC through Walgreens Specialty Pharmacy: If members are currently filling their prescriptions through a pharmacy other than those mentioned above: Prescribers can send a new prescription for Tyenne SC by one of the following methods:
How this will affect members under medical benefits For dates of service on or after June 1, 2025, TyenneIV and SC (tocilizumab-aazg), HCPCS code Q5135, will be the preferred tocilizumab biosimilar product. The nonpreferred tocilizumab products are Tofidence™ IV (intravenous), Avtozma® IV and SC and Actemra® IV and SC. Members who have active authorizations for a nonpreferred tocilizumab product are authorized to continue their current therapy through May 31, 2025. We’re issuing authorizations for Tyenne from June 1, 2025, to May 31, 2026, to avoid any interruptions in care. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. How to submit prior authorization requests For a self-administered ustekinumab SC product (covered under pharmacy benefits), submit the request using an electronic prior authorization, or ePA, tool such as CoverMyMeds® or Surescripts®. For an ustekinumab IV product that requires administration by a health care provider (covered under medical benefits), submit the request through the NovoLogix® online tool. NovoLogix® is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network. Walgreens Specialty Pharmacy is an independent company that provides specialty pharmacy services covered under the pharmacy benefit for various Blue Cross Blue Shield of Michigan and Blue Care Network members with commercial plans.
We won’t be implementing STI clinical test code bundle for Blue Cross commercialFor Blue Cross Blue Shield of Michigan commercial members, sexually transmitted infection test code bundling won’t occur at this time. In June 2024, we informed you that Blue Cross commercial would be introducing new claim edits to bundle STI test codes. After additional consideration, we’ve decided not to implement this editing at this time. We’ll communicate with you if a determination is made to pursue this initiative in the future.
Complete Continuity of Care Guideline in e referral system for some Medicare Advantage membersFor select Medicare Plus Blue℠ and BCN Advantage℠ members who are eligible for continuity of care arrangements, health care providers need to provide additional information in the e-referral system. This started April 3, 2025. When will the questionnaire open? Providers need to respond to the Continuity of Care Guideline when submitting prior authorization requests for: What information will be requested? Providers will have to indicate whether: Providers will also have to attest that:
Update: Commercial prior authorization requests submitted through NovoLogix must be submitted through a different applicationFor most Blue Cross Blue Shield of Michigan and Blue Care Network commercial members, health care providers need to submit prior authorization requests for medical benefit drugs that are currently submitted through the NovoLogix® online tool through the Medical and Pharmacy Drug PA Portal. In a Jan. 3 provider alert, we announced that this change would happen on April 1, 2025, but the date was extended to April 21. Use the Medical and Pharmacy Drug PA Portal to submit both medical and pharmacy drug prior authorization requests for commercial members.** To access it: Here are a few notes to remember: Training opportunities A demo of the new application is available on our provider training site. You can also register for upcoming Q&A sessions. To find these opportunities, search on drugs. Important: Before attending a live Q&A session, be sure to watch the recorded demo, called Medical and Pharmacy Drug PA Portal Overview. The Q&A sessions will take place in May. Check the Provider Training site for dates and times. To access the training site, follow these steps: For issues regarding access to or navigating the site, email ProviderTraining@bcbsm.com. **Submit prior authorization requests for oncology medical and pharmacy benefit drugs to OncoHealth. For more information, see the document titled Oncology Value Management program through OncoHealth: FAQ for providers. ***Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. OncoHealth is an independent company supporting Blue Cross Blue Shield of Michigan and Blue Care Network by providing cancer support services.
We’ve made changes to prior authorization for select servicesAction item Review the changes we’ve recently made to prior authorization for select services, which also affect some questionnaires in the e-referral system. On March 23, Blue Cross Blue Shield of Michigan and Blue Care Network changed prior authorization requirements for some services. We’ve updated the document Preview questionnaires and medical necessity criteria, previously titled Authorization criteria and preview questionnaires, on ereferrals.bcbsm.com to reflect any questionnaire changes. Changes to prior authorization requirements and questionnaires
Preview questionnaires and medical necessity criteria For some of the above services, health care providers are prompted to complete questionnaires in the e-referral system. Refer to the Preview questionnaires and medical necessity criteria for: As a reminder, we use the pertinent medical necessity criteria and your answers to the questionnaires in the e-referral system when making utilization management determinations on your prior authorization requests.
Pharmacy news roundupWhat you need to know To view all — including the most recent — pharmacy-related provider alerts: Here are links to pharmacy-related provider alerts from March: Tip: You can also subscribe to Provider Alerts Weekly to receive a weekly email with links to the previous week’s provider alerts. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Professional reimbursement increased for select procedures performed in ambulatory surgical facilitiesBlue Cross Blue Shield of Michigan and Blue Care Network professional reimbursement policy increased allowed amounts by 15% over our professional fee schedule for select procedures when these procedures are performed in an ambulatory surgical facility. The changes went into effect March 21, 2025, unless otherwise noted and affect Blue Cross commercial, Medicare Plus Blue℠, BCN commercial and BCN Advantage℠ members. We’re making these changes because technological and clinical advances allow more procedures to be safely performed in the ambulatory setting. However, we recognize that you may need to make some process changes when performing these procedures outside a hospital setting. Increased professional payments are applicable for certain procedures for the specialties and lines of business noted in the table below.
1The 15% enhanced reimbursement for Blue Cross commercial will begin for select ear, nose and throat and urology procedures in the second quarter. We’ll publish a provider alert when this goes into effect for Blue Cross commercial. 2The 15% enhanced reimbursement for these services went into effect in 2024. We’ll continue to closely monitor our list of eligible procedure codes and adjust it based on provider input and other factors, including the effectiveness of the policy. Any other procedures not listed will be paid following our standard fee schedules. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Skilled nursing facility claim reviews resume for Medicare Plus Blue on June 1, 2025.EXL, an independent company that reviews claims for Blue Cross Blue Shield of Michigan, will resume auditing Medicare Plus Blue℠ skilled nursing facility claims, starting June 1, 2025. We posted a provider alert on April 1, 2025, about this change. SNF level of care is reasonable and necessary if the patient meets all requirements. The audits will verify that the skilled nursing facility level of care is reasonable and necessary, and that the documentation provided meets the requirements. EXL will review the documentation to ensure that an appropriate number of days are billed for the Patient Driven Payment Model score generated on each Minimum Data Set assessment, based on the Centers for Medicare & Medicaid Services guidelines. Additionally, auditors will compare the payment-related items on the MDS assessment with the medical record to ensure the assessment was coded correctly. Audit details The audits will look back at 12 months of claims and review the following: What to expect Be ready to share medical charts. After an audit, EXL will send a letter with findings and information about requesting a reconsideration, if necessary. Questions? Contact EXL Provider Relations at 1-833-717-0378 from 8 a.m. to 5 p.m. Eastern time Monday through Friday.
Reminder: Prior authorization won’t be required for pain management procedures for Medicare Advantage members, starting May 1For dates of service on or after May 1, 2025, Blue Cross Blue Shield of Michigan and Blue Care Network will no longer require prior authorization for pain management procedures for Medicare Plus Blue℠ and BCN Advantage℠ members. We previously announced this change in a Jan. 31, 2025, provider alert. For pain management procedures with dates of service on or before April 30, 2025, health care providers can submit retroactive authorization requests to TurningPoint Healthcare Solutions through July 31, 2025. TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Tyenne will be preferred tocilizumab biosimilar product for most commercial members, starting June 1We will change how we manage Actemra® and Actemra biosimilar products, starting June 1, 2025. This change will affect most Blue Cross Blue Shield of Michigan and Blue Care Network commercial members covered under pharmacy and medical benefits. How this will affect members under pharmacy benefits Actemra (tocilizumab) subcutaneous, or SC, injection will no longer be covered for all commercial fully insured and self-funded groups using the Custom, Custom Select and Clinical drug lists. Tyenne® (tocilizumab-aazg) will be the preferred (tocilizumab) biosimilar product. Authorizations for Actemra will remain in effect until May 31, 2025. If members decide to use Actemra on or after June 1, they’ll be responsible for the full cost. New authorizations for Tyenne SC will be approved June 1, 2025, and active through May 31, 2026, so members can continue therapy without interruption. Filling the prescription We’ll only pay for Tyenne when filled through Walgreens Specialty Pharmacy, an independent company that provides specialty pharmacy services to Blue Cross and BCN. Members who currently fill their Actemra SC prescriptions at the Michigan Medicine Specialty Pharmacy may continue filling there. If members are currently filling Actemra SC through Walgreens Specialty Pharmacy: If members are currently filling their prescriptions through a pharmacy other than those mentioned above: Prescribers can send a new prescription for Tyenne SC by one of the following methods:
How this will affect members under medical benefits For dates of service on or after June 1, 2025, TyenneIV and SC (tocilizumab-aazg), HCPCS code Q5135, will be the preferred tocilizumab biosimilar product. The nonpreferred tocilizumab products are Tofidence™ IV (intravenous), Avtozma® IV and SC and Actemra® IV and SC. Members who have active authorizations for a nonpreferred tocilizumab product are authorized to continue their current therapy through May 31, 2025. We’re issuing authorizations for Tyenne from June 1, 2025, to May 31, 2026, to avoid any interruptions in care. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. How to submit prior authorization requests For a self-administered ustekinumab SC product (covered under pharmacy benefits), submit the request using an electronic prior authorization, or ePA, tool such as CoverMyMeds® or Surescripts®. For an ustekinumab IV product that requires administration by a health care provider (covered under medical benefits), submit the request through the NovoLogix® online tool. NovoLogix® is an independent company that provides an online prescription drug prior authorization tool for Blue Cross Blue Shield of Michigan and Blue Care Network. Walgreens Specialty Pharmacy is an independent company that provides specialty pharmacy services covered under the pharmacy benefit for various Blue Cross Blue Shield of Michigan and Blue Care Network members with commercial plans.
We won’t be implementing STI clinical test code bundle for Blue Cross commercialFor Blue Cross Blue Shield of Michigan commercial members, sexually transmitted infection test code bundling won’t occur at this time. In June 2024, we informed you that Blue Cross commercial would be introducing new claim edits to bundle STI test codes. After additional consideration, we’ve decided not to implement this editing at this time. We’ll communicate with you if a determination is made to pursue this initiative in the future.
Complete Continuity of Care Guideline in e referral system for some Medicare Advantage membersFor select Medicare Plus Blue℠ and BCN Advantage℠ members who are eligible for continuity of care arrangements, health care providers need to provide additional information in the e-referral system. This started April 3, 2025. When will the questionnaire open? Providers need to respond to the Continuity of Care Guideline when submitting prior authorization requests for: What information will be requested? Providers will have to indicate whether: Providers will also have to attest that:
Update: Commercial prior authorization requests submitted through NovoLogix must be submitted through a different applicationFor most Blue Cross Blue Shield of Michigan and Blue Care Network commercial members, health care providers need to submit prior authorization requests for medical benefit drugs that are currently submitted through the NovoLogix® online tool through the Medical and Pharmacy Drug PA Portal. In a Jan. 3 provider alert, we announced that this change would happen on April 1, 2025, but the date was extended to April 21. Use the Medical and Pharmacy Drug PA Portal to submit both medical and pharmacy drug prior authorization requests for commercial members.** To access it: Here are a few notes to remember: Training opportunities A demo of the new application is available on our provider training site. You can also register for upcoming Q&A sessions. To find these opportunities, search on drugs. Important: Before attending a live Q&A session, be sure to watch the recorded demo, called Medical and Pharmacy Drug PA Portal Overview. The Q&A sessions will take place in May. Check the Provider Training site for dates and times. To access the training site, follow these steps: For issues regarding access to or navigating the site, email ProviderTraining@bcbsm.com. **Submit prior authorization requests for oncology medical and pharmacy benefit drugs to OncoHealth. For more information, see the document titled Oncology Value Management program through OncoHealth: FAQ for providers. ***Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. OncoHealth is an independent company supporting Blue Cross Blue Shield of Michigan and Blue Care Network by providing cancer support services.
We’ve made changes to prior authorization for select servicesAction item Review the changes we’ve recently made to prior authorization for select services, which also affect some questionnaires in the e-referral system. On March 23, Blue Cross Blue Shield of Michigan and Blue Care Network changed prior authorization requirements for some services. We’ve updated the document Preview questionnaires and medical necessity criteria, previously titled Authorization criteria and preview questionnaires, on ereferrals.bcbsm.com to reflect any questionnaire changes. Changes to prior authorization requirements and questionnaires
Preview questionnaires and medical necessity criteria For some of the above services, health care providers are prompted to complete questionnaires in the e-referral system. Refer to the Preview questionnaires and medical necessity criteria for: As a reminder, we use the pertinent medical necessity criteria and your answers to the questionnaires in the e-referral system when making utilization management determinations on your prior authorization requests.
Pharmacy news roundupWhat you need to know To view all — including the most recent — pharmacy-related provider alerts: Here are links to pharmacy-related provider alerts from March: Tip: You can also subscribe to Provider Alerts Weekly to receive a weekly email with links to the previous week’s provider alerts. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||