Subscribe | The Record Archive | Contacts | bcbsm.com
|
August 2025
Reminder: Participating providers may only collect applicable deductibles, copayments from members upfrontWe want to remind participating providers that you must bill Blue Cross Blue Shield of Michigan and Blue Care Network for all covered services and may only bill members for their applicable deductibles and copayments. In keeping with provider contracts, you may not collect deposits or bill members upfront for unpaid balances of covered services. The following guidance comes from the “Patient Copayment and Deductible Requirements” chapter of the Blue Cross Commercial Provider Manual.
Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Coding corner: Morbid obesity and its connection to risk adjustmentsAccurately documenting morbid obesity is essential due to the rise of obesity rates — particularly when it affects a patient's overall health and risk score. This article outlines the current best practices and requirements for documenting and coding morbid obesity across the Affordable Care Act, Medicare Advantage and Medicaid risk adjustment models. Morbid obesity (ICD-10-CM: E66.01) is risk adjustable under HCC 22. Clinical indicators supporting morbid obesity To code E66.01 (morbid obesity due to excess calories), the health care provider should clearly document:
Documentation do’s and don’ts ✘ Don’t use vague terms such as “obesity” without including supporting criteria. Here’s an example of what incomplete and correct documentation looks like: ✘ Incomplete: Obesity noted. Monitoring Coder guidance When reviewing documentation:
Quick reference checklist
None of the information included here is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws, and regulations.
2025 HCPCS 2nd-quarter update: New, deleted codesThe Centers for Medicare & Medicaid Services has added several new codes as part of its quarterly Healthcare Common Procedure Coding System updates. The codes, effective dates and Blue Cross Blue Shield of Michigan’s coverage decisions are below. Surgery/skin substitute
Injections/chemotherapy
Injections
Procedures/professional services (temporary) evaluation and management non-face-to-face services
Procedures/professional services (temporary) care management service
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
HCPCS replacement codes established, effective July 1, 2025C9175 replaces C9399 when billing for Grafapex (treosulfan) Effective July 1, 2025, the Centers for Medicare & Medicaid Services, or CMS, has established a new procedure code for Grafapex™ (treosulfan). All services through June 30, 2025, will continue to be reported with code C9399. All services performed on and after July 1, 2025, must be reported with C9175. Prior authorization is required through the Medical Benefit Drug program for C9175 for all groups, unless they are opted out of the program. To see which groups particpate in the program, check out the Prior Authorization Master Opt-in/out Group List. For groups that have opted out of the prior authorization program, this code is covered for its FDA-approved indications. J7172 replaces C9399, J3490, J3590, J9999 when billing for Hympavzi Effective July 1, 2025, CMS has established a new procedure code for specialty medical drug Hympavzi™ (marstacimab-hncq). All services through June 30, 2025, will continue to be reported with codes C9399, J3490, J3590 and J9999. All services performed on and after July 1, 2025, must be reported with J7172. Prior authorization is required through the Medical Benefit Drug program for J7172 for all groups, unless they are opted out of the program. To see which groups particpate in the program, check out the Prior Authorization Master Opt-in/out Group List. For groups that have opted out of the prior authorization program, this code is covered for its FDA-approved indications. Q5098 replaces C9399, J3490, J3590, J9999 when billing for Imuldosa (ustekinumab-srlf) Effective July 1, 2025, CMS has established a new procedure code for specialty medical drug Imuldosa® (ustekinumab-srlf). All services through June 30, 2025, will continue to be reported with codes C9399, J3490, J3590 and J9999. All services performed on and after July 1, 2025, must be reported with Q5098. Prior authorization is required through the Medical Benefit Drug program for Q5098 for all groups, unless they are opted out of the program. To see which groups particpate in the program, check out the Prior Authorization Master Opt-in/out Group List. For groups that have opted out of the prior authorization program, this code is covered for its FDA-approved indications. Q5099 replaces C9399, J3490, J3590, J9999 when billing for Steqeyma (ustekinumab-stba) Effective July 1, 2025, CMS has established a new procedure code for specialty medical drug Steqeyma® (ustekinumab-stba). All services through June 30, 2025, will continue to be reported with codes C9399, J3490, J3590 and J9999. All services performed on and after July 1, 2025, must be reported with Q5099. Prior authorization is required through the Medical Benefit Drug program for Q5099 for all groups, unless they are opted out of the program. To see which groups particpate in the program, check out the Prior Authorization Master Opt-in/out Group List. For groups that have opted out of the prior authorization program, this code is covered for its FDA-approved indications. Q5100 replaces C9399, J3490, J3590, J9999 when billing for Yesintek (ustekinumab-kfce) Effective July 1, 2025, CMS has established a new procedure code for specialty medical drug Yesintek™ (ustekinumab-kfce). All services through June 30, 2025, will continue to be reported with codes C9399, J3490, J3590 and J9999. All services performed on and after July 1, 2025, must be reported with Q5100. Prior authorization is required through the Medical Benefit Drug program for Q5100 for all groups, unless they are opted out of the program. To see which groups particpate in the program, check out the Prior Authorization Master Opt-in/out Group List. For groups that have opted out of the prior authorization program, this code is covered for its FDA-approved indications. Q5153 replaces C9399, J3490, J3590, J9999 when billing for Opuviz (aflibercept-yszy) Effective July 1, 2025, CMS has established a new procedure code for specialty medical drug Opuviz™ (aflibercept-yszy). All services through June 30, 2025, will continue to be reported with codes C9399, J3490, J3590 and J9999. All services performed on and after July 1, 2025, must be reported with Q5153. Prior authorization is required through the Medical Benefit Drug program for Q5153 for all groups, unless they are opted out of the program. To see which groups particpate in the program, check out the Prior Authorization Master Opt-in/out Group List. For groups that have opted out of the prior authorization program, this code is covered for its FDA-approved indications.
Billing chart: Blue Cross highlights medical, benefit policy changesYou’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the “Billing chart.” The billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures. We’ll publish information about new Blue Cross groups or changes to group benefits under the Group Benefit Changes heading. For more detailed descriptions of Blue Cross’ policies for these procedures, check under the Commercial Policy tab in Benefit Explainer on Availity Essentials™. To access this online information:
To view the “August 2025 Billing chart,” click here. **Blue Cross Blue Shield of Michigan doesn’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Reminder: Follow these requirements when billing for noncovered servicesBlue Cross Blue Shield of Michigan has been informed that some health care providers have been billing our members for services that have been deemed “provider liable” on their remittance advice or payment vouchers. This action doesn’t align with the terms outlined in our provider agreements. As a result, we’re reminding our participating health care providers that they’re required to comply with the terms of their contracts. While our provider contracts allow members to choose to pay for noncovered services, providers must follow the steps outlined below before rendering the service:
All provider agreements, including the Participating Hospital Agreement (Article II, Section 7[b]) and the Traditional Professional Provider Agreement (Addendum F, Section 2), contain steps like those listed above. A general financial form stating that the member is responsible for additional costs not covered by insurance isn’t sufficient to meet this requirement. You must obtain a specific, signed agreement from the member for each noncovered service. Action required To avoid any issues, immediately stop billing members for amounts exceeding their cost share or provide a compliant agreement signed by the member to support continued billing. Failure to follow this process may result in additional action by Blue Cross, up to and including termination of the provider or facility contract.
Clinical editing updates: IMRT billing rules; sequela codes; clinical editing portal; add-on code G2211In support of correct coding and payment accuracy, we are providing the information below to keep you informed about forthcoming payment policy updates, new policies and coding reminders. Blue Cross Blue Shield of Michigan commercial Reminder: We’re updating IMRT billing rules to include professional claims In the July 2023 Record article, “Reminder: IMRT delivery codes ,” we detailed editing for facility claims to prevent separate billing for intensity-modulated radiation therapy, or IMRT, delivery services within 14 days of the IMRT planning code. As communicated in a June 27, 2025, provider alert , we will expand this editing to include professional claims this fall. Reminder: Sequela codes A sequela is the condition produced after the acute phase of an illness or injury has terminated. According to ICD-10-CM guidelines, it’s inappropriate to bill a sequela (7th character “S”) code as the primary, first listed or principal diagnosis, nor can it be the only diagnosis code on the claim. Claims not billed in accordance with the ICD-10-CM guidelines may be denied. This applies to professional and facility claims. Medicare Plus Blue℠ Reminder: Medicare Plus Blue clinical editing portal available through Availity In March 2024, we announced that the Medicare Plus Blue Clinical Editing System, or CES, portal is available through Availity EssentialsTM. The CES portal provides additional details to health care providers when a Medicare Plus Blue claim goes through clinical editing. Health care providers can use the portal to enter a hypothetical professional or facility claim or look up a processed claim to see the CES results for Medicare Plus Blue members whose member ID begins with X3L. When using the portal, providers must input claims data, whether hypothetical or a live claim. Once the claim has been analyzed, the line-by-line edits are returned and displayed in the user interface. The Professional Claim Entry and Facility Claim Entry tabs allow a user to enter claim scenarios to be analyzed by CES. Claims entered in the portal aren’t submitted into the claims system. The portal provides a way to test different claim scenarios and identify potential edits without submitting a live claim. The Claim Lookup tab provides users with an option to search for claims that have been processed by the claim adjudication system. When searching for a processed claim in the CES portal, provider-level information and claim selection criteria are required. One of the following claim selection criteria must be entered to search for a claim:
To access the clinical editing portal, follow these steps:
This is a simulation tool that doesn’t guarantee approval or reimbursement of a claim. Other edits may apply when a claim is submitted and processed. A user guide is available on the provider training site and is also accessible from the provider portal. Under the Applications tab, click on Provider Training Site. Once you are on the site, use the keyword “claims” to search for the Claims Edit System Portal User Guide. If you need assistance navigating the provider training site, email ProviderTraining@bcbsm.com. BCN Advantage℠ Update: Office, outpatient E/M visit complexity add-on code G2211 In June, we communicated that the Centers for Medicare & Medicaid Services added information on how to use procedure code G2211 with modifier 25 for certain Medicare Part B services starting Jan. 1, 2025, and that our systems were updated to accommodate the changes in May 2025. System updates occurred later than initially communicated but were completed in June. The affected claims, which were professional claims, will be reprocessed. To avoid duplicate claim denials and delayed processing, don’t resubmit claims. Please allow up to eight weeks for reprocessing of affected claims. For additional Blue Care Network commercial and BCN Advantage clinical editing information, view the latest BCN Provider News issue, and look for "Clinical Editing Billing Tips" in the "Billing Bulletin" section. None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Send questions, register for our live session about clinical editingIn support of correct coding and payment accuracy, we’re hosting a live Q&A session about clinical editing. The topics will include how clinical editing works, requests that are returned for no rationale, required documentation and whether a claim should be corrected or reconsidered. The sessions will focus on solutions for common issues; we won’t troubleshoot specific claims. To help us prepare and focus on your needs, send general questions to providertraining@bcbsm.com. Register for the Clinical editing Q&A on our provider training website. The session is Tuesday, Aug. 26 from noon to 12:45 p.m. How to access provider training
If you don’t have a provider portal account, click this link to access the training website. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Update: Medicare Advantage prior authorization requests submitted through NovoLogix must be submitted through different application, starting Aug. 1Starting Aug. 1, 2025, health care providers will need to submit both medical and pharmacy drug prior authorization requests that are currently submitted through the NovoLogix® online tool through a different application. This applies to Medicare Plus Blue℠ and BCN Advantage℠ members.** In a March 27 provider alert, we communicated that this change would happen July 1 and that it would apply only to medical benefit drugs. However, the change will apply to both medical and pharmacy requests. The name of the new application is Medical and Pharmacy Drug PA Portal. To access the new application:
Notes:
Training opportunity To view a recorded demo that shows how to work in the Medical and Pharmacy Drug PA Portal, log in to our Provider Training site, search drugs and click on the Medical and Pharmacy Drug PA Portal Overview Mini Module. Although the recorded demo is currently specific to our commercial lines of business, you’ll follow the same basic steps when submitting prior authorization requests for Medicare Advantage members. We’re creating a new recorded demo that covers both our commercial and our Medicare Advantage lines of business; we’ll post a provider alert when it’s available. To access the training site:
If you have issues accessing or navigating the site, email ProviderTraining@bcbsm.com. **Submit prior authorization requests for oncology medical and pharmacy benefit drugs to OncoHealth. For more information, see the document titled Oncology Value Management program through OncoHealth: FAQ for providers. Alternately, providers can submit prior authorization requests for most pharmacy benefit drugs through CoverMyMeds or other electronic prior authorization, or ePA, tools. ***Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. OncoHealth is an independent company supporting Blue Cross Blue Shield of Michigan and Blue Care Network by providing cancer support services.
Answers to questions about changes to requirements for pain management procedures for our Medicare Advantage membersAs we communicated previously, pain management services no longer require prior authorization for Medicare Plus Blue℠ and BCN Advantage℠ members for dates of service on or after May 1, 2025. If you have questions that aren’t answered below, see the document titled Musculoskeletal procedure authorizations: Frequently asked questions for providers. Question: What pain management procedure codes no longer require prior authorization? Answer: The following pain management procedure codes no longer require prior authorization for our Medicare Advantage members:
Q: How do I update an existing TurningPoint pain management authorization for dates of service before May 1, 2025? A: Complete the Post-service change request form and fax it to TurningPoint at 313-879-5509. Note: If you already submitted a claim, click Yes for the question “Have you submitted a claim to Blue Cross or BCN?” To access the form, click the link above or:
Q: Can I request advance coverage determinations for pain management procedures for dates of service on or after May 1, 2025? A: Providers can request advance coverage determinations (also known as organization determinations) for pain management procedures for Medicare Advantage members. The steps vary depending on the member’s plan.
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
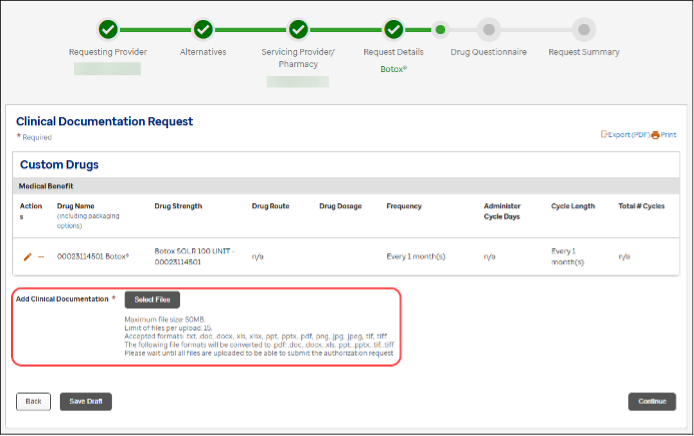
Submit clinical documentation through Medical and Pharmacy Drug PA PortalHealth care providers should upload clinical documentation through the Medical and Pharmacy Drug PA Portal. This means you can attach clinical documentation when submitting prior authorization requests, rather than faxing clinical documentation separately. We recommend that you attach clinical documentation when you create the request to help reduce:
Attach clinical documentation by clicking the Select Files button (shown below) when entering request details but before completing the drug questionnaires.
The restrictions and requirements for uploading clinical documentation are listed below the Select Files button. Note: If we need additional clinical documentation to review the request, you’ll need to fax it to the Blue Cross and BCN Pharmacy Clinical Help Desk. Learn more about the Medical and Pharmacy Drug PA Portal To learn how to work in the Medical and Pharmacy Drug PA Portal, view a recorded demo by going to Blue Cross and BCN’s Provider Training site, searching drugs and launching the “Medical and Pharmacy Drug PA Portal Overview Mini Module.” The demo will guide you through using the portal. To access the provider training site:
Email ProviderTraining@bcbsm.com if you have issues accessing or navigating the site. Additional information For additional information about submitting prior authorization requests for drugs, see the following pages on ereferrals.bcbsm.com:
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Enhancing care for seniorsAction item Explore a three-part webinar series focused on navigating sensitive topics. As physicians, you strive to deliver high-quality, patient-centered care to your senior patients. However, navigating sensitive topics and addressing unmet health concerns can be a challenge. That’s why we’re introducing an on-demand webinar series — Improving health outcomes for older adults — designed specifically for health care providers and their clinical staff. This three-part series is packed with practical strategies for discussing sensitive topics with seniors, such as mental health, urinary incontinence, fall risk and physical activity. You'll learn how to initiate and navigate these conversations with empathy and understanding, building trust and fostering open communication with your patients. By doing so, you'll not only improve patient outcomes but also strengthen your relationships with them. For Patient-Centered Medical Home practices, this series aligns with PCMH capabilities 9.13 (screening for fall risk and physical activity) and 9.14 (screening for bladder control). Here’s some of what you can expect from each part of the series: Part 1: Ensuring effective care through conversations Learn how to bring up sensitive topics with patients and get an introduction to the Health Outcomes Survey. You'll get tips for discussing urinary incontinence, physical activity and fall risk, as well as how the HOS is used by the Centers for Medicare & Medicaid Services to assess the health status of seniors over time. Part 2: Discussions to help older patients maintain or improve their mental and physical health Explore the risks of poor physical and mental health for older adults and learn strategies for discussing these topics with your patients. You'll also learn how patient-centered planning can improve or maintain patients’ health. Part 3: Overcoming barriers to sensitive conversations with patients Identify and overcome patient and provider anxiety around discussing sensitive topics. You'll gain tips to alleviate discomfort and learn how to prepare for these conversations with confidence. To access the patient experience library of content, log in to the provider training homepage through our provider portal, Availity Essentials™:
If you don’t have access to Availity, you can directly log in to the training website. You can also check out courses on other topics while you’re browsing. If you have questions about the provider training website, email ProviderTraining@bcbsm.com. Medical assistants and other health care professionals can earn continuing education credits with a certificate of completion. Physicians are eligible for continuing medical education credits upon successful completion of these courses and many other patient experience courses. We appreciate all you do to enhance the patient experience and are excited to support you in further developing your skills and expertise. For information, email PatientExperience@bcbsm.com. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Inpatient admissions for musculoskeletal procedures managed by TurningPointThe processes and requirements for inpatient admissions for musculoskeletal procedures vary depending on whether the inpatient setting is being requested before or after the procedure is performed. Before the procedure is performed If you request the inpatient setting for a musculoskeletal procedure before the procedure is performed, TurningPoint Healthcare Solutions LLC reviews the setting as part of the prior authorization request as follows:
Note: The TurningPoint medical policies are available in the TurningPoint provider portal.
Note: If an authorization for a procedure that’s on the list of inpatient-only procedures shows an outpatient setting for a Medicare Advantage member, contact TurningPoint toll-free at 1-833-217-9670 or locally at 313-908-6040 before performing the procedure. TurningPoint will update the setting on the authorization. After the procedure is performed If the member’s condition changes during the already approved outpatient stay and the member meets InterQual® guidelines for an inpatient admission, submit a prior authorization request for the inpatient stay to Blue Cross Blue Shield of Michigan or Blue Care Network through the e-referral system. Important:
Note: When entering requests for inpatient stays in the e-referral system, select “Inpatient Hospital” as the place of service, select “Direct” as the admission type and enter procedure code *99222. Additional information For additional information, see the following documents:
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Starting Oct. 6, submit prior authorization requests for FEP members through the e-referral systemStarting Oct. 6, 2025, health care providers can submit prior authorization requests for members who have coverage through the Blue Cross and Blue Shield Federal Employee Program® through the e-referral system. This change applies to procedures that are managed by Blue Cross Blue Shield of Michigan and affects FEP® members who have both commercial and Medicare Supplement plans. This change will benefit you by:
If you can’t submit prior authorization requests through the e-referral system, we’ll continue to accept prior authorization requests that are faxed to 1-866-294-5012 or sent through U.S. mail. In addition, you’ll be able to continue to check the status of prior authorization requests by calling:
Notes:
For more information about working in the e-referral system, see the e-referral User Guide. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services. For more information, go to our ereferrals.bcbsm.com website.
Pharmacy news roundupWhat you need to know To view all — including the most recent — pharmacy-related provider alerts:
Here are links to pharmacy-related provider alerts from June:
Tip: You can also subscribe to Provider Alerts Weekly to receive a weekly email with links to the previous week’s provider alerts. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Starting Sept. 1, we’ll change how we pay for certain medications for most Blue Cross, BCN commercial membersThe table below shows the medications we won’t pay for starting Sept. 1, 2025, as well as the alternative medications we’ll pay for starting Sept. 1. These drugs are managed through the Oncology Value Management program, which is administered by OncoHealth. These changes will affect most Blue Cross Blue Shield of Michigan and Blue Care Network commercial members with pharmacy benefits. These changes won’t apply to Medicare Advantage groups or members.
**Additional coverage requirements may apply for preferred alternatives. These requirements apply to the following Blue Cross and BCN commercial members when they receive these drugs in an outpatient setting in Michigan or in other states:
We’ll send letters about these changes to affected groups, members and their health care providers. How to submit prior authorization requests Submit prior authorization requests to OncoHealth on or after Aug. 20, 2025, using one of the following methods:
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Blue Cross, along with 17 other Blue plans, works with CivicaScript® (previously Civica Rx) to manufacture low-cost generic medications to reduce members’ out-of-pocket costs and improve savings for our customers. CivicaScript® is an independent company that will provide select generic drugs to Blue Cross Blue Shield of Michigan and Blue Care Network members. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. OncoHealth is an independent company supporting Blue Cross Blue Shield of Michigan and Blue Care Network by providing cancer support services.
We’re changing how we manage self-administered hemophilia products for most Blue Cross, BCN commercial members, starting Sept. 1Starting Sept. 1, 2025, self-administered formulations of hemophilia products will no longer be payable under medical benefits for Blue Cross Blue Shield of Michigan and Blue Care Network commercial members. Instead, they’ll be payable under pharmacy benefits. This change doesn’t apply to Medicare Advantage groups or members. Some members recently received a self-administered hemophilia product that was administered by a health care provider and billed under their medical benefits. Authorizations for self-administered hemophilia products will remain in effect under medical benefits until Aug. 31, 2025. If the hemophilia product they’re taking doesn't require prior authorization under medical benefits, no prior authorization is needed to transition to pharmacy benefits. A new authorization for a self-administered hemophilia product will be approved Sept. 1, 2025, under pharmacy benefits and active through Aug. 31, 2026, so members can continue therapy without interruption. Members can fill their prescriptions at in-network retail pharmacies. On or after Sept. 1, there will be no coverage provided for any self-administered hemophilia products through medical benefits. If members don’t have prescription coverage through Blue Cross or BCN and are currently filling their prescription for these medications through their Blue Cross or BCN medical benefit, they can check to see if their pharmacy plan will cover it. How to submit prior authorization requests Submit medical and pharmacy prior authorization requests through the Medical and Pharmacy Drug PA Portal, which you can access by clicking the Medical/Pharm Drug Benefit Prior Auth (Commercial) tile under the Applications tab in our provider portal at availity.com.** You can also submit pharmacy benefit drugs prior authorization requests using CoverMyMeds® . **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Reminder: CLIA numbers must be submitted for most lab testsWhen billing for laboratory tests, you must include your Clinical Laboratory Improvements Amendments certification number for any services that aren’t CLIA-waived. You should use the QW modifier for CLIA-waived tests and submit it in the first modifier field. Clinical Laboratory Improvements Amendments regulate laboratory testing. They require that clinical labs be certified by the state, as well as the Centers for Medicare & Medicaid Services, before they can accept samples for diagnostic testing. A certificate of waiver under CLIA is only granted to a lab that has performed a simple test such as the glucose meter test. These are tests that the Food and Drug Administration and the Centers for Disease Control and Prevention have determined are at little risk for error. For more details, see the Clinical Laboratory Improvement Amendments page** of the CMS.gov website. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Webinars for physicians, coders focus on documentation, codingAction item Register for our 2025 monthly Lunch & Learn webinars focusing on coding and documentation. In 2025, we’ll continue to offer webinars about documentation and coding of common challenging diagnoses. These live, lunchtime educational sessions will also include an opportunity to ask questions. Below is our schedule and topics for the sessions. All sessions start at noon Eastern time and should last for 30 minutes. Register for the sessions on the provider training website.
Provider training website access If you have an Availity Essentials™ account, you can access the provider training website this way:
Existing users who used the same email address as their provider portal profile email will be directed to the training site. If you used a different email address, contact ProviderTraining@bcbsm.com to update your profile. You can also directly access the training website if you don’t have a provider portal account. After logging in to the provider training website, look in Event Calendar to sign up for your desired session. You can also quickly search for all the sessions with the keyword “lunchtime” and then look under the results for Events. You can listen to the previously recorded sessions, too. Check out the following:
Questions?
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Resources to help manage mental health conditionsThis is part of an ongoing series of articles focusing on the tools and resources available to help FEP® members manage their health. Mental health is an important part of our overall health. It includes our emotional, psychological and social well-being. In the U.S., 1 in 5 adults experience mental illness** each year. Here are resources to help health care providers and patients manage mental health conditions. Antidepressants Antidepressants are many times a key part of treating depression symptoms. However, opinions vary on how effective antidepressants are in relieving symptoms. According to the National Center for Biotechnology Information’s article “Depression: Learn More – How effective are antidepressants?”** the main aim of treatment with antidepressants is to relieve the symptoms of severe depression. The NIH MedlinePlus Magazine article “Commonly prescribed antidepressants and how they work”** may help patients better understand their antidepressant medication. Safe opioid prescribing and use People who receive opioids from four or more prescribers or pharmacies have a higher likelihood of an opioid-related overdose death than those who receive opioids from one prescriber or one physician, according to the Journal of the American Medical Association. Blue Cross Blue Shield of Michigan continues to collaborate with the Overdose Prevention Engagement Network, or OPEN, to address the ongoing opioid crisis. In 2024, OPEN continued to refine its prescribing recommendations, which now include 32 adult procedures and 14 pediatric procedures. These evidence-based prescribing recommendations help providers deliver optimal pain control while reducing the risk of opioid dependence. The recommendations are accessible through the OPEN website.** For patients, the “Safe Way to Take Prescription Opioid Pain Medications” blog on MIBlueDaily talks about taking opioid medication safely and how to avoid an overdose. As a reminder, encouraging patients to follow up after an emergency department visit for a mental health or substance use condition can help improve mental health and reduce substance use, according to the National Committee for Quality Assurance. Resources for FEP members The Blue Cross and Blue Shield Federal Employee Program® offers additional resources to help members manage their conditions at home.
If providers or members have questions about FEP benefits, they can call Customer Service at 1-800-482-3600 for Federal Employees Health Benefits or 1-877-760-8574 for Postal Service Health Benefits, or go to fepblue.org. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Reminder: Make sure critical care services are billed appropriately for ER visitsBlue Cross Blue Shield of Michigan will recover funds for paid claims when we discover that critical care services were billed for an emergency room visit in which a patient was discharged home during the same ER visit. If a patient is discharged home from an ER, it’s usually not appropriate to bill the claim as a critical care service. If a patient is discharged home from the ER, and he or she isn’t critically ill, then it might be more appropriate to bill the service as an ER evaluation and management, or E/M, code. We encourage health care providers to review their claims for proper billing and coding before submitting them. Providers may rebill with a lower CPT code, when appropriate. Affected codes:
Note: We use the definition of “critically ill” that’s included in American Medical Association and Centers for Medicare & Medicaid Services guidelines.
Reminder: Submit prior authorization requests for non-emergency air ambulance flights to Alacura before takeoffMichigan and non-Michigan providers must submit prior authorization requests for all non-emergency air ambulance services to Alacura Medical Transportation Management before each flight. This requirement applies to Blue Cross Blue Shield of Michigan and Blue Care Network commercial members. The prior authorization process helps ensure that the air ambulance provider is in-network, which is crucial for helping patients manage their costs and receive optimal care. The high cost of using an out-of-network air ambulance provider falls largely to members and puts significant stress on both groups and members to assume financial responsibility. For information on how to submit prior authorization requests to Alacura, refer to the document Non-emergency air ambulance prior authorization program: Overview for Michigan and non-Michigan providers.
Alacura Medical Transport Management is an independent company that manages the authorization of non-emergency flights for Blue Cross Blue Shield of Michigan and Blue Care Network members who have commercial plans.
Reminder: Follow these requirements when billing for noncovered servicesBlue Cross Blue Shield of Michigan has been informed that some health care providers have been billing our members for services that have been deemed “provider liable” on their remittance advice or payment vouchers. This action doesn’t align with the terms outlined in our provider agreements. As a result, we’re reminding our participating health care providers that they’re required to comply with the terms of their contracts. While our provider contracts allow members to choose to pay for noncovered services, providers must follow the steps outlined below before rendering the service:
All provider agreements, including the Participating Hospital Agreement (Article II, Section 7[b]) and the Traditional Professional Provider Agreement (Addendum F, Section 2), contain steps like those listed above. A general financial form stating that the member is responsible for additional costs not covered by insurance isn’t sufficient to meet this requirement. You must obtain a specific, signed agreement from the member for each noncovered service. Action required To avoid any issues, immediately stop billing members for amounts exceeding their cost share or provide a compliant agreement signed by the member to support continued billing. Failure to follow this process may result in additional action by Blue Cross, up to and including termination of the provider or facility contract.
Clinical editing updates: IMRT billing rules; sequela codes; clinical editing portal; add-on code G2211In support of correct coding and payment accuracy, we are providing the information below to keep you informed about forthcoming payment policy updates, new policies and coding reminders. Blue Cross Blue Shield of Michigan commercial Reminder: We’re updating IMRT billing rules to include professional claims In the July 2023 Record article, “Reminder: IMRT delivery codes ,” we detailed editing for facility claims to prevent separate billing for intensity-modulated radiation therapy, or IMRT, delivery services within 14 days of the IMRT planning code. As communicated in a June 27, 2025, provider alert , we will expand this editing to include professional claims this fall. Reminder: Sequela codes A sequela is the condition produced after the acute phase of an illness or injury has terminated. According to ICD-10-CM guidelines, it’s inappropriate to bill a sequela (7th character “S”) code as the primary, first listed or principal diagnosis, nor can it be the only diagnosis code on the claim. Claims not billed in accordance with the ICD-10-CM guidelines may be denied. This applies to professional and facility claims. Medicare Plus Blue℠ Reminder: Medicare Plus Blue clinical editing portal available through Availity In March 2024, we announced that the Medicare Plus Blue Clinical Editing System, or CES, portal is available through Availity EssentialsTM. The CES portal provides additional details to health care providers when a Medicare Plus Blue claim goes through clinical editing. Health care providers can use the portal to enter a hypothetical professional or facility claim or look up a processed claim to see the CES results for Medicare Plus Blue members whose member ID begins with X3L. When using the portal, providers must input claims data, whether hypothetical or a live claim. Once the claim has been analyzed, the line-by-line edits are returned and displayed in the user interface. The Professional Claim Entry and Facility Claim Entry tabs allow a user to enter claim scenarios to be analyzed by CES. Claims entered in the portal aren’t submitted into the claims system. The portal provides a way to test different claim scenarios and identify potential edits without submitting a live claim. The Claim Lookup tab provides users with an option to search for claims that have been processed by the claim adjudication system. When searching for a processed claim in the CES portal, provider-level information and claim selection criteria are required. One of the following claim selection criteria must be entered to search for a claim:
To access the clinical editing portal, follow these steps:
This is a simulation tool that doesn’t guarantee approval or reimbursement of a claim. Other edits may apply when a claim is submitted and processed. A user guide is available on the provider training site and is also accessible from the provider portal. Under the Applications tab, click on Provider Training Site. Once you are on the site, use the keyword “claims” to search for the Claims Edit System Portal User Guide. If you need assistance navigating the provider training site, email ProviderTraining@bcbsm.com. BCN Advantage℠ Update: Office, outpatient E/M visit complexity add-on code G2211 In June, we communicated that the Centers for Medicare & Medicaid Services added information on how to use procedure code G2211 with modifier 25 for certain Medicare Part B services starting Jan. 1, 2025, and that our systems were updated to accommodate the changes in May 2025. System updates occurred later than initially communicated but were completed in June. The affected claims, which were professional claims, will be reprocessed. To avoid duplicate claim denials and delayed processing, don’t resubmit claims. Please allow up to eight weeks for reprocessing of affected claims. For additional Blue Care Network commercial and BCN Advantage clinical editing information, view the latest BCN Provider News issue, and look for "Clinical Editing Billing Tips" in the "Billing Bulletin" section. None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Update: Medicare Advantage prior authorization requests submitted through NovoLogix must be submitted through different application, starting Aug. 1Starting Aug. 1, 2025, health care providers will need to submit both medical and pharmacy drug prior authorization requests that are currently submitted through the NovoLogix® online tool through a different application. This applies to Medicare Plus Blue℠ and BCN Advantage℠ members.** In a March 27 provider alert, we communicated that this change would happen July 1 and that it would apply only to medical benefit drugs. However, the change will apply to both medical and pharmacy requests. The name of the new application is Medical and Pharmacy Drug PA Portal. To access the new application:
Notes:
Training opportunity To view a recorded demo that shows how to work in the Medical and Pharmacy Drug PA Portal, log in to our Provider Training site, search drugs and click on the Medical and Pharmacy Drug PA Portal Overview Mini Module. Although the recorded demo is currently specific to our commercial lines of business, you’ll follow the same basic steps when submitting prior authorization requests for Medicare Advantage members. We’re creating a new recorded demo that covers both our commercial and our Medicare Advantage lines of business; we’ll post a provider alert when it’s available. To access the training site:
If you have issues accessing or navigating the site, email ProviderTraining@bcbsm.com. **Submit prior authorization requests for oncology medical and pharmacy benefit drugs to OncoHealth. For more information, see the document titled Oncology Value Management program through OncoHealth: FAQ for providers. Alternately, providers can submit prior authorization requests for most pharmacy benefit drugs through CoverMyMeds or other electronic prior authorization, or ePA, tools. ***Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. OncoHealth is an independent company supporting Blue Cross Blue Shield of Michigan and Blue Care Network by providing cancer support services.
Answers to questions about changes to requirements for pain management procedures for our Medicare Advantage membersAs we communicated previously, pain management services no longer require prior authorization for Medicare Plus Blue℠ and BCN Advantage℠ members for dates of service on or after May 1, 2025. If you have questions that aren’t answered below, see the document titled Musculoskeletal procedure authorizations: Frequently asked questions for providers. Question: What pain management procedure codes no longer require prior authorization? Answer: The following pain management procedure codes no longer require prior authorization for our Medicare Advantage members:
Q: How do I update an existing TurningPoint pain management authorization for dates of service before May 1, 2025? A: Complete the Post-service change request form and fax it to TurningPoint at 313-879-5509. Note: If you already submitted a claim, click Yes for the question “Have you submitted a claim to Blue Cross or BCN?” To access the form, click the link above or:
Q: Can I request advance coverage determinations for pain management procedures for dates of service on or after May 1, 2025? A: Providers can request advance coverage determinations (also known as organization determinations) for pain management procedures for Medicare Advantage members. The steps vary depending on the member’s plan.
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Submit clinical documentation through Medical and Pharmacy Drug PA PortalHealth care providers should upload clinical documentation through the Medical and Pharmacy Drug PA Portal. This means you can attach clinical documentation when submitting prior authorization requests, rather than faxing clinical documentation separately. We recommend that you attach clinical documentation when you create the request to help reduce:
Attach clinical documentation by clicking the Select Files button (shown below) when entering request details but before completing the drug questionnaires.
The restrictions and requirements for uploading clinical documentation are listed below the Select Files button. Note: If we need additional clinical documentation to review the request, you’ll need to fax it to the Blue Cross and BCN Pharmacy Clinical Help Desk. Learn more about the Medical and Pharmacy Drug PA Portal To learn how to work in the Medical and Pharmacy Drug PA Portal, view a recorded demo by going to Blue Cross and BCN’s Provider Training site, searching drugs and launching the “Medical and Pharmacy Drug PA Portal Overview Mini Module.” The demo will guide you through using the portal. To access the provider training site:
Email ProviderTraining@bcbsm.com if you have issues accessing or navigating the site. Additional information For additional information about submitting prior authorization requests for drugs, see the following pages on ereferrals.bcbsm.com:
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Inpatient admissions for musculoskeletal procedures managed by TurningPointThe processes and requirements for inpatient admissions for musculoskeletal procedures vary depending on whether the inpatient setting is being requested before or after the procedure is performed. Before the procedure is performed If you request the inpatient setting for a musculoskeletal procedure before the procedure is performed, TurningPoint Healthcare Solutions LLC reviews the setting as part of the prior authorization request as follows:
Note: The TurningPoint medical policies are available in the TurningPoint provider portal.
Note: If an authorization for a procedure that’s on the list of inpatient-only procedures shows an outpatient setting for a Medicare Advantage member, contact TurningPoint toll-free at 1-833-217-9670 or locally at 313-908-6040 before performing the procedure. TurningPoint will update the setting on the authorization. After the procedure is performed If the member’s condition changes during the already approved outpatient stay and the member meets InterQual® guidelines for an inpatient admission, submit a prior authorization request for the inpatient stay to Blue Cross Blue Shield of Michigan or Blue Care Network through the e-referral system. Important:
Note: When entering requests for inpatient stays in the e-referral system, select “Inpatient Hospital” as the place of service, select “Direct” as the admission type and enter procedure code *99222. Additional information For additional information, see the following documents:
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Starting Oct. 6, submit prior authorization requests for FEP members through the e-referral systemStarting Oct. 6, 2025, health care providers can submit prior authorization requests for members who have coverage through the Blue Cross and Blue Shield Federal Employee Program® through the e-referral system. This change applies to procedures that are managed by Blue Cross Blue Shield of Michigan and affects FEP® members who have both commercial and Medicare Supplement plans. This change will benefit you by:
If you can’t submit prior authorization requests through the e-referral system, we’ll continue to accept prior authorization requests that are faxed to 1-866-294-5012 or sent through U.S. mail. In addition, you’ll be able to continue to check the status of prior authorization requests by calling:
Notes:
For more information about working in the e-referral system, see the e-referral User Guide. Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services. For more information, go to our ereferrals.bcbsm.com website.
Pharmacy news roundupWhat you need to know To view all — including the most recent — pharmacy-related provider alerts:
Here are links to pharmacy-related provider alerts from June:
Tip: You can also subscribe to Provider Alerts Weekly to receive a weekly email with links to the previous week’s provider alerts. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Starting Sept. 1, we’ll change how we pay for certain medications for most Blue Cross, BCN commercial membersThe table below shows the medications we won’t pay for starting Sept. 1, 2025, as well as the alternative medications we’ll pay for starting Sept. 1. These drugs are managed through the Oncology Value Management program, which is administered by OncoHealth. These changes will affect most Blue Cross Blue Shield of Michigan and Blue Care Network commercial members with pharmacy benefits. These changes won’t apply to Medicare Advantage groups or members.
**Additional coverage requirements may apply for preferred alternatives. These requirements apply to the following Blue Cross and BCN commercial members when they receive these drugs in an outpatient setting in Michigan or in other states:
We’ll send letters about these changes to affected groups, members and their health care providers. How to submit prior authorization requests Submit prior authorization requests to OncoHealth on or after Aug. 20, 2025, using one of the following methods:
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Blue Cross, along with 17 other Blue plans, works with CivicaScript® (previously Civica Rx) to manufacture low-cost generic medications to reduce members’ out-of-pocket costs and improve savings for our customers. CivicaScript® is an independent company that will provide select generic drugs to Blue Cross Blue Shield of Michigan and Blue Care Network members. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. OncoHealth is an independent company supporting Blue Cross Blue Shield of Michigan and Blue Care Network by providing cancer support services.
We’re changing how we manage self-administered hemophilia products for most Blue Cross, BCN commercial members, starting Sept. 1Starting Sept. 1, 2025, self-administered formulations of hemophilia products will no longer be payable under medical benefits for Blue Cross Blue Shield of Michigan and Blue Care Network commercial members. Instead, they’ll be payable under pharmacy benefits. This change doesn’t apply to Medicare Advantage groups or members. Some members recently received a self-administered hemophilia product that was administered by a health care provider and billed under their medical benefits. Authorizations for self-administered hemophilia products will remain in effect under medical benefits until Aug. 31, 2025. If the hemophilia product they’re taking doesn't require prior authorization under medical benefits, no prior authorization is needed to transition to pharmacy benefits. A new authorization for a self-administered hemophilia product will be approved Sept. 1, 2025, under pharmacy benefits and active through Aug. 31, 2026, so members can continue therapy without interruption. Members can fill their prescriptions at in-network retail pharmacies. On or after Sept. 1, there will be no coverage provided for any self-administered hemophilia products through medical benefits. If members don’t have prescription coverage through Blue Cross or BCN and are currently filling their prescription for these medications through their Blue Cross or BCN medical benefit, they can check to see if their pharmacy plan will cover it. How to submit prior authorization requests Submit medical and pharmacy prior authorization requests through the Medical and Pharmacy Drug PA Portal, which you can access by clicking the Medical/Pharm Drug Benefit Prior Auth (Commercial) tile under the Applications tab in our provider portal at availity.com.** You can also submit pharmacy benefit drugs prior authorization requests using CoverMyMeds® . **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||