|
October 2023

Starting Jan. 1, new cancer support program will be available for some commercial members
Blue Cross Blue Shield of Michigan and Blue Care Network are working with OncoHealth® to provide a cancer support program (Iris by OncoHealth) for adult members ages 18 and older who have a cancer diagnosis or who are cancer survivors.
Starting Jan. 1, 2024, this program will help members navigate the emotional, physical and financial challenges caused by cancer diagnosis and treatment. It also aims to lower the burden on health care providers and complement — not replace or interfere with — the care they provide. It’s meant to provide supplemental support and education between regularly scheduled, in-person appointments.
Iris by OncoHealth will be available to:
- Members who have coverage through Blue Cross and BCN commercial fully insured groups
- Commercial members who have individual coverage
- Members who have coverage through self-funded groups that purchase the program
There will be no cost to eligible members. With permission from the member, it will also be available to their caregivers.
Through the Iris mobile app or by phone, the program will include access to:
- 24/7 support from oncology nurses — Members can discuss symptoms and side effects with oncology nurses. The Iris nurses report new or worsening symptoms to the member’s primary oncology team by fax or phone. The Iris nursing team is supported by medical oncologists and advanced practice providers who are available for case escalation.
Note: The Iris nurses use OncoHealth Medical Group’s symptom management pathways to help members manage symptoms. The pathways are based on standards of care established by the National Comprehensive Cancer Network, the American Society of Clinical Oncology and the Oncology Nursing Society, adapted for use in virtual care.
Symptom management pathways won’t include prescription medications, but may include over-the-counter medications.
- Oncology-specific mental health support — Members can schedule virtual care appointments with licensed therapists. The Iris therapists offer members support for cancer-specific concerns, including adjusting to illness, coping with anxiety, depression and uncertainty, and communicating with their care teams. Members are often able to meet with a therapist within 24 to 48 hours of scheduling an appointment.
- Registered dietitian nutritionists with cancer expertise — The Iris dietitians offer personalized support to address high-impact nutritional symptoms and provide diagnosis-specific guidance related to food and nutrition.
- Peer mentors — A trained team of cancer patients, caregivers and survivors are available to support and advise members based on their own experiences navigating a cancer diagnosis.
- Customized educational information — This includes a library of clinically approved videos, articles and other self-guided content curated for each member.
- A symptom tracker — Members can report symptoms and side effects through the tracker in the mobile app. Iris nurses remotely monitor the information members enter, which enables them to intervene early when necessary.
- Advance care planning assistance
- Navigation to financial and community resources — These resources reduce barriers to care.
- Interpreters — If English isn’t the member’s first language, interpreters are available.
To learn more, view this Iris by OncoHealth video** or go to IrisOncology.com.**
OncoHealth is an independent company supporting Blue Cross Blue Shield of Michigan and Blue Care Network by providing cancer support services.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Reminder: We’re migrating Medicare Plus Blue membership to NASCO beginning in 2024
In a March 2023 Record article, we notified you that Blue Cross Blue Shield of Michigan is updating its internal processes in preparation for moving its Medicare Plus Blue℠ membership to the NASCO operating system beginning next year. The migration only affects Medicare Plus Blue provider vouchers and will take place in phases.
In January 2024, groups that are new to Medicare Plus Blue will be loaded to the operating system. Then, in January 2025, individual members and select non-key groups (smaller groups) will migrate to NASCO. In 2026, key and large groups will migrate.
The new Medicare Plus Blue provider voucher will look similar to the current Blue Cross commercial vouchers but will include a new field that indicates the provider network. The voucher will also include new columns to identify the tax ID and electronic funds transfer dates. In addition, it will have descriptions regarding the sequestration and withhold amounts in the remittance advice section.
Additional Information
When providers receive payments from the NASCO platform, the check or EFT number series on the voucher will be updated as follows:
- Paper checks — Check numbers will begin with “4;” currently they begin with “1.”
- EFT payments — Numbers will begin with “7;” currently they begin with “6.”
Also, all Medicare Advantage claims will be finalized on a Tuesday and either a check or EFT will be issued at that time. EFT funds will be received on Friday of the same week unless that day is a federal holiday.
These changes only apply to members being migrated to NASCO.
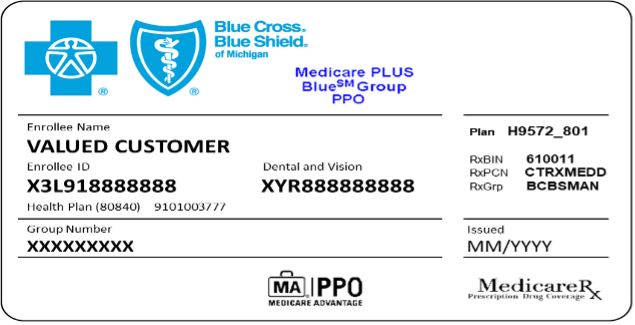
Member ID cards
We’ll also issue new Medicare Plus Blue member ID cards with a new alphanumeric prefix, deidentified ID number and nine-digit group number for those on the NASCO system. Members will receive the new cards according to their migration time frame indicated above. The image below provides an example of what the new group ID card will look like.
Example of a Medicare Plus Blue Group PPO ID card with Medicare Rx:
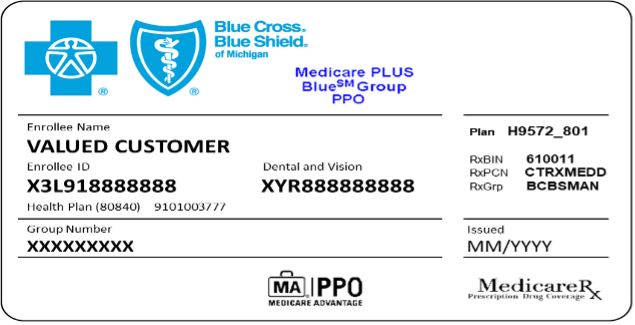
Note: Groups without prescription drug coverage won’t have the Medicare Rx symbol.
We’ll be providing more information about the migration in a future issue of The Record.
Next Drug Take Back Day scheduled for Oct. 28
The U.S. Drug Enforcement Agency’s next National Prescription Drug Take Back Day is from 10 a.m. to 2 p.m. Oct. 28. These twice-yearly events (held in April and October) provide your patients with a safe, convenient and responsible way to dispose of prescription drugs. They also help educate people about the potential for abuse of medications, including opioids.
At the most recent Drug Take Back Day in April, communities across the country removed nearly 664,000 pounds of unneeded prescriptions to help prevent drug misuse.
Resources
Blue Cross Blue Shield of Michigan supports Drug Take Back events as part of its ongoing efforts to combat the opioid epidemic. We offer a range of materials you can share with your patients and employees. For example:
- Our Opioid Resources Employer Toolkit contains an opioid resources guide and educational materials on topics such as how to safely store and dispose of medicine.
- Our Opioids website provides information about the opioid epidemic, opioid dependence and using opioids safely.
- We’ll publish a blog on mibluesperspectives.com in October.
Finding a drug disposal facility
Let your patients know they can find a drug disposal facility near them by checking out the DEA’s search tool.** For more information on Drug Take Back Day or the appropriate disposal of prescription drugs, visit the DEA Diversion Control Division website.**
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
We’re working to create awareness of fraudulent schemes and resources to report fraud
Our Corporate and Financial Investigations Unit conducts an annual fraud awareness campaign for employees each October — and this year, the unit is broadening its approach by reaching out to members and health care providers as well.
The goal of the campaign is to create awareness of fraud schemes and educate all stakeholders on how to recognize and report potential fraud, waste and abuse. Both our members and participating providers may become victims of fraud. For example, a member’s medical records may be affected by fraudulent claims activity.
DME fraud
One of the largest health care fraud schemes of the past year involves durable medical equipment fraud, costing the health care industry tens of millions of dollars a year. Since providers can be a victim of DME fraud, we reach out to providers whose NPIs are used without their knowledge. Providers may be approving DME without knowing the true cost charged to private insurers by DME companies.
“This is just one of the many ways we’re working to protect providers from becoming a victim of this and other fraud schemes,” said Daniel Crowell, senior director, Corporate and Financial Investigations.
Here’s an important guideline to keep in mind:
- DME is best suited for in-person visits, where devices can be properly fitted and assessed by the member’s provider.
Risk to members
Telemarketers sometimes market “free” DME to members, which results in high costs to insurers. Our Medicare members can be particularly susceptible to these schemes. Fraudulent telemarketers may reach out to seniors, intentionally confuse them and then get Medicare to pay for equipment that isn’t actually vetted by a medical professional.
Resources
- Contact CFI if you have concerns or recognize possible fraudulent activity. Call 1-844-STOP-FWA (1-844-786-7392) or send an email to StopFraud@bcbsm.com.
- Check out the Victimized Provider Project section** of the Centers for Medicare & Medicaid Services' website. The Victimized Provider Project helps keep providers from being held liable for overpayment for claims paid that are the result of identity theft.
By working together, we can help eliminate fraud, an effort that will improve patient safety and reduce costs.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
CPT 3rd-quarter update: New and deleted codes
Laboratory and Pathology/Proprietary Laboratory Analyses
Code |
Change |
Coverage comments |
Effective date |
*0066U |
Deleted |
Deleted Sept. 30, 2023 |
Sept. 30, 2023 |
*0357U |
Deleted |
Deleted Sept. 30, 2023 |
Sept. 30, 2023 |
*0386U |
Deleted |
Deleted Sept. 30, 2023 |
Sept. 30, 2023 |
*0397U |
Deleted |
Deleted Sept. 30, 2023 |
Sept. 30, 2023 |
*0402U |
Added |
Not covered |
Oct. 1, 2023 |
*0403U |
Added |
Not covered |
Oct. 1, 2023 |
*0404U |
Added |
Not covered |
Oct. 1, 2023 |
*0405U |
Added |
Not covered |
Oct. 1, 2023 |
*0406U |
Added |
Not covered |
Oct. 1, 2023 |
*0407U |
Added |
Not covered |
Oct. 1, 2023 |
*0408U |
Added |
Not covered |
Oct. 1, 2023 |
*0409U |
Added |
Not covered |
Oct. 1, 2023 |
*0410U |
Added |
Not covered |
Oct. 1, 2023 |
*0411U |
Added |
Not covered |
Oct. 1, 2023 |
*0412U |
Added |
Not covered |
Oct. 1, 2023 |
*0413U |
Added |
Not covered |
Oct. 1, 2023 |
*0414U |
Added |
Not covered |
Oct. 1, 2023 |
*0415U |
Added |
Not covered |
Oct. 1, 2023 |
*0416U |
Added |
Not covered |
Oct. 1, 2023 |
*0417U |
Added |
Not covered |
Oct. 1, 2023 |
*0418U |
Added |
Not covered |
Oct. 1, 2023 |
*0419U |
Added |
Not covered |
Oct. 1, 2023 |
Pathology and Laboratory/MAAA Administrative Code
Code |
Change |
Coverage comments |
Effective date |
*0019M |
Added |
Not covered |
Oct. 1, 2023 |
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
CPT code update: New immunization vaccine codes
Medicine Vaccines/Toxoids
Code |
Change |
Coverage comments |
Effective date |
*90589 |
Added |
Not covered |
Jan. 1, 2024 |
*90623 |
Added |
Not covered |
Jan. 1, 2024 |
*90683 |
Added |
Not covered |
Jan. 1, 2024 |
*90380 |
Added |
Payable |
July 17, 2023 |
*90381 |
Added |
Payable |
July 17, 2023 |
*90679 |
Added |
Payable |
May 3, 2023 |
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
HCPCS update: New code
The Centers for Medicare & Medicaid Services has added a new code as part of its Health Care Procedure Coding System update. The code, effective date and Blue Cross Blue Shield of Michigan’s coverage decision are below.
Injections
Code |
Change |
Coverage comments |
Effective date |
J0174 |
Added |
Not covered |
July 6, 2023 |
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
HCPCS replacement codes, effective July 6, 2023, established
J0174 replaces C9399 J3490, J3590 and J9999 when billing for Leqembi (lecanemab-irmb)
Effective July 6, 2023, the Centers for Medicare & Medicaid Services established a permanent procedure code for the specialty medical drug Leqembi (lecanemab-irmb).
Report all services through July 5, 2023, with J3490, J3590, C9399 and J9999. All services performed on and after July 6, 2023, must be reported with J0174.
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Billing chart: Blue Cross highlights medical, benefit policy changes
You’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart.
This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures.
We'll publish information about new Blue Cross groups or changes to group benefits under the Group Benefit Changes heading.
For more detailed descriptions of the Blue Cross' policies for these procedures, check under the Commercial Policy tab in Benefit Explainer on Availity®. To access this online information:
1. Log in to availity.com.
2 .Click on Payer Spaces on the Availity menu bar.
3. Click on the BCBSM and BCN logo.
4. Click on Benefit Explainer on the Applications tab.
5. Click on the Commercial Policy tab.
6. Click on Topic.
7. Under Topic Criteria, click on the circle for Unique Identifier and click the drop-down arrow next to Choose Identifier Type, then click on HCPCS Code.
8. Enter the procedure code.
9. Click on Finish.
10. Click on Search.
| Code* |
BCBSM changes to:
Basic Benefit and Medical Policy, Group
Variations Payment Policy, Guidelines
|
| POLICY CLARIFICATIONS |
Established
15822, 15823, 67900, 67901, 67902, 67903, 67904, 67906, 67908
Experimental
15820, 15821 |
Basic benefit and medical policy
Blepharoplasty and brow ptosis repair
Blepharoplasty procedures of the upper eyelid and repair of brow ptosis are safe and effective restorative procedures when performed to correct:
- Visual impairment due to dermatochalasis, blepharochalasis or blepharoptosis
- Symptomatic redundant skin weighing down on upper lashes
- Prosthetic difficulties in an anophthalmic socket
- Blepharospasm unresponsive to conservative treatment
Blepharoplasties of the lower lid are considered primarily cosmetic in nature. This service is usually performed to improve appearance or self-esteem, not to treat a specific disease state or improve function.
Inclusionary criteria have been updated, effective Sept. 1, 2023.
Inclusions:
Criteria for blepharoplasty:
This procedure is considered reconstructive and not cosmetic when one of the following solid bullets are met:
- Visual field measurement is obtainable and all the following are met:
- There is a difference of 12 degrees or more or at least 30% superior visual field difference is demonstrated between visual field testing before and after manual elevation of the upper eyelids
- The medical record should include visual field testing reports in both taped and untaped positions. Photographs should be maintained as part of the medical record, including photographs demonstrating the head held in an erect position with eyes open and focused straight ahead. Views should reveal the full-face anterior position, as well as the right and left lateral views with a straightforward gaze.
- Visual field measurement isn’t obtainable and all the following are met:
- Infants and children whose blepharoptosis is severe enough to cause a functional visual impairment.
- While it may not be possible to obtain visual field measurements, documentation and photographs reflective of the lid obstruction should be maintained as part of the medical record.
- To relieve eye symptoms associated with blepharospasm when other treatments have failed or are contraindicated (such as an injection of Botulinum Toxin A).
- Correction of an anophthalmic socket when one of the following are met:
- There is documented difficulties with a prosthesis due to lid position.
- A margin reflex distance of 2.5 mm or less.
- A palpebral fissure height on down-gaze of 1 mm or less.
Criteria for repair of brow ptosis (browplasty) and blepharoptosis:
This procedure is considered reconstructive and not cosmetic if all the following criteria are met:
- There is a difference of 12 degrees or more or at least 30% superior visual field difference is demonstrated between visual field testing before and after manual elevation of the upper eyelids.
- The medical record should include visual fieldtesting reports in both taped and untaped positions. Photographs should be maintained as part of the medical record. Views should reveal the full-face anterior position, as well as the right and left lateral views with a straightforward gaze.
Clinical review of these procedures is usually required. Providers should consult the plan to determine whether photographs should be forwarded with the request. Photos should be maintained in the record in the event they’re requested for later review.
Exclusions:
- Lower lid blepharoplasty is considered cosmetic.
- Blepharoplasty/ptosis repair or brow lift surgery to improve the appearance when no functional impairment exists is considered cosmetic.
|
20930, 20931, 20936, 20937, 20938, 20939 |
Basic benefit and medical policy
Bone graft substitutes
The use of bone grafts/substitutes is considered established for the promotion of bone healing when medical criteria is met, effective Sept. 1, 2023.
Inclusions:
The use of bone grafts/substitutes that are listed below are considered established for the promotion of bone healing when all the following are met:
- Graft is used according to FDA-approved (on-label) indications and contraindications, where applicable.
- Graft is used alone or in combination with another acceptable graft (an osteoconductive allograft with an osteoinductive allograft). Up to one type of osteoconductive allograft or one type of osteoinductive allograft is used per surgical incident.
- Recognizing that there are clinical scenarios where more product may be necessary, the amount of allograft is determined by the surgeon based on multiple factors including the number of levels fused, size of the patient, volume and quality of local bone or iliac crest bone harvested, and pseudoarthrosis risk.
- Bone substitute graft isn’t being used to backfill or reconstruct the donor site.
- The surgical plan or operative note (whichever is applicable) should identify the graft manufacturer, product name and amount or size of graft planned/used.
Where applicable, only grafts with FDA approval are considered medically necessary. The following are considered acceptable grafts:
- Autograft (preferred option: considered gold standard in bone healing enhancement)
- Allograft — morselized or structural
- Demineralized bone matrix, or DBM
- Calcium based synthetics:
- Beta-tricalcium phosphate
- Hydroxyapatite
- Calcium phosphate
- Calcium sulfate
- Bone marrow aspirate (not concentrated) combined with any other acceptable graft
- Bone morphogenic protein-rhBMP-2 (Infuse). See the JUMP Policy Bone Morphogenetic Protein.
- Peptide-15 (i-Factor) when all the following are met:
- Single level anterior cervical discectomy and fusion between C3 and C7 in a skeletally mature patients who meet criteria for cervical fusion
- Must be used in combination with a cortical ring allograft and anterior plate fixation
Note: Processed allograft substitutes must have meaningful human-based studies to be considered for approval.
Exclusions:
Due to lack of sufficient evidence to establish safety and efficacy, the following are considered experimental and not medically necessary:
- Cell-based substitute grafts
- Non-calcium-based synthetics:
- Bioactive glass
- Synthetic polymers, e.g., Cortoss (PMMA)
- Concentrated bone marrow aspirate
- Platelet rich plasma
- Human amniotic tissue
- Nano-crystalline surface-modified synthetics
Note: Exceptions may be made on a case-by-case basis for those who are unable to accept human tissue grafts, due to ethical or religious reasons, when autograft isn’t a viable option.
|
30469
|
Basic benefit and medical policy
Low-dose radiofrequency for nasal valve
Low-dose, temperature-controlled radiofrequency intranasal tissue remodeling as a treatment of nasal airway obstruction is considered experimental. The positive affect on clinical outcomes hasn’t been definitively demonstrated, effective Sept. 1, 2023.
Inclusionary and exclusionary guidelines:
Not applicable |
31647, 31648, 31649, 31651 |
Basic benefit and medical policy
Bronchial valves
The insertion of endobronchial valves is established in adult individuals with respiratory compromise from hyperinflation associated with severe heterogeneous lung emphysema with little to no collateral ventilation.
The insertion of endobronchial valves is established for persistent bronchopleural air leak causing pneumothorax that isn’t improving in five or more days after chest tube insertion.
The medical policy statement and inclusionary and exclusionary criteria have been updated, effective Sept. 1, 2023.
Inclusionary and exclusionary guidelines:
This procedure should be performed at a facility with the ability to admit. Admission should be based on perceived risks or complications.
Criteria for pleural air leak
Bronchopleural air leak not improving five or more days after chest tube placement, when the site of air leak can be identified by balloon occlusion of the distal affected bronchus.
Criteria for emphysema
Respiratory insufficiency caused by bullous emphysema in an individual found, after multidisciplinary evaluation, not to be a candidate for lung volume reduction surgery.
Inclusions:
- Ex-smokers
- PFT**
- Post BD** FEV1** 15-45%
- TLC** ≥100%
- RV** ≥150%
- ABG** with pCO2 <60
- Completed pulmonary rehabilitation program or enrollment in a pulmonary rehabilitation program of at least six to eight sessions or attestation from a physician that the patient has received adequate pulmonary rehabilitation to proceed with surgery
- CT imaging confirming intact fissure between lobes
Exclusions:
- Any general contraindications to bronchoscopy or general anesthesia
- Lung findings:
- Pulmonary nodule requiring work up
- Giant bullae (>1/3 hemithorax)
- Cardiovascular event (e.g., myocardial infarction or heart failure) in the prior six months
- Recent CVA**/stroke (three months)
- Evidence of uncontrolled pulmonary hypertension with systolic PAP >45 mmHg on TEE**
**PFT stands for pulmonary function test; BD stands for bronchodilator; FEV1 is forced expiratory volume at 1 second; TLC is total lung capacity; RV is right ventricular; ABG is arterial blood gas; PAH is pulmonary arterial hypertension; PAP is pulmonary artery pressure; CV is cardiovascular; CVA is cerebral vascular accident; TEE is transthoracic echocardiography. |
38204,38205, 38206, 38207, 38208, 38209, 38210, 38211, 38212, 38213, 38214, 38215, 38230, 38232, 38240, 38241, 38242, 38243, 81265, 81266, 81267, 81268, 81370, 81371, 81372, 81373, 81374, 81375, 81376, 81377, 81378, 81379, 81380, 81381, 81382, 81383, 86812, 86813, 86816, 86817, 86821, S2140, S2142, S2150 |
Basic benefit and medical policy
HCT for acute lymphoblastic leukemia
The safety and effectiveness of hematopoietic cell transplantation for acute lymphoblastic leukemia have been established. It may be considered a useful therapeutic option for individuals who meet specific selection criteria.
Inclusionary criteria have been clarified, effective Sept. 1, 2023.
Inclusionary and exclusionary guidelines:
Childhood acute lymphoblastic leukemia
Inclusions:
- Autologous or allogeneic hematopoietic cell transplantation to treat childhood acute lymphoblastic leukemia, or ALL, in first complete remissiona but at high riskb of relapse.
- Autologous or allogeneic cell transplantation to treat childhood ALL in second or greater remission or refractory ALL.
- Allogeneic hematopoietic cell transplantation to treat relapsing ALL after a prior autologous HCT.
- Reduced-intensity conditioning allogeneic hematopoietic cell transplantation as a treatment of ALL in children who are in completea first or second remission and who, for medical reasons, would be unable to tolerate a standard myeloablative conditioning regimen.
aDefined by bone marrow biopsy/aspirate demonstrating < 5% blasts
bChildhood high risk factors for relapse
Adverse prognostic factors and factors associated with high risk of relapse in children include the following:
- Age younger than 1 year or older than 9
- White blood cell count at presentation above 50,000/μL
- Hypodiploidy (<45 chromosomes)
- Translocation involving chromosomes 9 and 22 (t[9;22]), also known as BCR-ABL fusion
- Translocation involving chromosomes 4 and 11 (t[4;11]) aka MLL-AF4 fusion
- Pre-B or T-lineage immunophenotype
- Central nervous system involvement
- Poor response to initial therapy including poor response to prednisone prophase
- Poor treatment response to induction therapy at six weeks with high-risk having ≥ 0.01% minimal residual disease measured by flow cytometry
Exclusions:
- All other conditions not listed above
Adult acute lymphoblastic leukemia
Inclusions:
- Autologous hematopoietic cell transplantation to treat adult ALL in first complete remissiona but at high riskb of relapse
- Allogeneic hematopoietic cell transplantation to treat adult ALL in first complete remissiona for any risk level
- Allogeneic hematopoietic cell transplantation to treat adult ALL in second or greater remissions, or in adults with relapsed or refractory ALL
- Allogeneic hematopoietic cell transplantation to treat relapsing ALL after a prior autologous HCT
- Reduced-intensity conditioning allogeneic hematopoietic cell transplantation as a treatment of ALL in adults who are in completea first or second remission and who, for medical reasons, would be unable to tolerate a standard myeloablative conditioning regimen
aDefined by bone marrow biopsy/aspirate demonstrating < 5% blasts
bAdult high risk factors for relapse
Individual with any of the following may be considered at high-risk for relapse:
- Older than 35 years
- Leukocytosis at presentation of greater than 30,000/μl (B-cell lineage) or greater than 10,000/μl (T-cell lineage)
- “Poor prognosis” genetic abnormalities like the Philadelphia chromosome (t[9;22])
- Extramedullary disease
- Time to attain complete remission longer than four weeks
Exclusions:
- Autologous hematopoietic cell transplantation to treat adult ALL in second or greater remission or those with refractory disease
|
38204,38205, 38206, 38207, 38208, 38209, 38210, 38211, 38212, 38213, 38214, 38215, 38230, 38232, 38240, 38241, 38242, 38243, 81265, 81266, 81267, 81268, 81370, 81371, 81372, 81373, 81374, 81375, 81376, 81377, 81378, 81379, 81380, 81381, 81382, 81383, 86812, 86813, 86816, 86817, 86821, S2140, S2142, S2150 |
Basic benefit and medical policy
HCT for myelodysplastic syndromes and myeloproliferative neoplasms
The safety and effectiveness of allogeneic hematopoietic cell transplantation have been established as a treatment of myelodysplastic syndromes or myeloproliferative neoplasms. It’s a useful therapeutic option for individuals meeting selection criteria. Inclusionary criteria have been updated, effective Sept. 1, 2023.
Inclusions:
Allogeneica HCT may be considered established as a treatment for one of the following:
- Myelodysplastic syndromes
- Myeloproliferative neoplasms
aIncludes myeloablative, reduced-intensity conditioning and nonmyeloablative regimens
Exclusions:
Individuals not meeting the above diagnostic criteria |
38204, 38205, 38207, 38208, 38209, 38210, 38211, 38212, 38213, 38214, 38215, 38230, 38240, 38242, 38243, 81267, 81268, 81370, 81371, 81372, 81373, 81374, 81375, 81376, 81377, 81378, 81379, 81380, 81381, 81382, 81383, 86812, 86813, 86816, 86817, 86821, S2140, S2142, S2150 |
Basic benefit and medical policy BMT – HCT for genetic diseases and acquired anemias, allogeneic
The safety and effectiveness of allogeneic hematopoietic cell transplantation for specified genetic diseases and acquired anemias have been established. It may be considered a useful therapeutic or diagnostic option when indicated.
Inclusionary and exclusionary criteria have been updated, effective Sept. 1, 2023.
Inclusions:
Allogeneic hematopoietic cell transplantation is considered established for select individuals as listed below.
The conditioning regimens for the following diseases may include myeloablative conditioning, reduced intensity conditioning or non-myeloablative conditioning as determined by the treating provider/transplant center.
Hemoglobinopathies
- Sickle cell anemia for children or young adults
- Homozygous beta-thalassemia (i.e., thalassemia major)
Bone marrow failure syndromes
- Aplastic anemia including hereditary (including Fanconi anemia, dyskeratosis congenita, Shwachman-Diamond syndrome, Diamond-Blackfan syndrome) or acquired (e.g., secondary to drug or toxin exposure) forms.
Primary immunodeficiencies
- Absent or defective T-cell function
- Absent or defective natural killer function
- Absent or defective neutrophil function
The following diseases are examples of the above:
- Lymphocyte Immunodeficiencies
- Adenosine deaminase deficiency
- Artemis deficiency
- Calcium channel deficiency
- CD 40 ligand deficiency
- Cernunnos/X-linked lymphoproliferative disease deficiency
- CHARGE syndrome with immune deficiency
- Common gamma chain deficiency
- Deficiencies in CD45, CD3, CD8
- DiGeorge syndrome
- DNA ligase IV deficiency syndrome
- Interleukin-7 receptor alpha deficiency
- Janus-associated kinase 3 deficiency
- Major histocompatibility class II deficiency
- Omenn syndrome
- Purine nucleoside phosphorylase deficiency
- Recombinase-activating gene 1/2 deficiency
- Reticular dysgenesis
- Severe combined immunodeficiency
- Winged helix deficiency
- Wiskott-Aldrich syndrome
- X-linked lymphoproliferative disease
- Zeta-chain-associated protein-70 deficiency
- Phagocytic deficiencies
- Chédiak-Higashi syndrome
- Chronic granulomatous disease
- Griscelli syndrome, type 2
- Hemophagocytic lymphohistiocytosis
- Interferon-gamma receptor deficiencies
- Kostmann syndrome
- Leukocyte adhesion deficiency
- Severe congenital neutropenias
- Shwachman-Diamond syndrome
- Other immunodeficiencies
- Autoimmune lymphoproliferative syndrome
- Cartilage hair hypoplasia
- CD25 deficiency
- Hyper IgD and IgE syndromes
- Immunodeficiency, centromeric instability, and facial dysmorphism syndrome
- Immunodysregulation polyendocrinopathy enteropathy X-linked syndrome
- Nuclear factor-κ B (NF-κB) essential modulator deficiency
- NF-κB inhibitor, NF-κB-α deficiency
- Nijmegen breakage syndrome
Inherited metabolic disease
- Lysosomal and peroxisomal storage disorders except for Hunter, Sanfilippo and Morquio syndromes
The following diseases are examples of the above:
- Hurler
- Maroteaux-Lamy
- Sly syndromes
- Childhood onset cerebral X-linked adrenoleukodystrophy
- Globoid-cell leukodystrophy
- Metachromatic leukodystrophy
- Alpha-mannosidosis
- Aspartylglucosaminuria
- Fucosidosis
- Gaucher types 1 and 3
- Farber lipogranulomatosis
- Galactosialidosis
- GM1
- Gangliosidosis
- Mucolipidosis II (I-cell disease)
- Multiple sulfatase deficiency
- Niemann-Pick
- Neuronal ceroid lipofuscinosis
- Sialidosis
- Wolman disease
Genetic disorders affecting skeletal tissue
- Infantile malignant osteopetrosis (Albers-Schönberg disease or marble bone disease)
Exclusions:
Allogeneic HCT hasn’t been effective in treating:
- Hunter syndrome
- Sanfilippo syndrome
- Morquio syndrome
|
38206, 38207, 38210, 38211, 38212, 38213, 38214, 38215, 38232, 38241, S2150
Experimental
38204, 38205, 38207, 38208, 38209, 38210, 38211, 38212, 38213, 38214, 38215, 38230, 38240, 38242, 38243, 81267, 81268, 81370, 81371, 81372, 81373, 81374, 81375, 81376, 81377, 81378, 81379, 81380, 81381, 81382, 81383, 86812, 86813, 86816, 86817, 86821, S2140, S2142, S2150 |
Basic benefit and medical policy
BMT – HCT for cns and embryonal tumors and ependymoma
Embryonal tumors of the CNS
The safety and effectiveness of specified autologous hematopoietic cell transplants for embryonal tumors of the central nervous system have been established. It may be considered a useful therapeutic tool when indicated for individuals who meet specific selection criteria.
Ependymoma
Autologous, tandem autologous and allogeneic hematopoietic cell transplants are experimental for the treatment of ependymoma. They haven’t been scientifically demonstrated to improve clinical outcomes better than conventional treatment.
Triple tandem transplant
The effectiveness and clinical utility of an autologous triple tandem stem cell transplant have been established. It’s a useful therapeutic option for individuals with pediatric CNS tumors who meet specific selection criteria.
Inclusionary criteria have been updated, effective Sept. 1, 2023.
Inclusions:
The conditioning regimens for the following diseases may include myeloablative conditioning, reduced intensity conditioning or non-myeloablative conditioning as determined by the treating provider/transplant center.
Embryonal tumors and choroid plexus tumors of the CNS
Inclusions:
- Autologous hematopoietic cell transplantation for the initial treatment of (newly diagnosed) embryonala tumors of the central nervous system, or CNS, that show partial or complete response to induction chemotherapy, or stable disease after induction therapy
- Autologous hematopoietic cell transplantation for the treatment of recurrent embryonala tumors of the CNS
- Triple tandem autologous hematopoietic cell transplant for the treatment of embryonala or choroid plexus tumors when both of the following are met:
- Procedure may lead to reduced toxicities or less risk to future neurocognition
- Other established treatments, such as single autologous transplant, have been deemed too risky
aEmbryonal tumors of the CNS include medulloblastoma, medulloepithelioma, supratentorial PNETs (pineoblastoma, cerebral neuroblastoma, ganglioneuroblastoma), ependymoblastoma, atypical teratoid/rhabdoid tumors and embryonal tumor with multilayered rosettes.
Exclusions:
- Allogeneic hematopoietic cell transplantation for the treatment of embryonal or choroid plexus tumors of the CNS.
Ependymoma
Inclusions:
Not applicable
Exclusions:
- Autologous, tandem autologous and tandem allogeneic hematopoietic cell transplants are experimental for the treatment of ependymoma.
|
58679, 58825, 58970, 58974, 76948, 89250, 89254, 89258, 89259, 89268, 89335, 89337, 89342, 89343, 89346, 89352, 89353, 89356
Experimental
89398, 89344, 89354, 89335
|
Basic benefit and medical policy Infertility related to cancer treatment
Preservation of fertility (including collection of oocytes and spermatozoa; cryopreservation, storage and thawing of embryos, oocytes and spermatozoa) may be considered established for individuals diagnosed with cancer and at risk for treatment-related infertility when criteria are met.
Inclusionary and exclusionary criteria have been updated, effective Sept. 1, 2023.
Inclusions:
- Preservation of fertility in a post-pubertal biological female or a post-pubertal biological male may be considered established when:
- The individual is diagnosed with cancer, and the cancer treatment will result in irreversible infertility, such as with:
- Gonadotoxic chemotherapy
- Radiation therapy of the pelvis, lower abdomen or total body
- Surgical removal of ovaries or testicles
Procedures that may be considered established in fertility preservation:
- Collection of mature oocytes and spermatozoa
- Cryopreservation of embryos, mature oocytes and spermatozoa
- Storage of embryos, mature oocytes and spermatozoa for up to two years
- Thawing of embryos, mature oocytes and spermatozoa within two years of the procurement
- Culture of oocytes
- Ovarian transposition (in anticipation of pelvic or lower abdominal radiation)
- Embryo transfer, back to the member, within two years from cryopreservation
Exclusions:
- Storage of sperm, oocytes or embryos for longer than two years
- Co-culture of embryos
- Post-menopausal females
- Individuals who have undergone elective sterilization (vasectomy, tubal sterilization), with or without reversal
- Request for fertility preservation that doesn’t meet inclusion criteria
- Other assisted reproductive techniques, unless the member has additional benefit coverage for these services.
- Cryopreservation of ovarian tissue, immature oocytes and testicular tissue in post-pubertal biological males
- Cryopreservation of testicular tissue in pre-pubertal biologic males
|
61885, 61886, 61888 |
Basic benefit and medical policy
Codes *61885, *61886 and *61888
Procedure codes *61885, *61886 and *61888 are payable in the inpatient, outpatient and ambulatory surgery center locations only. |
80145, 80230, 80280, 80299,** 83520**
Experimental
84999**
**Unlisted procedure codes |
Basic benefit and medical policy
Measurement of serum and anti-drug antibody levels
Measurement of biologic agent drug levels and, if low, anti-drug antibody levels in individuals with inflammatory bowel disease, or IBD, is established.
Measurement of antidrug antibodies in other individuals being treated with a biologic agent, either alone or as a combination test, which includes the measurement of serum TNF blocking agent levels, is considered experimental. The use of these tests hasn’t been clinically proven to improve patient clinical outcomes or alter patient management.
The medical policy statement and inclusionary and exclusionary criteria have been updated, effective Sept. 1, 2023.
Inclusions:
Biologic agent drug levels are established in individuals who meet all the following:
- Diagnosed with inflammatory bowel disease
- Being treated with either Adalimumab, Infliximab, Ustekinumab and Vedolizumab
- Being monitored for their response to the agent by biologic agent drug level
If the biologic agent drug level is below the therapeutic range, testing for the anti-drug antibody level is established.
Exclusions:
- Any condition other than inflammatory bowel disease
|
81376, 81377, 81382, 81383 |
Basic benefit and medical policy
HLA testing for celiac disease
The effectiveness and clinical utility of human leukocyte antigen, or HLA, -DQ2 and HLA-DQ8 testing to rule out a diagnosis of celiac disease have been established. It may be considered a useful diagnostic option when indicated. Inclusionary criteria have been updated, effective Sept. 1, 2023.
Inclusions:
HLA-DQ2 and HLA-DQ8 testing to rule out celiac disease may be considered medically necessary when one of the following are met:
- Individuals with persistent symptoms despite negative serology (IgA tissue contaminants) and histology (biopsy)
- Symptomatic individuals with discordant serologic and histologic (biopsy) findings
- Symptomatic individuals with positive serology who are unable to undergo biopsy evaluation
Exclusions:
- Familial testing of asymptomatic family members of individuals with proven disease
- All other situations
|
81513, 81514, 87510- 87512, 87480- 87482, 87660, 87661
Experimental:
0352U |
Basic benefit and medical policy Testing for diagnosis of vaginitis
Nucleic acid amplification test or polymerase chain reaction, known as PCR, testing and multitarget PCR testing, when limited to known pathogenic species, is considered established for the diagnosis of vaginitis (BV, candidiasis, trichomonas) in symptomatic individuals, effective Sept. 1, 2023.
Inclusions:
The following are considered established for the management of vaginitis:
- Nucleic acid amplification test or PCR testing and multitarget PCR testing, when limited to known pathogenic species, is considered established for the diagnosis of vaginitis (BV, candidiasis, trichomonas) in symptomatic individuals.
Exclusions:
- All other tests for vaginitis not addressed above are considered experimental.
|
Established
82523, 83500, 83505, 83937, 84078, 84080**
**There is no specific CPT code for bone-specific alkaline phosphatase, or ALK, but several laboratories’ websites identify CPT *84080 |
Basic benefit and medical policy
Bone turnover markers for osteoporosis and other high bone turnover diseases
The safety and effectiveness of the measurement of alkaline phosphatase isoenzymes have been established. It’s a useful option for the diagnosis and monitoring of diseases of the bone, liver and endocrine system.
The measurement of bone turnover markers has been established in certain situations in individuals with osteoporosis.
The measurement of bone turnover marker levels has been established. It’s a useful diagnostic option for the initial diagnosis and subsequent monitoring of individuals with Paget’s disease of the bone.
The measurement of bone turnover markers is considered experimental in the diagnosis and management of individuals with all other conditions associated with high rates of bone turnover including, but not limited to, primary hyperparathyroidism and renal osteodystrophy. The peer-reviewed medical literature hasn’t demonstrated the clinical utility of these laboratory tests of bone turnover for improving patient clinical outcomes.
High-power laser therapy (nonsurgical laser) is considered experimental because evidence is insufficient to determine that the technology results in an improvement in the net health outcome.
The medical policy statement and inclusionary and exclusionary criteria have been updated, effective Sept. 1, 2023.
Inclusions:
Measurement of bone turnover markers** for individuals with osteoporosis when one of the following is present:
- Initial evaluation of osteoporosis
- Management of individuals with osteoporosis
- Determine fracture risk prediction in individuals with osteoporosis
- In individuals treated with bisphosphonates for assessment of patient compliance with bisphosphonate therapy
Measurement of bone turnover markers** in individuals with Paget’s disease of the bone when one of the following is present:
- Initial diagnosis of Paget’s disease
- Subsequent monitoring and management of patients with Paget’s disease of the bone
**Bone turnover markers include (Rosen, 2018, 2019a, 2019b; Talwar, 2020):
- Bone formation markers
- Serum bone – specific alkaline phosphatase, or BSAP/BALP
- Serum osteocalcin, or OC
- Serum type 1 procollagen (C-terminal/N-terminal): C1NP or P1NP
- Bone resorption markers
- Urinary hydroxyproline, or HYP
- Urinary total pyridinoline, or PYD
- Urinary free deoxypyridinoline, or DPD
- Urinary or serum collagen type 1 cross-linked N-telopeptide, or NTX
- Urinary or serum collagen type 1 cross-linked C-telopeptide, or CTX
- Bone sialoprotein, or BSP
- Serum Tartrate-resistant acid phosphatase 5b, or TRACP5b
- Cathepsin K
Exclusions:
- Measurement of bone turnover markers as a diagnostic test for osteoporosis
- Measurement of bone turnover markers for teriparatide treatment monitoring in individuals with osteoporosis
- Measurement of bone turnover markers in the diagnosis and management of all other conditions associated with high bone turnover including, but not limited to, individuals with primary hyperparathyroidism and renal osteodystrophy.
|
89253 |
Basic benefit and medical policy *89253 removed from Physician Office Laboratory List
Procedure code *89253 was removed from the Physician Office Laboratory List. This procedure can no longer be performed in a physician’s office. |
93797, 93798
Not covered:
S9472 |
Basic benefit and medical policy Cardiac rehabilitation
Short-term outpatient Phase II cardiac rehabilitation is established as safe and effective and is an accepted standard therapy in patients with a history of specific cardiac conditions or procedures.
Cardiac rehabilitation must be a physician-supervised program that furnishes a prescribed exercise program, cardiac risk factor modification that includes education, counseling and behavioral intervention as well as psychosocial assessment and outcomes assessment.
Exclusionary criteria have been updated, effective Sept. 1, 2023.
Inclusions (must meet all):
- Phase II cardiac rehabilitation
- Member must be medically stable and able to tolerate exercise for 20 to 40 minutes.
- Must have a least one diagnosis (documented within the last 12 months) listed below:
- Acute myocardial infarction
- Coronary artery bypass graft surgery
- Current stable angina pectoris
- Percutaneous transluminal coronary angioplasty or coronary stenting
- Heart valve surgery
- Heart or heart-lung transplant
- Stable, chronic heart failure
Exclusions:
- Phase III cardiac rehabilitation
- Phase IV cardiac rehabilitation
- Doesn’t meet diagnostic criteria
- Repeat participation in a cardiac rehabilitation program in the absence of another qualifying cardiac event
- Intensive cardiac rehabilitation (Refer to medical policy, “Intensive Cardiac Rehabilitation”)
- Virtual cardiac rehabilitation is considered investigational.
|
97129, 97130 |
Basic benefit and medical policy
Cognitive rehabilitation
The safety and effectiveness of cognitive rehabilitation (as a distinct and definable component of the rehabilitation process) have been established. It may be considered a useful therapeutic option in the rehabilitation of patients meeting specific selection criteria.
Exclusionary criteria have been updated, effective Sept. 1, 2023.
Group variations:
Be sure to check individual contract, certificate and rider for specific coverage information.
Inclusions:
Cognitive rehabilitation is an established procedure when used as an adjunctive treatment of cognitive deficits (e.g., attention, language, memory, reasoning, executive functions, problem-solving and visual processing) when all the following criteria are met:
- The cognitive deficits have been acquired as a result of neurologic impairment due to traumatic brain injury or stroke.
- Services must be provided by a qualified licensed professional and must be prescribed by the attending physician as part of the written care plan.
- There must be documentation of potential for improvements based on the patient’s pre-injury function.
- Patients must be able to actively participate in the program. The patient must have sufficient cognitive function to understand and participate in the program as well as adequate language expression and comprehension (e.g., the patient shouldn’t have severe aphasia).
The member is expected to make significant cognitive improvement (e.g., the member isn’t in a vegetative or custodial state).
Exclusions:
Excluded diagnoses include, but aren’t limited to:
- Mental retardation
- Multiple sclerosis
- Cerebral palsy
- Encephalopathy
- S/P brain surgery
- Dementia (e.g., from Alzheimer’s disease, HIV-infection or Parkinson’s disease)
- Cognitive decline chronic obstructive pulmonary disease
- Behavioral or psychiatric disorders such as attention-deficit/hyperactivity disorder and schizophrenia
- Pervasive developmental disorders
- Post-acute cognitive sequelae of SARS-CoV-2 infection
- Autism spectrum disorders
- Seizure disorders
- Cognitive deficits due to brain tumor or previous treatment for cancer
|
B4161 |
Basic benefit and medical policy Elemental formula
The safety and effectiveness of elemental formula for infants with a cow’s milk allergy have been established. Elemental formula is considered medically necessary when clinical criteria are met, effective Sept. 1, 2023.
Inclusions:
When all the following criteria are met:
- An infant must demonstrate an allergy to cow’s milk formula.
- Must have a documented failed trial of soy-based formula and a hydrolyzed formula, such as Alimentum, Nutramigen, Pregestimil, MJ3232A or Good Start, by clinical documentation of one of the following:
- Skin reaction such as eczema or atopic dermatitis
- Gastrointestinal disturbances, including malabsorption, blood or mucous in the stool, diarrhea, colic, abdominal distention or flatus
- Frequent upper or lower respiratory tract infections or bronchospasm
- Anaphylaxis
- Removal of common allergens from the infant’s or mother’s diet (if breastfed) has failed to resolve the symptoms.
Infants who meet these criteria may have Neocate, Neocate one plus, Neocate with DHA and ARA, Elecare, PurAmino, Alfamino reimbursed up to 12 months of age. Most infants outgrow their allergies by this time. Thereafter, reassessment by the pediatrician must be documented to justify continuance beyond 12 months.
Exclusions:
- All other formulas not included as Elemental formula aren’t covered on this policy.
- Elemental formula for adults
- Elemental diet for adults
- Elemental supplements
- Elemental formula for inborn errors of metabolism
|
J1741 |
Basic benefit and medical policy
Caldolor (ibuprofen injection)
Effective May 11, 2023, Caldolor (ibuprofen injection) is covered for the following FDA-approved indications:
Caldolor is a nonsteroidal anti-inflammatory drug indicated in adults and pediatric patients age 3 months and older for the:
- Management of mild to moderate pain and the management of moderate to severe pain as an adjunct to opioid analgesics
- Reduction of fever
Dosage and administration:
- Pediatric (pain and fever) age 3 months to less than 6 months: 10 mg/kg intravenously over 10 minutes up to a maximum single dose of 100 mg
|
J3262 |
Basic benefit and medical policy Actemra (tocilizumab)
Actemra (tocilizumab) is covered for the following updated FDA-approved indication, effective Dec. 21, 2022:
Hospitalized adult patients with COVID-19 who are receiving systemic corticosteroids and require supplemental oxygen, non-invasive or invasive mechanical ventilation, or extracorporeal membrane oxygenation |
J3490
J3590 |
Basic benefit and medical policy
Abilify Asimtufii (aripiprazole)
Abilify Asimtufii (aripiprazole) is considered established when criteria are met, effective April 27, 2023.
Abilify Asimtufii (aripiprazole) is an atypical antipsychotic indicated:
- For the treatment of schizophrenia in adults
- As maintenance monotherapy treatment of bipolar I disorder in adults
Dosage and administration:
- For patients naïve to aripiprazole, establish tolerability with oral aripiprazole before initiating treatment with Abilify Asimtufii (aripiprazole).
- Administered by intramuscular injection in the gluteal muscle by a health care professional. Don’t administer by any other route.
- Recommended dosage is 960 mg administered once every two months as a single injection. Dose can be reduced to 720 mg in patients with adverse reactions.
- Missed doses: Dosage adjustment may be required.
- Known CYP2D6 poor metabolizers: Recommended dosage is 720 mg administered once every two months as a single injection.
Dosage forms and strengths:
Extended-release injectable suspension: 960 mg/3.2 mL and 720 mg/2.4 mL single-dose pre-filled syringes
Abilify Asimtufii (aripiprazole) isn’t a benefit for URMBT. |
J3490
J3590 |
Basic benefit and medical policy Rezzayo (rezafungin)
Effective March 22, 2023, Rezzayo (rezafungin) is covered for the following FDA-approved indications:
Rezzayo (rezafungin) is an echinocandin antifungal indicated in patients 18 years of age or older who have limited or no alternative options for the treatment of candidemia and invasive candidiasis. Approval of this indication is based on limited clinical safety and efficacy data for Rezzayo (rezafungin).
Limitations of use:
Rezzayo (rezafungin) hasn’t been studied in patients with endocarditis, osteomyelitis and meningitis due to Candida.
Dosage and administration:
Administer the recommended dosage of Rezzayo (rezafungin) once weekly by intravenous infusion, with an initial 400 mg loading dose, followed by a 200 mg dose once weekly thereafter. The safety of Rezzayo (rezafungin) hasn’t been established beyond four weekly doses.
Dosage forms and strengths:
For injection: 200 mg as a solid (cake or powder) in a single-dose vial for reconstitution.
Rezzayo (rezafungin) isn’t a benefit for URMBT. |
J3490
J3590 |
Basic benefit and medical policy
Roctavian (valoctocogene roxaparvovec-rvox)
Roctavian (valoctocogene roxaparvovec-rvox) is considered established, effective June 29, 2023.
Coverage of Roctavian (valoctocogene roxaparvovec-rvox) is provided when all the following are met:
- FDA-approved age
- Prescribed by or in consultation with a specialist who works in a hemophilia treatment center
- Diagnosis of severe hemophilia A with factor VIII level < 1% IU/dL
- Must not have detectable pre-existing immunity to the AAV5 capsid as measured by AAV5 transduction inhibition or AAV5 total antibodies
- Must not have a history of factor VIII inhibitors and results for a modified Nijmegen-Bethesda assay of less than 0.6 Bethesda units (BU) on two consecutive occasions at least one week apart within the past 12 months must be submitted to the plan
- Must have been treated with or exposed to factor VIII concentrates or cryoprecipitate for a minimum of 150 exposure days
- Must be treatment experienced with Hemlibra for at least six months and experienced treatment failure, defined as any of the following:
- Spontaneous soft tissue bleeding event
- Micro-bleeding into a joint
- Ongoing joint pain of a known target joint B
Quantity limitations, authorization period and renewal criteria:
- Quantity limit: FDA-approved dosing
- Authorization period: Three months with no renewal
This drug isn’t a benefit for URMBT.
|
J3490
J3590 |
Basic benefit and medical policy Uzedy (risperidone)
Uzedy (risperidone) is considered established when criteria are met, effective April 28, 2023.
Uzedy (risperidone) is an atypical antipsychotic indicated for the treatment of schizophrenia in adults.
Dosage and administration:
- Establish tolerability with oral risperidone before initiating Uzedy.
- Administer Uzedy by subcutaneous injection in the abdomen or upper arm by a health care professional. Don’t administer by any other route.
- Initiate Uzedy at the clinically appropriate dose using the following:
- Prior oral risperidone therapy: 2 mg of oral risperidone per day
Uzedy dosage once monthly: 50 mg
Uzedy dosage once every two months: 150 m
- Prior oral risperidone therapy: 3 mg of oral risperidone per day
Uzedy dosage once monthly: 75 mg
Uzedy dosage once every two months: 150 mg
- Prior oral risperidone therapy: 4 mg of oral risperidone per day
Uzedy dosage once monthly: 100 mg
Uzedy dosage once every two months: 200 mg
- Prior oral risperidone therapy: 5 mg of oral risperidone per day
Uzedy dosage once monthly: 125 mg
Uzedy dosage once every two months: 250 mg
|
J3490
J3590 |
Basic benefit and medical policy
Vyjuvek (beremagene geperpavec-svdt)
Vyjuvek (beremagene geperpavec-svdt) is considered established, effective May 19, 2023.
Coverage of Vyjuvek (beremagene geperpavec-svdt) is provided when all the following are met:
- FDA-approved age
- For the treatment of open wounds in patients with a diagnosis of dystrophic epidermolysis bullosa as confirmed by all the following:
- Skin biopsy of an induced blister with immunofluorescence mapping or transmission electron microscopy
- Genetic test results documenting mutations in the COL7A1 gene
- Patient must not have current evidence or a history of squamous cell carcinoma in the area undergoing treatment.
- Trial and failure, intolerance or a contraindication to the preferred products as specified in the Blue Cross Blue Shield of Michigan medical utilization management drug list B.
Quantity limitations, authorization period and renewal criteria:
- Quantity limit: Align with FDA-recommended dosing.
- Initial authorization period: Six months
- Renewal criteria: Clinical documentation must be provided to confirm that current criteria are met and that the medication is providing clinical benefit.
This drug isn’t a benefit for URMBT.
|
J3490
J3590 |
Basic benefit and medical policy Xacduro (sulbactam/durlobactam)
Xacduro (sulbactam/durlobactam) is considered established effective May 23, 2023.
Xacduro is a co-packaged product containing sulbactam, a beta-lactam antibacterial and beta lactamase inhibitor, and durlobactam, a beta lactamase inhibitor, indicated in patients 18 years and older for the treatment of hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia, or HABP and VABP, caused by susceptible isolates of acinetobacter baumannii-calcoaceticus complex.
Limitations of use:
Xacduro isn’t indicated for the treatment of HABP and VABP caused by pathogens other than susceptible isolates of acinetobacter baumannii-calcoaceticus complex.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Xacduro and other antibacterial drugs, Xacduro should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
Dosage and administration:
- Administer Xacduro (1 g of sulbactam, 1 g of durlobactam) every six hours by intravenous infusion over three hours in patients with creatinine clearance, or CLcr, of 45 to 129 mL/min.
- Dosing regimen adjustments are recommended for CLcr less than 45 mL/min and CLcr greater than or equal to 130 mL/min.
- Administer all doses of Xacduro by IV infusion over three hours.
Dosage forms and strengths:
Xacduro is a co-packaged kit containing the following two components as sterile powders for reconstitution:
- One clear single-dose vial of sulbactam for injection 1 g, and
- Two amber single-dose vials of durlobactam for injection 0.5 g.
This drug isn’t a benefit for URMBT. |
J9173 |
Basic benefit and medical policy
Imfinzi (durvalumab)
The FDA has updated the payable indications for Imfinzi (durvalumab), effective Sept. 2, 2022. The payable indications include the following:
Imfinzi is a programmed death-ligand 1 (PD-L1) blocking antibody indicated in combination with gemcitabine and cisplatin, as treatment of adult patients with locally advanced or metastatic biliary tract cancer, or BTC.
Dosage and administration:
Administer Imfinzi as an intravenous infusion over 60 minutes after dilution.
BTC:
- Weight of 30 kg and more: Administer Imfinzi 1,500 mg every three weeks in combination with chemotherapy and then 1,500 mg every four weeks as a single agent.
- Weight less than 30 kg: Administer Imfinzi 20 mg/kg every three weeks in combination with chemotherapy and then 20 mg/kg every four weeks as a single agent.
|
Q5111 |
Basic benefit and medical policy Udenyca (pegfilgrastim-cbqv)
Udenyca (pegfilgrastim-cbqv) is covered for the following updated FDA-approved indication, effective Nov. 28, 2022:
- Udenyca (pegfilgrastim-cbqv) is a leukocyte growth factor indicated to increase survival in patients acutely exposed to myelosuppressive doses of radiation (hematopoietic subsyndrome of acute radiation syndrome).
Limitations of use:
Udenyca (pegfilgrastim-cbqv) isn’t indicated for the mobilization of peripheral blood progenitor cells for hematopoietic stem cell transplantation.
Dosage and administration:
Patients acutely exposed to myelosuppressive doses of radiation:
- Two doses, 6 mg each, administered subcutaneously one week apart. Administer the first dose as soon as possible after suspected or confirmed exposure to myelosuppressive doses of radiation and a second dose one week after.
- Use weight-based dosing for pediatric patients weighing less than 45 kg.
|
S9123, S9124 |
Basic benefit and medical policy
Private duty nursing
Private duty nursing may be considered established when specified criteria are met (refer to inclusionary and exclusionary guidelines).
Inclusionary and exclusionary criteria have been updated, effective June 1, 2023.
Inclusions:
All must be met:
- The PDN services must be ordered by a physician, M.D. or D.O., who is involved in the ongoing care of the patient.
- The patient must have a need for skilled nursing care.
- The patient’s condition must be complex or medically fragile.
- The patient’s complex or fragile condition requires continuous assessment, observation and monitoring.
- The patient must be medically stable at the time of discharge from the hospital such that PDN services can be provided safely.
- At least two caregivers (family, friends, etc.) must be trained and competent to give care.
- The patient needs skilled care that exceeds the scope of intermittent care.
- The family or caregivers must provide at least eight hours of skilled care/day (a maximum of 16 hours per day of PDN care may be approved per day if medical necessity criteria are met).
- Training and teaching activities by the private duty nurse to teach the patient, family or caregivers how to manage the treatment regimen is required and considered a skilled nursing service.
- Training is no longer appropriate if, after a reasonable period of time, the patient, family or caregiver won’t or isn’t able to be trained.
- If the caregiver/family member can’t or won’t accept responsibility for the care, private duty nursing will be considered not medically necessary as the home would be deemed an unsafe environment.
- Criteria for specific conditions, if present, in addition to the medically complex and or fragile condition of the patient, one of the following must be present:
- Tracheostomy tube suctioning is necessary for secretion control and required at least twice per eight-hour shift. (Tracheostomy tube changing is skilled; tracheostomy hygiene care isn’t.)
- Management of tube drainage, complex wounds, cavities or irrigations require documentation of services on the record when they occur.
- Complex medication administration (excluding PO medications that would ordinarily be taken by self-administration) of drugs with potential for serious side effects or drug interactions require documentation and appropriate monitoring. This includes intravenous administration of drugs or nutrition.
- Tube feedings that require frequent changes in formulation or administration rate or have conditions that increase the aspiration risk requires documentation.
PDN for patients on ventilators
- For patients who are on ventilators after discharge or suffer an acute event, up to 30 days of PDN services may be authorized.
- Ventilator management: There must be documentation of the initial settings of mode of ventilation, tidal volume, respiratory rate and wave form modifications, if any, PEEP, and FIO2 at the beginning of each shift.
- Oxygen saturation must be measured continuously for ventilator patients and any changes from baseline recorded thereafter.
- Hourly observations of the patient’s clinical condition related to the ventilator management must be documented along with any changes in oxygen saturation.
- The goal is to transition ventilator care to family or caregivers once the member is stable. When family or caregivers can provide the patient’s routine ventilator care, including weaning (when appropriate), under the direction of their health care professional, the patient is deemed stable.
Ventilator care/management isn’t considered a skilled service requiring PDN nursing.
Exclusions:
Services of a private duty nurse are considered not covered in any of the following instances:
- The PDN is acting as a nurse’s aide.
- Custodial care (bathing, feeding, exercising, homemaking, giving oral medications or acting as a companion/sitter) doesn’t qualify for PDN.
- The private duty nurse is a member of the patient’s household or if the cost of care is provided by one of the patient’s relatives (by blood, marriage or adoption).
- The PDN is for maintenance care after the patient’s condition has stabilized (including routine ostomy care, tube feeding administration and tracheostomy or ventilator management).
- Medical and nursing documentation shows that the patient’s condition is stable/predictable or controlled, and a licensed nurse isn’t required to monitor the condition.
- Care plan indicates a licensed nurse isn’t required to be in continuous attendance.
- Care plan doesn’t require hands-on nursing interventions (Note: Observation in case an intervention is required isn’t considered skilled care.)
- The caregiver or patient’s family has demonstrated the ability to carry out the plan of care.
- If the patient’s anticipated need is indefinite, lifetime private duty nursing isn’t a benefit.
- The care is for a person without an available caregiver in the home.
- It’s for respite care that includes (list isn’t all inclusive):
- Care during a caregiver vacation
- The convenience of the family or caregiver, so that the caregiver may attend work, school or care for other family members.
- If the caregiver or family can’t or won’t accept responsibility for the care, private duty nursing will be considered not medically necessary as the home would be deemed an unsafe environment.
- The PDN is provided outside the home (for example, school, nursing facility or assisted living facility).
- It’s a duplication or overlap of services (for example, when a person is receiving hospice care services or for the same hours of a skilled nursing home care visit).
- It’s for observational purposes only.
- The skilled nursing is provided as part-time/intermittent and not continuous care.
Documentation requirements need all of the following:
- Current plan of care signed by a physician (M.D. or D.O.) or signed by an advanced practitioner (NP, CNS or PA) in accordance with state law.
- Plan of care must reflect the patient’s current clinical condition and be updated at least every three months.
- Care plans greater than three months may indicate the patient is stable or that care is maintenance.
- A comprehensive assessment of the patient’s health status, including documentation of the skilled need and medication administration record.
- Discharge summary or recent progress note if patient is being discharged from an inpatient setting.
- Consultation notes if the patient is receiving services from subspecialist.
- Hourly documentation of the clinical information and services performed is required.
Additional documentation clarifying clinical status (such as well-child check or specialist visit notes) may be requested if clinical documentation provided doesn’t support the hours required. |
None of the information included in this billing chart is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.

Blue Cross, BCN covering additional vaccines
To increase access to vaccines and decrease the risk of vaccine-preventable disease outbreaks, Blue Cross Blue Shield of Michigan and Blue Care Network will add the following vaccines to our list of vaccines covered under the pharmacy benefit:
Vaccine |
Common name and abbreviation |
Effective date |
Arexvy™ |
Respiratory syncytial virus, or RSV
|
July 17, 2023
|
Abrysvo™ |
Following are all the vaccines that are covered under eligible members’ prescription drug plans. Most Blue Cross and BCN commercial (non-Medicare) members with prescription drug coverage are eligible. If a member meets the coverage criteria, the vaccine is covered with no out-of-pocket costs.
Note: Vaccines must be administered by certified, trained and qualified registered pharmacists.
Vaccines that are covered and have no age requirement
Vaccine |
Common name and abbreviation |
|
Dengue vaccine — DEN4CYD |
|
Diphtheria, tetanus, and acellular pertussis vaccine — DTaP |
- Diphtheria and tetanus toxoids
|
Diphtheria, tetanus vaccine — DT |
|
DTap and inactivated poliovirus vaccine — DTaP-IPV |
|
DTaP, hepatitis B, and inactivated poliovirus vaccine — DTaP-HepB-IPV |
|
DTaP, inactivated poliovirus, Haemophilus influenzae type b, and hepatitis B vaccine — DTaP-IPV-Hib-HepB |
- ActHIB®
- Hiberix®
- PedvaxHIB®
|
Haemophilus influenzae type b vaccine — Hib
|
|
Hepatitis A — HepA |
- Engerix-B®
- Heplisav-B®
- PreHevbrio™
- Recombivax HB®
|
Hepatitis B — HepB |
|
Hepatitis A & B — HepA-HEPB |
|
Measles, mumps, rubella vaccine — MMR |
|
Measles, mumps, rubella and varicella vaccine — MMRV |
|
Meningococcal serogroups A, C, W, Y vaccine — MenACWY-CRM |
|
Meningococcal serogroups A, C, W, Y vaccine — MenACWY-D |
|
Meningococcal serogroups A, C, W, Y vaccine — MenACWY-TT |
|
Meningococcal serogroup B vaccine — MenB-4C |
|
Meningococcal serogroup B vaccine — MenB-FHbp |
|
Pneumococcal 15-valent conjugate vaccine — PCV15 |
|
Pneumococcal 20-valent conjugate vaccine — PCV20 |
|
Pneumococcal 23-valent polysaccharide vaccine — PPSV23 |
|
Poliovirus — IPV |
|
Respiratory syncytial virus — RSV |
|
Rotavirus vaccine — RV1 |
|
Rotavirus vaccine — RV5 |
|
Tetanus and diphtheria vaccine — Td |
|
Tetanus, diphtheria and acellular pertussis vaccine — Tdap |
|
Varicella vaccine — VAR or chickenpox |
|
Zoster vaccine — RZV or shingles |
Covid vaccines
- Pfizer-BioNTech COVID-19 vaccine, bivalent
- Moderna COVID-19 vaccine, bivalent
- Novavax COVID-19 vaccine
Vaccines with age requirements
If a member doesn’t meet the age requirement for a certain vaccine, Blue Cross and BCN won’t cover it under the prescription drug plan, and the claim will reject.
Accurate billing and coding reminders
To ensure accurate coding and billing, Blue Cross Blue Shield of Michigan would like to offer these reminders about laser treatments for psoriasis and anesthesia medication modifiers.
Laser treatment for psoriasis
The following procedure codes should only be reported for the treatment of psoriasis:
- *96920 ̶ Laser treatment for inflammatory skin disease (psoriasis); total area less than 250 sq cm
- *96921 ̶ Laser treatment for inflammatory skin disease (psoriasis); 250 sq cm to 500 sq cm
- *96922 ̶ Laser treatment for inflammatory skin disease (psoriasis); over 500 sq cm
Claims submitted with a diagnosis other than the treatment of psoriasis may receive a denial.
Medical direction modifiers for anesthesia
Blue Cross’ payment policy also requires accurate reporting of anesthesia medical direction modifiers. Please make sure the appropriate medical direction modifier is added to the anesthesia procedure code to indicate the level of service the physician or the non-physician practitioner provides.
Conflicts in the reporting of anesthesia medical direction modifiers may result in a claim denial.
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
We’ve announced our Collaborative Care designations
We recently announced that 239 primary care practices and five OB/GYN practices have been designated for our Collaborative Care Designation Program for the September 2023 through August 2024 designation cycle. This was the first year that OB/GYN practices were included in the program.
Designated practices deliver care using the highly effective Collaborative Care Model. Collaborative Care adds a behavioral health component to the partnership between a patient and their PCMH-designated physician.
The Collaborative Care team consists of a doctor, who is the head of a care team, a behavioral health care manager and a consulting psychiatrist. These individuals work collaboratively to ensure patients get the care they need.
This approach can help improve the behavioral health of Michigan residents, addressing both mental health and substance use disorder conditions. Collaborative Care can also improve the overall health of Michiganders by providing value-based care that helps avoid emergency room visits and duplicative services.
As we explained in a Hospital and Physician Update article on Collaborative Care, a primary care practice must have a Patient-Centered Medical Home designation and meet certain criteria to receive the Collaborative Care designation. The criteria, which consist of a set of capabilities, reflect elements that a practice needs to have to effectively deliver care using the Collaborative Care Model.
The largest concentration of Collaborative Care practices is in Southeast Michigan and the west side of the state.
The Collaborative Care Model has been in use by early adopters in Michigan since 2015. After reviewing preliminary results from those early adopters, Blue Cross Blue Shield of Michigan launched a formal training program for primary care practices seeking to implement Collaborative Care in 2020, along with an incentive structure for learning about and using the model.
Practices that would like to earn a PCMH or Collaborative Care designation are encouraged to reach out to their physician organization for details.
We’ll require prior authorization for some diabetes drugs prescribed to Medicare Advantage members, starting Jan. 1
We continually review prescription drugs to provide the best value for our members, control costs and make sure members are using the right drug for the right situation.
As part of our process, certain diabetes medications will require prior authorization if they’re prescribed for Medicare Plus Blue℠ and BCN Advantage℠ members who don’t have a supporting prescription or medical record with a diabetes diagnosis, beginning Jan. 1, 2024. Original Medicare prohibits Part D plans from covering drugs used for weight loss.
The drugs that will require prior authorization are listed below:
Brand-name medication |
FDA-approved indication |
Plan payment requirement |
- Bydureon®
- Byetta®
- Mounjaro®
- Ozempic®
- Rybelsus®
- Trulicity®
- Victoza®
|
Type 2 diabetes |
- Payment will only be approved if using for Type 2 diabetes
- Excluded if used for weight loss
|
Health care providers prescribing any of the medications listed above for our Medicare Plus Blue and BCN Advantage members will need to request a prior authorization for the medication to be covered for their patients. For information on how to submit the request electronically, click here.
We’ll let your affected patients know about this change and encourage them to speak with you about any concerns.
For a complete list of drugs and associated requirements, go to 2023 Drug Lists.
Kidney-only transplants to require prior authorization, starting Jan. 1
For dates of service on or after Jan. 1, 2024, hospital transplant financial coordinators must submit prior authorization requests for kidney-only transplants through the e-referral system for:
- Blue Cross Blue Shield of Michigan fully insured group and individual commercial members
- Blue Care Network fully insured group and individual commercial members
- All BCN Advantage℠ members
As with other transplants that already require prior authorization — including simultaneous pancreas-kidney, or SPK — it’s a two-step process in the e-referral system:
- Submit an outpatient prior authorization request that includes:
- Procedure codes *50360 and *50365
- The facility
- For commercial members, enter a Blue Distinction® Center for Transplants.
- For BCN Advantage members, enter a facility that’s accredited by the Centers for Medicare & Medicaid Services for kidney transplants.
- The completed questionnaire — The questionnaire automatically opens in the e-referral system for you to fill out.
- Clinical information — Include the history and physical, the letter of intent and clinical documentation to support the need for the transplant.
The request will pend for clinical review. In addition, the request will require medical director review if the facility isn’t a Blue Distinction Center for Transplants (for commercial members), the facility isn’t accredited by CMS for kidney transplants (for BCN Advantage members) or the member doesn’t meet medical policy criteria.
If the authorization is approved, it will be valid for one year.
- When a kidney becomes available, submit a prior authorization request for the inpatient stay. Include the outpatient authorization number for the transplant procedure codes in the Case Communication field. This will enable us to issue an approval quickly as it makes the connection between the inpatient request and the already-approved outpatient authorization.
You’ll be able to start submitting requests through the e-referral system for kidney-only transplants on Jan. 1, 2024.
We’ll update the e-referral User Guide for kidney-only transplants before Jan. 1. The pertinent information will be in “Section IV: Referrals and Authorizations,” in the subsection titled “5. Submit an Outpatient Authorization.” (The e-referral User Guide also includes information about submitting a re-authorization request, if the authorization obtained through Step 1, mentioned above, expires before a kidney becomes available.)
Notes:
Here are some key guidelines for NICU billing
When billing room and board services for pediatric patients outside of the defined newborn age of 28 days or less for new admissions, health care providers should use the appropriate corresponding pediatric room and board revenue codes.
According to ICD-10-CM classification guidelines, a newborn is defined as a baby who is in the first 28 days of life. Critical care services for the newborn take place in a nursery or neonatal intensive care unit, also called NICU, and are represented by revenue codes 0170-0174. If a medical condition presents after the first 28 days of life, it’s no longer considered a newborn medical condition.
Exclusions to this billing guideline are when the patient is transferred from the birth hospital to another hospital for non-routine care, with services beginning during the newborn period.
Newborn and pediatric revenue codes and descriptions:
0170 |
Room and Board Nursery |
Used for routine newborn care |
0171 |
Newborn Level 1 |
Used for non-routine newborn care |
0172 |
Newborn Level II |
Used for non-routine newborn care |
0173 |
Newborn Level III |
Used for non-routine newborn care |
0174 |
Newborn Level IV |
Used for non-routine newborn care |
0113 |
Pediatric Room and Board |
Private |
0123 |
Pediatric Two Beds |
Semi-private |
0203 |
Pediatric Intensive Care |
Used for intensive pediatric care |
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Review requirements for prior authorization of Omisirge
Omisirge® is a new-to-market cellular therapy that was recently approved by Blue Cross Blue Shield of Michigan’s and Blue Care Network’s Pharmacy and Therapeutics committee.
On May 23, 2023, we published a provider alert stating that Omisirge will require prior authorization for most commercial members for dates of service on or after June 8, 2023. The member must have an approval for a stem cell transplant on file through Blue Cross’ and BCN’s Human Organ Transplant Program before a prior authorization request for Omisirge can be approved.
You can view the complete requirements in our Omisirge medical policy. To access the medical policy:
- Go to bcbsm.com/providers.
- Click on Resources.
- Click on Search Medical Policies.
- In the Medical Policy Router Search page, type “Omisirge” in the Policy/Topic Keyword field and press Enter.
- Click on the link to open the Omisirge medical policy.
Select Medicare Advantage members received in-home test kits in September
Blue Cross Blue Shield of Michigan and Blue Care Network contracted with Everlywell, an independent company, to distribute in-home test kits in September to select Medicare Advantage members.
Some members may have received the following tests:
- Members who had a gap in care for colorectal cancer screening received a fecal immunochemical test, or FIT, kit.
- Members who had a gap in care for hemoglobin A1c, or HbA1c, testing, received an HbA1c testing kit.
If your patients reach out to you about these tests, you may want to encourage them to take advantage of this convenient, no-cost testing.
Members who were sent the tests were encouraged to discuss test results with their primary care providers. Here’s how the test result notification process works:
|
Normal results |
Abnormal results |
Blue Cross or BCN MA member |
Mail |
Mail and phone call
Certified letter if unable to reach |
Primary care provider |
Mail |
Fax |
We’ve added and updated questionnaires in e-referral system
On Aug. 27, 2023, Blue Cross Blue Shield of Michigan and Blue Care Network added and updated questionnaires in the e-referral system. We also updated the corresponding authorization criteria and preview questionnaires on the ereferrals.bcbsm.com website.
As a reminder, we use our authorization criteria, our medical policies and your answers to the questionnaires in the e-referral system when making utilization management determinations on your prior authorization requests.
New questionnaire
We added the following questionnaire to the e-referral system:
Questionnaire |
Opens for |
Details |
Balloon ostial dilation |
- Medicare Plus Blue℠
- BCN commercial
- BCN Advantage℠
|
Opens for procedure codes *31295, *31296, *31297 and *31298
Note: For dates of service on or before Aug. 27, 2023, the Sinusotomy questionnaire opens for these procedure codes. |
Updated questionnaires
We updated the following questionnaires:
Questionnaire |
Opens for |
Updates |
Deep brain stimulation |
- Medicare Plus Blue
- BCN commercial
- BCN Advantage
|
Updated two questions |
Endovascular intervention, peripheral artery |
- Medicare Plus Blue
- BCN Advantage
|
No longer opens for procedure codes *0238T, *34101, *34111, *34151, *34201, *34203, *37184 and *37222
Note: Effective Sept. 1, 2023, this questionnaire no longer opens for BCN commercial members because these procedures will be managed by Carelon Medical Benefits Management. |
Responsive neurostimulator/deep brain stimulation trigger |
- BCN commercial
- BCN Advantage
|
Updated the question |
Responsive neurostimulation for the treatment of refractory focal epilepsy |
- BCN commercial
- BCN Advantage
|
Updated the title of the questionnaire to align with the title of the updated medical policy. |
Septoplasty |
- Medicare Plus Blue
- BCN commercial
- BCN Advantage
|
Updated two questions |
Sinusotomy |
- Medicare Plus Blue
- BCN commercial
- BCN Advantage
|
- “No longer open for procedure codes *31295, *31296, *31297 and *31298”
- Removed questions related to balloon ostial dilation
- Updated several questions
|
Thyroidectomy, total |
- Medicare Plus Blue
- BCN commercial
- BCN Advantage
|
Updated five questions |
Preview questionnaires
Preview questionnaires show the questions you’ll need to answer in the e-referral system so you can prepare your answers ahead of time.
To find the preview questionnaires, go to ereferrals.bcbsm.com and:
- For Medicare Plus Blue: Click on Blue Cross and then click on Authorization Requirements & Criteria. Scroll down and look under the Authorization criteria and preview questionnaires — Medicare Plus Blue heading.
- For BCN: Click on BCN and then click on Authorization Requirements & Criteria. Scroll down and look under the Authorization criteria and preview questionnaires heading.
Authorization criteria and medical policies
The Authorization Requirements & Criteria pages explain how to access the pertinent authorization criteria and medical policies.
Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services. For more information, go to our ereferrals.bcbsm.com website.
Lunch and learn webinars for physicians and coders focus on risk adjustment, coding
As a reminder, we’re offering live, 30-minute educational webinars that provide updated information on documentation and coding for common challenging diagnoses. Webinars also include an opportunity to ask questions.
Here’s our upcoming schedule and tentative topics for the webinars. Each session starts at noon Eastern time. Log in to the provider training website to register for sessions that work with your schedule.
Session date |
Topic |
Oct. 18 |
ICD-10-CM updates and changes for 2024 |
Nov. 15 |
Coding chronic kidney disease and rheumatoid arthritis |
Dec. 13 |
CPT coding scenarios for 2024 |
If you haven’t already registered for the provider training website, follow these steps:
- Click here to register.
- Complete the registration. We recommend using the same email you use to communicate with Blue Cross Blue Shield of Michigan for other needs. This will become your login ID.
Locating a session
Click here if you’re already registered for the provider training website. On the provider training website, look in the Event Calendar or use the search feature using the keyword “lunch” to quickly locate all 2023 sessions.
See the screenshots below for more details.
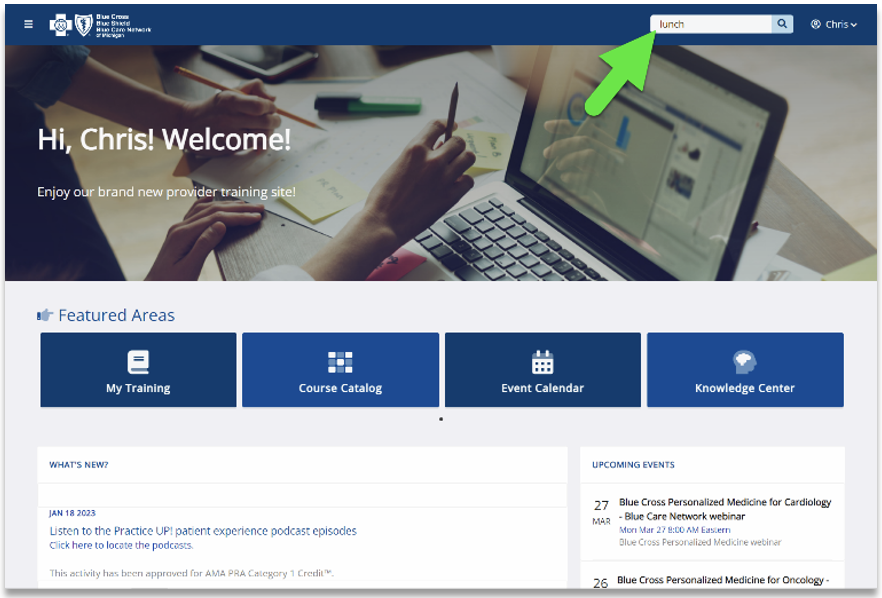
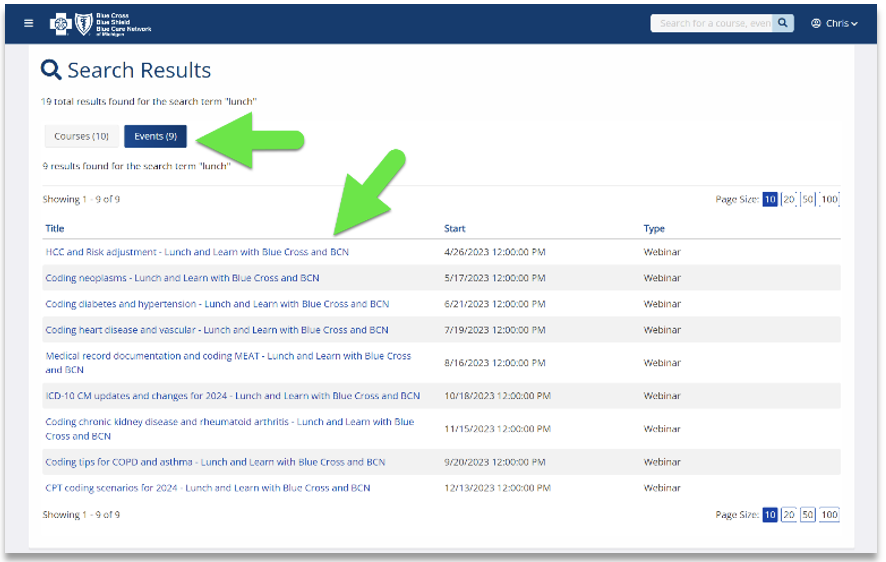
Previous sessions
You can also listen to previously recorded sessions. Check out the following:
Date |
Topic |
April 26 |
HCC and risk adjustment coding scenarios |
May 17 |
Coding neoplasms |
June 21 |
Coding diabetes and hypertension |
July 19 |
Coding heart disease and vascular disease |
Aug. 16 |
Medical Record Documentation and MEAT |
Sept. 20 |
Coding Tips for COPD and asthma |
For more information
If you have any questions about the sessions, contact April Boyce at aboyce@bcbsm.com. If you have questions regarding a session or website registration, email ProviderTraining@bcbsm.com.
Reminder: Resources, on-demand courses available on our training website
Action item
We encourage you to use our provider training website to take courses and learn about topics relevant to your work.
Take advantage of the training resources we offer to health care providers and their staff. Resources include on-demand courses designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network.
See the information below to find out about some of the learning opportunities we launched earlier this year that we think you’ll find worthwhile.
Blue Cross Personalized Medicine℠ presentations: We hosted a series of webinars discussing this new program, which is based on pharmacogenomics, a subgroup of precision medicine. The presentations are specific to primary care physicians, behavioral health providers, cardiologists and oncologists. Search “personalized” on the training website to quickly locate the four presentations.
CMS Star measures overview for 2023: This course is an overview of HEDIS® quality measures that are also Medicare Star Ratings measures. Updated for 2023, the course has a new section on the CAHPS® survey, tips for closing gaps in care, clarifications on quality measure requirements and assistance with coding and documentation. You can earn continuing education credits for completing these courses. Search “star” to locate the series.
HEDIS® measures scenarios for 2023: This course shows you how to close quality gaps using the HEDIS® tip sheets. Learn the tips and tricks through a series of scenarios where you’ll help figure out why an office is seeing gaps in specific measures. The course has been updated for 2023 and is also eligible for continuing education credits. Search “HEDIS” to locate the course.
To log in to the provider training site, click here.
To request access to our training site:
- Visit the registration page and provide the requested information. We recommend using the same email you use to communicate with Blue Cross for provider-related needs. This will become your login ID.
- Click on Register, and follow the prompts to log in.
If you need assistance registering or navigating the site, contact providertraining@bcbsm.com.
HEDIS®, which stands for Healthcare Effectiveness Data and Information Set, is a registered trademark of the National Committee for Quality Assurance, or NCQA.
Resources for prenatal care, well-child visits and childhood immunizations
This is part of an ongoing series of articles focusing on the tools and resources available to help FEP members manage their health.
Early prenatal care, regular well-child visits and routine immunizations support a healthy pregnancy and healthy start to a child’s life. Blue Cross Blue Shield of Michigan developed the following HEDIS® tip sheets on prenatal care, well-child visits and immunizations to assist health care providers and their staff in treating their patients:
Blue Cross and Blue Shield Federal Employee Program® members have access to resources and programs to support growing families. Here are some helpful resources:
The Blue Cross and Blue Shield Service Benefit Plan provides benefit coverage for members at no out-of-pocket cost for prenatal care, well-child visits and most immunizations when serviced by a Preferred provider.
For more information on FEP benefits and resources, members and providers should call Customer Service at 1-800-482-3600 or go to fepblue.org.
HEDIS®, which stands for Healthcare Effectiveness Data and Information Set, is a registered trademark of the National Committee for Quality Assurance, or NCQA.

Look for status note in e-referral system when we pend prior authorization requests for some services
In the Blue Cross Blue Shield of Michigan and Blue Care Network e-referral system, we’re adding a status note to let health care providers know when we’ve pended prior authorization requests for initial admissions to and extensions of stays in:
- Acute (non-behavioral health) inpatient hospitals
- Skilled nursing facilities, acute inpatient rehabilitation facilities and long-term acute care hospitals — for commercial members only
Note: As a reminder, naviHealth manages these requests for Medicare Plus Blue℠ and BCN Advantage℠ members.
We recently implemented this function to make it easier for providers to see the status of their requests. Here’s how it works:
When a Blue Cross or BCN Utilization Management staff member pends a prior authorization request for review by a medical director, a status note appears in the upper-left portion of the Inpatient Authorization Details screen.
The status note says, “Request is being reviewed by physician,” as shown below.
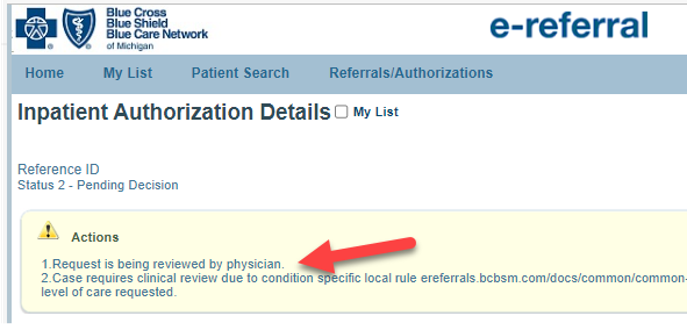
The status note is displayed for Blue Cross commercial, Medicare Plus Blue, BCN commercial and BCN Advantage requests that are managed by the Blue Cross and BCN Utilization Management department.
When we make a determination on the request — whether an approval or a denial — you’ll no longer see the status note.
Previously, when we pended a request, we added a statement to that effect in the Case Communication field.
naviHealth is an independent company that manages authorizations for post-acute care services for Blue Cross Blue Shield of Michigan and Blue Care Network members who have a Medicare Advantage plan.
Reminder: Include preadmission testing services on inpatient claim
Blue Cross Blue Shield of Michigan payment policy requires that health care providers include all preadmission testing services, rendered up to seven days prior to admission, on the inpatient claim. These services shouldn’t be considered for separate reimbursement.
Claims submitted for preadmission testing services within seven days of a related inpatient stay may be denied if billed separately.
Kidney-only transplants to require prior authorization, starting Jan. 1
For dates of service on or after Jan. 1, 2024, hospital transplant financial coordinators must submit prior authorization requests for kidney-only transplants through the e-referral system for:
- Blue Cross Blue Shield of Michigan fully insured group and individual commercial members
- Blue Care Network fully insured group and individual commercial members
- All BCN Advantage℠ members
As with other transplants that already require prior authorization — including simultaneous pancreas-kidney, or SPK — it’s a two-step process in the e-referral system:
- Submit an outpatient prior authorization request that includes:
- Procedure codes *50360 and *50365
- The facility
- For commercial members, enter a Blue Distinction® Center for Transplants.
- For BCN Advantage members, enter a facility that’s accredited by the Centers for Medicare & Medicaid Services for kidney transplants.
- The completed questionnaire — The questionnaire automatically opens in the e-referral system for you to fill out.
- Clinical information — Include the history and physical, the letter of intent and clinical documentation to support the need for the transplant.
The request will pend for clinical review. In addition, the request will require medical director review if the facility isn’t a Blue Distinction Center for Transplants (for commercial members), the facility isn’t accredited by CMS for kidney transplants (for BCN Advantage members) or the member doesn’t meet medical policy criteria.
If the authorization is approved, it will be valid for one year.
- When a kidney becomes available, submit a prior authorization request for the inpatient stay. Include the outpatient authorization number for the transplant procedure codes in the Case Communication field. This will enable us to issue an approval quickly as it makes the connection between the inpatient request and the already-approved outpatient authorization.
You’ll be able to start submitting requests through the e-referral system for kidney-only transplants on Jan. 1, 2024.
We’ll update the e-referral User Guide for kidney-only transplants before Jan. 1. The pertinent information will be in “Section IV: Referrals and Authorizations,” in the subsection titled “5. Submit an Outpatient Authorization.” (The e-referral User Guide also includes information about submitting a re-authorization request, if the authorization obtained through Step 1, mentioned above, expires before a kidney becomes available.)
Notes:
Here are some key guidelines for NICU billing
When billing room and board services for pediatric patients outside of the defined newborn age of 28 days or less for new admissions, health care providers should use the appropriate corresponding pediatric room and board revenue codes.
According to ICD-10-CM classification guidelines, a newborn is defined as a baby who is in the first 28 days of life. Critical care services for the newborn take place in a nursery or neonatal intensive care unit, also called NICU, and are represented by revenue codes 0170-0174. If a medical condition presents after the first 28 days of life, it’s no longer considered a newborn medical condition.
Exclusions to this billing guideline are when the patient is transferred from the birth hospital to another hospital for non-routine care, with services beginning during the newborn period.
Newborn and pediatric revenue codes and descriptions:
0170 |
Room and Board Nursery |
Used for routine newborn care |
0171 |
Newborn Level 1 |
Used for non-routine newborn care |
0172 |
Newborn Level II |
Used for non-routine newborn care |
0173 |
Newborn Level III |
Used for non-routine newborn care |
0174 |
Newborn Level IV |
Used for non-routine newborn care |
0113 |
Pediatric Room and Board |
Private |
0123 |
Pediatric Two Beds |
Semi-private |
0203 |
Pediatric Intensive Care |
Used for intensive pediatric care |
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Review requirements for prior authorization of Omisirge
Omisirge® is a new-to-market cellular therapy that was recently approved by Blue Cross Blue Shield of Michigan’s and Blue Care Network’s Pharmacy and Therapeutics committee.
On May 23, 2023, we published a provider alert stating that Omisirge will require prior authorization for most commercial members for dates of service on or after June 8, 2023. The member must have an approval for a stem cell transplant on file through Blue Cross’ and BCN’s Human Organ Transplant Program before a prior authorization request for Omisirge can be approved.
You can view the complete requirements in our Omisirge medical policy. To access the medical policy:
- Go to bcbsm.com/providers.
- Click on Resources.
- Click on Search Medical Policies.
- In the Medical Policy Router Search page, type “Omisirge” in the Policy/Topic Keyword field and press Enter.
- Click on the link to open the Omisirge medical policy.
Lunch and learn webinars for physicians and coders focus on risk adjustment, coding
As a reminder, we’re offering live, 30-minute educational webinars that provide updated information on documentation and coding for common challenging diagnoses. Webinars also include an opportunity to ask questions.
Here’s our upcoming schedule and tentative topics for the webinars. Each session starts at noon Eastern time. Log in to the provider training website to register for sessions that work with your schedule.
Session date |
Topic |
Oct. 18 |
ICD-10-CM updates and changes for 2024 |
Nov. 15 |
Coding chronic kidney disease and rheumatoid arthritis |
Dec. 13 |
CPT coding scenarios for 2024 |
If you haven’t already registered for the provider training website, follow these steps:
- Click here to register.
- Complete the registration. We recommend using the same email you use to communicate with Blue Cross Blue Shield of Michigan for other needs. This will become your login ID.
Locating a session
Click here if you’re already registered for the provider training website. On the provider training website, look in the Event Calendar or use the search feature using the keyword “lunch” to quickly locate all 2023 sessions.
See the screenshots below for more details.
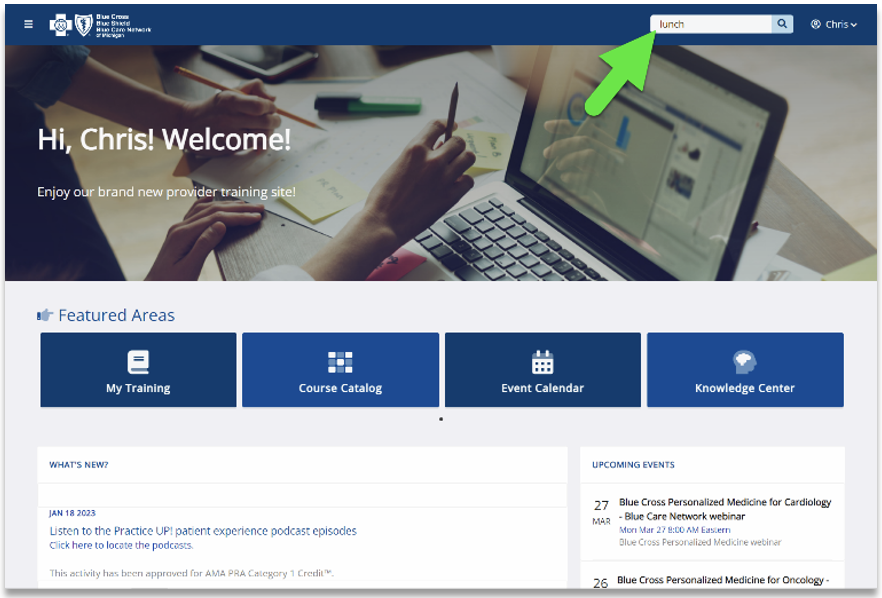
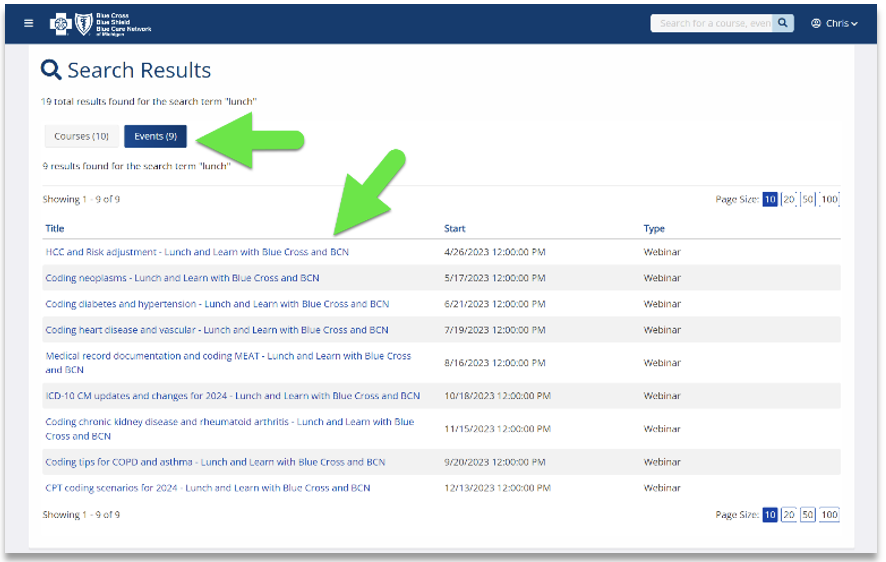
Previous sessions
You can also listen to previously recorded sessions. Check out the following:
Date |
Topic |
April 26 |
HCC and risk adjustment coding scenarios |
May 17 |
Coding neoplasms |
June 21 |
Coding diabetes and hypertension |
July 19 |
Coding heart disease and vascular disease |
Aug. 16 |
Medical Record Documentation and MEAT |
Sept. 20 |
Coding Tips for COPD and asthma |
For more information
If you have any questions about the sessions, contact April Boyce at aboyce@bcbsm.com. If you have questions regarding a session or website registration, email ProviderTraining@bcbsm.com.
|