Forward to a friend |
Subscribe | The Record Archive | Contacts | bcbsm.com | Print this article
|
March 2021
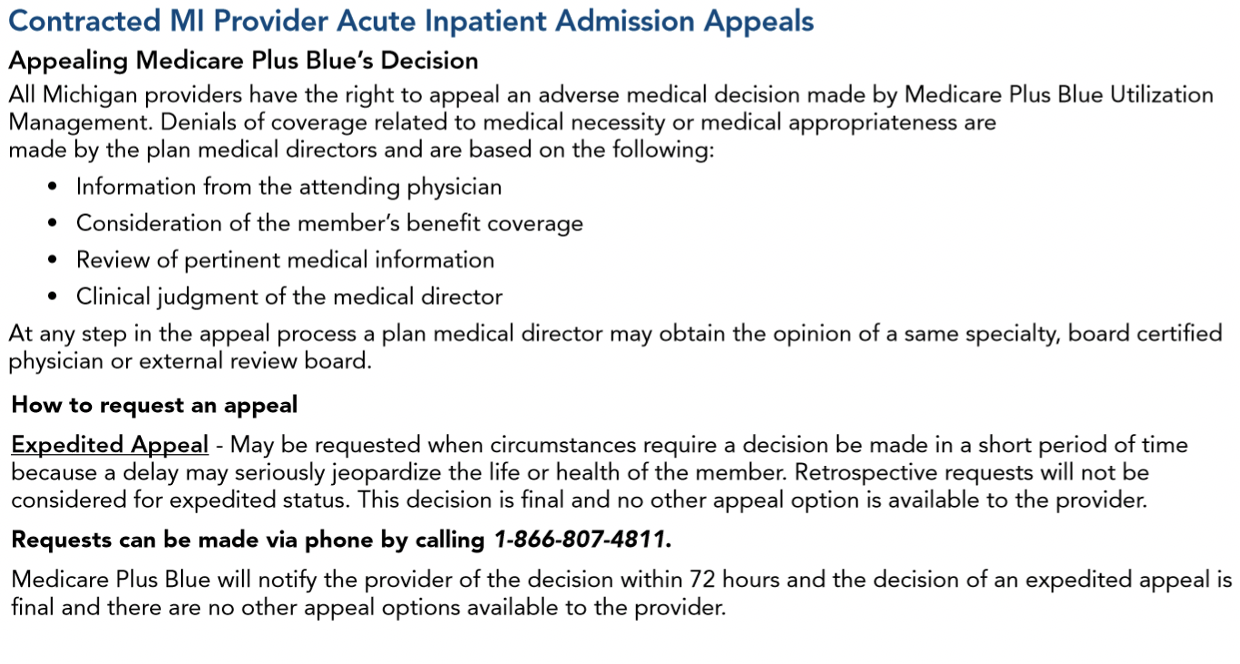
How to submit appeals of Medicare Advantage inpatient acute care admissionsProviders who need to submit appeals for denied authorization requests for Medicare Plus Blue℠ and BCN Advantage℠ inpatient acute care admissions (non‑behavioral health) should follow the process described in the provider manuals. Instructions can also be found in the denial letters Blue Cross Blue Shield of Michigan or Blue Care Network send providers. Medicare Plus Blue For Medicare Plus Blue members, providers can find the process in the “Contracted MI Provider Acute Inpatient Admission Appeals” section of the Medicare Plus Blue℠ PPO Provider Manual. Here’s a screenshot:
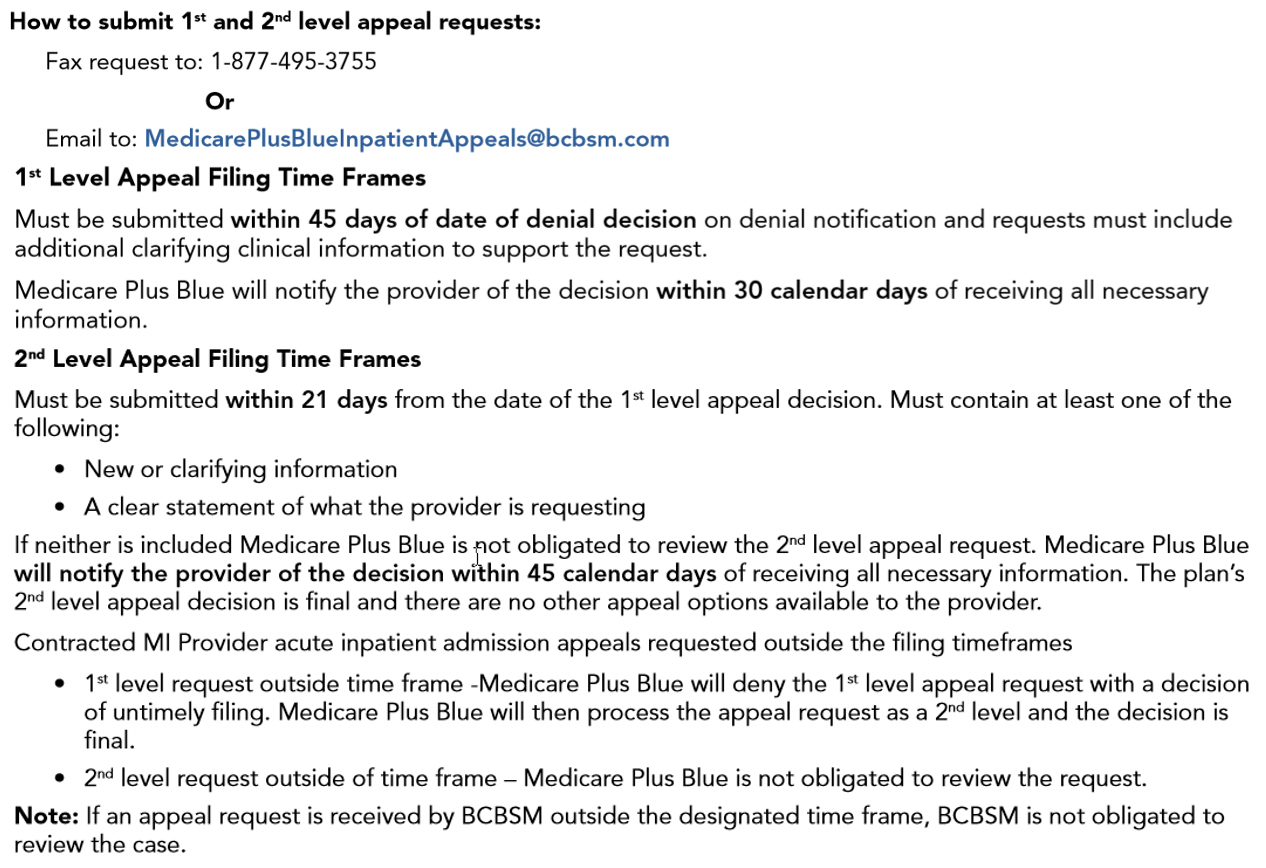
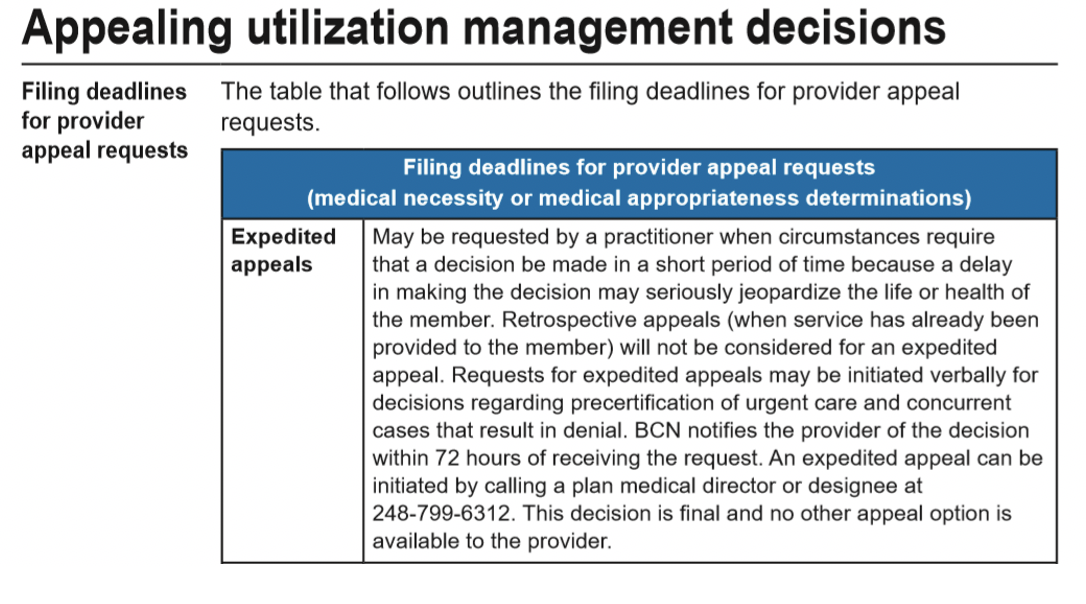
BCN Advantage For BCN Advantage members, providers can find instructions in the “Utilization Management” chapter of the BCN Provider Manual. Look in the section titled “Appealing utilization management decisions.” Here’s a screenshot:
|
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|