|
April 2020

Blue Cross committed to coordination of care among practitioners
Blue Cross Blue Shield of Michigan collects and analyzes data each year to assess the coordination of care and exchange of information among specialists, behavioral health providers and primary care physicians following inpatient and outpatient consultations. This information is important as we work to improve continuity and coordination of care within our network.
Patient care that isn’t coordinated across care settings results in confusion for members, increased risks to patient safety and unnecessary costs due to duplicate testing or procedures. Collaboration among health care providers can also greatly improve member satisfaction.
We can work together to accomplish our goal of 100% coordination of care among all providers by:
- Ensuring that specialists and behavioral health care providers have the correct contact information about the patient’s primary care doctor at the time of the visit
- Requesting that specialists and behavioral health providers forward post-visit information to the patient’s primary care provider
- Asking behavioral health patients to sign an authorization for release of information or including a note of refusal in their chart if a patient declines to share information
We encourage all heath care providers to continue to take steps to enhance the information exchange across the continuum of care.
New Blue Cross, BCN members to be issued alphanumeric subscriber IDs in 2020
Blue Cross Blue Shield of Michigan and Blue Care Network will issue alphanumeric subscriber IDs to new members, starting July 1, 2020. This will apply to all Blue Cross and BCN members, including our Medicare Advantage members.
Blue Cross will use the letter M after the prefix to begin the alphanumeric ID. For example, a new subscriber ID could look like this: XYZM91234567.
The alphanumeric subscriber IDs (de-identified IDs, which appear on subscribers’ member ID cards) are being implemented to avoid duplication with existing Social Security numbers, align with other health plans and to automate manual processes formerly used to correct the duplicate numbers.
There are currently no plans to change subscriber IDs for existing members.
Blue Cross changing practitioner fees July 1
Blue Cross Blue Shield of Michigan will change practitioner fees with dates of service on or after July 1, 2020. This change applies to services provided to our Traditional, TRUST and Blue Preferred PlusSM members, regardless of customer group.
Blue Cross will use the 2020 Medicare resource-based relative value scale for most relative value unit-priced procedures for dates of service on and after July 1. Most fees are currently priced using the 2019 values. Keep in mind that the Physician Group Incentive Program allocation of professional fees will remain unchanged this year. The entire adjustment of 2.0% will be directed toward increasing the funding of value-based reimbursement.
In addition, the conversion factor used to calculate approved amounts in Blue Cross’ anesthesia fee structure will increase to $63.76. Also, the anesthesia base units for CPT code *00812 (anesthesia for procedures on the lower abdomen) used in the same fee structure will be reduced from “4” to “3.”
Fee schedules effective July 1 will be available on web-DENIS on April 1. To find fee schedule information, go to the homepage of web-DENIS and follow these steps:
- Click on BCBSM Provider Publications and Resources.
- Click on Entire Fee Schedules and Fee Changes, which will bring up the End User Agreement.
- Click on Accept.
Only claims submitted with dates of service on or after July 1 will be reimbursed at the new rates.
State of Michigan retirees join our Medicare Advantage PPO plan
State of Michigan retirees became members of our Medicare Plus BlueSM plan, effective Jan. 1, 2020. Their plan, called State Health Plan MA, provides coverage for medical and surgical benefits (Part C). OPTUMRx® administers their prescription drug benefits (Part D).
How do I recognize a State Health Plan MA member?
State Health Plan MA members have Blue Cross Blue Shield of Michigan identification cards with the Medicare Plus Blue Group PPO logo at the top and State Health Plan MA in the middle on the right side. They use group number 35894 and have the XYL alpha prefix.
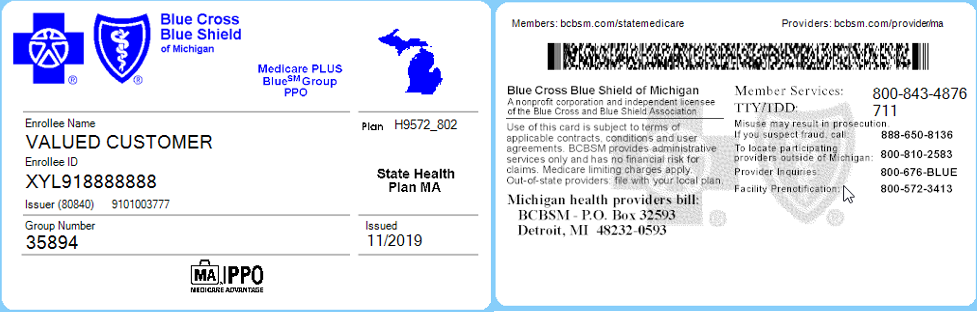
The PPO logo shows that the member is enrolled in a preferred provider organization plan; however, you should verify eligibility and coverage at every visit.
For benefit information, view their 2020 Summary of Benefits here. State Health Plan MA members have some additional enhanced benefits not offered to other groups. Refer to Blue Cross’ Medicare Advantage Enhanced Benefits Fee Schedule and search for State Health Plan MA for more information.
What do I need to know about prior authorization or precertification for State Health Plan MA members?
Like other Medicare Plus Blue PPO members, State Health Plan MA benefits require prenotification for all acute admissions, prior authorization for specified high-tech radiology services and precertification for skilled nursing, long-term acute care and inpatient rehabilitation admissions. Refer to the Medicare Plus Blue PPO Manual for prior authorization and precertification requirements.
We’re improving explanation of benefits statements for Medicare Advantage members
Members with Medicare Advantage plans through Blue Cross Blue Shield of Michigan and Blue Care Network will receive updated explanation of benefits statements, starting in April.
The new EOBs will include additional information about preventive services and cost-share amounts. In case patients ask you about these updates, we wanted to provide you with the notice members will receive with their new EOBs:
We’ve added information to your Explanation of Benefits (EOB).
- Important messages will now be displayed on the front page.
- Preventive services and what you might pay will be more easily identified.
- We’ve grouped together important information about your claims.
- Your benefits have not changed.
April ICD-10-CM code update now available
The Centers for Medicare & Medicaid Services has added an April ICD-10-CM code update that will be effective with dates of service on or after April 1, 2020. This update contains diagnosis (CM) code U07.0, vaping-related disorder, and U07.1, COVID-19.
Additional information about COVID-19 coding
As we communicated through web-DENIS on March 19, the Centers for Disease Control and Prevention has provided interim coding guidance on the ICD-10-CM Official Coding Guidelines for encounters related to the COVID-19 outbreak.
You can use the ICD-10-CM Official Coding Guidelines Supplement** for information about coding encounters related to COVID-19 diagnosis or exposure. The supplement provides clarification on how to use current ICD-10-CM codes for COVID-19 to ensure uniform coding practices.
You can find the latest information about COVID-19 on our Coronavirus information updates for providers page, which is available on BCBSM Newsletters and Resources or BCN Provider Publications and Resources on web-DENIS. (You'll be prompted to log in to access the page.) You may want to check back frequently for updates.
For more information about ICD-10-CM code updates, visit the ICD-10 section of the CMS website.**
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
A9590 replaces A9699 and C9399 when billing for Azedra
The Centers for Medicare & Medicaid Services has an established permanent HCPCS procedure code for radiopharmaceutical medical drug Azedra (iodine i-131, iobenguane, 1 millicurie).
All services performed on and after Jan. 1, 2020, must be reported with procedure code A9590. This code replaces A9699 and C9399 when billing for Azedra.
The National Drug Codes are 71258-0015-02 and 71258-0015-22.
Azedra (iodine i-131, iobenguane, 1 millicurie) continues to be covered for the Food and Drug Administration-approved indications.
Pharmacy doesn’t require preauthorization for this drug.
Billing chart: Blues highlight medical, benefit policy changes
You’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart.
This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures.
You will also see that descriptions for the codes are no longer included. This is a result of recent negotiations with the AMA on use of the codes.
We will publish information about new BCBS groups or changes to group benefits under the Group Benefit Changes heading.
For more detailed descriptions of the BCBSM policies for these procedures, please check under the Medical/Payment Policy tab in Explainer on web-DENIS. To access this online information:
- Log in to web-DENIS.
- Click on BCBSM Provider Publications & Resources.
- Click on Benefit Policy for a Code.
- Click on Topic.
- Under Topic Criteria, click on the drop-down arrow next to Choose Identifier Type and then click on HCPCS Code.
- Enter the procedure code.
- Click on Finish.
- Click on Search.
| Code* |
BCBSM changes to:
Basic Benefit and Medical Policy, Group
Variations Payment Policy, Guidelines
|
| UPDATES TO PAYABLE PROCEDURES |
J9035
|
Basic benefit and medical policy
Avastin® (bevacizumab)
Payable diagnoses for Avastin® (bevacizumab) have been updated. Diagnosis C17.0 and C71.9 have been added as payable for Avastin (bevacizumab).
|
| POLICY CLARIFICATIONS |
J3490
J3590
|
Basic benefit and medical policy
Enhertu (Fam-trastuzumab deruxtecan-nxki)
Effective Dec. 20, 2019, Enhertu (Fam-trastuzumab deruxtecan-nxki) is considered established for the treatment of adult patients with unresectable or metastatic HER2-positive breast cancer who have received two or more prior anti-HER2-based regimens in the metastatic setting.
This indication is approved under accelerated approval based on tumor response rate and duration of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial.
This service isn’t a covered benefit for URMBT. |
J9035
|
Basic benefit and medical policy
Bevacizumab (Avastin®)
Bevacizumab (Avastin®), HCPCS code J9035, is approved for the treatment of vulvar cancer (ICD-10 — C51.0, C51.1, C51.2, C51.8, C51.9) effective Feb. 1, 2019. The above ICD-10 diagnosis codes are payable in addition to those diagnosis already payable.
This is not a benefit for FEP and URMBT.
These diagnosis updates apply to all professional claims and to all facility claims, excluding inpatient. |
| GROUP BENEFIT CHANGES |
Rock Central LLC |
Effective March 9, 2020, the name of group number 71544 is changing from Quicken Loans Inc. to Rock Central LLC.
Rock Central LLC
Group number: 71544
Alpha prefix: PPO (IQU)
Platform: NASCO
Plans offered:
PPO, medical/surgical
CDH — HSA, FSA
Prescription drug plans
Hearing plans |

We’re rescheduling some of our provider symposium sessions, providing registration links
Due to the public health emergency caused by the outbreaks of COVID-19, we’re rescheduling some of the dates of our upcoming provider symposiums. See end of this article for the revised dates and registration links.
Blue Cross Blue Shield of Michigan and Blue Care Network’s 2020 provider symposiums, A Prescription for Success, are scheduled to begin in June.
What’s included
The morning sessions are targeted to physician office staff responsible for closing gaps related to quality measures and creating a positive patient experience. Topics include:
- The latest information about HEDIS® updates to close gaps in care, the Consumer Assessment of Healthcare Providers and Systems surveys and the Health Outcomes Survey
- Why patient experience matters: The importance of convenience to your patients, the effect on patients and your office, and how to focus on, measure and improve patient experience and satisfaction
The afternoon sessions are for coders, billers and administrative staff. Topics include:
- New coding guidelines for evaluation and management visits
- Scenarios
- Coding tips
New this year: Nurses, in addition to coders, will receive continuing education credits for attending the sessions.
Schedule of events:
- Registration begins at 8 a.m.
- The morning session starts at 8:30 a.m. (except in Marquette where the schedule will be 30 minutes later) and ends at 11:30 a.m. It includes a continental breakfast.
- Lunch is from 11:30 a.m. to 12:15 p.m.
- The afternoon session is from 12:15 to 1:15 p.m.
Locations and registration links
Below is the current schedule of events and registration links. You can register for the full day or choose to attend just the morning or afternoon session. Every person must register for the session of their choice.
The Hagerty Center: 715 E. Front St., Traverse City
Date: Tuesday, June 2
Register for the morning session
Register for the afternoon session
Register for both sessions
Mid-Michigan College: 2600 S. Summerton Road, Mt. Pleasant
Date: Wednesday, June 3
Register for the morning session
Register for the afternoon session
Register for both sessions
Frankenmuth Credit Union Event Center: 11600 N. Beyer Road, Birch Run
Date: Thursday, June 18
Register for the morning session
Register for the afternoon session
Register for both sessions
Holiday Inn Marquette: 1951 U.S. 41 West, Marquette
Date: Tuesday, June 23
Register for the morning session
Register for the afternoon session
Register for both sessions
Weber’s Hotel and Restaurant: 3050 Jackson Road, Ann Arbor
Date: Tuesday, July 14
Register for the morning session
Register for the afternoon session
Register for both sessions
Fetzer Center: 2251 Business Court, Kalamazoo
Date: Wednesday, July 15
Register for the morning session
Register for the afternoon session
Register for both sessions
Laurel Manor: 39000 Schoolcraft, Livonia
Date: Tuesday, July 21
Register for the morning session
Register for the afternoon session
Register for both sessions
Century Banquet Center: 33204 Maple Lane, Sterling Heights
Date: Wednesday, July 22
Register for the morning session
Register for the afternoon session
Register for both sessions
The MTG Space: 4039 Legacy Parkway, Lansing
Date: Tuesday July 28
Register for the morning session
Register for the afternoon session
Register for both sessions
HEDIS® is a registered trademark of the National Committee for Quality Assurance.
New quantity limits coming for migraine medication
Starting July 1, 2020, Blue Cross Blue Shield of Michigan and Blue Care Network will have new quantity limits for the migraine medications listed below. The new quantity limits follow U.S. Food and Drug Administration-approved dosing guidelines to help prevent unsafe use.
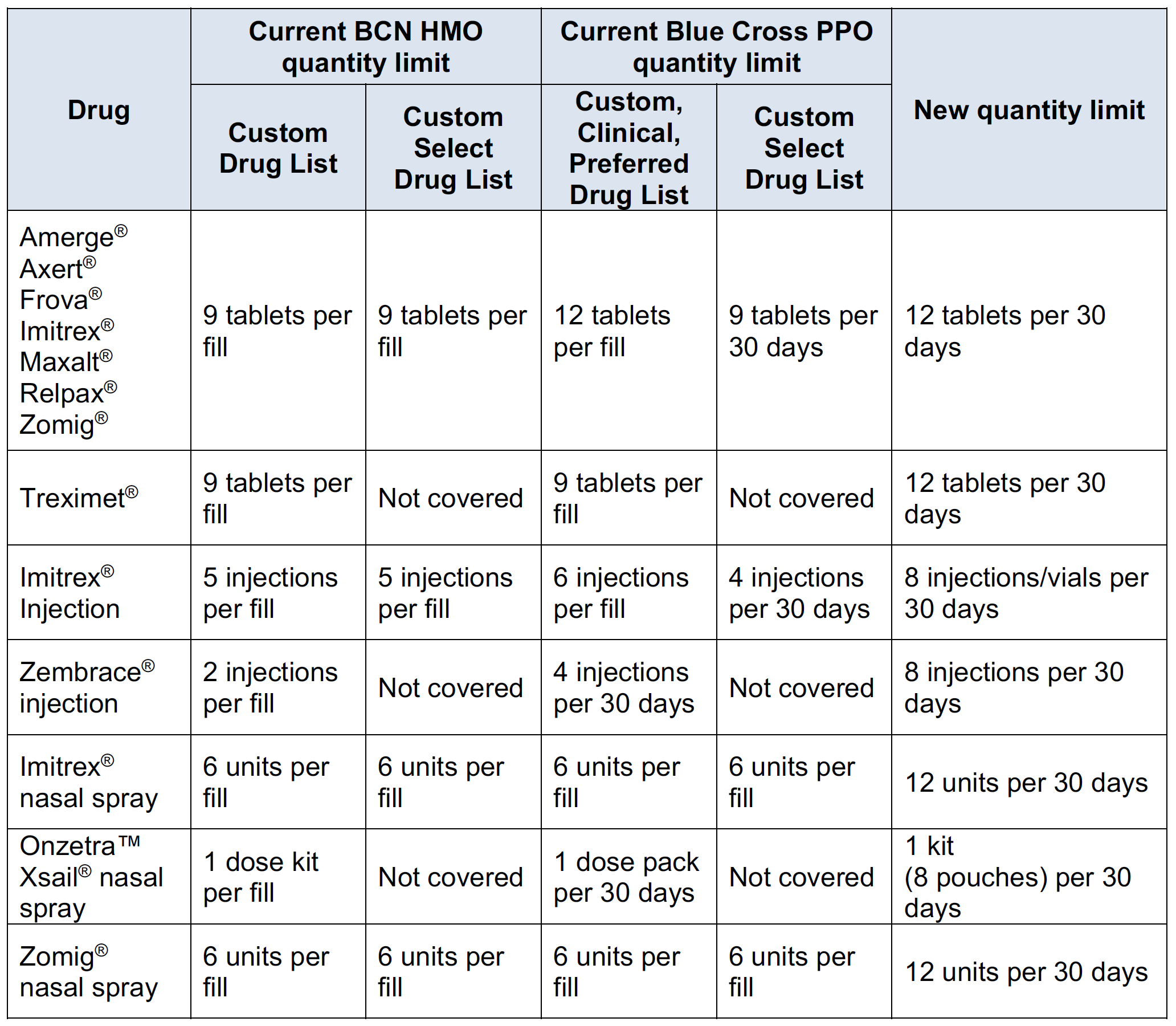
Members who are currently taking one of these medications may continue to receive it but must request approval if the use exceeds the new quantity limit.
We’ll notify affected members of these changes and encourage them to talk with their providers about treatment options. Also, we’ll tell them to talk with their providers about this change if they:
- Take a greater quantity than listed
- Need to increase the quantity
- Aren’t sure about the quantity they take
Starting July 1, we’ll change how we cover some medications that treat nausea and vomiting
Starting July 1, 2020, Blue Cross Blue Shield of Michigan and Blue Care Network will change how we cover the medications listed below.
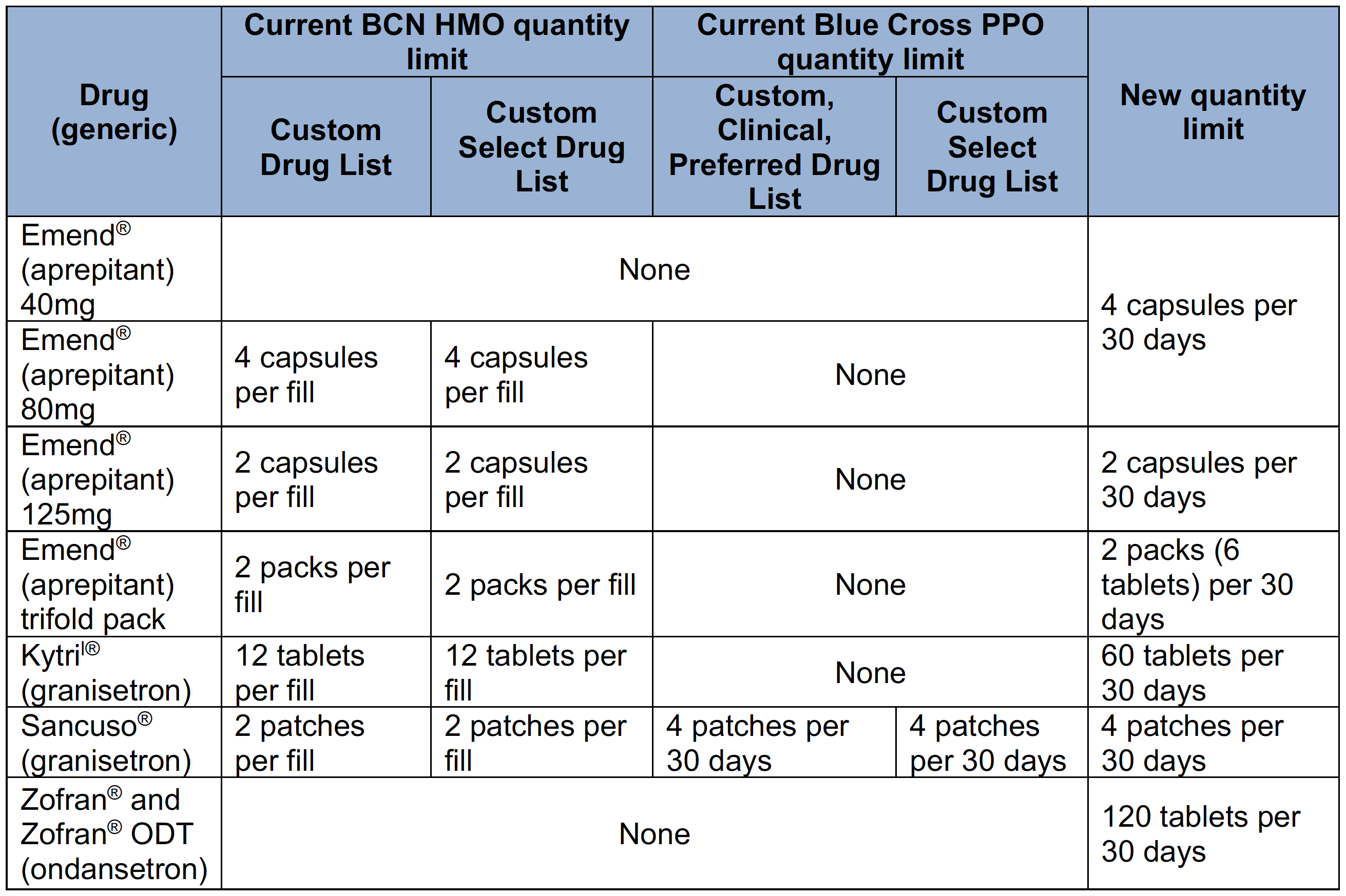
The medication in the following table is excluded. Members who currently receive this medication will need to get a prescription for one of the covered alternatives, also listed below.
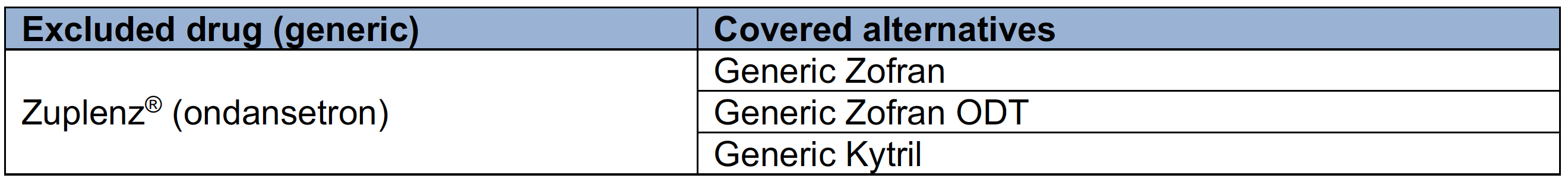
We’ll notify affected members of these changes and encourage them to talk with their providers about treatment options.
Providers rate online tools in recent survey
We recently conducted a survey as part of an effort to improve online tools for health care providers. Results highlighted the many features you like as well as suggested improvements.
Here’s what providers said they like about our secure provider website:
- There are minimum system outages.
- Providers receive adequate web support.
- Providers like that they:
- Only need a name and date of birth for a member search in web-DENIS
- Can access coordination of benefit information
- Can check claim status for dependents
- Can obtain claim status information
- Have access to our electronic referral and authorization system
Room for improvement
Survey respondents identified opportunities to improve our provider web tools. Specifically, respondents said they want:
- The ability to check referral and authorization requirements by patient at a CPT code level
- Consistent benefit and eligibility functionality across all product lines
- Access to a graphic of a real patient ID card (both front and back)
- Benefit Explainer to be easier to use
- An accumulator for counting patient visits for services with limits
- A search function for content on the website
- An automated claims appeal process
- The ability to scan and upload documents when needed
Next steps
We’re exploring options for improving our provider web tools while keeping the features you like. We hope to announce improvements in a future issue of this newsletter. Stay tuned.
How we conducted the survey
We conducted an online survey in September 2019 with follow-up interviews by an outside research firm. We targeted physicians and office and hospital staff members responsible for obtaining patient information from our website. A total of 159 people responded; 27 participated in an in-depth interview.
Sign up for next training webinar
Provider Experience is continuing its series of training webinars for health care providers and staff. The webinars are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network.
Here’s how to register for the next one:
| Webinar name |
Date and time |
Registration |
| Blue Cross 101 — Understanding the Basics |
Tuesday, May 12,
10 to 11:30 a.m. |
Click here to register. |
As additional training webinars become available, we’ll communicate about them through The Record, BCN Provider News or web-DENIS.
Update Provider Authorization form when changes occur
Blue Cross Blue Shield of Michigan is dedicated to safeguarding the protected health information of our members. Actions such as completing a Trading Partner Agreement and Provider Authorization form have become part of the electronic data interchange setup process. All EDI trading partners must complete a TPA and Provider Authorization form before exchanging PHI with Blue Cross.
Terms of the TPA require you to notify Blue Cross of any changes in your trading partner information. If you switch service bureaus (clearinghouses), software vendors, billing services or the recipient for your 835 files, you must update your Provider Authorization form. Updating the form ensures information is routed to the appropriate destination. You don’t need to update the Provider Authorization form if your submitter and Trading Partner IDs don’t change.
You should review the information on your Provider Authorization form if you’ve:
- Joined a new group practice
- Left a group practice and now bill using your own NPI
- Hired a new billing service
- Started submitting claims through a clearinghouse or you’ve changed clearinghouses
- Decided you no longer want to receive 835 remittance files
- Selected a new destination for your 835s
You must update your Provider Authorization form if you’ll be sending claims using a different submitter ID or route your 835s to a different unique receiver or Trading Partner ID. To change your EDI setup, go to bcbsm.com/providers and follow these steps:
- Click on Quick Links.
- Click on Electronic Connectivity (EDI).
- Click on How to use EDI to exchange information with us electronically.
- Click on Update your Provider Authorization Form under EDI Agreements.
If you have any questions about EDI enrollment, contact the EDI Help Desk at
1-800-542-0945. For assistance with the TPA and Provider Authorization form, select the TPA option.
Interventional pain management services for *64451 and *64625 require authorization starting May 1
Services associated with procedure codes *64451 and *64625 will require authorization by eviCore healthcare for dates of service on or after May 1, 2020. We had first let health care providers know about this in web-DENIS message and a news item on ereferrals.bcbsm.com in February.
This requirement applies to all Blue Cross Blue Shield of Michigan and Blue Care Network members with plans subject to eviCore healthcare authorization requirements as follows:
- Blue Cross PPO
- Medicare Plus BlueSM PPO
- BCN HMOSM
- BCN AdvantageSM
For more details, see the web-DENIS message posted on Feb. 10, 2020. If you have any questions, contact your provider representative.
Medicare Plus Blue PPO defines modifier 55 in update
Medicare Plus BlueSM PPO updated its claims information in October 2019 to include the following definition of modifier 55:
- Indicate a physician, other than the surgeon, is billing for part of the outpatient postoperative care
- Also, used by the surgeon when providing only a portion of the post-discharge postoperative care
According to the Modifier 55 Fact Sheet, the Centers for Medicare & Medicaid Services requires health care providers to file a beginning and end date for the postoperative care.
LabCorp added to Medicare Plus Blue PPO lab network
The Medicare Plus BlueSM PPO laboratory network includes LabCorp as of Aug. 1, 2019. LabCorp, along with Quest Diagnostics and JVHL, provides lab services to Medicare Plus Blue members.
Medicare Plus Blue referring physicians must use the lab network for all outpatient lab and pathology services (facilities – nonpatient only). Using the Medicare Plus Blue lab network also minimizes out-of-pocket costs for members.
For LabCorp’s patient service center locations, visit labcorp.com** or call LabCorp’s administrative offices at 1-888-LabCorp (1-888-522-2677).
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Announcing claim editing updates to our screening policy for abdominal aortic aneurysms
In December 2018 and April 2019, Blue Cross Blue Shield of Michigan made updates to our claim editing processes for select groups. When we informed you of these changes, we let you know that we were doing this to:
- Promote correct coding
- Make our claims payment system easier for you and your billing staff to navigate
We’ve also made updates to our claim editing system for screenings for abdominal aortic aneurysms (CPT code *76706). Please be aware that a screening for abdominal aortic aneurysms isn’t recommended for the following patients and, as a result, you may experience claim denials:
- A female patient and a diagnosis of family history of abdominal aortic aneurysms isn’t present on the claim.
- A male patient younger than age 65 and a diagnosis of family history of abdominal aortic aneurysms isn’t present on the claim.
- A male patient older than age 75 and a diagnosis of family history of abdominal aortic aneurysms isn’t present on the claim.
Note: For an ultrasound or duplex ultrasound of the abdominal aorta other than screening, use CPT codes *76770, *76775, *93978 and *93979.
If you have questions about the Blue Cross’ claim editing process, contact Provider Inquiry – Professional at 1-800-344-8525 or Provider Inquiry – Facility at 1-800-249-5103.
Educate members about cancer statistics, remind them of need for preventive screenings
In 2020, the American Cancer Society estimates there will be 1,806,950 new cancer cases and 606,520 cancer deaths in the U.S.
Here are statistics from the ACS for three common cancer types in 2020 and previous years:
| Cancer type |
Estimated new cases, 2020 |
Estimated deaths, 2020 |
| Breast |
279,100 |
42,690 |
| Cervix |
13,800 |
4,290 |
| Colorectum |
147,950 |
53,200 |
Incidence and death rates for previous years:
| Cancer type |
Incidence rates 2012-2016
(per 100,000)
|
Death rates 2013-2017
(per 100,000)
|
| Breast |
125.3 |
20.3 |
| Cervix |
7.6 |
2.3 |
| Colorectum |
38.7 |
13.9 |
Regular screening for breast, cervical and colorectal cancer and increased knowledge of symptoms among patients have led to earlier detection and fewer deaths.
Consider these statistics from the National Cancer Institute:
- Between 1989 and 2017, the death rate for breast cancer declined 40%.
- Since the mid-1970s, the death rate for cervical cancer dropped more than half.
- From 1970 to 2017, the death rate for colorectal cancer dropped 54%.
By screening for cancer and modifying risk factors, thousands of additional cancer cases and deaths can be prevented. Approximately 42% of cancer cases and 45% of deaths are attributed to modifiable risk factors.
Visit the NCI website** for more information on modifiable risk factors to share with your patients.
A note from the Federal Employee Program®
FEP members’ mammograms, cervical cancer and colorectal screenings are covered once per calendar year with no out-of-pocket cost. Additional information on FEP cancer screening benefits can be found online at www.fepblue.org or by calling Customer Service at 1-800-482-3600.
As a reminder, non-FEP members can log in to their member account or call the number on the back of their member ID card for benefit information.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
CDC campaign seeks to improve antibiotic prescribing and use
More than 2.8 million antibiotic-resistant infections occur in the United States each year, with 35,000 people dying as a result, according to the Centers for Disease Control and Prevention. This has made improving antibiotic prescribing and use a national priority.
“Be Antibiotics Aware” is the CDC’s national campaign to help fight antibiotic resistance and improve antibiotic prescribing and use.
By raising awareness, the CDC aims to:
- Improve the way health care professionals prescribe antibiotics.
- Educate patients on when and how to take antibiotics.
- Fight antibiotic resistance and ensure these life-saving drugs will be available in the future.
When antibiotics are carefully used and prescribed, we can combat antibiotic resistance.
To learn more about antibiotic use, patient education and more, visit the Antibiotic Prescribing and Use** page on the CDC website.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Reminder: Guidelines for using Advance Notice of Member Responsibility form
As a reminder, all professional, non-Medicare claims that include the modifiers GY or GZ, along with modifier GA, will be rejected and the member will be responsible for paying for the services provided.
Blue Cross Blue Shield of Michigan adopted the Centers for Medicare & Medicaid Services’ Advance Beneficiary Notice policy and refers to it as Advance Notice of Member Responsibility. Health care providers should include the GA modifier on all claims, including Not Otherwise Classified and Unlisted Procedure Codes, billed with a GY or GZ modifier, which will acknowledge that:
- The services are expected to be rejected.
- The member was informed and agreed to accept total responsibility.
- An ANM responsibility form was signed before services were rendered and is on file.
The ANM billing guidelines don’t apply to Medicare supplemental and MESSA group member claims.
If providers don’t include the GA modifier on claims appended with a GY or GZ, they’ll be held responsible for the cost of the services.
Providers must present an Advance Notice of Member Responsibility form to the Blue Cross members before providing medical services or supplies that are expected to be rejected. This form can be found on the BCBSM Newsletters and Resources web-DENIS page under Forms.
For the notice to be acceptable, a provider must:
- Complete the form in its entirety.
- Clearly identify the specific item or service that’s expected to be denied.
- State the specific reason that Blue Cross will deny payment for the item or service.
- Indicate the estimated cost of the item or service that’s associated with the denied claim and the member’s responsible amount.
The form should be issued before rendering a service or dispensing durable medical equipment, prosthetics and orthotics, or medical supplies that Blue Cross isn’t expected to cover. This form doesn’t supersede or change any member’s benefits.
Here are some reasons the medical claims for those items may be rejected:
- Blue Cross medical criteria haven’t been met.
- Blue Cross doesn’t usually pay for this quantity of treatments or services.
- Blue Cross doesn’t usually pay for this service.
- Blue Cross doesn’t pay for this service because it’s a treatment that hasn’t been proven safe or effective.
- Blue Cross doesn’t pay for this quantity of services within this time period.
- Blue Cross doesn’t pay for such an extensive treatment.
- Blue Cross doesn’t pay for this medical equipment for the illness or condition stated.
If a provider properly issues a notice, the member will be held financially liable for the reason indicated above on the signed form. Keep in mind that a provider who fails to properly issue a notice will be held liable for the medical service. The provider won’t be allowed to bill or collect funds from the member, and the provider must refund money collected from the member.
Other important information about the Advance Member Notice of Responsibility form
- For an extended course of treatment, a member responsibility form is valid for one year. If the course of treatment extends beyond one year, a new form is required each year for the remainder of the treatment.
- Once signed by the member, a member responsibility form may not be modified or revised. When a member must be notified of new information, a new form must be provided and signed.
Correction: Using network labs for your patients
We need to correct some information that was in an article in the June 2019 issue of The Record and provide additional clarification. The chart in the article, which provided information about independent labs to be used by our members, should have indicated that GM and Ford hourly employees, not salaried employees, must use Quest Diagnostics. GM and Ford salaried employees can find a contracted lab by using the Find a Doctor tool on bcbsm.com.

Sign up for next training webinar
Provider Experience is continuing its series of training webinars for health care providers and staff. The webinars are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network.
Here’s how to register for the next one:
| Webinar name |
Date and time |
Registration |
| Blue Cross 101 — Understanding the Basics |
Tuesday, May 12,
10 to 11:30 a.m. |
Click here to register. |
As additional training webinars become available, we’ll communicate about them through The Record, BCN Provider News or web-DENIS.
Update Provider Authorization form when changes occur
Blue Cross Blue Shield of Michigan is dedicated to safeguarding the protected health information of our members. Actions such as completing a Trading Partner Agreement and Provider Authorization form have become part of the electronic data interchange setup process. All EDI trading partners must complete a TPA and Provider Authorization form before exchanging PHI with Blue Cross.
Terms of the TPA require you to notify Blue Cross of any changes in your trading partner information. If you switch service bureaus (clearinghouses), software vendors, billing services or the recipient for your 835 files, you must update your Provider Authorization form. Updating the form ensures information is routed to the appropriate destination. You don’t need to update the Provider Authorization form if your submitter and Trading Partner IDs don’t change.
You should review the information on your Provider Authorization form if you’ve:
- Joined a new group practice
- Left a group practice and now bill using your own NPI
- Hired a new billing service
- Started submitting claims through a clearinghouse or you’ve changed clearinghouses
- Decided you no longer want to receive 835 remittance files
- Selected a new destination for your 835s
You must update your Provider Authorization form if you’ll be sending claims using a different submitter ID or route your 835s to a different unique receiver or Trading Partner ID. To change your EDI setup, go to bcbsm.com/providers and follow these steps:
- Click on Quick Links.
- Click on Electronic Connectivity (EDI).
- Click on How to use EDI to exchange information with us electronically.
- Click on Update your Provider Authorization Form under EDI Agreements.
If you have any questions about EDI enrollment, contact the EDI Help Desk at
1-800-542-0945. For assistance with the TPA and Provider Authorization form, select the TPA option.
Medicare Plus Blue PPO defines modifier 55 in update
Medicare Plus BlueSM PPO updated its claims information in October 2019 to include the following definition of modifier 55:
- Indicate a physician, other than the surgeon, is billing for part of the outpatient postoperative care
- Also, used by the surgeon when providing only a portion of the post-discharge postoperative care
According to the Modifier 55 Fact Sheet, the Centers for Medicare & Medicaid Services requires health care providers to file a beginning and end date for the postoperative care.
LabCorp added to Medicare Plus Blue PPO lab network
The Medicare Plus BlueSM PPO laboratory network includes LabCorp as of Aug. 1, 2019. LabCorp, along with Quest Diagnostics and JVHL, provides lab services to Medicare Plus Blue members.
Medicare Plus Blue referring physicians must use the lab network for all outpatient lab and pathology services (facilities – nonpatient only). Using the Medicare Plus Blue lab network also minimizes out-of-pocket costs for members.
For LabCorp’s patient service center locations, visit labcorp.com** or call LabCorp’s administrative offices at 1-888-LabCorp (1-888-522-2677).
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Correction: Using network labs for your patients
We need to correct some information that was in an article in the June 2019 issue of The Record and provide additional clarification. The chart in the article, which provided information about independent labs to be used by our members, should have indicated that GM and Ford hourly employees, not salaried employees, must use Quest Diagnostics. GM and Ford salaried employees can find a contracted lab by using the Find a Doctor tool on bcbsm.com.
DRG coding validation audits begin in June for Medicare Plus Blue claims
Beginning June 1, 2020, SCIO Health Analytics, an independent company that provides auditing services for Blue Cross Blue Shield of Michigan, will perform audits on Medicare Plus BlueSM hospital diagnosis‑related group paid claims.
The audits will:
- Review data going back one year.
- Base the look-back date on the date the claim was paid.
- Require providers to submit medical charts.
The audits will only focus on DRG coding validation, not clinical validation.
Medical records will be reviewed to:
- Detect, prevent and correct fraud, waste and abuse.
- Facilitate accurate claim payments.
Before an audit, be ready to share medical charts for review. After an audit, SCIO will send you a letter with the findings and information on how to request an appeal.
You may speak with a SCIO representative during an audit by calling 1-866-628-3488.
Follow these guidelines for audits of catastrophic cases
Please use the following information as a guide for what to expect and do for your hospital’s next utilization review of catastrophic cases.
Blue Cross Blue Shield of Michigan sends appointment letters to the hospital at least 30 days in advance of the audit, listing the cases to be audited and the items required to conduct the audit.
Audits of catastrophic cases require:
- The complete medical record
- Progress notes
- Medication administration sheets organized by date order
The file needs to include emergency room records, outpatient procedures, the utilization review worksheets and a copy of the most current itemized bill.
Blue Cross will only consider adjustments, late charge claims reported with frequency code 5 or replacement claims reported with frequency code 7 if billed to the catastrophic claim 30 or more days before the audit. This allows Blue Cross to finalize the late charge or replacement claim adjustments and post the new claim information to our financial systems before the scheduled audit.
Late charge or replacement adjustment claims reported less than 30 days of the scheduled audit won’t be considered in the catastrophic outlier audit.
If the audit is conducted at your site and you have electronic medical records, please provide:
- One computer for each auditor
- An individual access or login permission for each auditor
The auditor will need someone from your staff to help him or her access and navigate your electronic medical record.
Each auditor will also need an electrical outlet for his or her Blue Cross computer and a telephone in the designated audit room.
If the audit is conducted at our offices and you grant us web access, we require an individual login for each auditor and a contact person who can help access the electronic record.
The Blue Cross auditor usually makes a courtesy call to the hospital contact person before beginning the audit to answer questions that may occur during the preparation.
We’ll provide you with daily deletion sheets during the audit so you have the opportunity to gather additional supporting documentation. While onsite, the auditor will identify the itemized bills to be mailed to Blue Cross.
We’ll need the name, title and email address of the person who should receive the reporting letter. The hospital staff has the responsibility to share audit findings with other individuals or departments in the hospital.
After you receive the reporting letter, you have the opportunity to provide clarification or missing documentation during the appeal process. Hospitals are allowed 50 calendar days from receipt of the audit reporting letter to submit a written request for internal review.
Need more information?
For more information on reviews of catastrophic cases, see your online provider manual. Refer to the chapter titled Catastrophic case review – Peer Groups 1-4 (Inpatient hospital facility).
Reminder: Be sure to include occurrence code 11 and onset date when billing for medical emergencies
When billing for a medical emergency or accidental illness, facility providers should be sure to report occurrence code 11 on their claim and include the onset date of the condition. This is important because Blue Cross Blue Shield of Michigan benefit policy doesn’t allow payment of outpatient facility claims for these services when the onset date of a patient’s symptoms (or illness) is more than 72 hours before the date of service on a claim.
Making sure that you include the occurrence code and onset date — and bill according to our benefit policy — helps reduce potential claim rejections and overpayment recoveries.
Consult your provider manual for more information on billing and coding.
Home health care moratorium has been lifted
In 2019, the Centers for Medicare & Medicaid Services lifted its home health care moratorium that had prevented new home health agencies from enrolling in Medicare and Medicaid. Blue Cross Blue Shield of Michigan has reviewed the CMS procedures and guidelines for home health agencies and implemented internal procedures to ensure that we are consistent in our review and approval processes for new and existing home health care providers.
Home health care facilities are now eligible to enroll in Traditional, Medicare Plus BlueSM, Blue Care Network and BCN AdvantageSM networks. To submit and review required documentation, enrollment and change forms, visit bcbsm.com/providers, scroll down to Prepare to Enroll and then click on Enroll now.
If you have any questions regarding the Blue Cross and Blue Care Network enrollment and change process, contact Provider Enrollment at 1-800-822-2761.

New quantity limits coming for migraine medication
Starting July 1, 2020, Blue Cross Blue Shield of Michigan and Blue Care Network will have new quantity limits for the migraine medications listed below. The new quantity limits follow U.S. Food and Drug Administration-approved dosing guidelines to help prevent unsafe use.
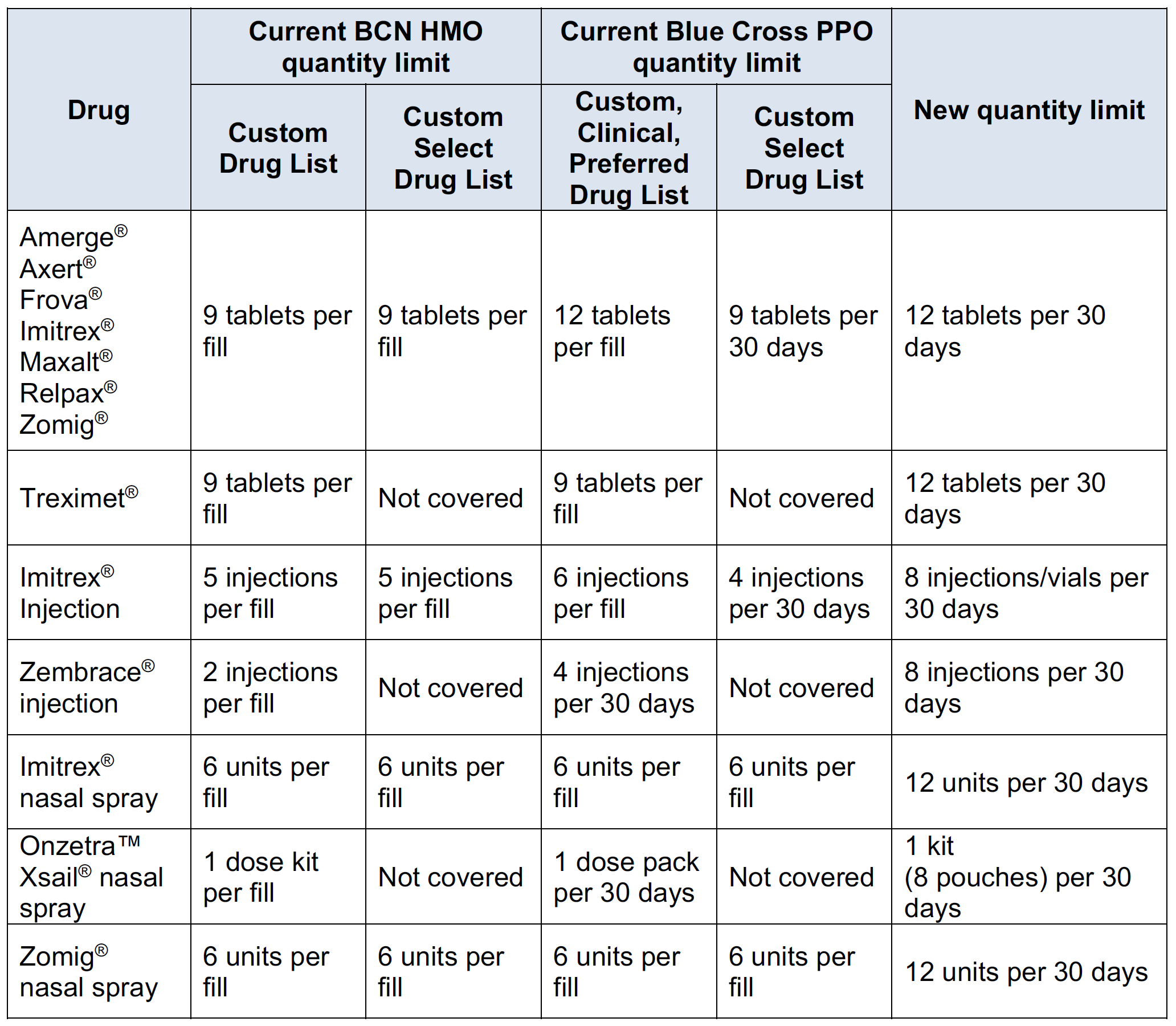
Members who are currently taking one of these medications may continue to receive it but must request approval if the use exceeds the new quantity limit.
We’ll notify affected members of these changes and encourage them to talk with their providers about treatment options. Also, we’ll tell them to talk with their providers about this change if they:
- Take a greater quantity than listed
- Need to increase the quantity
- Aren’t sure about the quantity they take
Starting July 1, we’ll change how we cover some medications that treat nausea and vomiting
Starting July 1, 2020, Blue Cross Blue Shield of Michigan and Blue Care Network will change how we cover the medications listed below.
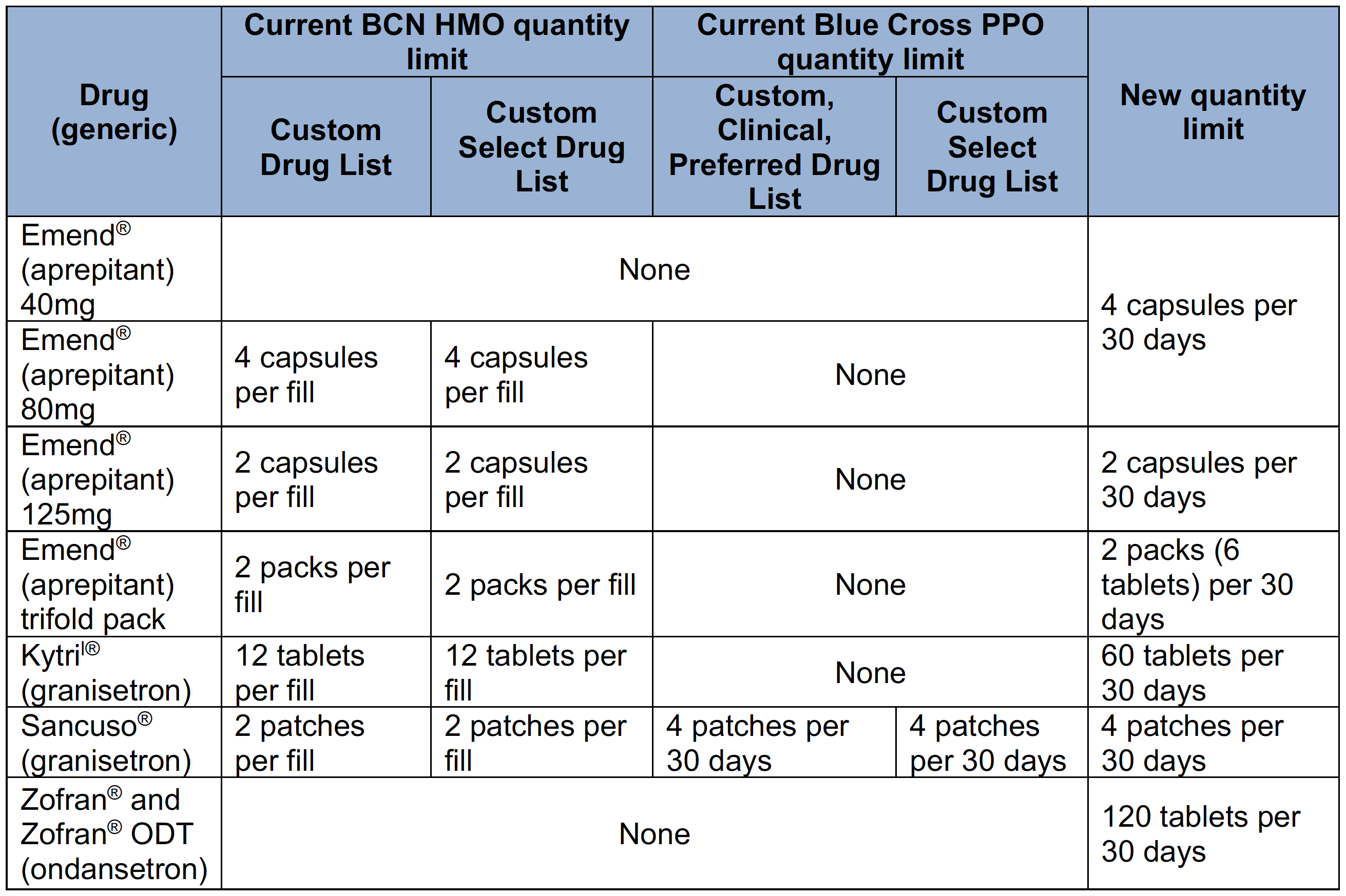
The medication in the following table is excluded. Members who currently receive this medication will need to get a prescription for one of the covered alternatives, also listed below.
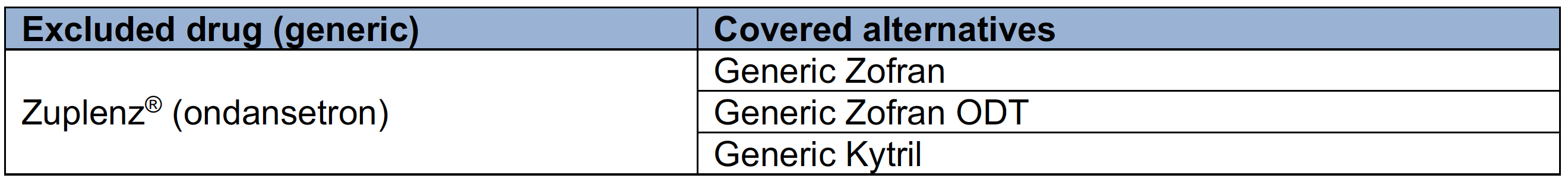
We’ll notify affected members of these changes and encourage them to talk with their providers about treatment options.
| 

