
|
||
|---|---|---|
|
|
||
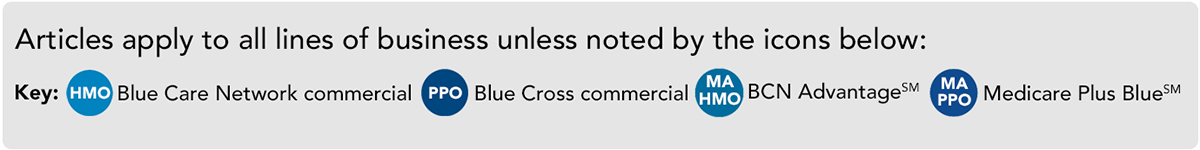
This newsletter includes short summaries, reminders and updates for Blue Cross and BCN providers. Please visit The Record or BCN Provider News for complete newsletter editions.
Update: We’re aligning local rules for acute inpatient medical admissions For certain conditions, authorization requests for acute medical admissions should be submitted only after the member has spent two days in the hospital. Once the two days has elapsed, the facility can submit the request to authorize an inpatient admission on the third day. You must provide clinical documentation that demonstrates that the InterQual® criteria have been met at the time you submit the request. Read more: Holiday office closings Blue Cross and BCN offices will be closed Dec. 23 through Dec. 24 and Dec. 30 through Dec. 31. Prior authorization requirements expanding for Medicare Plus Blue℠, BCN commercial and BCN Advantage members on Jan. 1 We’re expanding our prior authorization requirements for Medicare Plus Blue, BCN commercial and BCN Advantage℠ members. For certain procedure codes, you’ll need to complete questionnaires in the e-referral system when you submit prior authorization requests for dates of service on or after Jan. 1, 2022. Read more: Here’s what you need to know about DRG readmission processing and how to provide input Blue Cross is proposing an enhancement to DRG readmission processing. This improvement is scheduled for implementation on March 1, 2022, for Blue Cross commercial members. The program update will identify inpatient readmission claims prior to payment. Read more: December 2021 issue of The Record Prior authorization requests for commercial SNF admissions will need to be submitted through e‑referral system Beginning Jan. 1, 2022, we’ll require skilled nursing facilities to submit prior authorization requests through the e-referral system and not by fax. This applies to requests for initial admissions and additional days. Read more:
Behavioral Health updates Behavioral health services delivered via synchronous telemedicine Read more: Intensive outpatient program and partial hospital program services now payable via telemedicine on an ongoing basis Read more: Additional autism interventions now payable via telemedicine on an ongoing basis and restrictions are removed from protocol modification Read more: Update: CADC, CAADC credentials not required for facilities that treat substance use disorders Read more: | ||
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. |