Services That Need Prior Authorization
Blue Cross Blue Shield of Michigan and Blue Care Network require prior authorization for certain benefits. This means we need to review a service to be sure it is medically necessary and appropriate.
If a service requires prior authorization, it's important to make sure that your provider receives the prior authorization before you receive the services. If you receive those services without prior authorization, the service may not be covered. If a service isn't covered, we'll pay nothing and you may have to pay up to the full amount of the provider’s charge.
If a prior authorization is required for your medical service, your doctor or health care professional must submit the prior authorization request. Note that only your doctor or health care professional can submit the request; you will not be allowed to submit it yourself. Once we get the request and supporting medical records, we will begin the review process.
If you're looking for more information about prescription drug prior authorization, or how to file a coverage review request, read Why do I need prior authorization for a prescription drug?
There are four types of review for health care services:
- Prior authorization non-urgent review: When you need to get a certain health care service, but it is not urgent. It can take up to seven days for us to make our decision. This is the most common type of prior authorization request. Decisions may take longer if your provider does not submit all the information that we need to review the request. We will collaborate directly with your provider to get all the necessary information to make the best decision.
- Prior authorization urgent review: When you need to get a certain health care service as soon as possible, but it is not an emergency. It can take up to three days for us to make our decision.
- Urgent concurrent review: When you are already getting care, your provider may ask us to approve further services to help treat you. This usually occurs after a person has been stabilized in the emergency room and needs to be admitted to the hospital for further treatment. It can take up to 72 hours for us to make our decision.
- Postservice review: When your provider submits an authorization request after you have already gotten the care you need. It can take up to 30 days for us to decide.
These time limits may differ for Medicare and Blue Cross and Blue Shield Federal Employment Program® members.
If you disagree with our decision, you can appeal.
For more information on prior authorization for Michigan Education Special Services Association, or MESSA, members, visit the MESSA website.
Do you need prior authorization?
Services summary
If you have a Blue Cross Blue Shield of Michigan PPO or Blue Care Network HMO plan, our Procedure codes for which providers must request prior authorization (PDF) shows the services that require prior authorization before you receive them.
A prior authorization is not a guarantee of benefits or payment. Please check your member eligibility and benefits and medical policy coverage guidelines.
Clinical review criteria
Blue Cross and BCN use evidence-based clinical standards of care to help determine whether a benefit may be covered under the member’s health plan.
The criteria to determine if a service is medically necessary can be accessed on our Medical Policy Router Search page and in additional criteria.
Additional information on specific certain procedures is available in Preview questionnaires and medical necessity criteria (PDF).
Prior authorization requests
Prior authorization requests managed by BCBSM and BCN of medical and surgical services
Blue Cross and BCN use the following:
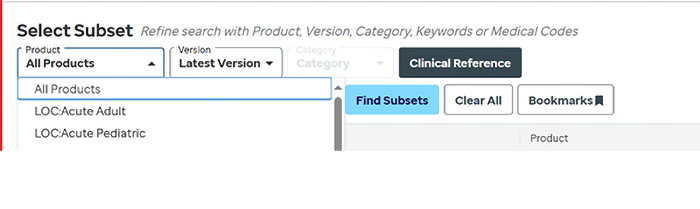
- For acute medical and surgical inpatient requests: Nationally recognized InterQual® medical necessity criteria select:
- LOC: Acute Adult
- LOC: Acute Pediatric
- For post-acute care requests:
- LOC: Long-Term Acute Care
- LOC: Inpatient Rehabilitation
- LOC: Subacute/SNF
- Local rules: We sometimes modify InterQual criteria for certain services. These modifications are called local rules. To view our modification to InterQual criteria for post-acute care services, see the following:
- For select elective inpatient and outpatient services select:
- CP: Procedures
Sign up or log in to One Healthcare ID to view InterQual criteria for medical and surgical services.
Providers/Members should select a “Product” under the Select Subset menu to view criteria.
Behavioral Health Services (effective Jan. 1, 2024)
Blue Cross Behavioral HealthSM manages behavioral health prior authorizations and case management services for Blue Cross commercial and BCN commercial members. The medical necessity criteria used are the same for all members.
The following guidelines are used for all lines of business:
- Level of Care Utilization System (LOCUS) (PDF) - To evaluate behavioral health treatment requests for adults age 19+
- Child and Adolescent Level of Care Utilization System (CALOCUS) (PDF) - To evaluate mental health treatment requests for children and adolescents ages 6 – 18 years
- Early Childhood Service Intensity Instrument (ECSII) (PDF) - To evaluate mental health treatment requests for infants, toddlers, and children ages birth through 5 years
- ASAM Criteria (PDF) - To evaluate substance use disorder service and treatment requests for dates of service from April 1, 2023, through March 31, 2024
- The ASAM Criteria, Fourth Edition - To evaluate substance use disorder service and treatment requests for dates of service on or after April 1, 2024, scroll to the “What’s new in The ASAM Criteria, Fourth Edition?” section.
- Applied behavior analysis
- Applied Behavior Analysis (ABA) Supplemental Policy (PDF) — For dates of service on or after Jan. 1, 2026
- Applied Behavior Analysis (ABA) Supplemental Policy (PDF) — For dates of service from April 22, 2025, through Dec. 31, 2025
- Applied Behavior Analysis (ABA) Supplemental Policy (PDF) — For dates of service from Jan. 1, 2024, through April 21, 2025
Outside review of prior authorization requests
Prior authorization requests for certain types of services are sometimes reviewed by outside vendors.
- Cardiology: Carelon Medical Benefits Management Cardiology Guidelines
- Echocardiogram: Carelon Imaging of the Heart
- High-tech radiology: Carelon Radiology Guidelines
- In-lab sleep management: Carelon Sleep Guidelines
- Musculoskeletal services: TurningPoint Healthcare Solutions
- Proton beam therapy: Carelon Proton Beam Therapy
- Radiation oncology: EviCore by Evernorth® Radiation Oncology Solution
- Cardiology: Carelon Cardiology Guidelines
- Echocardiogram: Carelon Imaging of the Heart
- High-tech radiology: Carelon Radiology Guidelines
- Musculoskeletal services: TurningPoint
- PT, OT, ST and physical medicine services: EviCore Musculoskeletal Therapies
- Radiation oncology: EviCore Radiation Oncology Solution
Additional information for providers
Before providing services, make sure you check benefits and eligibility and medical policy coverage guidelines, using the self-service tools on Availity Essentials™.
If you have questions, please contact Provider Inquiry from 8:30 a.m. to noon or 1 to 5 p.m., Monday through Friday:
- Professional: 1-800-344-8525
- Facility: 1-800-249-5103
Michigan provider prior authorization
Providers can get information on how to request a prior authorization through Availity Essentials.
You can view benefit details through Benefit Explainer. This is available on the Applications tab within the Blue Cross and BCN Payer Space on Availity Essentials.
You can review medical policy through our Medical Policy Router Search.
Non-Michigan provider prior authorization
Contact your local Blue Plan for information on how to submit a prior authorization request.
Providers may request prior authorization for MESSA members by visiting the MESSA website.
*Blue Cross and BCN do not own or control this website.
Availity® is an independent company that contracts with Blue Cross and BCN to offer provider portal and electronic data interchange services.
Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services. For more information, go to our ereferrals.bcbsm.com website.
EviCore by Evernorth is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services. For more information, go to our ereferrals.bcbsm.com website.
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
Questions?
Privacy issues: To report a concern or if you think your protected health information has been compromised, please call us at 1-800-552-8278 or email us. Don't include any protected health information in your email.
Other issues: For customer service, call the number on the back of your member ID card.