

Ready to help you get the most out of your plan
Explore My plans
Find care
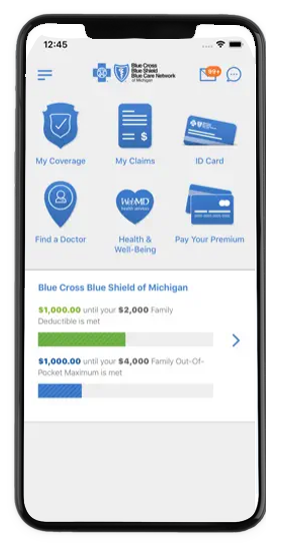
Download our mobile app
Connect with providers and manage your health and benefits securely on the go
Learn how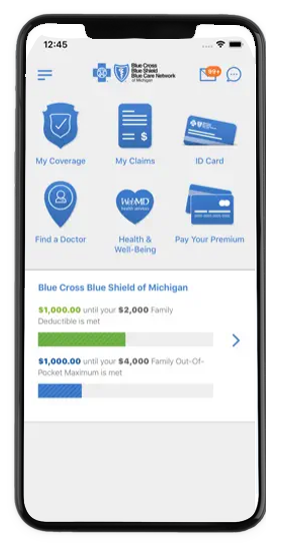
Download our mobile app
Connect with providers and manage your health and benefits securely on the go
Learn how-

Do you qualify for special enrollment?
Learn moreOur health plan advisors are ready to help with your insurance needs.
-

-

We’re here for you and your family
Learn how we can helpIf you’re losing your Medicaid coverage, find out how we can help.
A leader in health care
Through continuous innovation, Blue Cross Blue Shield of Michigan improves the quality and value of health care. Members enjoy smarter, better personalized medical, dental and vision coverage that addresses health disparities and strengthens communities across the country.



