Forward to a friend |
Subscribe | The Record Archive | Contacts | bcbsm.com | Print this article
|
July 2025
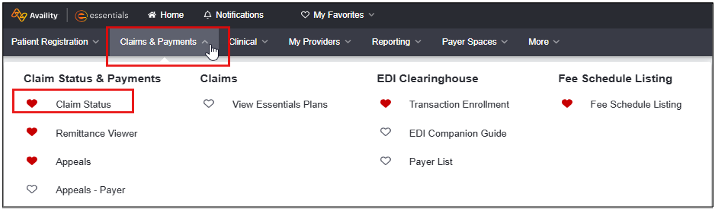
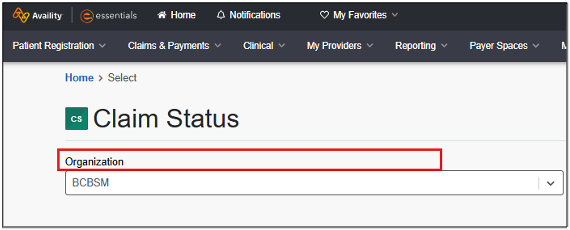
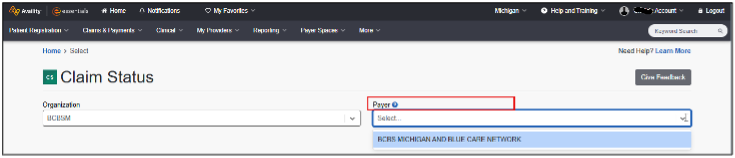
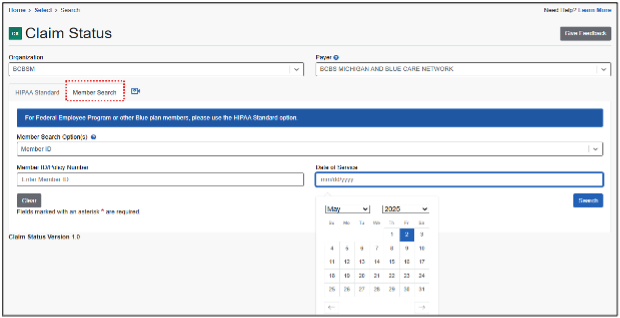
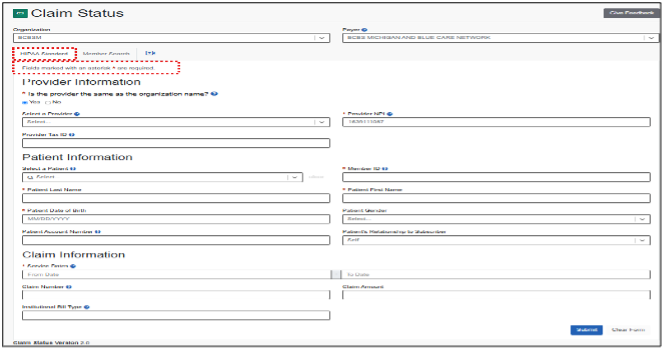
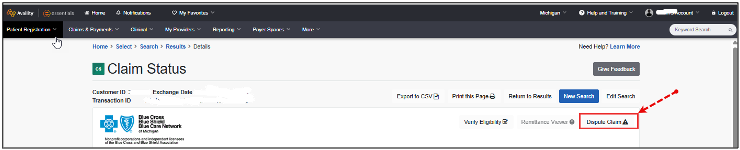
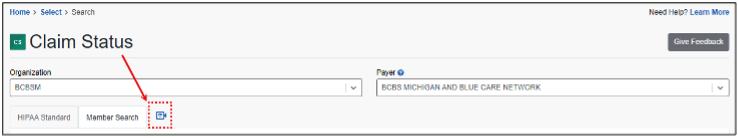
Provider portal pointersThis is an article ongoing series of tips and tricks designed to help you do your job more efficiently by getting the most out of the applications and tools available on our provider portal. Claims status inquiry process The claims status inquiry process is designed to streamline access to insurance claim statuses, identify issues and dispute claims, when necessary. Note: To conduct a claims status inquiry, administrators must first assign the user the Claims Status role using Manage My Team(s), as previously discussed on Page 9 of the May-June issue of BCN Provider News. Without this role, users will be unable to access the claims status inquiry tool within the portal. The steps to conduct a claims status inquiry are as follows:
If the user is tied to only one organization, it will be selected automatically. Those with access to multiple organizations will see all options displayed alphabetically.
Hint: In cases where a patient appears multiple times due to coverage types or group changes, select the correct record carefully.
Hint: For best search results, only enter data for required fields marked with an asterisk.
Note: Appeals are based on EX codes, which differ for each line of business. To access EX code lists for each line of business:
Additional help is available A short video demonstrating the claims status process is also available. To view the video, click the camera icon on the Claim Status page.
Help us help you If you have a suggestion for a provider portal topic you would like to see in future issues of The Record or BCN Provider News, contact us at bcnprovidernews@bcbsm.com. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. |
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|