Forward to a friend |
Subscribe | The Record Archive | Contacts | bcbsm.com | Print this article
|
April 2024
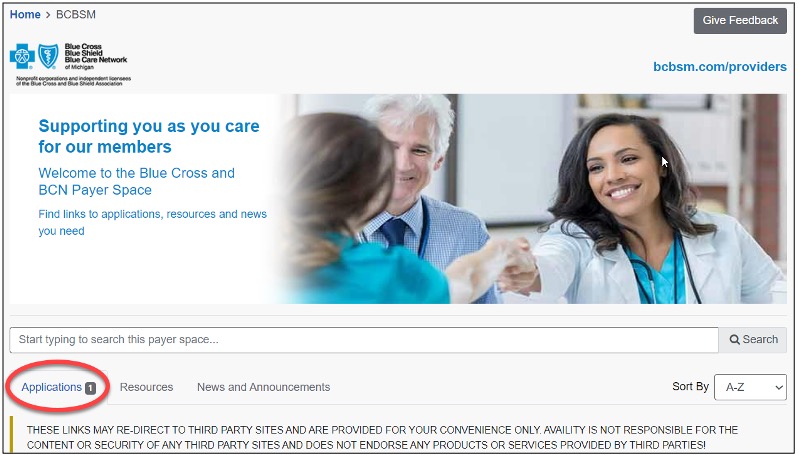
Reminder: How to check the status of prior authorization requests to share with your patientsAs a reminder, if a patient who has coverage through Blue Cross Blue Shield of Michigan or Blue Care Network asks about the status of a prior authorization request, you can check it by following these steps:
Additional information available for providers Providers can also find a summary of services that require prior authorization through our Summary of utilization management programs for Michigan providers document on ereferrals.bcbsm.com. Note: For help using the e-referral tool, go to ereferrals.bcbsm.com and, under Access & Training, click on Training Tools. **Blue Cross Blue Shield of Michigan doesn’t own or control this website. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. |
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|