Subscribe | The Record Archive | Contacts | bcbsm.com
|
September 2023
We’re connecting you to information and resources that can help prevent suicideSeptember is Suicide Prevention Awareness Month,** a time to raise awareness of this public health crisis and to help eliminate the stigma associated with it. Suicide is one of the leading causes of death in the U.S. According to the Centers for Disease Control and Prevention, 48,283 people died by suicide in 2021 (most recent verifiable data). That equates to one death every 11 minutes. Other compelling statistics from that same year:
Suicidal thoughts, much like mental health conditions, can affect almost anyone regardless of age, gender or background, according to the National Alliance on Mental Illness, or NAMI.** In fact, suicide is often the result of an untreated mental health condition. That’s why Blue Cross Blue Shield of Michigan has taken a multipronged approach to addressing mental health and substance use disorder conditions. This includes a wide array of behavioral health communications and resources for members, customers and providers. Here are three recently updated resources:
988 Suicide & Crisis Lifeline The Suicide & Crisis Lifeline provides 24/7 confidential support for people in distress. If you or someone you know is experiencing a mental health crisis, call or text 988 immediately. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Do you know about Quartet?We began using Quartet in July to assist our members who are seeking outpatient care for mental health or substance use disorders. This service, available at no extra cost to eligible members, is especially useful for people who are having difficulty locating and obtaining timely care from a behavioral health specialist in their area. Emails and other communications were sent to eligible members beginning July 11. Within three days, 300 members had contacted Quartet to receive referrals to a behavioral health specialist. If one of your patients is unsure whether they are eligible for Quartet services, you can recommend they call the Customer Service number on the back of their member ID card. Quartet’s services are available to the following adult members, 18 years or older, who reside in Michigan:
Joining the Quartet online platform Providers interested in registering on the Quartet online platform are still welcome to sign up. Through Quartet, a behavioral health specialist can receive referrals, accept new patients, track the patient’s progress, and access clinical assessments and other resources. For more information
Quartet is an independent company contracted by Blue Cross Blue Shield of Michigan to provide behavioral health services for Blue Cross and BCN members. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Providers can upload some medical records through Availity Essentials, starting Sept. 16Action item Watch for a provider alert with links to sign up for a training session to learn how to upload requested medical records into Availity® Essentials. Starting Sept. 16, 2023, health care providers will be able to upload requested medical records through Availity® Essentials for Blue Cross Blue Shield of Michigan commercial members when requested through the Medical Record Request Form. Here’s why we’re encouraging providers to upload the records into the Availity Essentials portal:
Providers will only need to upload the medical records when Blue Cross requests them through the Medical Record Request Form to help us adjudicate claims or decide on an appeal. We’ll continue to accept paper and fax submissions. How to upload the records To submit the medical records on Availity Essentials:
Training There will be two training sessions to demonstrate how to load records into Availity Essentials. Watch for a provider alert that will contain the registration links for the following training sessions:
Stay tuned for more information Our expanded use of Availity Essentials will be implemented in phases. We’ll continue to communicate changes through future Record articles. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
What to do now that voluntary prior authorization has endedAs we reported in the February and April 2023 issues of The Record, Blue Cross Blue Shield of Michigan stopped accepting voluntary prior authorization requests on May 1, 2023. Before providing services to members, be sure to follow all these steps:
Some procedures require prior authorization, as stated in Step 2 above. For summary information about prior authorization requirements, see the following documents:
Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Subscribe now for Provider Alerts Weekly emailYou can now subscribe to receive Provider Alerts Weekly, a list of links to the previous week’s provider alerts from Blue Cross Blue Shield of Michigan and Blue Care Network. Provider alerts give you information you may need to know before the publication dates of our provider newsletters. They’re housed on the secure Provider Resources website, and can be accessed through the Payer Space on our provider portal. We decided to create Provider Alerts Weekly after learning that office staff thought a weekly email with links to our provider alerts would be helpful. Beginning this fall, the email will give you a week’s worth of headlines as links so you can view the details for the alerts that interest you. Go to the Subscribe to Provider Newsletters webpage to sign up for Provider Alerts Weekly emails and then look for the emails to start arriving this fall. Billing chart: Blue Cross highlights medical, benefit policy changesYou’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart. This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures. We'll publish information about new Blue Cross groups or changes to group benefits under the Group Benefit Changes heading. For more detailed descriptions of the Blue Cross' policies for these procedures, check under the Commercial Policy tab in Benefit Explainer on Availity®. To access this online information:
2 .Click on Payer Spaces on the Availity menu bar. 3. Click on the BCBSM and BCN logo. 4. Click on Benefit Explainer on the Applications tab. 5. Click on the Commercial Policy tab. 6. Click on Topic. 7. Under Topic Criteria, click on the circle for Unique Identifier and click the drop-down arrow next to Choose Identifier Type, then click on HCPCS Code. 8. Enter the procedure code. 9. Click on Finish. 10. Click on Search.
None of the information included in this billing chart is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Blue Cross and BCN behavioral health changes coming Jan. 1Starting Jan. 1, 2024, Blue Cross Blue Shield of Michigan and Blue Care Network will consolidate the prior authorization and case management functions for behavioral health services, including treatment for autism. This change will affect all members:
The consolidation will result in two new programs that will align and standardize prior authorization and case management functions for all lines of business. This will make it easier for you to manage administrative functions for your Blue Cross and BCN patients. As part of this change, Lucet (New Directions) will no longer manage these functions for Blue Cross commercial members. What are the names of the new programs? The new programs are:
What changes will providers and members see? Here are some changes to expect:
There will be no changes to:
What’s changing for prior authorization requests? For autism treatment services: Because prior authorizations for autism treatment services are typically approved for a longer period of time than for other services, we began handling them differently, starting in July, to ensure we can transition them into the new system.
Starting in November:
Starting in 2024:
Note: For BCN commercial members, providers will continue to submit authorization requests and information updates for autism treatment services through our provider portal (availity.com).** Faxes won’t be accepted. For services other than autism treatment:
Additional information Look for more information about these and other changes in upcoming newsletter articles. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
We’re continuing to grow our crisis services programOur crisis services program, offering members who may be experiencing a mental health crisis a wider array of appropriate options, continues to grow. Two additional facilities recently joined the program:
Also, as we announced in an August Record article, the program is expanding to include our Medicare Advantage members (Medicare Plus Blue℠ and BCN Advantage℠), effective Jan. 1, 2024. The crisis services facilities that are part of this program offer the following types of care options:
Our Help in times of crisis flyer includes details on the care options available at each of the eight facilities across Michigan that participate in the program, along with their contact information. We encourage you to print this flyer and share it with your patients. In a crisis, members or other individuals — including family members, friends, law enforcement personnel or emergency department staff — can call the number of a crisis location in their service area for guidance. Walk-ins are also accepted at some locations. “These options can be used in place of going to an emergency room as part of our ongoing efforts to hasten access to behavioral health-focused care,” said Dr. William Beecroft, medical director of behavioral health for Blue Cross Blue Shield of Michigan. “Our goal is to make sure our members get treated at the right place at the right time.” A key component of this program is our mobile crisis services. Once a facility is contacted, a mobile unit may be deployed to offer both assessment and prompt treatment. If you’re a health care provider interested in joining this program, send an email to Dr. William Beecroft at wbeecroft@bcbsm.com. Also, we’ll keep you informed as additional locations join this program.
Starting Jan. 1, 2024, all DME codes will be removed from CareCentrix HIT and AIS programFor dates of service on or after Jan. 1, 2024, the durable medical equipment codes listed in the table below will be removed from the CareCentrix network management program for home infusion therapy and ambulatory infusion suite providers.
This change applies to:
Note: Ambulatory infusion suite providers are a subset of ambulatory infusion centers. These codes are still part of the DME benefit. Providers who participate in the Blue Cross or BCN DME network can bill them following existing Blue Cross or BCN billing guidelines. Prior to Jan. 1, 2024, we’ll update the Home infusion therapy and ambulatory infusion suite provider network management: Frequently asked questions document to reflect this change. CareCentrix is an independent company that manages the in-state, independent home infusion services and ambulatory infusion center provider network for Blue Cross Blue Shield of Michigan and Blue Care Network members who have commercial plans.
Physician appointment access survey in progressBlue Cross Blue Shield of Michigan and Blue Care Network must meet the requirements of several regulatory and accreditation bodies, such as the National Committee for Quality Assurance, the Centers for Medicare & Medicaid Services and the state of Michigan. To help ensure we meet these requirements, we’re reaching out to some physician offices to request the completion of an Appointment Access Survey for each physician in the office. Your office may receive a phone call or a fax request to complete the survey. Your participation is important to demonstrate that you’re meeting regulatory requirements. Below are the physician specialties that will be included in the survey. If you have physicians with these specialties at your office, you can follow the instructions below to complete the survey before we contact you.
Note: Be sure to complete a separate survey for each physician in the office. How to access the survey
Review appointment access standards You can review appointment access standards in our provider manuals. Here’s how to find them:
For the Blue Cross Commercial Provider Manual:
For the BCN Provider Manual:
For the Medicare Plus Blue℠ PPO Provider Manual:
**Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services.
How to find Blue Cross and BCN policies related to COVID-19 public health emergencySince the COVID-19 public health emergency ended on May 11, 2023, there’s a reduced need for viewing Blue Cross Blue Shield of Michigan and Blue Care Network’s temporary policies for COVID-19. As a result, we’re removing most of them from our public website, bcbsm.com/providers. However, we know that health care providers may need to reference these policies when working on claims for dates of service on or before May 11, 2023. Therefore, providers can still access the temporary policies by following these steps:
COVID-19-related documents for pharmacies Some COVID-19-related documents for pharmacies are still available on our public website but have moved to a new location. They are:
Here’s the new location where you can find these documents on our public website:
Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Help patients avoid a gap in coverage due to Medicaid redeterminationDuring the COVID-19 public health emergency, the Families First Coronavirus Response Act mandated that Medicaid programs maintain continuous enrollment for individuals. Now that the public health emergency has ended, all Medicaid and Healthy Michigan Plan members must go through a Medicaid redetermination process. This process began in June 2023 and will run through May 2024. Monthly renewal notices are sent three months before a member’s renewal date. Blue Cross Blue Shield of Michigan, Blue Care Network and our Medicaid health plan, Blue Cross Complete, encourage you to help your patients with Medicaid and Healthy Michigan Plan coverage understand the Medicaid redetermination process. This process verifies whether members still qualify for coverage. Those who no longer meet the eligibility criteria can be disenrolled. Blue Cross wants to help your patients understand the process and learn about various options that may be available if they lose eligibility. To learn more:
Here’s an overview of our Family Building and Women’s Health Support SolutionIn 2023, Blue Cross Blue Shield of Michigan and Blue Care Network began working with Maven** to provide the Family Building and Women’s Health Support Solution to eligible commercial members. This solution includes programs that support members of all backgrounds and lifestyles through four important stages of life — building a family, pregnancy, parenting and menopause. We recently published a document titled Family Building and Women’s Health Support Solution: Overview for providers that provides more detailed information than the articles we previously ran in our provider newsletters and alerts. If there are changes to the programs, we’ll update this document to reflect the changes. You can access the document linked above in the Care management section of the For Providers: Forms and Document page of the bcbsm.com website. **Maven is an independent company supporting Blue Cross Blue Shield of Michigan and Blue Care Network by providing family building and women’s health support services.
Here are some resources for patients monitoring chronic conditions while taking over-the-counter medicationsThis is part of an ongoing series of articles focusing on the tools and resources available to help FEP members manage their health. Viruses, such as acute bronchitis, are generally treated with over-the-counter medications instead of antibiotics, according to the National Library of Medicine.** Patients who have acute bronchitis and diabetes, hypertension, cardiovascular disease or another chronic condition may run into problems when taking over-the-counter medications due to their effect on these conditions. In addition to regular monitoring of A1c levels and blood pressure, more frequent home monitoring may be needed. Use these resources to help patients keep track of their conditions during an illness:
The following are informational flyers and a brochure to share with Blue Cross and Blue Shield Federal Employee Program® members: As always, health care providers and members can call Customer Service at 1-800-482-3600 or go visit fepblue.org for information on benefits, incentives and support services. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Blue Cross and TurningPoint update medical policies for musculoskeletal and pain management proceduresBlue Cross Blue Shield of Michigan, Blue Care Network and TurningPoint Healthcare Solutions LLC are adding and updating TurningPoint medical policies for musculoskeletal and pain management procedures. These policies apply to dates of service on or after Oct. 1, 2023. The TurningPoint medical policies will be available in the TurningPoint provider portal on Oct. 1, 2023. To see a list of the new TurningPoint medical policies and details about updates to existing TurningPoint medical policies, see our July 27, 2023, provider alert.
For commercial LTACH requests, remember to submit information about 3 SNFs to avoid delaysWhen submitting prior authorization requests for admissions to long-term acute care hospitals, you must include information about three skilled nursing facilities you’ve already contacted that indicated they can’t provide the level of care the member requires. This applies to LTACH placement requests for both Blue Cross Blue Shield of Michigan and Blue Care Network commercial members. If the information that’s required about the three SNFs isn’t included when you submit the prior authorization request, we’ll consider your request incomplete. We’ll ask you to resubmit the request when the information is available. This delays the processing of the request. Here’s the information we need about the three SNFs:
Be aware that:
You can read more about these and other requirements in the document Blue Cross and BCN Local Rules for 2023 for post-acute care: Modifications of InterQual® criteria. You can access this document at ereferrals.bcbsm.com, on these webpages:
Cost of external peer reviews to increaseWhat you need to know Providers will need to pay the cost of appeal reviews if the peer review agency upholds Blue Cross’ decision regarding a claim. The cost of external peer reviews for facilities (including hospitals) and doctors’ offices will increase, effective Sept. 1, 2023. Health care providers typically request peer reviews when they dispute an audit finding. Here’s a look at the current and new fees: Facility standard clinical review Facility coding review Professional standard clinical review Professional standard coding review According to Blue Cross Blue Shield of Michigan and Blue Care Network participation agreements with health care providers, if the peer review agency upholds Blue Cross’ decision regarding a claim, the facility or practitioner’s office will pay the cost of the appeal review.
New on-demand training available: Check out our new learning path, behavioral health video and moreAction item Visit our provider training site to find new resources on topics that are important to your role. Provider Experience continues to offer training resources for health care providers and staff. Our on-demand courses are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network. As part of our ongoing efforts, we recently added the following new learning opportunities: New learning path on provider training website A new learning path informs you of key courses for the front office staff. It’s a new approach to help staff members determine the right courses to take. Primary care providers and specialists should encourage new front office staff to start their journey on the learning path to help ensure they work with Blue Cross and BCN as efficiently as possible. To locate the recommended courses for front-office staff, open the Course Catalog on the provider training website and click on Learning paths to find the course for front office staff. Products at a glance This course is for those who are new to Blue Cross and BCN, and is also geared to front office staff. It’s designed to help new staff members get an overall understanding of our products, as well as an understanding of the information on a patient’s member ID card. As a new front office staff or provider, you may need to know how to identify which Blue Cross or BCN product your patients have, or you may need assistance knowing where the resources are related to our products. This course is part of our new approach to helping you find and take courses that fit the needs of your specific role. This course, along with another new course, “Prior authorization basic tools,” are part of the Front Office Staff Learning Path found on our provider training site. Search “products” to quickly locate the course. Behavioral health enrollment tips video This video is designed for behavioral health providers new to Blue Cross and BCN, and gives behavioral health providers and staff key tips as they complete their enrollment. Behavioral health providers new to Blue Cross will now have an additional resource to guide them through their initial journey with us. The video provides an alternative to learning about the enrollment steps for new providers on bcbsm.com. Search “behavioral” to quickly locate the video. And don’t forget to check the dashboard on our provider training site, designed to enhance the training experience for health care providers and staff, for announcements as we add more courses, including those with CME offerings. To request access to the training site, follow these steps:
If you need assistance creating your login ID or navigating the site, please contact ProviderTraining@bcbsm.com.
Lunch and learn webinars for physicians and coders focus on risk adjustment, codingAs a reminder, we’re offering live, 30-minute educational webinars that provide updated information on documentation and coding for common challenging diagnoses. Webinars also include an opportunity to ask questions. Here’s our upcoming schedule and tentative topics for the webinars. Each session starts at noon Eastern time. Log in to the provider training website to register for sessions that work with your schedule.
If you haven’t already registered for the provider training website, follow these steps:
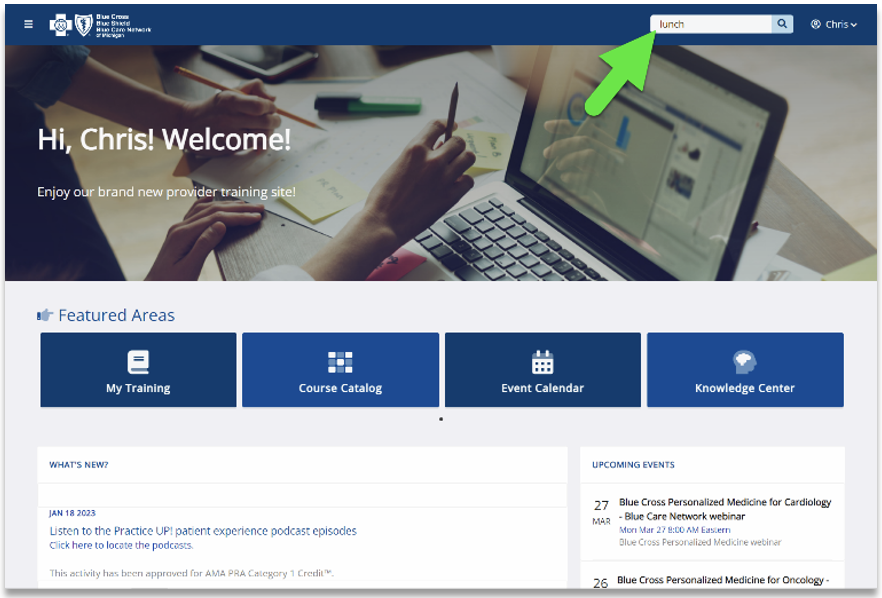
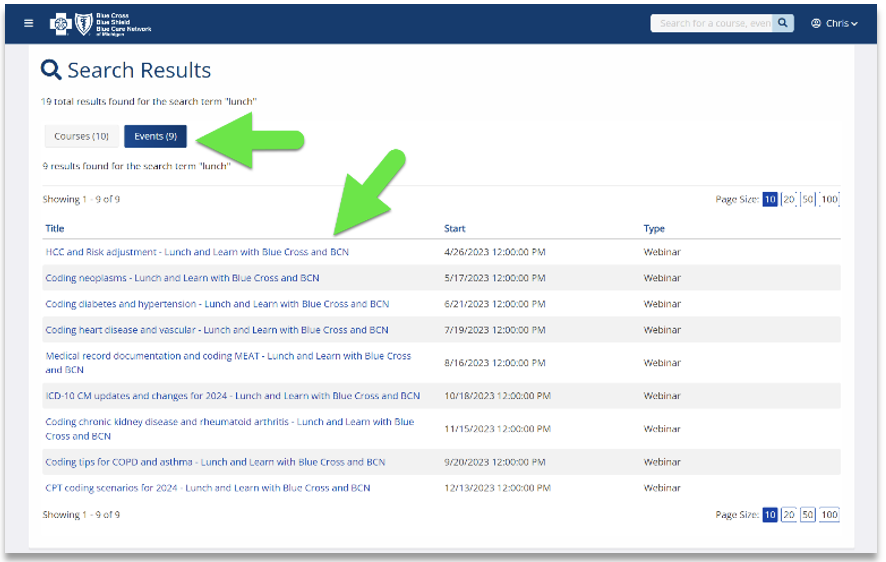
Locating a session Click here if you’re already registered for the provider training website. On the provider training website, look in the Event Calendar or use the search feature using the keyword “lunch” to quickly locate all 2023 sessions. See the screenshots below for more details.
Previous sessions You can also listen to previously recorded sessions. Check out the following:
If you have any questions about the sessions, contact April Boyce at aboyce@bcbsm.com. If you have questions regarding a session or website registration, email ProviderTraining@bcbsm.com.
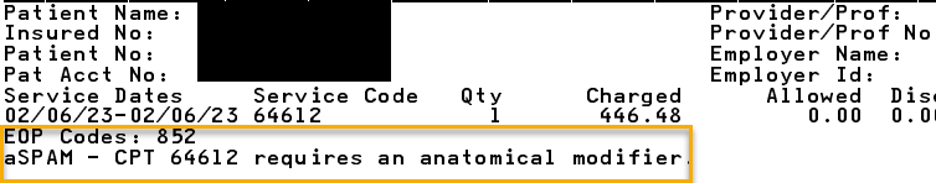
Reminder: Appeals shouldn’t be submitted for certain clinical edits on Medicare Plus Blue claimsMany clinical edits that apply to Medicare Plus Blue℠ claims shouldn’t be appealed. Health care providers should simply submit corrected claims for reconsideration. Here are some common examples of these types of clinical edits. 852_aSPAM Surgical CPT codes in the *10000 through *69999 range that have a Medicare Physician Fee Schedule bilateral indicator of “1” denote the surgical code is eligible to be billed on both sides of the body. We edit the surgical code when anatomical modifiers (50, LT, RT, E1, E2, E3, E4, F1, F2, F3, F4, F5, F6, F7, F8, F9, FA, T1, T2, T3, T4, T5, T6, T7, T8, T9, TA, LC, LD, RC, LM, RI) are appropriate, but not appended to the claim line. Providers should submit a corrected claim appending the appropriate modifier for reconsideration of services. Below is an example of a provider voucher indicating an anatomical modifier is required. CO*16-Claim/Service lacks information, has submission or billing errors, or has missing procedure modifiers.
852_aCLTRf Below is the required information for facility clinical trial claims. Inpatient claims:
Outpatient claims:
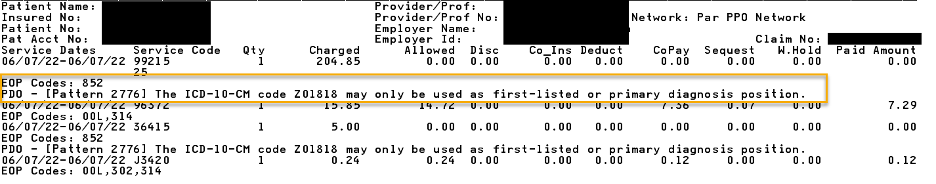
If one or more of the clinical trial billing requirements is missing, a corrected replacement claim should be submitted for reconsideration of charges. 852_PDO Certain diagnosis codes can only be billed in the first-listed or primary diagnosis code field on claims, according to the International Classification of Diseases, or ICD. There’s an identifier in some ICD-10-CM manuals for these codes. We edit the claim line if a primary-only diagnosis code is billed in a position other than the first-listed or primary position. Submitting a corrected claim changing the position of the primary-only diagnosis code will result in reconsideration of services. Below is an example of a provider voucher indicating that diagnosis Z01.818 may only be used as the first-listed or primary diagnosis. CO*16-Claim/Service lacks information, has submission or billing errors, or has a missing, incomplete or invalid principal diagnosis.
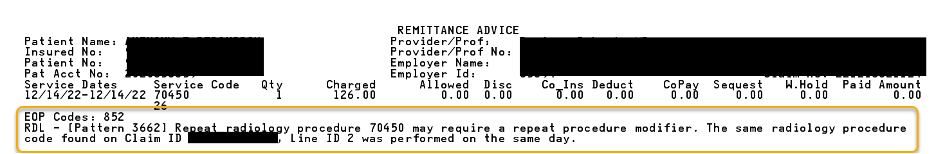
852_RDL In this example, the same radiology procedure code that’s on the current claim was found on another claim for the same date of service in the member’s claims history. Since this is a repeat radiology procedure, a repeat procedure modifier is required. Submitting a corrected claim appending the appropriate repeat procedure modifier (for example, modifiers 76 or 77) will result in a reconsideration of the charge without the need for an appeal submission. Below is an example of a provider voucher for this denial. CO*16-Claim/Service lacks information, has submission or billing errors, or has missing procedure modifiers
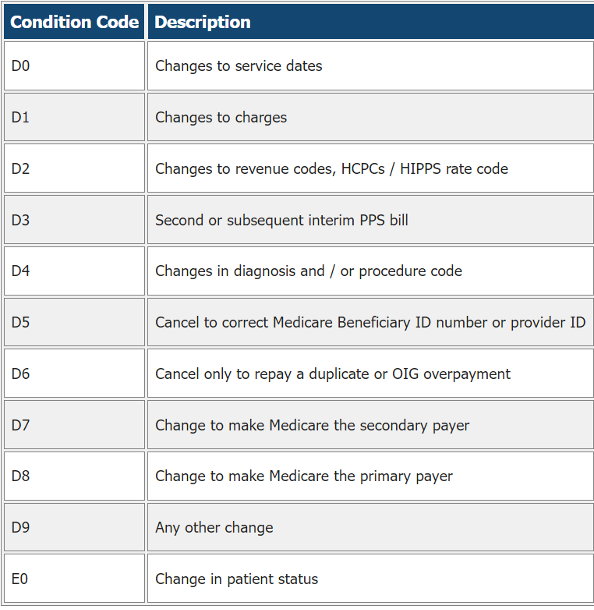
852_CCRCf When submitting adjusted or canceled facility claims (type of bill XX7 or XX8), an appropriate claim change reason or condition code is required.
Resubmit the facility claim with the appropriate condition code for reconsideration of the charges. Below is an example of a provider voucher for this denial. CO*16-Claim/Service lacks information, has submission or billing errors, or has a missing, incomplete or invalid condition code.
852_aMTOB131f Subsequent TOB 0131 claims submitted after an initial outpatient TOB 0131 claim for the same member and the same date of service are denied for a corrected billing that includes all outpatient charges for that date of service. Bill type 0131 indicates a complete claim. There should only be one claim with bill type 0131 per patient per facility per day. The fourth character of the bill type is the frequency indicator. If a claim is submitted with bill type 0131 and additional charges or changes need to be submitted, a corrected claim should be submitted with either a 0137 or 0138 bill type. Another claim with the 0131 bill type should not be submitted. If a 0137 bill type is submitted, this indicates that the previous claim was incomplete, and the current claim has all the information that should have been included from the first claim. Below are several other examples where a corrected claim should be submitted for reconsideration of services:
These are a few common examples. There are other clinical edits that don’t require an appeal submission for reconsideration. If an appeal is filed and the claim remains coded incorrectly, the appeal will be upheld. Submitting a corrected claim is the most accurate and efficient way to correct these denials. None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
We’re adding more codes to multiple procedure reduction payment policyStarting in December, Blue Cross Blue Shield of Michigan will add additional procedure codes to a payment policy that applies a 50% reduction when multiple procedures are performed during the same session. The multiple procedure reduction policy is based on guidelines from the Centers for Medicare & Medicaid Services and supports correct coding and payment accuracy. Below is a list of the procedure codes that we recently added to the reduction policy. It will apply to these codes starting in December 2023.
We’re making changes to payment policy for debridement procedures billed with arthroscopic proceduresBeginning in December, Blue Cross Blue Shield of Michigan’s payment policy will no longer allow separate and distinct modifiers to bypass bundling claim edits when shoulder debridement procedures are billed with arthroscopic shoulder procedures. If you submit a claim for a debridement procedure and an arthroscopic procedure on the same shoulder, you may receive a denial on the debridement procedure. Even if you append a separate and distinct modifier, bundling edits will still apply. We’re making this change to help ensure correct coding and payment accuracy. The following procedure codes apply to this policy:
Exception: Separate reporting of extensive debridement will apply to three arthroscopic CPT codes: *29824, *29827 and *29828.
Use new mailing address for provider appeals of some utilization management decisionsThe mailing address for submitting provider appeals of some utilization management decisions has changed as indicated below:
We’ve updated our denial letters to include the new address. Follow the instructions in the denial letters to ensure your appeal arrives at the appropriate location within the time frame allowed.
Reminder: Confirm data every 90 days and attest in CAQH every 120 daysWhat you need to know To remain listed in Blue Cross Blue Shield of Michigan’s provider directories, including Find a Doctor, health care providers must re-attest every 120 days. Have you confirmed your data within the past 90 days and attested in CAQH within the past 120 days? Ninety-day confirmation is needed for data elements such as name, specialty, address, phone number and digital contact information, while 120-day attestation is for all other data elements, including credentialing, licensing and demographics. If health care providers don’t re-attest with CAQH every 120 days, they won’t be included in Blue Cross Blue Shield of Michigan’s provider directories, including our Find a Doctor search tool. Failing to re-attest will result in your credentialing status ending, requiring you to reapply. Here are three key reasons to attest with CAQH:
Regardless of whether providers are practicing at an office location or practicing exclusively in an inpatient hospital setting, they need to perform this attestation. If you’re practicing exclusively in an inpatient hospital setting, you must indicate it on your CAQH application. This information is used to determine whether full credentialing is required. CAQH is a nonprofit alliance of health plans and trade associations focused on simplifying health care administration. Blue Cross uses CAQH to gather and coordinate our practitioner credentialing information. All health care practitioners, including hospital-based providers, need to be registered with CAQH. If you have questions about CAQH, call the help desk at 1-888-599-1771, or go to CAQH.org.** **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
We updated questionnaires in e-referral systemOn July 30, 2023, we updated questionnaires in the e-referral system, and also updated the corresponding preview questionnaires on the ereferrals.bcbsm.com website. As a reminder, we use our authorization criteria, our medical policies and your answers to these questionnaires when making utilization management determinations on your prior authorization requests. Updated questionnaires We updated the following:
Preview questionnaires Preview questionnaires show the questions you’ll need to answer in the e-referral system so you can prepare ahead of time. To find the preview questionnaires, go to ereferrals.bcbsm.com and:
Authorization criteria and medical policies The Authorization Requirements & Criteria pages explain how to access the pertinent authorization criteria and medical policies.
Blue Cross and BCN behavioral health changes coming Jan. 1Starting Jan. 1, 2024, Blue Cross Blue Shield of Michigan and Blue Care Network will consolidate the prior authorization and case management functions for behavioral health services, including treatment for autism. This change will affect all members:
The consolidation will result in two new programs that will align and standardize prior authorization and case management functions for all lines of business. This will make it easier for you to manage administrative functions for your Blue Cross and BCN patients. As part of this change, Lucet (New Directions) will no longer manage these functions for Blue Cross commercial members. What are the names of the new programs? The new programs are:
What changes will providers and members see? Here are some changes to expect:
There will be no changes to:
What’s changing for prior authorization requests? For autism treatment services: Because prior authorizations for autism treatment services are typically approved for a longer period of time than for other services, we began handling them differently, starting in July, to ensure we can transition them into the new system.
Starting in November:
Starting in 2024:
Note: For BCN commercial members, providers will continue to submit authorization requests and information updates for autism treatment services through our provider portal (availity.com).** Faxes won’t be accepted. For services other than autism treatment:
Additional information Look for more information about these and other changes in upcoming newsletter articles. Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
We’re continuing to grow our crisis services programOur crisis services program, offering members who may be experiencing a mental health crisis a wider array of appropriate options, continues to grow. Two additional facilities recently joined the program:
Also, as we announced in an August Record article, the program is expanding to include our Medicare Advantage members (Medicare Plus Blue℠ and BCN Advantage℠), effective Jan. 1, 2024. The crisis services facilities that are part of this program offer the following types of care options:
Our Help in times of crisis flyer includes details on the care options available at each of the eight facilities across Michigan that participate in the program, along with their contact information. We encourage you to print this flyer and share it with your patients. In a crisis, members or other individuals — including family members, friends, law enforcement personnel or emergency department staff — can call the number of a crisis location in their service area for guidance. Walk-ins are also accepted at some locations. “These options can be used in place of going to an emergency room as part of our ongoing efforts to hasten access to behavioral health-focused care,” said Dr. William Beecroft, medical director of behavioral health for Blue Cross Blue Shield of Michigan. “Our goal is to make sure our members get treated at the right place at the right time.” A key component of this program is our mobile crisis services. Once a facility is contacted, a mobile unit may be deployed to offer both assessment and prompt treatment. If you’re a health care provider interested in joining this program, send an email to Dr. William Beecroft at wbeecroft@bcbsm.com. Also, we’ll keep you informed as additional locations join this program.
Starting Jan. 1, 2024, all DME codes will be removed from CareCentrix HIT and AIS programFor dates of service on or after Jan. 1, 2024, the durable medical equipment codes listed in the table below will be removed from the CareCentrix network management program for home infusion therapy and ambulatory infusion suite providers.
This change applies to:
Note: Ambulatory infusion suite providers are a subset of ambulatory infusion centers. These codes are still part of the DME benefit. Providers who participate in the Blue Cross or BCN DME network can bill them following existing Blue Cross or BCN billing guidelines. Prior to Jan. 1, 2024, we’ll update the Home infusion therapy and ambulatory infusion suite provider network management: Frequently asked questions document to reflect this change. CareCentrix is an independent company that manages the in-state, independent home infusion services and ambulatory infusion center provider network for Blue Cross Blue Shield of Michigan and Blue Care Network members who have commercial plans.
How to find Blue Cross and BCN policies related to COVID-19 public health emergencySince the COVID-19 public health emergency ended on May 11, 2023, there’s a reduced need for viewing Blue Cross Blue Shield of Michigan and Blue Care Network’s temporary policies for COVID-19. As a result, we’re removing most of them from our public website, bcbsm.com/providers. However, we know that health care providers may need to reference these policies when working on claims for dates of service on or before May 11, 2023. Therefore, providers can still access the temporary policies by following these steps:
COVID-19-related documents for pharmacies Some COVID-19-related documents for pharmacies are still available on our public website but have moved to a new location. They are:
Here’s the new location where you can find these documents on our public website:
Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Blue Cross and TurningPoint update medical policies for musculoskeletal and pain management proceduresBlue Cross Blue Shield of Michigan, Blue Care Network and TurningPoint Healthcare Solutions LLC are adding and updating TurningPoint medical policies for musculoskeletal and pain management procedures. These policies apply to dates of service on or after Oct. 1, 2023. The TurningPoint medical policies will be available in the TurningPoint provider portal on Oct. 1, 2023. To see a list of the new TurningPoint medical policies and details about updates to existing TurningPoint medical policies, see our July 27, 2023, provider alert.
For commercial LTACH requests, remember to submit information about 3 SNFs to avoid delaysWhen submitting prior authorization requests for admissions to long-term acute care hospitals, you must include information about three skilled nursing facilities you’ve already contacted that indicated they can’t provide the level of care the member requires. This applies to LTACH placement requests for both Blue Cross Blue Shield of Michigan and Blue Care Network commercial members. If the information that’s required about the three SNFs isn’t included when you submit the prior authorization request, we’ll consider your request incomplete. We’ll ask you to resubmit the request when the information is available. This delays the processing of the request. Here’s the information we need about the three SNFs:
Be aware that:
You can read more about these and other requirements in the document Blue Cross and BCN Local Rules for 2023 for post-acute care: Modifications of InterQual® criteria. You can access this document at ereferrals.bcbsm.com, on these webpages:
Cost of external peer reviews to increaseWhat you need to know Providers will need to pay the cost of appeal reviews if the peer review agency upholds Blue Cross’ decision regarding a claim. The cost of external peer reviews for facilities (including hospitals) and doctors’ offices will increase, effective Sept. 1, 2023. Health care providers typically request peer reviews when they dispute an audit finding. Here’s a look at the current and new fees: Facility standard clinical review Facility coding review Professional standard clinical review Professional standard coding review According to Blue Cross Blue Shield of Michigan and Blue Care Network participation agreements with health care providers, if the peer review agency upholds Blue Cross’ decision regarding a claim, the facility or practitioner’s office will pay the cost of the appeal review.
Lunch and learn webinars for physicians and coders focus on risk adjustment, codingAs a reminder, we’re offering live, 30-minute educational webinars that provide updated information on documentation and coding for common challenging diagnoses. Webinars also include an opportunity to ask questions. Here’s our upcoming schedule and tentative topics for the webinars. Each session starts at noon Eastern time. Log in to the provider training website to register for sessions that work with your schedule.
If you haven’t already registered for the provider training website, follow these steps:
Locating a session Click here if you’re already registered for the provider training website. On the provider training website, look in the Event Calendar or use the search feature using the keyword “lunch” to quickly locate all 2023 sessions. See the screenshots below for more details.
Previous sessions You can also listen to previously recorded sessions. Check out the following:
If you have any questions about the sessions, contact April Boyce at aboyce@bcbsm.com. If you have questions regarding a session or website registration, email ProviderTraining@bcbsm.com.
Reminder: Appeals shouldn’t be submitted for certain clinical edits on Medicare Plus Blue claimsMany clinical edits that apply to Medicare Plus Blue℠ claims shouldn’t be appealed. Health care providers should simply submit corrected claims for reconsideration. Here are some common examples of these types of clinical edits. 852_aSPAM Surgical CPT codes in the *10000 through *69999 range that have a Medicare Physician Fee Schedule bilateral indicator of “1” denote the surgical code is eligible to be billed on both sides of the body. We edit the surgical code when anatomical modifiers (50, LT, RT, E1, E2, E3, E4, F1, F2, F3, F4, F5, F6, F7, F8, F9, FA, T1, T2, T3, T4, T5, T6, T7, T8, T9, TA, LC, LD, RC, LM, RI) are appropriate, but not appended to the claim line. Providers should submit a corrected claim appending the appropriate modifier for reconsideration of services. Below is an example of a provider voucher indicating an anatomical modifier is required. CO*16-Claim/Service lacks information, has submission or billing errors, or has missing procedure modifiers.
852_aCLTRf Below is the required information for facility clinical trial claims. Inpatient claims:
Outpatient claims:
If one or more of the clinical trial billing requirements is missing, a corrected replacement claim should be submitted for reconsideration of charges. 852_PDO Certain diagnosis codes can only be billed in the first-listed or primary diagnosis code field on claims, according to the International Classification of Diseases, or ICD. There’s an identifier in some ICD-10-CM manuals for these codes. We edit the claim line if a primary-only diagnosis code is billed in a position other than the first-listed or primary position. Submitting a corrected claim changing the position of the primary-only diagnosis code will result in reconsideration of services. Below is an example of a provider voucher indicating that diagnosis Z01.818 may only be used as the first-listed or primary diagnosis. CO*16-Claim/Service lacks information, has submission or billing errors, or has a missing, incomplete or invalid principal diagnosis.
852_RDL In this example, the same radiology procedure code that’s on the current claim was found on another claim for the same date of service in the member’s claims history. Since this is a repeat radiology procedure, a repeat procedure modifier is required. Submitting a corrected claim appending the appropriate repeat procedure modifier (for example, modifiers 76 or 77) will result in a reconsideration of the charge without the need for an appeal submission. Below is an example of a provider voucher for this denial. CO*16-Claim/Service lacks information, has submission or billing errors, or has missing procedure modifiers
852_CCRCf When submitting adjusted or canceled facility claims (type of bill XX7 or XX8), an appropriate claim change reason or condition code is required.
Resubmit the facility claim with the appropriate condition code for reconsideration of the charges. Below is an example of a provider voucher for this denial. CO*16-Claim/Service lacks information, has submission or billing errors, or has a missing, incomplete or invalid condition code.
852_aMTOB131f Subsequent TOB 0131 claims submitted after an initial outpatient TOB 0131 claim for the same member and the same date of service are denied for a corrected billing that includes all outpatient charges for that date of service. Bill type 0131 indicates a complete claim. There should only be one claim with bill type 0131 per patient per facility per day. The fourth character of the bill type is the frequency indicator. If a claim is submitted with bill type 0131 and additional charges or changes need to be submitted, a corrected claim should be submitted with either a 0137 or 0138 bill type. Another claim with the 0131 bill type should not be submitted. If a 0137 bill type is submitted, this indicates that the previous claim was incomplete, and the current claim has all the information that should have been included from the first claim. Below are several other examples where a corrected claim should be submitted for reconsideration of services:
These are a few common examples. There are other clinical edits that don’t require an appeal submission for reconsideration. If an appeal is filed and the claim remains coded incorrectly, the appeal will be upheld. Submitting a corrected claim is the most accurate and efficient way to correct these denials. None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
We’re adding more codes to multiple procedure reduction payment policyStarting in December, Blue Cross Blue Shield of Michigan will add additional procedure codes to a payment policy that applies a 50% reduction when multiple procedures are performed during the same session. The multiple procedure reduction policy is based on guidelines from the Centers for Medicare & Medicaid Services and supports correct coding and payment accuracy. Below is a list of the procedure codes that we recently added to the reduction policy. It will apply to these codes starting in December 2023.
We’re making changes to payment policy for debridement procedures billed with arthroscopic proceduresBeginning in December, Blue Cross Blue Shield of Michigan’s payment policy will no longer allow separate and distinct modifiers to bypass bundling claim edits when shoulder debridement procedures are billed with arthroscopic shoulder procedures. If you submit a claim for a debridement procedure and an arthroscopic procedure on the same shoulder, you may receive a denial on the debridement procedure. Even if you append a separate and distinct modifier, bundling edits will still apply. We’re making this change to help ensure correct coding and payment accuracy. The following procedure codes apply to this policy:
Exception: Separate reporting of extensive debridement will apply to three arthroscopic CPT codes: *29824, *29827 and *29828.
Use new mailing address for provider appeals of some utilization management decisionsThe mailing address for submitting provider appeals of some utilization management decisions has changed as indicated below:
We’ve updated our denial letters to include the new address. Follow the instructions in the denial letters to ensure your appeal arrives at the appropriate location within the time frame allowed.
Starting Jan. 1, 2024, all DME codes will be removed from CareCentrix HIT and AIS programFor dates of service on or after Jan. 1, 2024, the durable medical equipment codes listed in the table below will be removed from the CareCentrix network management program for home infusion therapy and ambulatory infusion suite providers.
This change applies to:
Note: Ambulatory infusion suite providers are a subset of ambulatory infusion centers. These codes are still part of the DME benefit. Providers who participate in the Blue Cross or BCN DME network can bill them following existing Blue Cross or BCN billing guidelines. Prior to Jan. 1, 2024, we’ll update the Home infusion therapy and ambulatory infusion suite provider network management: Frequently asked questions document to reflect this change. CareCentrix is an independent company that manages the in-state, independent home infusion services and ambulatory infusion center provider network for Blue Cross Blue Shield of Michigan and Blue Care Network members who have commercial plans. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||