Forward to a friend |
Subscribe | The Record Archive | Contacts | bcbsm.com | Print this article
|
September 2023
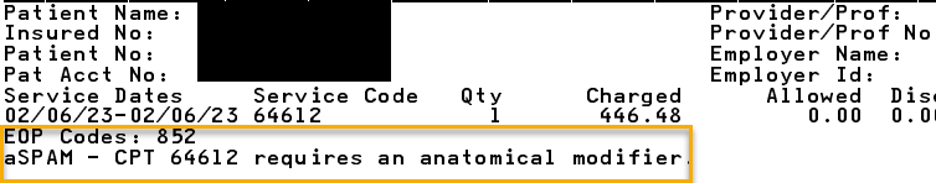
Reminder: Appeals shouldn’t be submitted for certain clinical edits on Medicare Plus Blue claimsMany clinical edits that apply to Medicare Plus Blue℠ claims shouldn’t be appealed. Health care providers should simply submit corrected claims for reconsideration. Here are some common examples of these types of clinical edits. 852_aSPAM Surgical CPT codes in the *10000 through *69999 range that have a Medicare Physician Fee Schedule bilateral indicator of “1” denote the surgical code is eligible to be billed on both sides of the body. We edit the surgical code when anatomical modifiers (50, LT, RT, E1, E2, E3, E4, F1, F2, F3, F4, F5, F6, F7, F8, F9, FA, T1, T2, T3, T4, T5, T6, T7, T8, T9, TA, LC, LD, RC, LM, RI) are appropriate, but not appended to the claim line. Providers should submit a corrected claim appending the appropriate modifier for reconsideration of services. Below is an example of a provider voucher indicating an anatomical modifier is required. CO*16-Claim/Service lacks information, has submission or billing errors, or has missing procedure modifiers.
852_aCLTRf Below is the required information for facility clinical trial claims. Inpatient claims:
Outpatient claims:
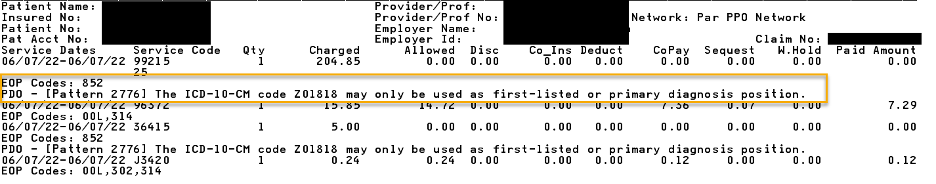
If one or more of the clinical trial billing requirements is missing, a corrected replacement claim should be submitted for reconsideration of charges. 852_PDO Certain diagnosis codes can only be billed in the first-listed or primary diagnosis code field on claims, according to the International Classification of Diseases, or ICD. There’s an identifier in some ICD-10-CM manuals for these codes. We edit the claim line if a primary-only diagnosis code is billed in a position other than the first-listed or primary position. Submitting a corrected claim changing the position of the primary-only diagnosis code will result in reconsideration of services. Below is an example of a provider voucher indicating that diagnosis Z01.818 may only be used as the first-listed or primary diagnosis. CO*16-Claim/Service lacks information, has submission or billing errors, or has a missing, incomplete or invalid principal diagnosis.
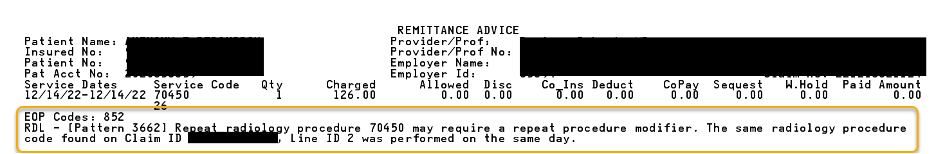
852_RDL In this example, the same radiology procedure code that’s on the current claim was found on another claim for the same date of service in the member’s claims history. Since this is a repeat radiology procedure, a repeat procedure modifier is required. Submitting a corrected claim appending the appropriate repeat procedure modifier (for example, modifiers 76 or 77) will result in a reconsideration of the charge without the need for an appeal submission. Below is an example of a provider voucher for this denial. CO*16-Claim/Service lacks information, has submission or billing errors, or has missing procedure modifiers
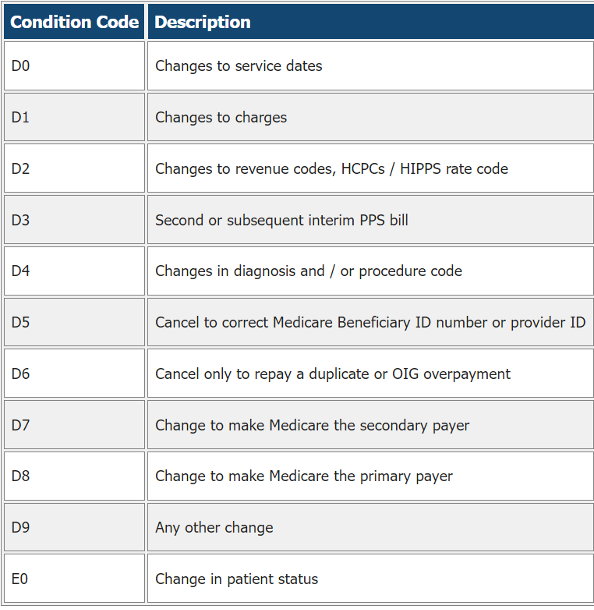
852_CCRCf When submitting adjusted or canceled facility claims (type of bill XX7 or XX8), an appropriate claim change reason or condition code is required.
Resubmit the facility claim with the appropriate condition code for reconsideration of the charges. Below is an example of a provider voucher for this denial. CO*16-Claim/Service lacks information, has submission or billing errors, or has a missing, incomplete or invalid condition code.
852_aMTOB131f Subsequent TOB 0131 claims submitted after an initial outpatient TOB 0131 claim for the same member and the same date of service are denied for a corrected billing that includes all outpatient charges for that date of service. Bill type 0131 indicates a complete claim. There should only be one claim with bill type 0131 per patient per facility per day. The fourth character of the bill type is the frequency indicator. If a claim is submitted with bill type 0131 and additional charges or changes need to be submitted, a corrected claim should be submitted with either a 0137 or 0138 bill type. Another claim with the 0131 bill type should not be submitted. If a 0137 bill type is submitted, this indicates that the previous claim was incomplete, and the current claim has all the information that should have been included from the first claim. Below are several other examples where a corrected claim should be submitted for reconsideration of services:
These are a few common examples. There are other clinical edits that don’t require an appeal submission for reconsideration. If an appeal is filed and the claim remains coded incorrectly, the appeal will be upheld. Submitting a corrected claim is the most accurate and efficient way to correct these denials. None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations. |
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|