Subscribe | The Record Archive | Contacts | bcbsm.com
|
May 2023
Do you know about our BlueCard processes?At Blue Cross Blue Shield of Michigan, we want to ensure that health care providers have the information they need about BlueCard®. This national program enables members of one Blue Cross Blue Shield plan to obtain health care services while traveling or living in another Blue Cross Blue Shield plan's service area. About BlueCard The program links participating health care providers with independent Blue Cross Blue Shield plans across the United States and in more than 200 countries and territories worldwide through a single electronic network for claims processing and reimbursement. The BlueCard program lets you conveniently submit claims for members from other Blue Cross Blue Shield plans, including international Blue Cross Blue Shield plans, directly to Blue Cross Blue Shield of Michigan. Blue Cross is your single point of contact for all your claims-related questions. Verifying coverage and eligibility When a member from an out-of-state Blue Cross Blue Shield plan (the home plan) requests care and presents a current Blue Cross Blue Shield identification card, prior to providing services, you (as the service provider for the host plan), should:
Members with coverage from a Blue Cross Blue Shield plan may also present a debit card, which may be Blue-branded, to cover cost-sharing payments. BlueCard Eligibility Call Center Call the BlueCard Eligibility Call Center at 1-800-676-2583. State the three-character alpha-numeric prefix on the patient's ID card, and you’ll be connected with the patient's home plan to verify eligibility and benefits for health care coverage. Prior authorization You can call the BlueCard Eligibility Call Center and choose the appropriate prior authorization prompt, or you can use the Authorizations & Referrals page on Availity®, our provider portal. Timely filing All original facility claims must be reported to Blue Cross within 12 months from the date of service and all original professional claims must be reported to Blue Cross within 180 days of the date of service. All claim adjustment requests for both professional and facility claims must be billed to Blue Cross within 24 months of the date of service. For more details, including information on how to submit claims for various services, see the “BlueCard Program” chapter of the Blue Cross Commercial Provider Manual. Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services.
Here’s more information about changes that will result from end of COVID-19 public health emergencyOn Jan. 30, 2023, the White House announced that it will end the public health emergency on May 11, 2023. As we’ve reported previously, Blue Cross Blue Shield of Michigan and Blue Care Network enacted temporary measures to support providers and protect members during the COVID-19 pandemic. Now that the public health emergency is ending, you need to know which temporary measures are continuing and which are ending. Check out our Temporary changes due to the COVID-19 pandemic document. We’ve been regularly updating this as we determine which temporary changes become permanent and which will end. Several temporary measures to continue Here are a few examples of changes that are no longer temporary and will continue after the public health emergency ends:
Coverage for certain other temporary measures to end Here are a couple examples of temporary changes that are ending when the public health emergency ends:
For other temporary measures that have ended, see the Temporary changes due to the COVID-19 pandemic document. Resources Here are some additional resources for information related to the end of the public health emergency.
Through May 11, we’ll continue to update the Temporary changes due to the COVID-19 pandemic document as decisions are made. As a reminder, you can view our COVID-19 provider communications as follows:
You can also access these communications on the COVID-19 webpage for health care providers on our public website. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Blue Cross expanding covered services for substance use disorders and mental healthEffective July 1, 2023, we’ll cover the following as standard benefits for all Blue Cross Blue Shield of Michigan commercial members:
Currently, Blue Cross covers partial hospitalization program services only for mental health and intensive outpatient program services only for substance use disorders. Blue Care Network already covers these services, as do some groups with Blue Cross commercial coverage. Aligning these benefits across our Blue Cross and BCN lines of business will do the following for our Blue Cross commercial members:
This change won’t affect members’ out-of-pocket costs. Additional information Partial hospitalization program services will continue to require prior authorization through New Directions. For more information, see the For Blue Cross commercial members section of the Blue Cross Behavioral Health page on our ereferrals.bcbsm.com website.
Prior authorization processes for MESSA members to change June 1Michigan’s prior authorization law requirements** go into effect on June 1, 2023. These requirements apply to health plans and health care providers in Michigan for members who have commercial coverage. One of the requirements is that health plans must provide an online method through which providers can submit prior authorization requests for all services. The Michigan Education Special Services Association, known as MESSA, manages most prior authorization requests for its members, with exceptions for certain services. Online submission tools for submitting prior authorization requests for MESSA members are shown in the table below — including a new online method for submitting requests to MESSA. Note: Alternate submission methods will continue to be available for situations when providers are unable to submit requests online. Those occasions include power and internet outages, and similar events.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
EDI transitioning to Availity starting in 2023Blue Cross Blue Shield of Michigan and Blue Care Network will move our electronic data interchange services, known as EDI, to Availity® beginning in August 2023. The EDI transition affects HIPAA electronic transactions. The transition will occur in phases, starting with claims (837) and remittance (835) transactions, but all electronic transactions will transition to Availity. Examples of electronic transactions include the electronic 837 claims, 835 electronic remittance advice, 270/271 eligibility and benefit, 276/277 claim status and 278 prior authorizations. This transition includes electronic transactions for all Blue Cross and BCN fully insured and self-funded health plans. This includes:
If you submit HIPAA EDI transactions to Blue Cross for payers other than Blue Cross and BCN and our health plans listed above, you’ll need to find a new method to submit those transactions. Blue Cross Blue Shield of Michigan EDI will no longer accept non-Blue Cross and BCN health plan transactions once our EDI transitions to Availity. Many of our EDI submitters and trading partners already submit to Availity’s EDI clearinghouse for other health plans. In 2022, Blue Cross and BCN moved our provider portal to Availity’s secure platform where you can find information for members associated with multiple health plans. We expect the EDI transition to begin in August 2023. Availity will handle all transition activities and will start sending communications to our EDI submitters and trading partners 90 to 120 days prior to the transition.
If you have any questions about the EDI transition, send an email to partnermanagement@availity.com. Don’t contact Blue Cross EDI. Availity is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Reminder: Reporting instructions for Blue Cross or FEP supplemental when Medicare Advantage is primary payerWhen a member has a Medicare Advantage or Medicare Advantage HMO primary and a Blue Cross Blue Shield of Michigan or Blue Cross and Blue Shield Federal Employee Program® supplemental policy, remember to report the primary payer with a claim filing indicator of MA or MB in loop 2320. Institutional:
Professional:
Has the member responded to the Letter of Other Insurance inquiry? Members can update their coverage details with Blue Cross by the following methods:
Allow up to five business days for Blue Cross to process the requested changes. Billing chart: Blue Cross highlights medical, benefit policy changesYou’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart. This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures. We'll publish information about new Blue Cross groups or changes to group benefits under the Group Benefit Changes heading. For more detailed descriptions of the Blue Cross' policies for these procedures, check under the Commercial Policy tab in Benefit Explainer on Availity®. To access this online information:
2 .Click on Payer Spaces on the Availity menu bar. 3. Click on the BCBSM and BCN logo. 4. Click on Benefit Explainer on the Applications tab. 5. Click on the Commercial Policy tab. 6. Click on Topic. 7. Under Topic Criteria, click on the circle for Unique Identifier and click the drop-down arrow next to Choose Identifier Type, then click on HCPCS Code. 8. Enter the procedure code. 9. Click on Finish. 10. Click on Search.
None of the information included in this billing chart is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Behavioral health telehealth flexibilities for Medicare Advantage members to continue after PHE endsDuring the COVID-19 public health emergency, the Centers for Medicare & Medicaid Services temporarily waived certain requirements and allowed flexibilities for providing telehealth services for behavioral health care. The Consolidated Appropriations Act, 2023, extended these flexibilities through Dec. 31, 2024. Some of these flexibilities will become permanent. Blue Cross Blue Shield of Michigan and Blue Care Network will follow Medicare telehealth guidelines for our Medicare Plus Blue℠ and BCN Advantage℠ members. Flexibilities becoming permanent for Medicare members:
Temporary Medicare flexibilities that will end on Dec. 31, 2024:
For more information on these changes, visit the Telehealth policy changes after the COVID-19 public health emergency** webpage on telehealth.hhs.gov. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
MyMichigan Family Practice Center: Building a high-functioning teamThis is the second article in a series highlighting some top performers in the Patient-Centered Medical Home Designation Program.  Dr. Sasha Savage When Sasha Savage, M.D., attended a conference on the Patient-Centered Medical Home model, held in Savannah, Georgia, in 2008, he was intrigued and impressed. He networked with the presenters to gather additional information, then headed home to think about how he could begin implementing the PCMH model in his own practice. “This represented a completely different perspective on care delivery,” said Dr. Savage, who practices at MyMichigan Family Practice Center in Midland, part of University of Michigan Health. “I recognized we had a huge opportunity to improve performance by implementing the PCMH model.” PCMH uses a team-based approach to provide efficient, cost-effective care that’s centered around the patient. The goal is to help prevent disease, reduce hospitalizations and emergency department visits, track patient care and better manage common and chronic medical conditions to ensure patients are getting the right care at the right time in the right setting. Becoming a PCMH practice Dr. Savage’s first task after attending the conference was to reach out to his employed physician group, MyMichigan Medical Group, to get performance data. He and his colleagues analyzed the data to determine opportunities for improvement and establish initiatives. He then built a business model and worked with the health system executives and providers in the practice to get their buy-in to move forward. Educating providers and staff about PCMH was a key element of implementation, along with support from Blue Cross Blue Shield of Michigan. Next, he set about building an effective care team. “At our practice, all team members have the innate ability to perform and participate in all practice initiatives,” said Dr. Savage. “All team members are considered equal and important to success in improving patient outcomes. All staff are engaged in discussions around improvement. The supervisory team’s role is to remove barriers that hold people back.” Today, in addition to physicians and other key staff members, the practice includes a behavioral health care manager, chronic care manager, pharmacist and a community health worker. Building and maintaining a successful team The practice also serves as a training facility for 24 resident physicians per year. Eight faculty attending physicians oversee and advise the residents. “Each faculty provider advises two to four residents,” explained Bonnie Khabir, the practice manager. “Faculty don’t use hospitalists. They make rounds on patients in the hospital to facilitate transitions of care.” Khabir added that residents come to the clinic every day and are critiqued on patient engagement and clinical matters. They also participate in quality improvement projects as part of their training. The practice sends out a Quality Corner email each month and maintains a Quality Book that contains the data and reports the staff uses to close gaps in care. Staff is encouraged to regularly review the book and to reach out to patients to ensure they receive timely services.  Dr. Savage stands “A focus of residency training in this practice is how to develop a highly efficient and effective team,” said Khabir. “The practice has a scheduling coordinator who assists with transitioning patients as the resident rotates out of the practice to ensure smooth transition to a new provider.” According to Meranda Collins, R.N. supervisor, ongoing education is another factor contributing to the success of the practice. “All staff are coached one-on-one as needed, with a focus on educational opportunities for everyone.” This approach has led to the development of a high-functioning team. “We work to support our staff to prevent burnout and dissatisfaction,” Dr. Savage said. He added that the staff recently received training in improving the provider-patient relationships and how to cope with challenging behavior. Following are some other processes that have been initiated to encourage team building:
Asked if he had any advice for other practices that want to build a high-functioning team that creates a good patient experience, Dr. Savage replied, “Build a culture of excellence, engage staff and ensure that all team members feel valued and important. If you want to go fast, go alone, but if you want to succeed, build a team.”
Pilot kidney health management program offered to URMBT Blue Cross non-Medicare members starting in MayChronic kidney disease affects more than 1 in 7 U.S. adults, and the majority of people aren’t aware they have it, according to the National Institute of Diabetes and Digestive and Kidney Diseases. To address this challenge, Blue Cross Blue Shield of Michigan is working with Healthmap Solutions, an independent specialty population management company that offers a kidney health management solution. This small-scale pilot program targets UAW Retiree Medical Benefits Trust non-Medicare members diagnosed with chronic kidney disease, or CKD, stages 3 through 5, unspecified CKD and end-stage renal disease. Outreach to physicians is underway. Select members will be encouraged to register, starting in May. There is no cost for them to participate. Using member and provider-facing teams, this program will complement office-based primary and specialty care services with care navigation to educate members while incorporating kidney-related comorbidity management and addressing unmet social needs. Among the goals are to slow disease progression, prevent unnecessary admissions and readmissions, and ensure appropriate transitions of care. Healthmap will work with members and health care providers to assist in coordinating the start of dialysis or developing a personal renal replacement therapy plan to avoid unplanned dialysis. If you have any questions or need additional information, send an email to jmurray2@bcbsm.com.
Don’t forget to register for 2023 virtual provider symposium sessionsAction item Register for one of the upcoming virtual provider symposium sessions below. As you may have read previously in The Record, this year’s virtual provider symposiums run throughout May and June. Physicians, physician assistants, nurse practitioners, nurses and coders can receive continuing education credits for attending. You’re welcome to register for any session listed below. Click here to log in to the provider training website to register for sessions. If you don’t already have access, you can easily create an account. Click here to register. We recommend that you use the same email address you use to communicate with Blue Cross Blue Shield of Michigan when creating the account. Once you’re logged in to the provider training site, open the event calendar to sign up for any of the following sessions. Reach for the Stars-HEDIS®/Star Measure Overview: For physicians and office staff responsible for closing gaps in care related to quality adult measures
Patient Experience: For physicians and office staff responsible for creating positive patient experiences. Learn how to ensure your practice has the knowledge and tools needed to set and meet patients’ expectations.
Coding Complex Cases: For physicians, coders, billers and administrative staff
Questions? Contact Ellen Kraft at ekraft@bcbsm.com if you have questions about the sessions. Contact the provider training team at ProviderTraining@bcbsm.com if you have questions about registration or using the provider training website. HEDIS® is a registered trademark of the National Committee for Quality Assurance. Accreditation Statement: This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of the Minnesota Medical Association and Blue Cross Blue Shields of Michigan. The Minnesota Medical Association (MMA) is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
New on-demand training availableAction item Visit our provider training site to find new resources on topics that are important to your role. Provider Experience continues to offer training resources for health care providers and staff. Our on-demand courses can help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network. We recently added the following new learning opportunities:
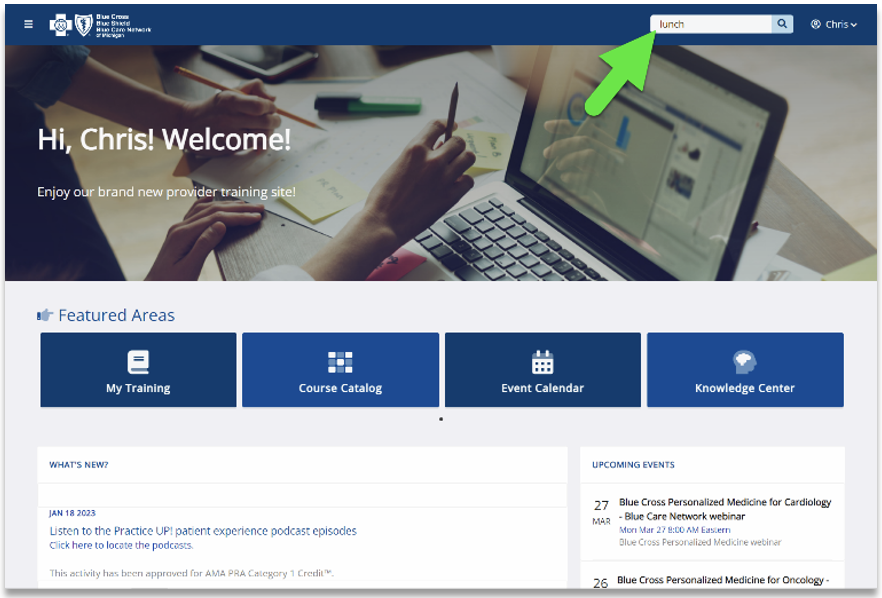
These are both on-demand courses, so you can complete them at your own pace. To locate the courses, enter Star for the CMS Star measures course and HEDIS for the HEDIS measures course in the search box at the upper right corner of the training site. Also, check out the dashboard on our provider training site, which can enhance the training experience for health care providers and staff. The site features announcements of new courses, including those with CME offerings. If you don’t already have access to the training site, you can request it by completing the following steps:
If you need assistance creating your login ID or navigating the site, contact ProviderTraining@bcbsm.com. HEDIS®, which stands for Healthcare Effectiveness Data and Information Set, is a registered trademark of the National Committee for Quality Assurance.
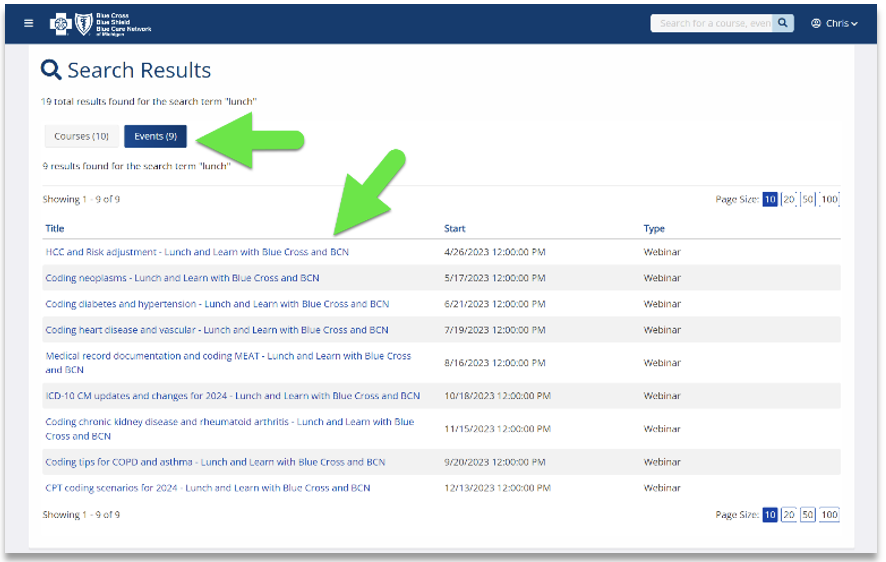
Lunch and learn webinars for physicians and coders focus on risk adjustment, codingWe’re offering educational webinars that will provide updated information on documentation and coding of common challenging diagnoses. These live, lunchtime sessions will also include an opportunity to ask any questions that you may have. Here’s our current schedule and the tentative topics for the webinars. These 30-minute sessions start at noon Eastern time. Log in to the provider training website and register for the session that best works with your schedule.
If you haven’t already registered for the provider training website, follow these steps:
Locating a session Click here if you are already registered for the provider training website. On the provider training website, look in the Event Calendar or use the search feature with the keyword lunch to quickly locate all 2023 sessions.
You can listen to the previously recorded sessions too. Check out the following:
For more information
Patient support can reduce complications when managing chronic conditionsWhen chronic conditions, such as diabetes, hypertension or cardiovascular disease, are managed, complications are reduced. And when complications are reduced, the need for urgent or emergency care services, hospitalizations and readmissions also are reduced. For quick reference, here are the latest Michigan Quality Improvement Consortium guidelines for these conditions:
Patient education and compliance are key factors to managing a chronic condition. Here is information to share with your patients from the Centers for Disease Control and Prevention:
For more information on Federal Employee Program® Service Benefit Plan incentive programs and benefits, health care providers and members can visit fepblue.org or call Customer Service at 1-800-482-3600. **Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Requirements for some medical benefit drugs change for most membersBlue Cross Blue Shield of Michigan and Blue Care Network encourage proper use of high-cost medications billed under the medical benefit. As part of this effort, we maintain comprehensive lists of requirements for our members. In January through March 2023, we added requirements for some medical benefit drugs. For Blue Cross commercial and BCN commercial members: We added prior authorization requirements and site-of-care requirements as shown in the table below.
For Medicare Plus Blue℠ and BCN Advantage℠ members: We added prior authorization requirements as shown in the table below.
Drug lists For additional details, see the following drug lists:
These lists are also available by following these steps:
Additional information about these requirements We communicated these changes previously through provider alerts, which contain additional details. You can view the provider alerts at ereferrals.bcbsm.com and on our Provider Resources site, which is accessible through our provider portal at availity.com.*** Additional information for Blue Cross commercial groups For Blue Cross commercial groups, prior authorization requirements apply only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group List. To find this list:
Note: Blue Cross and Blue Shield Federal Employee Program® members and non-Medicare United Auto Workers Retiree Medical Benefits Trust members don't participate in the standard prior authorization program. Reminder A prior authorization approval isn’t a guarantee of payment. Health care providers need to verify eligibility and benefits for members.
**May be assigned a unique code in the future.
Briumvi to have site-of-care requirement for most commercial members starting July 1For dates of service on or after July 1, 2023, we’re adding a site-of-care requirement for Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members for the following drug covered under the medical benefit:
The NovoLogix® online tool will prompt you to select a site of care when you submit prior authorization requests for this drug. If the request meets clinical criteria for the drug and is for one of the following sites of care, it will be approved automatically:
Additional information or documentation may be required for requests to administer Briumvi in an outpatient hospital setting. As a reminder, this drug already requires prior authorization; providers can submit prior authorization requests using NovoLogix. The new site-of-care requirement is in addition to the current prior authorization requirement. Members who start courses of treatment with Briumvi before July 1, 2023, will be able to continue receiving the drug in their current location until their existing authorization expires. If those members then continue treatment under a new prior authorization, the site-of-care requirement outlined above will apply. Some groups not subject to these requirements For Blue Cross commercial groups, the prior authorization and site-of-care requirements apply only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. Note: Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don’t participate in the standard prior authorization program. List of requirements For a full list of requirements related to drugs covered under the medical benefit, see the Blue Cross and BCN utilization management medical drug list for Blue Cross commercial and BCN commercial members. We’ll update this list prior to July 1, 2023. You can access this list and other information about requesting prior authorization at ereferrals.bcbsm.com, at these locations: As a reminder, authorization isn't a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members.
Rolvedon to require prior authorization for URMBT members with Blue Cross non-Medicare plansFor dates of service on or after May 31, 2023, Rolvedon™ (eflapegrastim-xnst), HCPCS code J1449, will require prior authorization through Carelon Medical Benefits Management (formerly known as AIM Specialty Health®) for UAW Retiree Medical Benefits Trust members with Blue Cross Blue Shield of Michigan non-Medicare plans. This drug is covered under the medical benefit. The prior authorization requirement applies only when Rolvedon is administered in an outpatient setting. Note: The prior authorization requirement doesn’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714). How to submit authorization requests Submit prior authorization requests to Carelon using one of the following methods:
More about authorization requirement Authorization isn’t a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members. For additional information on requirements related to drugs covered under the medical benefit for URMBT members with Blue Cross non-Medicare plans, see:
We’ll update the pertinent drug lists to reflect the information in this message prior to the effective date.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
We made some questionnaire changes in e-referral systemOn March 26 and April 9, 2023, we added, updated and removed questionnaires in the e-referral system. We also made changes in the corresponding preview questionnaires on the ereferrals.bcbsm.com website. As a reminder, we use our authorization criteria, our medical policies and your answers to the questionnaires in the e-referral system when making utilization management determinations on your authorization requests. New questionnaire On March 26, we added a Breast reduction questionnaire that’s specific to BCN Advantage℠ members. This questionnaire will open for adolescent and adult BCN Advantage members for procedure code *19318. Updated questionnaires We updated the following questionnaires on the date specified below:
Removed questionnaire On March 26, we removed the Blepharoplasty, lower lid questionnaire. Although this service continues to require prior authorization for Medicare Plus Blue, BCN commercial and BCN Advantage members, the questionnaire no longer opens. Preview questionnaires Preview questionnaires show the questions you’ll need to answer so you can prepare your answers ahead of time. To access them, go to ereferrals.bcbsm.com and follow instructions below:
Authorization criteria and medical policies The pertinent authorization criteria and medical policies are also available on the Authorization Requirements & Criteria pages.
Reminder: Anatomical modifiers requiredIn the September 2021 Record, we let you know that we require anatomical modifiers for surgical procedure codes. Anatomical modifiers identify the specific area of the body where a procedure is performed. Requiring these modifiers aligns with AMA CPT guidelines and supports our commitment to implementing payment integrity solutions that enhance payment accuracy. Please be sure to append the appropriate modifier to surgical procedures. Claims that are submitted without the appropriate anatomical modifier may receive a denial.
Starting June 1, requests for commercial LTACH admissions and extensions must be submitted through e-referralLong-term acute care hospitals, or LTACHs, in Michigan must submit prior authorization requests through the e-referral system and not by fax, starting June 1, 2023. This applies to requests for our Blue Cross Blue Shield of Michigan and Blue Care Network commercial members for:
Many LTACH providers in Michigan currently use the Blue Cross and BCN LTACH Assessment Form to fax their prior authorization requests. For Michigan providers Starting June 1, 2023, we’ll accept faxes only for urgent requests and when the e-referral system isn’t available. Follow the instructions on the document titled e-referral system maintenance times and what to do. If we receive a form for an admission or extension by fax when the e-referral system is available, we won’t accept it. We’ll notify you by fax or phone that you must submit the request through the e-referral system. For non-Michigan providers LTACH providers outside of Michigan can either:
Training opportunities We’ll schedule webinars in May on how to use the e‑referral system. Watch for upcoming communications. Sign up now to use e-referral system Get information on our ereferrals.bcbsm.com website as follows:
How to access the e-referral system Access the e-referral system through our provider portal:
You’ll first need to register for access to our portal if you haven’t already done that. Refer to the Register for web tools webpage for instructions on how to:
Submit Medicare Advantage requests to naviHealth naviHealth manages prior authorization requests for post-acute care admissions for our Medicare Plus Blue℠ and BCN Advantage℠ members. **Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
COVID-19 DRG enhancements end with public health emergencyThe federal Coronavirus Aid, Relief and Economic Security, or CARES, Act implemented a temporary inpatient diagnosis-related group enhancement for Original Medicare payments. The DRG enhancement represented a 20% increase in the weighting factor for inpatient DRG payments for Medicare patients diagnosed with COVID-19. Blue Cross Blue Shield of Michigan and Blue Care Network applied the DRG enhancement to our Medicare Advantage plans (Medicare Plus Blue℠ and BCN Advantage℠) for both in-network and out-of-network providers. When the public health emergency ends on May 11, 2023, the DRG enhancement will also end. For more information on changes occurring with the end of the public health emergency, see our Temporary changes due to the COVID-19 pandemic document.
Lunch and learn webinars for physicians and coders focus on risk adjustment, codingWe’re offering educational webinars that will provide updated information on documentation and coding of common challenging diagnoses. These live, lunchtime sessions will also include an opportunity to ask any questions that you may have. Here’s our current schedule and the tentative topics for the webinars. These 30-minute sessions start at noon Eastern time. Log in to the provider training website and register for the session that best works with your schedule.
If you haven’t already registered for the provider training website, follow these steps:
Locating a session Click here if you are already registered for the provider training website. On the provider training website, look in the Event Calendar or use the search feature with the keyword lunch to quickly locate all 2023 sessions.
You can listen to the previously recorded sessions too. Check out the following:
For more information
Reminder: Outpatient services provided during inpatient admission should be reported with inpatient claimBlue Cross Blue Shield of Michigan continues to expand its claim editing process to further support payment policy. Beginning in May 2023, Blue Cross payment policy requires that outpatient services provided during an inpatient admission be reported with the inpatient claim if there is a similar diagnosis. Claims submitted for outpatient services during an inpatient admission may be denied if they’re billed separately.
Requirements for some medical benefit drugs change for most membersBlue Cross Blue Shield of Michigan and Blue Care Network encourage proper use of high-cost medications billed under the medical benefit. As part of this effort, we maintain comprehensive lists of requirements for our members. In January through March 2023, we added requirements for some medical benefit drugs. For Blue Cross commercial and BCN commercial members: We added prior authorization requirements and site-of-care requirements as shown in the table below.
For Medicare Plus Blue℠ and BCN Advantage℠ members: We added prior authorization requirements as shown in the table below.
Drug lists For additional details, see the following drug lists:
These lists are also available by following these steps:
Additional information about these requirements We communicated these changes previously through provider alerts, which contain additional details. You can view the provider alerts at ereferrals.bcbsm.com and on our Provider Resources site, which is accessible through our provider portal at availity.com.*** Additional information for Blue Cross commercial groups For Blue Cross commercial groups, prior authorization requirements apply only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group List. To find this list:
Note: Blue Cross and Blue Shield Federal Employee Program® members and non-Medicare United Auto Workers Retiree Medical Benefits Trust members don't participate in the standard prior authorization program. Reminder A prior authorization approval isn’t a guarantee of payment. Health care providers need to verify eligibility and benefits for members.
**May be assigned a unique code in the future.
Briumvi to have site-of-care requirement for most commercial members starting July 1For dates of service on or after July 1, 2023, we’re adding a site-of-care requirement for Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members for the following drug covered under the medical benefit:
The NovoLogix® online tool will prompt you to select a site of care when you submit prior authorization requests for this drug. If the request meets clinical criteria for the drug and is for one of the following sites of care, it will be approved automatically:
Additional information or documentation may be required for requests to administer Briumvi in an outpatient hospital setting. As a reminder, this drug already requires prior authorization; providers can submit prior authorization requests using NovoLogix. The new site-of-care requirement is in addition to the current prior authorization requirement. Members who start courses of treatment with Briumvi before July 1, 2023, will be able to continue receiving the drug in their current location until their existing authorization expires. If those members then continue treatment under a new prior authorization, the site-of-care requirement outlined above will apply. Some groups not subject to these requirements For Blue Cross commercial groups, the prior authorization and site-of-care requirements apply only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list. Note: Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don’t participate in the standard prior authorization program. List of requirements For a full list of requirements related to drugs covered under the medical benefit, see the Blue Cross and BCN utilization management medical drug list for Blue Cross commercial and BCN commercial members. We’ll update this list prior to July 1, 2023. You can access this list and other information about requesting prior authorization at ereferrals.bcbsm.com, at these locations: As a reminder, authorization isn't a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members.
Rolvedon to require prior authorization for URMBT members with Blue Cross non-Medicare plansFor dates of service on or after May 31, 2023, Rolvedon™ (eflapegrastim-xnst), HCPCS code J1449, will require prior authorization through Carelon Medical Benefits Management (formerly known as AIM Specialty Health®) for UAW Retiree Medical Benefits Trust members with Blue Cross Blue Shield of Michigan non-Medicare plans. This drug is covered under the medical benefit. The prior authorization requirement applies only when Rolvedon is administered in an outpatient setting. Note: The prior authorization requirement doesn’t apply to the UAW Retiree Health Care Trust (group number 70605) or the UAW International Union (group number 71714). How to submit authorization requests Submit prior authorization requests to Carelon using one of the following methods:
More about authorization requirement Authorization isn’t a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members. For additional information on requirements related to drugs covered under the medical benefit for URMBT members with Blue Cross non-Medicare plans, see:
We’ll update the pertinent drug lists to reflect the information in this message prior to the effective date.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||