|
July 2023

Help patients avoid being balance billed by noncontracted ambulance services
Action item
Health care providers should order transfers only from contracted ambulance services when arranging for non-emergency ground transfers to prevent patients from being balance billed large amounts from noncontracted ambulance services.
Blue Cross Blue Shield of Michigan and Blue Care Network haven’t been able to secure a network contract with Superior Ambulance Service. Superior remains noncontracted (or nonparticipating) and continues to balance bill our members for amounts nearly four times our in-network rates.
You can help us prevent this type of situation from occurring with our Blue Cross commercial, Medicare Plus Blue℠, BCN commercial and BCN Advantage℠ members. As a reminder, health care providers should order transfers from contracted ambulance services when arranging for non-emergency ground transfers to prevent patients from being balance billed large amounts from noncontracted ambulance services.
To determine which ground ambulance services are contracted with or participate with a member’s health plan:
- Go to bcbsm.com.
- Click on Find a Doctor.
- Click on the Search without logging in link.
- If prompted, choose a location.
- In the upper-right corner of the screen, do one of the following:
- Click on the I don’t know my network button.
- Click on the Change your location or plan link and then click on I don’t know my network.
- Click on the Find a different plan button.
- Select the appropriate plan.
- Click on the Confirm selection button.
- Click on Places by type.
- Enter Land ambulance or the name of a specific ambulance provider and press Enter.
The search results include the ground ambulance services that are contracted with or participate with the plan you selected.
See our Ground Ambulance Services medical policy for additional information. To view the policy:
- Go to bcbsm.com/providers.
- Click on Resources.
- Scroll down the page and click on the Search Medical Policies button.
- In the Medical Policy Router Search page, enter ground ambulance services in the Policy/Topic Keyword field and press Enter.
- Click on the Medical Policy – Ground Ambulance Services link.
Reminder: Only charge patients their cost share
When you treat a patient with Blue Cross Blue Shield of Michigan or Blue Care Network coverage, including our Medicare Advantage plans, Medicare Plus Blue℠ or BCN Advantage℠, be sure to bill Blue Cross or BCN for covered services and only charge the member the appropriate cost share according to their health plan coverage.
Always ask to see the patient’s health plan ID card and check their eligibility and benefits through one of these methods:
- Eligibility and Benefits Inquiry in our provider portal
- Provider Inquiry (Professional providers: 1-800-344-8525; hospital and facility providers: 1-800-249-5103)
- Electronic standard transaction
This can help you determine the appropriate member cost share, including deductible, coinsurance and copay, prior to providing the service so you can charge the member the correct amount at the time of service.
As an alternative, you can provide the service, submit the claim and wait for the remittance advice or voucher to explain the member’s cost share before billing the member. If you wait to bill the member, be sure to check that the member’s coverage is active and that the service you’re providing is a covered benefit before providing the service.
Our provider agreements prohibit participating or contracted providers from charging Blue Cross or BCN members any amounts beyond the member’s applicable cost share. If the remittance advice or voucher indicates the member’s cost share should have been less than what you charged, you’ll need to refund the member the overcharged amount.
Change to member reimbursement
Blue Cross and BCN are changing the way we manage reimbursement requests from members with Blue Cross and BCN commercial coverage. When a member sends in a request for reimbursement, we’ll look to see if the health care provider is a participating or contracted provider. If so, we’ll direct payment to the provider. The provider will then need to reimburse the member.
If your practice has been asking patients to pay for the service and request reimbursement from us, this will result in additional work for you.
2023 CPT code update: New Category I vaccine code added
Medicine vaccines/toxoids
Code |
Change |
Coverage comments |
Effective date |
90679 |
Added |
Not covered |
May 3, 2023 |
None of the information above is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Billing chart: Blue Cross highlights medical, benefit policy changes
You’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart.
This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures.
We'll publish information about new Blue Cross groups or changes to group benefits under the Group Benefit Changes heading.
For more detailed descriptions of the Blue Cross' policies for these procedures, check under the Commercial Policy tab in Benefit Explainer on Availity®. To access this online information:
1. Log in to availity.com.
2 .Click on Payer Spaces on the Availity menu bar.
3. Click on the BCBSM and BCN logo.
4. Click on Benefit Explainer on the Applications tab.
5. Click on the Commercial Policy tab.
6. Click on Topic.
7. Under Topic Criteria, click on the circle for Unique Identifier and click the drop-down arrow next to Choose Identifier Type, then click on HCPCS Code.
8. Enter the procedure code.
9. Click on Finish.
10. Click on Search.
| Code* |
BCBSM changes to:
Basic Benefit and Medical Policy, Group
Variations Payment Policy, Guidelines
|
| NEW PAYABLE PROCEDURES |
15877**
Additional covered codes:
15832, 15833, 15836, 15878, 15879, 15834, 15835, 38999,*** 99199***
Not covered:
15839, 15876
**Inclusionary criteria and coverage for *15877 have been added, effective March 1, 2023.
Payment policy:
***Not otherwise classified procedures requiring individual consideration |
Basic benefit and medical policy
Surgical treatment for lipedema
The safety and effectiveness of suction-assisted lipectomy and surgical removal of excessive abnormal adipose tissue by excision involving the arms, legs, trunk and buttocks have been established for select patients. It may be considered a useful therapeutic option when indicated.
All surgical interventions should be performed by hospital-credentialed, board-certified plastic surgeons. Photographs should accompany all requests.
Inclusions:
Liposuction/excision/debulking for lipedema of the extremities may be a therapeutic option when all the following criteria are met.
- The diagnosis of lipedema can be documented by clinical exam and photography on the basis of all the following:
- Typical appearance of extremity involvement with thickened subcutaneous fat in the affected extremities bilaterally and symmetrically
- Pain or hypersensitivity to touch in lipelipedema-affectedas
- History of easy bruising or bruising without apparent cause in lipedema-affected areas
- Tenderness and nodularity of fat deposits in lipedema-affected areas (dimpled or orange peel texture)
- Documentation of significant physical functional impairment (e.g., difficulty ambulating or difficulty performing activities of daily living) or medical complications such as recurrent cellulitis or skin ulcerations.
- A failed response to three or more consecutive months of conservative management (compression or manual therapy)
- Lack of improvement on lipedema-affected areas with weight loss
- Lack of improvement of swelling with limb elevation
- Absence of pitting edema (no “pitting” when finger or thumb pressure is applied to the area of fat unless there is comorbid lymphedema)
Liposuction for lipedema of the trunk may be a therapeutic option when all the following criteria are met:
- The diagnosis of lipedema can be documented by clinical exam and photography on the basis of all the following:
- Pain or hypersensitivity to touch in lipedema-affected areas
- History of easy bruising or bruising without apparent cause in lipedema-affected areas
- Tenderness and nodularity of fat deposits in lipedema-affected areas (dimpled or orange peel texture)
- A failed response to three or more consecutive months of conservative management (compression or manual therapy)
- Lack of improvement of weight loss on lipedema-affected areas
Exclusions:
- Liposuction/excision/debulking for indications other than lipedema or lymphedema (reference lymphedema-surgical treatment policy) that don’t meet criteria is considered cosmetic and therefore not covered.
- Liposuction/excision/debulking of excess adipose tissue or excessive subcutaneous skin for the diagnosis of lipedema involving the head and neck area.
|
95012
Experimental:
83987 |
Basic benefit and medical policy
Exhaled nitric oxide/exhaled breath condensate
Measurement of fractional exhaled nitric oxide is considered established in the diagnosis of mild, moderate or severe asthma and the management of asthma when criteria are met.
Measurement of fractional exhaled nitric oxide in the diagnosis and management of other respiratory disorders such as asthma variants (for example, eosinophilic asthma, cough variant asthma and asthma-COPD overlap syndrome) is considered established when criteria are met.
Measurement of exhaled breath condensate in the diagnosis and management of other respiratory disorders including, but not limited to, chronic obstructive pulmonary disease and chronic cough is considered experimental.
The clinical utility of exhaled breath condensate in the diagnosis and management of respiratory disorders, including asthma, hasn’t been demonstrated. In addition, there is insufficient evidence that the use of this test improves health outcomes.
This policy change is effective March 1, 2023.
Payment policy:
Modifiers 26 and TC don’t apply to this procedure.
Inclusions:
Diagnosis of asthma:
Measurement of fractional exhaled nitric oxide, or FeNO, is considered medically necessary. It’s covered when used as an adjunctive test to aid in the diagnosis of asthma using spirometry for individuals with suspected mild, moderate, severe asthma or asthma variants.
Management of asthma:
Measurement of fractional exhaled nitric oxide, or FeNO, in individuals with an established diagnosis of mild, moderate, severe asthma or asthma variants is considered medically necessary and is established when used for any of the following purposes:
- Evaluation of response to anti-inflammatory treatment
- Monitoring compliance with anti-inflammatory treatment
- Aid with identification of underlying inflammatory phenotype or identification of inflammatory phenotypes to guide with the appropriate therapy
Exclusions:
Measurement of fractional exhaled nitric oxide, or FeNO, for the diagnosis and management of other respiratory disorders including, but not limited to, chronic obstructive pulmonary disease, or COPD, and chronic cough, is considered experimental. The safety and efficacy of these procedures haven’t been shown to improve clinical health outcomes.
Measurement of exhaled breath condensate in the diagnosis and management of asthma and other respiratory disorders including, but not limited to, chronic obstructive pulmonary disease and chronic cough is considered experimental. The safety and efficacy of these procedures haven’t been shown to improve clinical health outcomes. |
| POLICY CLARIFICATIONS |
0338T, 0339T |
Basic benefit and medical policy
RFA of renal sympathetic nerves as treatment for resistant or uncontrolled hypertension
Radiofrequency ablation of the renal sympathetic nerves as a treatment of resistant or uncontrolled hypertension is considered experimental. The evidence is insufficient to determine whether radiofrequency ablation of the renal sympathetic nerves improves health outcomes in patients with resistant hypertension.
The medical policy statement has been updated, effective May 1, 2023.
Inclusionary and exclusionary guidelines:
Not applicable |
11920, 11921, 11922, 17380, 17999,** 19303, 19318, 19325, 19350, 21120, 21121, 21122, 21123, 21125, 21127, 21137, 21138, 21139, 21209, 30400, 30410, 30420, 31599,** 31899,** 54520, 55970, 55980, 56805, 57291, 57292, 57335, 58150, 58152, 58180, 58260, 58262, 58275, 58291, 58541, 58542, 58543, 58544, 58550, 58552, 58553, 58554
Experimental
11950, 11951, 11952, 11954, 15769, 15771, 15772, 15773, 15774, 15820, 15821, 15822, 15823, 15824, 15825, 15826, 15828, 15830, 15832, 15833, 15834, 15835, 15836, 15837, 15838, 15839, 15876, 15877, 15878, 15879, 19316, 21208, 30430, 30435, 30450, 69300, Q2026, Q2028
**Unlisted codes |
Basic benefit and medical policy
Gender-affirming services
The safety and effectiveness of select medical and surgical treatments for gender dysphoria have been established. The established treatments for gender dysphoria include:
- Puberty suppression in adolescents
- Hormone therapy (for masculinization/feminization) for adolescents who meet criteria, and adults
- Medically necessary gender-affirming surgery:**
- Genitalia reconstruction
- Mastectomy for a transgender man (a person who has a gender identity as a man and who was assigned female at birth)
- Augmentation mammoplasty (implants) for transgender women (a person who has a gender identity as a woman and who was assigned male at birth)
- Thyroid reduction chondroplasty (tracheal shave)
- Facial feminization
- Facial masculinization
**Gender-affirming surgery may require prior authorization.
Gender-specific services may be medically necessary for transgender and gender-diverse people appropriate to their anatomy. Examples include:
- Breast cancer screening in transgender and gender-diverse people with breasts from natal puberty who haven’t undergone gender-affirming chest surgery and for transgender and gender-diverse people who have received estrogens, taking into account the length of time of hormone use, dosing, current age and age at which the hormones were initiated
- Prostate cancer screening for transgender and gender-diverse people who have retained their prostate
- Cervical screening for transgender and gender-diverse people who currently have or previously had a cervix following local guidelines for cisgender women
- Obstetric services for transgender and gender-diverse people when they are pregnant
- To guide preventive medical care, any anatomical structure present that warrants screening should be screened, regardless of gender identity.
Exclusionary criteria have been updated, effective May 1, 2023.
Inclusions:
While the following procedures are considered established for this policy, the specific coverage for each member is based on the benefit, which is defined by the group or employer.
Assessment, diagnosis and treatment should be provided through a multidisciplinary gender services clinic or program affiliated with a major medical center. If this level of service is unavailable, there should be documentation that reflects a coordinated approach to care by specialists involved (mental health specialists, physicians, surgeons, etc.).
Puberty suppression**
Health care professionals taking care of transgender and gender-diverse adolescents should involve relevant disciplines, including mental health and medical professionals, to reach a decision about whether puberty suppression, hormone initiation or gender-related surgery for these adolescents is appropriate and remain involved throughout the course of treatment until the transition is made to adult care. Puberty suppression hormones for adolescents may be indicated for members who meet all the following inclusionary criteria:
- Meets diagnostic criteria for gender dysphoria.
- Gender dysphoria is marked and sustained.
- Demonstrates emotional and cognitive maturity required to provide informed consent for the treatment; and, particularly when the adolescent hasn’t reached the age of medical consent, the parents, guardians or other legally authorized caretakers have consented to the treatment and are involved in supporting the adolescent throughout the treatment process.
- Mental health concerns (if any) that may interfere with diagnostic clarity, capacity to consent and gender-affirming medical treatments have been addressed; sufficiently so that gender-affirming medical treatment can be provided optimally.
- Onset of puberty to at least Tanner stage 2 has been reached.
- The absence of contraindications to therapy in the judgment of the managing physician.
**Medications for puberty suppression may be managed under the member’s pharmacy benefit.
Hormone therapy**
Hormone therapy may be indicated for members that meet all the following inclusionary criteria.
Inclusions for adolescents, defined as from the start of puberty until the legal age of majority (18 years of age):
- Meets diagnostic criteria for gender dysphoria.
- Gender dysphoria is marked and sustained.
- Demonstrates emotional and cognitive maturity required to provide informed consent for the treatment; and, particularly when the adolescent hasn’t reached the age of medical consent, the parents, guardians or other legally authorized caretakers have consented to the treatment and are involved in supporting the adolescent throughout the treatment process.
- Mental health concerns (if any) that may interfere with diagnostic clarity, capacity to consent, and gender-affirming medical treatments have been addressed; sufficiently so that gender-affirming medical treatment can be provided optimally.
- Onset of puberty to at least Tanner stage 2 has been reached.
- The absence of contraindications to therapy in the judgment of the managing physician.
- One letter of assessment as indicated below***
- Medications will be prescribed by or in consultation with a pediatric endocrinologist that has collaborated care with a mental health care provider for members less than 18 years of age.
Inclusions for adults:
- Age 18 or older (age of majority).
- Meets diagnostic criteria for gender dysphoria.
- Gender dysphoria is marked and sustained.
- Other possible causes of apparent gender incongruence have been identified and excluded.
- Demonstrates capacity to make a fully informed decision and to consent for gender-affirming hormone treatment.
- The absence of contraindications to therapy in the judgment of the managing physician.
- Mental health and physical conditions that could negatively affect the outcome of gender-affirming medical treatments have been assessed, with the risks and benefits discussed, before a decision is made regarding treatment.
**Medications for hormone therapy may be managed under the member’s pharmacy benefit.
Hair removal
- If gender-affirming surgery is approved for a transgender or gender-diverse person, hair removal (e.g., electrolysis, laser hair removal) may be considered established following medical review:
- Hair removal is considered established only when the scrotal and surrounding tissues are used in the surgical construction of the vagina.
- Hair removal is considered established only when free flap, or other donor tissues, are used for phalloplasty performed in conjunction with vaginectomy and full-length urethroplasty.
Gender affirming surgery
Inclusions:
Gender-affirming surgery may be indicated for members that meet all the following inclusionary criteria:
- Chest surgery**
- Mastectomy is considered reconstructive when all the following criteria have been met:
- The individual is at least 18 years of age.
- The individual has been diagnosed with gender dysphoria (see Description/Background section for diagnostic criteria).
- Gender dysphoria is marked and sustained.
- The individual has capacity to make fully informed decisions and consent for treatment.
- One letter of assessment as indicated below***
- Other possible causes of apparent gender incongruence have been identified and excluded.
- Mental health and physical conditions that could negatively affect the outcome of gender-affirming medical treatments have been assessed, with the risks and benefits discussed, before a decision is made regarding treatment.
- Hormone therapy prior to mastectomy isn’t required, as the aim of hormone therapy before facial surgery or gonadectomy is primarily to introduce a period of reversible testosterone or estrogen suppression before the individual undergoes irreversible surgical intervention.
- Living in a gender role congruent with gender identity for 12 continuous months isn’t required prior to a mastectomy.
- Pre-operative and post-operative care that addresses both surgical results and possible behavioral health results is highly recommended.
Nipple reconstruction, including tattooing, following a gender affirming mastectomy that meets the reconstructive criteria above is considered reconstructive.
- Breast augmentation is considered reconstructive when all the following criteria have been met:
- The individual is at least 18 years of age.
- The individual has been diagnosed with gender dysphoria (see Description/Background section for diagnostic criteria).
- Gender dysphoria is marked and sustained.
- The individual has capacity to make fully informed decisions and consent for treatment.
- One letter of assessment as indicated below***
- Other possible causes of apparent gender incongruence have been identified and excluded.
- Mental health and physical conditions that could negatively affect the outcome of gender-affirming medical treatments have been assessed, with the risks and benefits discussed, before a decision is made regarding treatment.
- The individual is stable on their gender-affirming hormonal treatment regimen for at least 12 months, unless a rationale is provided by the HCP that indicates that hormone treatment is either contraindicated or not necessary for the individual’s clinical situation.
- Living in a gender role congruent with gender identity for 12 continuous months isn’t required prior to breast augmentation.
- Existing chest appearance demonstrates significant variation from normal appearance for the experienced gender.
- Pre-operative and post-operative care that addresses both surgical results and possible behavioral health results is highly recommended.
Note: ***The procedures needed to reconstruct a feminine/masculine appearance can only be performed once per lifetime.
- Facial surgery† is considered reconstructive when all the following criteria have been met:
- The individual is at least 18 years of age.
- The individual has been diagnosed with gender dysphoria (see Description/Background section for diagnostic criteria).
- Gender dysphoria is marked and sustained.
- The individual has capacity to make fully informed decisions and consent for treatment.
- Other possible causes of apparent gender incongruence have been identified and excluded.
- One letter of assessment as indicated below***
- Mental health and physical conditions that could negatively affect the outcome of gender-affirming medical treatments have been assessed, with the risks and benefits discussed, before a decision is made regarding treatment.
- The individual is stable on their gender-affirming hormonal treatment regimen for at least 12 months, unless a rationale is provided by the HCP that indicates that hormone treatment is either contraindicated or not necessary for the individual’s clinical situation.
- The new gender identity should be present for at least 12 months.
- The member has a consistent stable gender identity that is well documented by their treating providers and, when possible, lives as their affirmed gender in places where it is safe to do so.
- Existing facial appearance demonstrates significant variation from normal appearance for the experienced gender.
- The procedure directly addresses variation from normal appearance for the experienced gender (Note: Each procedure requested should be considered separately as some procedures may be cosmetic and others may be reconstructive).
- Pre-operative and post-operative care that addresses both surgical results and possible behavioral health results is highly recommended.
Note: ***The procedures needed to reconstruct a feminine/masculine appearance can only be performed once per lifetime.
†List of procedures included in this group is thyroid reduction chondroplasty (tracheal shave), genioplasty (repositioning or reshaping of the chin), mandible augmentation (jawline contouring/reconstruction), facial bone reduction, forehead reduction/contouring, rhinoplasty (reshaping/contouring of the nose).
- Genital surgery is considered medically necessary when all the following criteria have been met:
- The individual is at least 18 years of age.
- The individual has been diagnosed with gender dysphoria (see Description/Background section for diagnostic criteria).
- Gender dysphoria is marked and sustained.
- The individual has capacity to make fully informed decisions and consent for treatment.
- Other possible causes of apparent gender incongruence have been identified and excluded.
- One letter of assessment as indicated below****
- Mental health and physical conditions that could negatively affect the outcome of gender-affirming medical treatments have been assessed, with the risks and benefits discussed, before a decision is made regarding treatment.
- The individual is stable on their gender affirming hormonal treatment regimen for at least 12 months, unless a rationale is provided by the HCP that indicates that hormone treatment is either contraindicated or not necessary for the individual’s clinical situation.
- The new gender identity should be present for at least 12 months.
- The member has a consistent stable gender identity that is well documented by their treating providers and, when possible, lives as their affirmed gender in places where it is safe to do so.
- Pre-operative and post-operative care that addresses both surgical results and possible behavioral health results is highly recommended.
These criteria don’t apply to patients who are having these surgical procedures for medical indications other than gender dysphoria.
***Letter requirements:
- Required for hormone therapy for adolescents
- Required for facial, pelvic, gonadal and/or genital surgery for adults
Adolescents
One letter of assessment from the multidisciplinary team (or in situations where a multidisciplinary team is not available, a professional from one of the multiple disciplines who are experts in transgender health and in the management of the care required for transgender and gender-diverse adolescents who is taking care of the individual) is required for adolescents receiving gender-affirming medical treatment. This letter needs to reflect the assessment and opinion of the team, which involves both medical HCPs and mental health professionals, supports that the individual meets the criteria for gender dysphoria. The detailed assessment must have been performed within 12 months of the requested submission.
The HCP assessing and working with the adolescent should meet all the following criteria:
- Are licensed by their professional body and hold a postgraduate degree or its equivalent in a clinical field related to transgender health granted by a nationally accredited institution.
- Receive theoretical and evidenced-based training and develop expertise in general child, adolescent, and family mental health across the developmental spectrum.
- Receive training and have expertise in gender identity development, gender diversity in children and adolescents, have the ability to assess capacity to assent/consent and possess general knowledge of gender diversity across the life span.
- Continue engaging in professional development in all areas relevant to gender-diverse children, adolescents, and families.
Adults
One letter of assessment from an HCP who has competencies in the assessment of transgender and gender-diverse people documenting that the individual meets the criteria for gender dysphoria is required for transgender and gender-diverse adults who meet the below criteria for gender-affirming medical and surgical treatments. The detailed assessment must have been performed within 12 months of the requested submission.
The HCP should meet all the following criteria:
- Are licensed by their professional body and hold, at a minimum, a master’s degree or equivalent training in a clinical field related to transgender health or equivalent further clinical training in this area and granted by a nationally accredited institution.
- Should be competent using the latest edition of the Diagnostic and Statistical Manual of Mental Disorders, or DSM-5, for diagnosis.
- Are able to identify co-existing mental health or other psychosocial concerns and distinguish these from gender dysphoria, incongruence and diversity.
- Are able to assess capacity to consent for treatment.
- Have experience or be qualified to assess clinical aspects of gender dysphoria, incongruence and diversity.
- Undergo continuing education in health care relating to gender dysphoria, incongruence and diversity.
Exclusions:
- Gender-affirming services aren’t covered if contract or certificate language contains specific exclusion of these services.
- Reversal of physical or functional outcomes due to gender-affirming services.
- Reversal of surgical procedures performed for gender-affirming services.
- All procedures that are primarily cosmetic and not reconstructive or not medically necessary including, but not limited to:
- Abdominoplasty
- Blepharoplasty
- Brow lift
- Calf implants
- Cheek/malar implants
- Chin/nose implants
- Collagen injections
- Drugs for hair loss or growth
- Forehead lift
- Hair removal (for exception: see Inclusions, Electrolysis)
- Hair transplantation
- Injectable dermal fillers (for example, Sculptra, Radiesse)
- Lip reduction
- Liposuction
- Mastopexy
- Neck tightening
- Otoplasty
- Pectoral implants
- Removal of redundant skin
- Rhytidectomy
- Speech-language therapy
- Non-covered services
|
20979, E0760 |
Basic benefit and medical policy
Bone stimulation for fracture healing
The safety and effectiveness of low-intensity ultrasound treatment for the treatment of specified fractures have been established. It’s a useful therapeutic option for patients at high risk for delayed fracture healing or nonunion.
Inclusionary criteria have been updated, effective May 1, 2023.
Inclusions:
- Low-intensity ultrasound treatment may be considered established when used as an adjunct to conventional management (for example, closed reduction and cast immobilization) for the treatment of fresh, closed fractures in skeletally mature individuals. A fracture is most commonly defined as “fresh” for seven days after the fracture occurs. Candidates for ultrasound treatment are those at high risk for delayed fracture healing or nonunion. These risk factors may include either locations of fractures or patient comorbidities and include the following:
Patient comorbidities:
- Diabetes
- Steroid therapy
- Osteoporosis
- Autoimmune disease
- Chemotherapy
- History of or current alcoholism
- History of or current smoking
- Over age 60
Fracture locations:
- Jones fracture (fracture in the meta-diaphyseal junction of the fifth metatarsal of the foot)
- Fracture of navicular bone in the wrist (also called the scaphoid)
- Closed fractures of the distal radius (Colles fracture)
- Closed or grade I open, tibial diaphyseal fractures
- Fracture of metatarsal
- Fractures associated with extensive soft tissue or vascular damage
- Low-intensity ultrasound treatment may be considered established when used as a treatment of delayed union of bones, excluding the skull and vertebra. Delayed union is defined as a decelerating healing process as determined by serial X-rays, together with a lack of clinical and radiologic evidence of union, bony continuity, or bone reaction at the fracture site for no less than three months from the index injury or the most recent intervention.
- Low intensity ultrasound treatment may be considered established for nonunion of the appendicular skeleton (non-skull or vertebrae) if there has been no X-ray evidence of progression of healing for three or more months despite appropriate fracture care, and all the following criteria are met:
- Bone is noninfected.
- Bone is stable on both ends by means of cast or fixation.
- The two portions of the involved bone are separated by less than 1cm.
- Nonunion isn’t related/secondary to malignancy.
Exclusions:
Other applications of low-intensity ultrasound treatment are experimental including, but not limited to, treatment of:
- Congenital pseudarthroses
- Open fractures
- Fresh surgically treated closed fractures in patients who aren’t at high risk for delayed fracture healing or nonunion stress fractures
- Stress fractures
- Arthrodesis
- Failed arthrodesis
|
20982, 32994, 32998, 50542, 50592, 58674
Experimental
0673T |
Basic benefit and medical policy
Radiofrequency ablation of miscellaneous solid tumors
The safety and effectiveness of radiofrequency ablation to palliate pain in patients with osteolytic bone metastases have been established. It may be considered a useful therapeutic option when indicated.
The safety and effectiveness of radiofrequency ablation of osteoid osteomas have been established. It may be considered a useful therapeutic option when indicated.
The safety and effectiveness of radiofrequency ablation of renal tumors have been established. It may be considered a useful therapeutic option when indicated.
Radiofrequency ablation is an established treatment option in selected patients with primary, non-small cell lung cancer and metastatic pulmonary tumors who aren’t candidates for surgical intervention.
Exclusionary criteria have been updated, effective May 1, 2023.
Inclusions:
Radiofrequency ablation is appropriate to palliate pain in patients with osteolytic bone metastases for those who have failed or are poor candidates for standard treatments such as radiation or opioids.
Radiofrequency ablation is appropriate for osteoid osteomas for those who can’t be managed successfully with medical treatment.
Radiofrequency ablation is appropriate to treat localized renal cell carcinoma that is no more than 4 cm in size when any of the following criteria are met:
- It’s necessary to preserve kidney function in patients with significantly impaired renal function (i.e., the patient has one kidney or renal insufficiency defined by a glomerular filtration rate [GFR] of less than 60 mL/min/m2).
- The standard surgical approach (i.e., resection of renal tissue) is likely to substantially worsen existing kidney function.
- The patient isn’t considered a surgical candidate.
Radiofrequency ablation is appropriate to treat an isolated peripheral non-small cell lung cancer lesion that is no more than 3 cm in size when all the following criteria are met:
- Surgical resection or radiation treatment with curative intent is considered appropriate based on stage of disease, however, medical co-morbidity renders the individual unfit for those interventions.
- The tumor is located at least 1 cm from the trachea, main bronchi, esophagus, aorta, aortic arch branches, pulmonary artery and the heart.
Radiofrequency ablation is appropriate to treat malignant non-pulmonary tumors metastatic to the lung that are no more than 3 cm in size when all the following criteria are met:
- It’s necessary to preserve lung function when surgical resection or radiation treatment is likely to substantially worsen pulmonary status.
- The patient isn’t considered a surgical candidate.
- There’s no evidence of extrapulmonary metastases.
- The tumor is located at least 1 cm from the trachea, main bronchi, esophagus, aorta, aortic arch branches, pulmonary artery and the heart.
Additional criteria that have been developed by clinical judgment/consensus and existing guidelines for the use of radiofrequency ablation in metastatic tumors to the lung are as follows:
- No more than three tumors per lung should be ablated.
- Tumors should be amenable to complete ablation.
- Twelve months should elapse before a repeat ablation is considered.
Radiofrequency ablation may be appropriate to treat uterine fibroids (Refer to “Myolysis of Uterine Fibroids using Laparoscopic, Percutaneous, or Transcervical Techniques” for criteria)
Exclusions:
- Breast tumors
- Lung cancer not meeting the criteria above
- Renal cell cancer not meeting the criteria above
- Osteoid osteomas that can be managed with medical treatment
- Initial treatment of painful bony metastases
- Benign thyroid nodule
- All indications and tumor types not specifically noted in the Inclusion section of this policy
|
38204-38215, 38230, 38232, 38240-38243, 81267, 81268, 81370-81383,
86812, 86813, 86816, 86817, 86821,
S2140, S2142, S2150 |
Basic benefit and medical policy
Hematopoietic cell transplantation for acute myeloid leukemia and blastic plasmacytoid dendritic cell neoplasm
The safety and effectiveness of hematopoietic cell transplantation for acute myeloid leukemia and blastic plasmacytoid dendritic cell neoplasm, known as BPDCN, have been established. It may be considered a useful therapeutic option for patients meeting specified guidelines.
Inclusionary criteria have been updated, effective May 1, 2023.
Inclusions:
- Allogeneic hematopoietic cell transplantation, or HCT, using a myeloablative conditioning regimen for patients with one of the following:
- Poor- to intermediate-risk AML in first complete remission, or CR1 (see Policy Guidelines for information on risk stratification)
- AML that is refractory to standard induction chemotherapy but can be brought into CR with intensified chemotherapy; (note: primary refractory acute myeloid leukemia [AML] is defined as leukemia that doesn’t achieve a complete remission after conventionally dosed [non-marrow ablative] chemotherapy)
- AML that relapses following chemotherapy-induced CR1 but can be brought into CR2 or beyond with intensified induction chemotherapy
- AML in patients who have relapsed following a prior autologous HCT, but can be brought into CR with intensified induction chemotherapy and are medically able to tolerate the procedure.
- AML in patients who have relapsed more than 6 months post allogeneic hematopoietic cell transplantation
- AML in patient when the first allogeneic hematopoietic cell transplantation was unsuccessful due to primary graft failure
- Blastic plasmacytoid dendritic cell neoplasm following first complete remission CR1
- Allogeneic hematopoietic cell transplantation, or HCT, using a reduced-intensity conditioning regimen in patients with one of the following:
- AML who are in complete marrow and extramedullary remission (CR1 or beyond), and who for medical reasons would be unable to tolerate a myeloablative conditioning regimen (See Policy Guidelines section)
- AML in patients who have relapsed more than six months post allogeneic hematopoietic cell transplantation
- AML in patient when the first allogeneic hematopoietic cell transplantation was unsuccessful due to primary graft failure
- BPDCN-reduced intensity conditioning may be considered in patients who achieve CR but cannot tolerate myeloablative transplantation
- Autologous hematopoietic stem-cell transplantation, or HCT, in patients with one of the following:
- AML in CR1 or beyond
- Relapsed AML if responsive to intensified induction chemotherapy
Exclusions:
All other indications not specified under the inclusions. |
73225, 70544, 70545, 70546, 70547, 70548, 70549, 71555, 72198, 73725, 74185, 72159 |
Basic benefit and medical policy
Magnetic resonance angiography and venography
The magnetic resonance angiography and venography
policy has been updated to cover procedure *73225 when criteria are met, effective March 1, 2023.
The safety and effectiveness of magnetic resonance angiography, or MRA, and magnetic resonance venography, or MRV, specified conditions of the head, chest, abdomen, pelvis, spinal canal, upper/lower extremities and allergy have been established. They may be considered useful diagnostic options in patients with documented allergy to iodinated contrast material and in patients who have accelerating hypertension or accelerating renal insufficiency.
MRA inclusions:
Head and neck:
- MRA is used to evaluate the carotid arteries, the Circle of Willis, the anterior, middle or posterior cerebral arteries, the vertebral or basilar arteries or the venous sinuses for diagnosis of suspected stenosis of occlusion or management of known stenosis or occlusion with worsening neurologic symptoms or signs.
- MRA for the diagnosis and management of:
- Tumor
- Extracranial (carotid or vertebral) aneurysms
- Arteriovenous malformation, or AVM, or fistula, or AVF
- Dissection-intracranial or extracranial
- Fibromuscular dysplasia
- Intracranial hemorrhage in all pediatric patients and in adults with either intracerebral hemorrhage with clinical or imaging features atypical for hypertensive hemorrhage or subarachnoid hemorrhage suggested by lumbar puncture or by imaging
- Intracranial vascular occlusions or thrombosis
- Extracranial vascular occlusions or thrombosis following nondiagnostic venous ultrasound
- Intracranial or extracranial vascular occlusions or thrombosis
- MRA for the evaluation of a suspected vascular lesion:
- Horner’s syndrome
- Pulsatile tinnitus
- Trigeminal neuralgia
- MRA for the following:
- Intracranial stenosis or occlusion:
- Diagnosis of suspected intracranial stenosis
- Management of known intracranial stenosis
- Surveillance in patients with established Moyamoya disease who are being considered for revascularization
- Vascular malformations
- MRA for screening for intracranial aneurysm may be used for screening in any of the following high-risk groups:
- Two or more first-degree relatives with intracranial aneurysm or subarachnoid hemorrhage
- Heritable condition that’s associated with intracranial aneurysm (examples include autosomal dominant polycystic kidney disease and Ehlers-Danlos syndrome type IV)
- Known fibromuscular dysplasia
- MRA is used for the diagnosis and management of traumatic vascular injuries and vasculitis.
- MRA may be used for the diagnosis of clinically suspected aneurysm when:
- CT or MRI findings suspicious for aneurysm
- Neurologic signs or symptoms (including headache) suggestive of intracranial aneurysm with any of the following:
- At least one first-degree relative with intracranial aneurysm or subarachnoid hemorrhage
- Presence of a heritable condition associated with intracranial aneurysm (such as autosomal dominant polycystic kidney disease, Ehlers-Danlos syndrome type IV)
- Known fibromuscular dysplasia
- Cranial nerve deficits
- Focal nerve deficits unexplained by CT or MRI
- Headache with any of the following features:
- Sudden onset worst headache of life (“thunderclap”)
- Brought on by and occurring in association with exertion or valsalva
- Persistent headache that meets Brain Imaging Guidelines for headache and that remains undifferentiated/unexplained by MRI
- Management of known intracranial aneurysm:
- Evaluation for aneurysm progression or recurrence based on new or worsening neurologic symptoms
- Preoperative evaluation
- Initial postoperative evaluation
- Diagnosis, management and surveillance for extracranial carotid artery stenosis or occlusion in patients who are candidates for carotid revascularization when duplex arterial ultrasound can’t be performed, is nondiagnostic or shows moderate to severe stenosis or occlusion
- Intracranial or extracranial evaluation of acute- stoke or transient ischemic attack, or TIA
- Surveillance of intracranial aneurysm, initial evaluation at 6 to 12 months following diagnosis, then annually
- MRA is used for vascular evaluation prior to transcatheter aortic valve implantation/replacement. MRA of neck requires duplex arterial ultrasound first.
- MRA and contrast angiography, or CA, aren’t expected to be performed on the same patient for the diagnostic purpose prior to the application of anticipated therapy.
Spinal canal:
MRA is useful in the following circumstances:
- Preoperative or postoperative imaging
- Follow-up of prior imaging findings suggestive of a vascular lesion
Peripheral arteries of lower extremities:
Studies have proven that MRA of peripheral arteries is useful in determining the presence and extent of peripheral vascular disease in lower extremities. MRA is useful in:
- Evaluation of common femoral, superficial femoral and calf veins for suspected venous thromboembolic disease. MRA for the diagnosis and management of venous thrombosis or occlusion when venous ultrasound can’t be performed or is nondiagnostic.
- Evaluation of the lower arterial vasculature for disease when the patient is at significant risk for contrast-induced renal failure, allergic reaction to contrast material and complications associated with arterial cannulation (e.g., bleeding, poor vascular access).
- Non-invasive follow-up for prior revascularization procedure (e.g., angioplasty or surgical revascularization).
- Diagnosis, management and annual surveillance of peripheral arterial disease after venous graft has been used for surgical revascularization
- When imaging results are essential in establishing a diagnosis and/or direct management of the following conditions:
- Arterial entrapment syndrome
- Aneurysm/dilation
- Arteriovenous malformation or arteriovenous fistula
- Dissection or intramural hematoma
Peripheral arteries of upper extremities:
Studies have proven that MRA of peripheral arteries is useful for the diagnosis, management and surveillance of the following:
- Peripheral arterial disease of the upper extremities
- Vascular access procedures when ultrasound cannot be performed or is nondiagnostic
- Venous thrombosis or occlusion
- Aneurysm
- Arterial entrapment syndrome
- AVM or AVF
- Dissection or intramural hematoma
Abdomen or pelvis:
- Abdominal aortic or iliac aneurysm with elective repair of the aneurysm. MRA abdomen or pelvis for management, surveillance with endografts or surgical repair or when duplex arterial ultrasound can’t be performed or is nondiagnostic and has criteria for management and surveillance.
- Evaluation of the portal and/or hepatic venous system.
- Evaluation of the renal or aortoiliac arteries when a contrast agent is contraindicated (e.g., allergy or potential contrast-induced nephrotoxicity).
- Diagnosis, management and annual surveillance of acute aortic syndrome (including aortic dissection, rupture, intramural hematoma, penetrating ulcer and pseudoaneurysm)
- Diagnosis and management of arteriovenous malformation or fistula.
- Diagnosis and management of hematoma/hemorrhage within the abdomen
- Diagnosis and management of mesenteric ischemia or portal hypertension
- In patients suspected of having renal artery stenosis, or RAS, or renovascular hypertension
- Diagnosis of suspected aortoiliac stenosis or occlusion. Presurgical evaluation and management of known stenosis and annual surveillance of bypass grafts.
- Diagnosis and management of venous thrombosis or occlusion of major abdominal vessels, except for initial evaluation of hepatic or portal veins unless ultrasound can’t be performed or is nondiagnostic.
- Diagnosis, management and surveillance of visceral artery aneurysm involving any of the following arteries: renal, celiac, splenic, hepatic or superior/inferior mesenteric arteries and their branches
- MRA is used for vascular evaluation prior to transcatheter aortic valve implantation/replacement
Chest:
MRA of the chest is appropriate for any of the following conditions:
- For initial diagnosis, management and annual surveillance for acute aortic syndrome (aortic dissection, rupture, intramural hematoma, penetrating ulcer and pseudoaneurysm) when CTA can’t be performed or is nondiagnostic
- For screening, diagnosis, management and surveillance for aortic aneurysm
- For diagnosis, treatment planning and postoperative follow-up for conditions of the thoracic aorta such as aneurysm (true or pseudoaneurysm), dissection or stenotic/occlusive vascular disease:
- Surveillance for aneurysms <4.4 cm, annual
- Surveillance for aneurysms larger than 4.4 cm, every six months
- Atheromatous disease, adults only, to evaluate the thoracic aorta as a distal emboli source when a cardiac source hasn’t been identified on echocardiography and CTA is non-diagnostic or can’t be performed
- For diagnosis, treatment planning and postoperative surgical shunt evaluation in patients with congenital heart disease, or CHD, or developmental anomalies of the thoracic vasculature (e.g., coarctation of the aorta, right-sided aortic arch, double aortic arch, truncus arteriosus, persistent left superior vena cava, interrupted inferior vena cava, total anomalous pulmonary venous connection, partial anomalous venous connection, atresia or hypoplasia of the pulmonary arteries)
- For diagnosing a suspected pulmonary embolism when the use of intravascular iodinated contrast material is contraindicated, or as a substitute for pulmonary angiography when a VQ scan does not provide sufficient information to make treatment decisions
- MRA may be considered an option for the diagnosis and management of the following conditions:
- Hematoma
- Pulmonary ateriovenous malformation
- Pulmonary sequestration
- Subclavian steal syndrome
- Superior vena cava syndrome
- Systemic venous thrombosis or occlusion
- Thoracic outlet syndrome
- MRA is used for vascular evaluation prior to transcatheter aortic valve implantation/replacement
Allergy:
The use of MRA is appropriate in patients with documented allergy to iodinated contrast material and in patients who have accelerating hypertension or accelerating renal insufficiency.
MRA exclusions:
Medical literature doesn’t support the use of magnetic resonance angiography for the following conditions:
- Screening of the general population for intracranial aneurysms
- Ruling out intracranial aneurysms in patients who have vague CNS symptoms (e.g., non-specific sensory loss, dizziness, vertigo or headache)
- Evaluating patients with symptoms suggestive of dural, sagittal or cavernous sinus thrombosis/occlusion
- Screening for reno-vascular hypertension
- For the evaluation of accessory renal arteries in prospective renal donors, including potential living kidney donors
MRV inclusions:
MRV is appropriate for any of the following conditions:
- For evaluation of thrombosis or compression by tumor of the cerebral venous sinus in patients who are at risk (e.g., otitis media, meningitis, sinusitis, oral contraceptive use, underlying malignant process, hypercoagulable disorders) or have signs or symptoms (e.g., papilledema, focal motor or sensory deficits, seizures, or drowsiness and confusion accompanying a headache).
- For evaluation of venous thrombosis or occlusion in the large systemic veins (e.g., superior vena cava, subclavian, or other deep veins in the chest).
- For evaluation of venous thrombosis or occlusion in the portal and/or hepatic venous system (e.g., Budd-Chiari syndrome).
|
81099, 84999, 83520, 86849 |
Basic benefit and medical policy
Evaluation of biomarkers for Alzheimer’s
Cerebrospinal fluid biomarker testing including, but not limited to, amyloid beta peptides, tau protein or neural thread proteins as an adjunct to clinical diagnosis in individuals with mild cognitive impairment is considered experimental.
Cerebrospinal fluid biomarker testing including, but not limited to, amyloid beta peptides, tau protein or neural thread proteins, as an adjunct to clinical diagnosis in individuals with mild dementia due to Alzheimer’s disease is considered experimental.
Cerebrospinal fluid biomarker testing including, but not limited to, amyloid beta peptides, tau protein or neural thread proteins, as part of an evaluation for the initiation of amyloid beta targeting therapy in individuals with mild cognitive impairment or mild dementia due to Alzheimer’s disease is considered experimental.
Cerebrospinal fluid biomarker testing including, but not limited to, amyloid beta peptides, tau protein or neural thread proteins, as part of an evaluation for the continuation of amyloid beta targeting therapy in individuals with mild cognitive impairment or mild dementia due to Alzheimer’s disease is considered experimental.
Measurement of urinary and blood biomarkers as an adjunct to clinical diagnosis in individuals with mild cognitive impairment or mild dementia due to Alzheimer’s disease is considered experimental. There is insufficient evidence in medical literature to determine the effect of this testing on patient clinical outcomes.
The medical policy statement has been updated, effective May 1, 2023.
Inclusionary and exclusionary guidelines:
Not applicable |
Established
81120, 81121, 81287 |
Basic benefit and medical policy
Genetic testing: Analysis of MGMT in malignant gliomas
The safety and effectiveness of the analysis of MGMT promoter methylation and IDH1/IDH2 mutation testing in malignant gliomas are established. It may be considered a useful option when indicated.
The medical policy statement, as well as inclusionary and exclusionary criteria, have been updated, effective May 1, 2023.
Inclusions:
Methylation analysis of the O6-methylguanine DNA methyltransferase, or MGMT, gene promoter from glioma tumor tissue is established for individuals who meet all the following criteria:
- They have a tumor type consistent with high-grade malignant glioma (e.g., glioblastoma multiforme, anaplastic astrocytoma).
- Candidate for temozolomide therapy or radiation therapy.
- Methylation results will be used to direct their therapy choices.
IDH1/IDH2
IDH mutation testing is required in the workup of all gliomas.
Exclusions:
MGMT promoter methylation analysis and IDH1/IDH2 testing are experimental in situations that don’t meet the above criteria. |
81306, 81335, 81401, 82657, 80299,** 0034U, 0169U
**Unlisted procedure code |
Basic benefit and medical policy
Pharmacogenomic and metabolite markers for treatment with thiopurines
The safety and effectiveness of one-time genotypic or phenotypic analysis of the enzyme TMPT and Nudix hydrolase, or NUDT15, have been established. It may be considered a useful tool to guide therapy in specified situations.
Monitoring of thiopurine metabolite levels in individuals with inflammatory bowel disease and acute lymphoblastic leukemia has been established. It may be considered a useful tool in specific situations.
Analysis of the metabolite markers of azathioprine, or AZA, and mercaptopurine, or 6-MP, including 6-methyl-mercaptopurine ribonucleotides, or 6-MMRP, and 6-thioguanine nucleotides, or 6-TGN, in all other conditions not listed below, is considered experimental.
The medical policy statement and inclusionary criteria have been updated, effective May 1, 2023.
Inclusions:
One-time genotypic or phenotypic analysis of the enzyme TMPT/NUDT15 may be considered established in one of the following situations:
- In patients beginning therapy with azathioprine, mercaptopurine or thioguanine
- In patients on thiopurine therapy with abnormal complete blood count results that don’t respond to dose reduction
Monitoring of thiopurine metabolite levels in individuals with inflammatory bowel disease may be considered established for the following indications:
- To measure blood levels in individuals suspected of having toxic responses to AZA or 6-MP (e.g., hepatotoxicity or myelotoxicity)
- To measure drug levels in individuals who have not responded to therapy (e.g., persistent fever, further weight loss and bloody diarrhea)
Monitoring of thiopurine metabolite levels in individuals with acute lymphoblastic leukemia may be considered established in the following situations:
- For patients showing signs of a lack of myelosuppression while on therapy
- For patients with normal function for TPMT and NUDT15 who don’t appear to tolerate thiopurines
Exclusions:
Analysis of the metabolite markers of azathioprine and mercaptopurine, including 6-methyl-mercaptopurine ribonucleotides and 6-thioguanine nucleotides in all other conditions. |
81450, 81455, 0017U, 81219, 81270,
81279, 81338, 81339 |
Basic benefit and medical policy
JAK2, MPL and CALR genetic testing for myeloproliferative neoplasms
The safety and effectiveness of JAK2 testing have been established. It may be considered a useful diagnostic option for patients presenting with clinical, laboratory or pathologic findings suggesting polycythemia vera, essential thrombocythemia or primary myelofibrosis.
The safety and effectiveness of MPL and CALR testing have been established. They may be considered useful diagnostic options for patients presenting with clinical, laboratory or pathologic findings suggesting essential thrombocythemia or primary myelofibrosis.
The use of a genomic panel for hematolymphoid neoplasms may be considered appropriate for the diagnosis and for selecting the therapy of a myeloproliferative disorder or myelodysplastic syndrome.
The peer-reviewed medical literature hasn’t yet demonstrated the clinical utility for JAK2, MPL and CALR testing in other circumstances. Therefore, these services are considered experimental.
Inclusionary and exclusionary criteria have been updated, resulting in updated payable diagnoses for procedures *81450 and *81455. The change is effective March 1, 2023.
*81450: Payable for C92.10, C92.11, C92.12, C93.90-
C93.92, C94.6, C96.20- C96.22, C96.29, D45, D46.9,
D47.1, D47.3, D47.4, D75.81
*81455: Added D45, D46.9, D47.1, D47.3, D47.4, D75.81
Inclusions:
JAK2 testing as a diagnostic option for patients presenting with clinical, laboratory or pathologic findings suggesting polycythemia vera, essential thrombocythemia or primary myelofibrosis.
MPL and CALR testing as diagnostic options for patients presenting with clinical, laboratory or pathologic findings suggesting essential thrombocythemia or primary myelofibrosis.
The use of a genomic panel for hematolymphoid neoplasms may be considered appropriate for the diagnosis and for selecting the therapy of a myeloproliferative disorder or myelodysplastic syndrome.
Exclusions:
JAK2, MPL and CALR testing in other circumstances including, but not limited to, the following:
- Diagnosis of nonclassic forms of myeloproliferative neoplasms, or MPNs
- Molecular phenotyping of patients with MPNs
|
90715 |
Basic benefit and medical policy
Adacel (tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine adsorbed)
Effective Jan. 20, 2023, Adacel (tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine adsorbed) is covered for the following FDA-approved indications:
Adacel is a vaccine indicated for:
- Immunization during the third trimester of pregnancy to prevent pertussis in infants younger than 2 months.
Dosage and administration:
For intramuscular injection only.
To provide protection against pertussis in infants younger than 2 months of age, administer Adacel during the third trimester of pregnancy. |
90867, 90868, 90869 |
Basic benefit and medical policy
Transcranial magnetic stimulation
Transcranial magnetic stimulation of the brain has been established. It may be a useful treatment option in certain specified situations.
Inclusionary criteria have been updated, effective May 1, 2023.
Inclusions:
Transcranial magnetic stimulation therapy should be ordered by a board-certified psychiatrist upon completion of a comprehensive evaluation.
Major depressive disorder
Transcranial magnetic stimulation must be administered by an approved U.S. Food and Drug Administration-cleared device for the treatment of major depressive disorder, or MDD, and modalities may include conventional TMS, deep TMS and theta burst stimulation. Specified stimulation parameters as follows: five days a week for six weeks (total of 30 sessions), however, the treatment plan can be individualized depending on the type of device used, safety and side effect considerations and response to treatment.
Must meet all:
- The member is 18 to 70 years of age.
- A drug screen is obtained if indicated by history, current clinical evaluation or a high degree of clinical suspicion.
- A confirmed diagnosis of severe major depressive disorder (single or recurrent episode) measured by evidence-based scales such as Beck Depression Inventory (score 30-63), Zung Self-Rating Depression Scale (>70), PHQ-9 (>20), Hamilton Depression Rating Scale (>20), or Montgomery-Asberg Depression Rating Scale (MADRS) (score >34).
- At least one of the following:
- The individual has tried and had an inadequate response to two antidepressant agents from two different antidepressant classes (e.g., selective serotonin reuptake inhibitors, serotonin and norepinephrine reuptake inhibitors, tricyclic antidepressants, bupropion or mirtazapine). An adequate trial of an antidepressant is defined by both of the following:
- The trial length was at least six weeks at generally accepted doses or of sufficient duration as determined by the treating physician at the generally accepted doses.
- Individual was ≥ 80% adherent to the agent during the trial.
- The individual is unable to tolerate a therapeutic dose of medications. Intolerance is defined as severe somatic or psychological symptoms that can’t be modulated by any means including, but not limited to, additional medications to ameliorate side effects. Examples of somatic side effects: persistent electrolyte imbalance, pancytopenia, severe weight loss, poorly controlled metabolic syndrome or diabetes. Examples of psychological side effects: suicidal-homicidal thinking/attempts, impulse dyscontrol.
Note: A trial of less than one week of a medication isn’t considered a qualifying trial to establish intolerance.
- The individual has a history of response to TMS in a previous depressive episode (and it has been at least three months since the prior episode)
- The individual is a candidate for electroconvulsive therapy; further, electroconvulsive therapy wouldn’t be clinically superior to transcranial magnetic stimulation. For example, in cases with psychosis, acute suicidal risk, catatonia or life-threatening inanition, TMS should not be utilized).
- The individual failed a trial of an evidence-based psychotherapy known to be effective in the treatment of MDD of an adequate frequency and duration without significant improvement in depressive symptoms as documented by standardized rating scales that reliably measure depressive symptoms (e.g., Becks Depression Inventory, Zung Self-Rating Depression Scale, PHQ-9, Hamilton Depression Rating Scale or MADRS).
Obsessive-compulsive disorder
Individual consideration may be extended to patients based on review of applicable medical records for refractory OCD defined as two therapeutic trials of medications and psychotherapy with one augmentation episode that has failed.
Conditions that must be met during the entire TMS treatment:
- The treatment must be administered by a board-certified psychiatrist trained in TMS therapy or a trained technician, under the supervision of a board-certified psychiatrist trained in TMS therapy.
- An attendant trained in BCLS, the management of complications (such as seizures), and the use of appropriate equipment, must be present.
- Adequate resuscitation equipment must be available (e.g., suction and oxygen).
- The facility must maintain awareness of response times of emergency services (either fire/ambulance or “code team”), which should be available within five minutes. These relationships are reviewed at least once per year and include mock drills.
Exclusions:
- All other behavioral health, neuropsychiatric or medical conditions (e.g., anxiety disorders, mood disorders, schizophrenia, Alzheimer’s, dysphagia, seizures, migraine headaches, etc.)
- Pregnancy
- Maintenance treatment
- Presence of psychosis in the current episode
- Seizure disorder or any history of seizure, except those induced by ECT or isolated febrile seizures in infancy without subsequent treatment or recurrence
- Presence of an implanted magnetic-sensitive medical device located less than or equal to 30 centimeters from the TMS magnetic coil or other implanted metal items including, but not limited to, a cochlear implant, implanted cardioverter defibrillator, pacemaker, vagus nerve stimulator, or metal aneurysm clips or coils, staples, or stents
Note: Dental amalgam fillings aren’t affected by the magnetic field and are acceptable for use with TMS.
- If the patient (or, when indicated, the legal guardian) is unable to understand the risk and benefits of TMS and provide informed consent
- Presence of a medical or co-morbid psychiatric contraindication to TMS
- Patient lacks a suitable environmental, or social or professional support system for post-treatment recovery
- There isn’t a reasonable expectation that the patient will be able to adhere to post-procedure recommendations
Note: Caution should be exercised in any situation where the patient’s seizure threshold may be decreased. Examples include:
- Presence in the bloodstream of a variety of agents including, but not limited to, tricyclic antidepressants, clozapine, antivirals, theophylline, amphetamines, PCP, MDMA, alcohol and cocaine as these present a significant risk
- Presence of the following agents including, but not limited to, SSRIs, SNRIs, bupropion, some antipsychotics, chloroquine, some antibiotics and some chemotherapeutic agents as they present a relative risk and should be considered when making risk-benefit assessments
- Withdrawal from alcohol, benzodiazepines, barbiturates and chloral hydrate also present a strong relative hazard
|
B4105 |
Basic benefit and medical policy
Relizorb
The policy has been updated to cover procedure code B4105 when criteria are met, effective March 1, 2023.
The safety and efficacy of FDA-approved digestive enzyme cartridges (e.g., Relizorb™) have been established. They may be considered a useful therapeutic option for patients who meet specific selection criteria.
Inclusions:
Digestive enzyme cartridges (e.g., Relizorb™) when all the following are met:
- Pediatric or adult age 5 and older
- Criteria for enteral nutrition has been met
- Used with enteral tube feeding for the treatment of pancreatic insufficiency due to cystic fibrosis
- There is documented failure of pancreatic enzyme replacement therapy (e.g., malnutrition, poor growth [pediatric], bloating, cramping, gassiness, diarrhea, fatty stools, nausea, vomiting constipation, abdominal discomfort).
- Failure to achieve or maintain target body mass index
- Overnight enteral feeding with lipase delivery throughout the feeding is required to meet caloric and nutritional demands.
Exclusions:
- Use of in-line digestive enzymes cartridges not meeting the criteria above
|
E1399**
**Unlisted code |
Basic benefit and medical policy
Digital health therapies: Diagnostic
Prescription digital health technologies for diagnostic application that have received clearance for marketing by the U.S. Food and Drug Administration as a diagnostic aid for autism spectrum disorder (Canvas Dx) are considered experimental, effective May 1, 2023.
Inclusionary and exclusionary guidelines:
Not applicable |
J0248 |
Basic benefit and medical policy
Veklury (remdesivir)
Effective Dec. 15, 2022, the FDA has updated the indications for Veklury (remdesivir). The following usage is no longer indicated in the drug’s description:
- With positive results of direct SARS-CoV-2 viral testing
|
J3490
J3590 |
Basic benefit and medical policy
Altuviiio (antihemophilic factor [recombinant], Fc-VWF-XTEN fusion protein-ehtl)
Altuviiio (antihemophilic factor [recombinant], Fc-VWF-XTEN fusion protein-ehtl) is considered established, effective Feb. 23, 2023.
Altuviiio (antihemophilic factor [recombinant], Fc-VWF-XTEN fusion protein-ehtl) is a recombinant DNA-derived, Factor VIII concentrate indicated for use in adults and children with hemophilia A (congenital factor VIII deficiency) for:
- Routine prophylaxis to reduce the frequency of bleeding episodes
- On-demand treatment and control of bleeding episodes
- Perioperative management of bleeding
Limitation of use:
Altuviiio isn’t indicated for the treatment of von Willebrand disease.
Dosage forms and strengths:
For intravenous use only.
- Each Altuviiio vial label states Factor VIII activity in international units (IU or unit)
- For routine prophylaxis: 50 IU/kg once weekly.
- For on-demand treatment and control of bleeding episodes and perioperative management: 50 IU/kg
Estimated Increment of Factor VIII (IU/dL or % of normal) = 50 IU/kg x 2 (IU/dL per IU/kg.)
To achieve a specific target Factor VIII activity level, use the following formula: Dosage (IU) = Body Weight (kg) x Desired Factor VIII Increase (IU/dL or % normal) x 0.5 (IU/kg per IU/dL).
Dosage forms and strengths:
For injection: Nominally 250, 500, 750, 1000, 2000, 3000 or 4000 IU, lyophilized powder in single-dose vials for reconstitution.
This drug isn’t a benefit for URMBT. |
J3490
J3590 |
Basic benefit and medical policy
Prevduo (neostigmine methylsulfate and glycopyrrolate)
Prevduo (neostigmine methylsulfate and glycopyrrolate) is considered established effective, Feb. 23, 2023.
Prevduo, a fixed-dose combination of a cholinesterase inhibitor and antimuscarinic agent, is indicated in patients ages 2 years and older for the reversal of the effects of non-depolarizing neuromuscular blocking agents, or NMBAs, after surgery, while decreasing the peripheral muscarinic effects (e.g., bradycardia and excessive secretions) associated with cholinesterase inhibition following NMBA reversal administration.
Dosage and administration:
- Should be administered by trained health care providers
- Peripheral nerve stimulator and monitoring for twitch responses should be used to determine when Prevduo should be initiated and if additional doses are needed
- For reversal of NMBAs with shorter half-lives in patients ages 2 years and older, when first twitch response is substantially greater than 10% of baseline, or when a second twitch is present: 0.03 mg/kg of neostigmine methylsulfate (0.006 mg/kg of glycopyrrolate) by intravenous route
- For reversal of NMBAs with longer half-lives or when first twitch response is close to 10% of baseline in patients ages 2 years and older: 0.07 mg/kg of neostigmine methylsulfate (0.014 mg/kg of glycopyrrolate) by intravenous route
- Maximum total dosage is 0.07 mg/kg of neostigmine methylsulfate or up to a total of 5 mg neostigmine methylsulfate (whichever is less)
Dosage forms and strengths:
Injection: Clear, colorless solution available as 3 mg/3 mL of neostigmine methylsulfate and 0.6 mg/3 mL of glycopyrrolate (1 mg/mL of neostigmine methylsulfate and 0.2 mg/mL of glycopyrrolate) in a single-dose 3 mL prefilled syringe.
This drug isn’t a benefit for URMBT. |
J3490
J3590 |
Basic benefit and medical policy
Skysona (elivaldogene autotemcel)
Effective Sept. 16, 2022, Skysona (elivaldogene autotemcel) is covered for the following FDA-approved indications:
Skysona (elivaldogene autotemcel) is indicated to slow the progression of neurologic dysfunction in boys ages 4 to 17 with early, active cerebral adrenoleukodystrophy, or CALD. Early, active CALD refers to asymptomatic or mildly symptomatic (neurologic function score, NFS ≤ 1) boys who have gadolinium enhancement on brain magnetic resonance imaging and Loes scores of 0.5-9.
This indication is approved under accelerated approval based on 24-month Major Functional Disability-free survival. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trials.
Limitations of use:
- Skysona (elivaldogene autotemcel) doesn’t treat or prevent adrenal insufficiency.
- An immune response to Skysona (elivaldogene autotemcel) may cause rapid loss of efficacy of Skysona (elivaldogene autotemcel) in patients with full deletions of the human adenosine triphosphate binding cassette, sub family D, member 1 (ABCD1) gene.
- Skysona (elivaldogene autotemcel) hasn’t been studied in CALD secondary to head trauma.
- Given the risk of hematologic malignancy with Skysona (elivaldogene autotemcel), and unclear long-term durability of Skysona (elivaldogene autotemcel) and human adrenoleukodystrophy protein, or ALDP, expression, careful consideration should be given to the timing of treatment for each boy and treatment of boys with isolated pyramidal tract disease as clinical manifestations don’t usually occur until adulthood.
Dosage and administration:
For autologous use only. For intravenous use only.
- Patients must undergo hematopoietic stem cell, or HSC, mobilization and apheresis to obtain CD34+ cells for Skysona manufacturing.
- Dosing of Skysona is based on the number of CD34+ cells in the infusion bags per kg of body weight.
- The minimum recommended dose is 5.0 × 106 CD34+ cells/kg.
- Full myeloablative and lymphodepleting conditioning must be administered before infusion of Skysona.
- Verify the patient’s identity matches the unique patient identification information on the Skysona infusion bags prior to infusion.
- Don’t sample, alter or irradiate Skysona.
- Don’t use an in-line blood filter or an infusion pump.
Dosage forms and strengths:
Skysona is a cell suspension for intravenous infusion.
- A single dose of Skysona contains a minimum of 5.0 × 106 CD34+ cells/kg of body weight, suspended in a solution containing 5% dimethyl sulfoxide, or DMSO.
Skysona (elivaldogene autotemcel) isn’t a benefit for URMBT.
|
J9042 |
Basic benefit and medical policy
Adcetris (brentuximab vedotin)
The FDA has updated the approved indications for Adcetris (brentuximab vedotin), effective Nov. 10, 2022. The payable indications include the following:
- Pediatric patients age 2 and older with previously untreated high risk classical Hodgkin lymphoma, or cHL, in combination with doxorubicin, vincristine, etoposide, prednisone and cyclophosphamide
Dosage and administration:
The recommended dosage in combination with chemotherapy for pediatric patients 2 years and older with previously untreated high-risk cHL is 1.8 mg/kg up to a maximum of 180 mg every three weeks for a maximum of five doses. |
J9173 |
Basic benefit and medical policy
Imfinzi (durvalumab)
The FDA has updated the payable indications for Imfinzi (durvalumab), effective Nov. 10, 2022. The payable indications include the following:
- In combination with tremelimumab-actl, for the treatment of adult patients with unresectable hepatocellular carcinoma, or uHCC
- In combination with tremelimumab-actl and platinum-based chemotherapy, for the treatment of adult patients with metastatic non-small cell lung cancer, or NSCLC, with no sensitizing epidermal growth factor receptor, or EGFR, mutations or anaplastic lymphoma kinase, or ALK, genomic tumor aberrations
|
J9271 |
Basic benefit and medical policy
Keytruda (pembrolizumab)
Effective Jan. 26, 2023, Keytruda (pembrolizumab) is payable for the following usage related to small-cell lung cancer:
- As a single agent, for adjuvant treatment following resection and platinum-based chemotherapy for adult patients with stage IB (T2a ≥4 cm), II, or IIIA NSCLC.
|
S2202, 36465, 36466, 36470, 36471,
76942, 37799 |
Basic benefit and medical policy
Echosclerotherapy for varicose veins
The safety and effectiveness of echosclerotherapy for the treatment of the saphenous vein varicosities are established. It may be considered a useful therapeutic option in individuals for whom traditional sclerotherapy of saphenous vein varicosities would be indicated.
The policy inclusions were updated, effective May 1, 2023.
Inclusions:
Ultrasound guidance to the saphenous vein in individuals having sclerotherapy would be considered established.
Ultrasound guidance to symptomatic varicose tributaries in individuals having sclerotherapy would be considered established. |
| GROUP BENEFIT CHANGES |
Kellogg |
Effective July 30, 2023, Kellogg will become two entities:
Kellanova
Group numbers: 71425 (non-union) and 72212 (union)
WK Kellogg Co
Group numbers: 71847 (non-union) and 71846 (union)
Members will receive new ID cards in the mail. Kellanova members will keep the existing phone numbers while WK Kellogg members will receive updated phone numbers. Benefits and coverage will remain the same. |
None of the information included in this billing chart is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.

Blue Cross begins using Quartet to help connect members with behavioral health providers
Blue Cross Blue Shield of Michigan is now using Quartet, an independent company, to assist our members who are seeking outpatient care for mental health or substance use disorders. This service, which is available at no extra cost to eligible members, is especially useful for people who are having difficulty locating and obtaining timely care from a behavioral health specialist in their area.
Effective July 1, 2023, Quartet will begin referring eligible members seeking outpatient treatment to behavioral health providers registered on Quartet’s online platform, based on their clinical specialty and their availability.
Quartet’s services will be available to the following adult members (18 years of age or older) who reside in Michigan:
- Fully insured Blue Cross commercial members
- Fully insured Blue Care Network commercial members
- All BCN Advantage℠ members
- Select Medicare Plus Blue℠ members
Joining the Quartet online platform
Quartet began reaching out to Blue Cross and BCN participating behavioral health providers in April to assist them in joining the Quartet platform. Participation is voluntary, and providers are still welcome to sign up. Through Quartet, a behavioral health provider can receive referrals, accept new patients, track the patient’s progress and access clinical assessments and other resources.
“We hope our behavioral health providers are encouraged to join and will see the value in this tool for both practitioners and patients,” said Dr. Amy McKenzie, vice president, Clinical Partnerships, and associate chief medical officer for Blue Cross. “We know that some of our members struggle to find the behavioral health care they need, and our relationship with Quartet is designed to help meet their needs.”
For more information
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Quartet is an independent company contracted by Blue Cross Blue Shield of Michigan to provide behavioral health services for Blue Cross and BCN members.
Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal services.
We’ll use 2023 InterQual criteria, starting Aug. 1
Blue Cross Blue Shield of Michigan and Blue Care Network will start using 2023 InterQual® criteria to make determinations on prior authorization requests for the behavioral and nonbehavioral health services we manage, starting Aug. 1, 2023.
The information below applies to lines of business and members whose authorizations are managed by Blue Cross or BCN directly and not by independent companies that provide services to Blue Cross.
Nonbehavioral health services
We’ll use updated criteria for all levels of care to make determinations on prior authorization requests for nonbehavioral health services for the following members:
- Blue Cross commercial
- Medicare Plus Blue℠
- BCN commercial
- BCN Advantage℠
When clinical information is requested for a medical or surgical admission — or for other services — we require providers to submit specific components of the medical record that show that the request meets the criteria. We review this information when making determinations on prior authorization requests.
Blue Cross and BCN also use local rules, which are modifications of InterQual criteria, in making determinations. You can access these rules as follows:
Refer to the table below for more specific information about which criteria we use in making determinations for various types of nonbehavioral health prior authorization requests.
Starting Aug. 1, we’ll no longer use the condition-specific local rules for acute inpatient medical admissions.
|
Criteria |
Services |
InterQual acute — adult and pediatrics |
- Inpatient admissions
- Continued stay discharge readiness
|
InterQual level of care — subacute and skilled nursing facility |
- Subacute and skilled nursing facility admissions
- Continued stay discharge readiness
|
InterQual rehabilitation — adult and pediatrics |
- Inpatient admissions
- Continued stay and discharge readiness
|
InterQual level of care — long-term acute care |
- Long-term acute care facility admissions
- Continued stay discharge readiness
|
InterQual imaging |
- Imaging studies and X-rays
|
InterQual procedures — adult and pediatrics |
- Surgery and invasive procedures
|
Medicare coverage guidelines (as applicable) |
- Services that require clinical review for medical necessity and benefit determinations
|
Blue Cross and BCN medical policies |
- Services that require clinical review for medical necessity
|
Local rules for post-acute care (apply to inpatient rehabilitation, skilled nursing facility and long-term acute care admissions for Blue Cross commercial and BCN commercial) |
- Exceptions to the application of InterQual criteria that reflect the accepted practice standards for Blue Cross and BCN
|
Behavioral health services
On Aug. 1, 2023, we’ll begin using the 2023 InterQual criteria to make determinations on prior authorization requests for behavioral health services for these members:
- Medicare Plus Blue
- BCN commercial
- BCN Advantage
In addition, certain determinations will be based on modifications to InterQual criteria or on local rules or medical policies, as shown in the table below.
Products |
Modified InterQual criteria for: |
Local rules or medical policies for: |
BCN commercial and BCN Advantage |
- Mental health disorders: partial hospital program
- Residential mental health treatment (adult, geriatric, child and adolescent members)
Note: Neither BCN commercial members with BCN1, BCN5 and BCN10 plans nor BCN Advantage members have residential mental health treatment benefits. |
- Applied behavior analysis for autism spectrum disorder
- Neurofeedback for attention deficit disorder and attention deficit hyperactivity disorder
- Transcranial magnetic stimulation, or TMS
- Telemedicine (telepsychiatry and teletherapy)
|
Medicare Plus Blue |
- Mental health disorders: partial hospital program
|
- Telemedicine (telepsychiatry and teletherapy)
|
You can find links to the current modified behavioral health and autism local rules, as well as instructions for accessing the medical policies, on these webpages:
We’ll update these pages before Aug. 1 to reflect the criteria changes.
Note: Determinations on Blue Cross commercial behavioral health authorization requests are handled by New Directions Behavioral Health®. New Directions uses its own medical necessity criteria.
New Directions Behavioral Health is an independent company that manages authorizations for behavioral health and autism services for Blue Cross Blue Shield of Michigan members who have commercial plans.
Behavioral health providers: How to bill prolonged services
In January 2023, we posted a provider alert that asked behavioral health providers to hold claims for dates of service on or after Jan. 1, 2023, that contain procedure codes *99354 and *99355. These codes were for prolonged services and were terminated by the American Medical Association as of Jan. 1, 2023.
At that time, we indicated that we were working on identifying active codes to bill in place of the terminated codes.
What to do with claims you’ve been holding
- For Blue Cross Blue Shield of Michigan and Blue Care Network commercial members, use HCPCS code G2212 in place of procedure codes *99354 and *99355 for dates of service on or after Jan 1, 2023. The G2212 code can now be billed with procedure codes *90837 and *90847.
- For Medicare Plus Blue℠ and BCN Advantage℠ members, follow the Centers for Medicare & Medicaid Services billing guidelines.
Additional information and reminders
- HCPCS code G2212 is billed in increments of 15 minutes for each unit of prolonged service after the time of the base code is exhausted.
- You can submit claims with G2212 for dates of service as early as Jan. 1, 2023.
- Any claims for dates of service on or after Jan. 1, 2023, that contain codes *99354 and *99355 will be rejected, even if the claims also contain codes that are payable.
- Claims with dates of service prior to Jan. 1, 2023, can still be billed with procedure codes *99354 and *99355.
Starting in August, Blue Cross to provide behavioral health benefits for GM hourly employees with group number 83200
Effective Aug. 1, 2023, Blue Cross Blue Shield of Michigan will administer behavioral health and substance use disorder benefits to GM hourly employees under group number 83200. Carelon will no longer be the behavioral health and substance use disorder benefits provider for this group.
Members will receive new ID cards in the mail with updated phone numbers so they can contact Customer Service if they have questions. Benefits and coverage will remain the same. Nonparticipating providers aren’t covered.
On and after Aug. 1, 2023, contact Blue Cross if you have benefit and claims questions. You can also log in to Provider Secured Services to review benefits and submit claims. If you have questions, call Provider Relations and Servicing at the number on the back of the card or one of the following phone numbers:
- Physicians and other professional providers: 1-800-344-8525
- Hospital and facility providers: 1-800-249-5103
For processing or if you have questions about claims on or before July 31, 2023, call Carelon at 1-800-235-2302.
Reminder: Blue Cross now covers in-state mental health services provided by intensive outpatient programs
Effective July 1, 2023, Blue Cross Blue Shield of Michigan will cover in-state mental health services provided through an intensive outpatient program, or IOP, as announced in a May Record article. This coverage, an enhancement to Blue Cross’ behavioral health benefits, applies to our commercial members.
Coding
Outpatient psychiatric care providers should report intensive outpatient program services for mental health using an appropriate HCPCS procedure code:
- For IOP mental health services provided in an outpatient hospital setting: Revenue codes 0905 and 0906 must be reported with an appropriate mental health diagnosis and a valid CPT/HCPCS procedure code combination.
These revenue codes are being added to the “All-Other Remainder” category for fee-based reimbursement and will follow Participating Hospital Agreement guidelines.
- For IOP mental health services provided in an approved freestanding residential hospital or outpatient substance abuse facility: Revenue code 0905 (Psychiatric) should be billed with an appropriate mental health diagnosis.
Other information
- Reimbursement for these locations will be based on an established rate.
- Mental health services for IOP admissions don’t require preauthorization.
- Benefits may vary based on group specifics.
Reminder: Blue Cross now covers partial hospitalization program services for substance use disorders
Effective July 1, 2023, Blue Cross Blue Shield of Michigan will cover partial hospitalization program, or PHP, services for substance use disorders, as announced in a May Record article.
This is an enhancement to behavioral health benefits for our commercial members.
Coding
Outpatient psychiatric care providers should report partial hospitalization program services for substance use disorders using HCPCS code S0201.
A quantity of one unit per date of service will be allowed for members of Blue Cross fully insured and self-funded groups. Quantities greater than one will reject back to the psychiatric provider as “daily max met, provider liable.”
For PHP services for substance use disorders provided in an outpatient hospital setting, revenue code 0913 (partial hospitalization-intensive and more than four hours per day) should be reported with a substance use disorder diagnosis and a valid CPT/HCPCS procedure code combination.
About revenue code 0913
This code:
- Is considered fee-based reimbursement and processes under the “All-Other Remainder” category in the Participating Hospital Agreement.
- Is being added as payable when reported with a substance use disorder diagnosis in a freestanding residential substance abuse facility or outpatient substance abuse facility. Reimbursement in these locations will be based on an established rate.
Admission to a partial hospitalization program for substance use disorder will require preauthorization if the patient is admitted to a hospital or residential inpatient facility. Benefits may vary based on group specifics.
Starting Aug. 15, we’ll require prior authorization for some diabetes drugs
Beginning Aug. 15, 2023, health care providers for Blue Cross Blue Shield of Michigan and Blue Care Network commercial members will need to obtain prior authorization to show that the brand-name medications listed below are being used for Type 2 diabetes for us to pay for them. Medicare members are excluded from this change.
Brand-name medication |
FDA-approved indication |
Plan payment requirement |
Bydureon®
Byetta®
Mounjaro®
Ozempic®Rybelsus®
Trulicity®
Victoza® |
Type 2 diabetes |
Payment from Blue Cross or BCN will require one of the following:
- Being used for the treatment of Type 2 diabetes
- Trial of one generic or preferred medication for the treatment of Type 2 diabetes
|
Members should ask their prescribing doctor to contact us to request a prior authorization for the medications listed above. If the prescription isn’t authorized in advance, it may not be paid for.
We announced a similar change on Feb. 1, 2023, which didn’t apply to members who were already taking these medications. Effective Aug. 15, all members are required to have a prior authorization for these medications.
Providers can request prior authorization electronically. For information on how to submit the request:
- Go to ereferrals.bcbsm.com.
- Click on Blue Cross for commercial members or BCN for BCN members.
- Click on Pharmacy Benefit Drugs on the left.
For a complete list of drugs and associated requirements, go to bcbsm.com/druglists.
Elahere, Imjudo, Tecvayli and Lunsumio to require prior authorization for most members, starting Aug. 23
For dates of service on or after Aug. 23, 2023, the following drugs will require prior authorization through Carelon Medical Benefits Management (formerly known as AIM Specialty Health®) for most Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members:
- Elahere™ (mirvetuximab soravtansine-gynx), HCPCS code J9063
- Imjudo® (tremelimumab-actl), HCPCS code J9347
- Tecvayli™ (teclistamab-cqyv), HCPCS code J9380
- Lunsumio™ (mosunetuzumab-axgb), HCPCS code J9350
These drugs are covered under the members’ medical benefits, not their pharmacy benefits.
Prior authorization requirements apply when these drugs are administered in outpatient settings for:
- Blue Cross commercial
Note: This requirement doesn’t apply to members who have coverage through the Blue Cross and Blue Shield Federal Employee Program®.
- Medicare Plus Blue℠ members
- BCN commercial members
- BCN Advantage℠ members
How to submit authorization requests
Submit authorization requests to Carelon using one of the following methods:
- Through the Carelon ProviderPortal, which you can access by doing one of the following:
- Logging in to our provider portal at availity.com,** clicking on Payer Spaces and then clicking on the BCBSM and BCN logo. This takes you to the Blue Cross and BCN payer space where you’ll click on the Carelon ProviderPortal tile.
- Logging in directly to the Carelon ProviderPortal at providerportal.com.**
- Calling the Carelon Contact Center at 1-844-377-1278.
More about the authorization requirements
Authorization isn’t a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members.
For additional information on requirements related to drugs covered under the medical benefit, refer to the following drug lists:
- Blue Cross commercial and BCN commercial:
- URMBT members with Blue Cross non-Medicare plans:
- Medicare Plus Blue and BCN Advantage members:
We’ll update the pertinent drug lists to reflect the information in this message prior to the effective date.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services.
Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Clarification: Xgeva continues to require prior authorization through NovoLogix for most commercial members
Xgeva® (denosumab), HCPCS code J0897, continues to require prior authorization for most Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members. Providers should submit prior authorization requests for these members through the NovoLogix® online tool.
Note: On Dec. 6, 2022, we published a provider alert stating that Xgeva would no longer require prior authorization through Carelon Medical Benefits Management (formerly known as AIM Specialty Health®). That change applied only to Medicare Plus Blue℠ and BCN Advantage℠ members, starting Jan. 1, 2023.
How to submit prior authorization requests
Submit prior authorization requests through NovoLogix. It offers real-time status checks and immediate approvals for certain medications.
To access NovoLogix, log in to our provider portal at availity.com,** click on Payer Spaces in the menu bar and then click on the BCBSM and BCN logo. You’ll find links to the NovoLogix tools on the Applications tab.
Note: If you need to request access to our provider portal, see the Register for web tools webpage on bcbsm.com.
Some Blue Cross commercial groups aren’t subject to this requirement
For Blue Cross commercial groups, this prior authorization requirement applies only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list.
Note: Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don’t participate in the standard prior authorization program.
List of requirements
For a full list of requirements related to drugs covered under the medical benefit, see the Blue Cross and BCN utilization management medical drug list for Blue Cross commercial and BCN commercial members.
You can access this list and other information about requesting prior authorization on the following pages of the ereferrals.bcbsm.com website:
Authorization isn't a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services.
Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Carelon to expand existing prior authorization program, starting Sept. 1
For dates of service on or after Sept. 1, 2023, additional services will require prior authorization by Carelon Medical Benefits Management (formerly known as AIM Specialty Health®).
Carelon currently manages select services for Blue Cross Blue Shield of Michigan commercial, Blue Care Network commercial, Medical Plus Blue℠ and BCN Advantage℠ members.
Here’s a summary of the changes that will occur starting Sept. 1:
- For both Blue Cross and BCN commercial members, additional cardiology and advanced imaging services will require prior authorization.
- For Blue Cross commercial members, additional sleep study services will require prior authorization.
- For BCN commercial members, Carelon will start managing in-lab sleep studies.
By Aug. 14, the Carelon ProviderPortal® and the Carelon call center will be ready to accept prior authorization requests for these additional services.
These changes apply to:
- Most Blue Cross commercial members
- All BCN commercial members
For the services that Carelon already manages, you’ll continue to request prior authorization through the Carelon ProviderPortal.
Look for additional details about these changes in upcoming provider alerts and newsletter articles.
Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services.
We’ve made questionnaire changes in e-referral system
What you need to know
Several questionnaires in the e-referral system have been updated. Providers can preview questionnaires on ereferrals.bcbsm.com.
In May, we updated and removed questionnaires in the e-referral system, as well as the corresponding preview questionnaires on the ereferrals.bcbsm.com website.
We use our authorization criteria, our medical policies and your answers to the questionnaires in the e-referral system when making utilization management determinations on your authorization requests.
Updated questionnaires
We updated the following questionnaires on the dates specified below:
Questionnaire |
Opens for |
Updates |
Release date |
Abdominoplasty |
- BCN commercial
- BCN Advantage
|
Added a question |
May 14, 2023 |
Bone-anchored hearing aid |
- BCN commercial
- BCN Advantage
|
Updated several questions |
May 14, 2023 |
Excess skin removal |
- BCN commercial
- BCN Advantage
|
Updated several questions |
May 14, 2023 |
Experimental and investigational services |
- BCN commercial
- BCN Advantage
|
Opens for both pediatric and adult members |
May 14, 2023 |
Oral surgery |
- BCN commercial
- BCN Advantage
|
Updated a question |
May 14, 2023 |
In addition, we limited the number of units providers can request per procedure code to two for endovascular intervention. This change affects Medicare Plus Blue℠, BCN commercial and BCN Advantage℠ members.
Removed questionnaire
We removed the Cholecystectomy (laparoscopic) questionnaire for BCN commercial and BCN Advantage members. Plan notification will be required for procedure codes *47562, *47563 and *47564, but no clinical review will be performed.
Preview questionnaires
Preview questionnaires show the questions you’ll need to answer in the e-referral system so that you can prepare your answers ahead of time. To access them, go to ereferrals.bcbsm.com and:
Authorization criteria and medical policies
The Authorization Requirements & Criteria page explains how to access the pertinent authorization criteria and medical policies.
Forest Hills Pediatric Associates: Using PCMH and Collaborative Care to better serve patients
This is the fourth article in a series highlighting some top performers in the Patient-Centered Medical Home Designation Program.  Dr. Barbara Periard Asked how the Patient-Centered Medical Home program has helped to improve the value of health care delivered at the practice, Barbara Periard, M.D., was quick to reply: “PCMH provides structure to our processes. It helps us identify the metrics we need to push forward. It also helps us to explain to families and staff why we’re doing what we’re doing, to monitor progress and put a framework around the work we do.”
Dr. Periard is one of 12 physicians at Forest Hills Pediatric Associates, located in Grand Rapids. The practice also includes a care management team that helps patients and their families manage asthma, ADHD, mental health issues and other chronic or complex conditions. They hired a mental health care coordinator more than five years ago, long before they joined Blue Cross Blue Shield of Michigan’s Collaborative Care Designation Program, which was launched last year.
“Care management has changed the way we practice and has brought about increased provider and patient satisfaction,” Dr. Periard said. “For example, kids with special needs used to require a lot of prep time for providers prior to appointments, but now care managers take care of the family’s needs before and in between visits. Pediatricians now report that visits are pleasant instead of stressful, allowing them more time to spend with their patients.”
One of the first metrics the practice delved into was well-child visits. The practice had been using recall reminders, texts and email blasts but wanted to improve its metrics. They started out by opening up their schedule to the year ahead so that patients could schedule their next annual appointment before leaving the office.
The result? Within a few months, they reduced the number of “missed” visits from 20% to 12%. Now, one year later, it’s below 10%.
“This has helped us improve the care delivered and made us more efficient by freeing up phone lines,” Dr. Periard said. “The overall benefits far outweigh any effort put forth.”
Other areas of success include:
Portal usage — The practice now has at least 93% portal usage and is looking at ways to use the portal in the future for remote patient monitoring.
Building remodel — With the recent remodeling of the building, half of it now features spaces with negative airflow, which is where they treat all sick patients. The practice also downsized the waiting room to create newborn-specific rooms at the front of the building to avoid exposing them to germs.
Vaccine process — The practice has established a vaccine process in its office to better support patients and their families. On any given day, all vaccines, including COVID-19 vaccines, can be administered.
“The time we’ve spent outlining processes and training staff has really paid off,” Dr. Periard said. “We’ve been able to spread the PCMH work across all team members.”
To read more
To read about other practices that have been profiled as part of this series, check out the following articles:
Reminders: Our affiliation agreements and our concierge medicine policy
Health care providers must comply with their affiliation agreements. Blue Cross Blue Shield of Michigan affiliation agreements require providers to:
- Submit claims for covered services directly to Blue Cross.
- Accept our payment for covered services as payment in full.
- Only charge the member the applicable copay or deductible (or both) for the covered service.
- Avoid discriminating against members based on payment level, benefit or reimbursement policies.
Concierge medicine policy
In a concierge practice, patients pay membership fees to a health care provider or third-party vendor for enhanced services or amenities. As a benefit of paying this fee, members typically receive:
- Easy appointment access
- Extended office visits
- Enhanced email and telephone communication with doctors
- Care coordination (including referrals) between the concierge practice and specialists
- Wellness programs and plans, genetic and nutritional counseling, risk appraisals
Policy information
Blue Cross’ concierge medicine policy states:
“Health care practitioners who wish to use this model in their practice may not be eligible for any value-based reimbursement (VBR) opportunities through Blue Cross and Blue Care Network (BCN) programs such as, but not limited to, Physician Group Incentive Program-related VBR opportunities through the Patient-Centered Medical Home (PCMH) designation program or other programs.”
Also, providers must ensure that the requirements of the concierge model are permitted by their affiliation agreements with Blue Cross.
Providers may charge a concierge fee if:
- Blue Cross and BCN members aren’t required to pay the concierge fee to become or continue to be a patient in the practice.
- Blue Cross and BCN members aren’t required to pay the concierge fee to obtain access to the provider. Blue Cross members who don’t pay the concierge fee may not be restricted to access only to ancillary providers, such as physician assistants or nurse practitioners.
- The services or products being offered as part of the concierge fee aren’t considered “covered services” as defined under our affiliation agreements or the member’s benefit plan, or both. Because benefit structures vary significantly among our members, providers are expected to understand each member’s benefit structure to ensure that covered services aren’t included in the concierge fee.
- Blue Cross and BCN members who don’t pay the concierge fee continue to receive the same level of access and services as they previously received.
- Providers continue to meet Blue Cross and BCN performance standards regarding access and service.
- The concierge level of service is clearly over and above usual practice in Michigan. Complaints from members who experience a decline in service level may result in Blue Cross concluding that the practice is noncompliant with the nondiscrimination clause of our affiliation agreements.
Well-managed chronic conditions can help members avoid ER visits or hospital stays
This is part of an ongoing series of articles focusing on the tools and resources available to help FEP members manage their health.
When patients have access to resources and support to help manage a chronic condition, such as diabetes, hypertension or cardiovascular disease, the chances of an emergency room visit or inpatient hospital stay may be reduced.
Here are resources from the American Heart Association to help members manage a chronic condition:
The Blue Cross Coordinated Care℠ program is also available to provide education and support from a care manager to members with complex or chronic conditions. Blue Cross and Blue Shield Federal Employee Program® members can request enrollment by calling 1-800-775-2583.
Additional programs for FEP members include:
- Hypertension Management Program: Members with hypertension may receive a free blood pressure monitor every two years. If you have questions, call Customer Service at 1-800-482-3600.
- Diabetic Meter Program: Members with diabetes may obtain a free glucose meter kit every year. Members can call 1-855-582-2024 to order a free glucose meter kit.
For more information on support programs, incentives and benefits, providers and members can call Customer Service at 1-800-482-3600 or go online to fepblue.org.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Lunch and learn webinars for physicians and coders focus on risk adjustment, coding
As a reminder, we’re offering live, 30-minute educational webinars that provide updated information on documentation and coding for common challenging diagnoses. Webinars include an opportunity to ask questions.
Here’s our upcoming schedule and tentative topics for the webinars. Each session starts at noon Eastern time. Log in to the provider training website to register for sessions that work with your schedule.
Session date |
Topic |
July 19 |
Coding heart disease and vascular |
Aug. 16 |
Medical record documentation and coding MEAT |
Sept. 20 |
Coding tips for COPD and asthma |
Oct. 18 |
ICD-10-CM updates and changes for 2024 |
Nov. 15 |
Coding chronic kidney disease and rheumatoid arthritis |
Dec. 13 |
CPT coding scenarios for 2024 |
If you haven’t already registered for the provider training website, follow these steps:
- Click here to register.
- Complete the registration. We recommend using the same email you use to communicate with Blue Cross Blue Shield of Michigan for other needs. This will become your login ID.
Locating a session
Click here if you are already registered for the provider training website. On the provider training website, look in the Event Calendar or use the search feature using the keyword “lunch” to quickly locate all 2023 sessions.
See the screenshots below for more details. 
Previous sessions
You can also listen to previously recorded sessions. Check out the following:
Previous sessions
You can also listen to previously recorded sessions. Check out the following:
Date |
Topic |
April 26 |
HCC and risk adjustment coding scenarios |
May 17 |
Coding neoplasms |
June 21 |
Coding diabetes and hypertension |
For more information
If you have any questions about the sessions, contact April Boyce at aboyce@bcbsm.com. If you have questions regarding a session or website registration, email ProviderTraining@bcbsm.com.
New training guide for behavioral health providers posted on training site
Action item
Visit our provider training site regularly to find new resources on topics that are important to your role.
Provider Experience continues to offer training resources for health care providers and staff. Our on-demand courses are designed to help you work more efficiently with Blue Cross Blue Shield of Michigan and Blue Care Network.
We recently added the following guide:
- Provider training and resource guide for behavioral health providers. Providers new to our networks will find a list of training courses and reference documents that will help them as they begin working with Blue Cross and BCN. The guide covers such topics as getting enrolled in online tools, checking benefits and eligibility, and submitting prior authorization requests and claims. It's located in the provider training site’s Knowledge Center.
Check the dashboard on our provider training site regularly for announcements as we add more courses, including those with CME offerings. The dashboard was designed to enhance the training experience for health care providers and staff.
Access our training site
If you don’t already have access to our training site, you can request access by following these steps:
- Open the registration page.
- Complete the registration. We recommend using the same email you use to communicate with Blue Cross for provider-related needs. This will become your login ID.
- Follow the link to log in.
If you need help creating your login ID or navigating the site, contact ProviderTraining@bcbsm.com.
For additional training opportunities, see the article on upcoming lunch and learn webinars, also in this issue.
Reminder: Physical medicine treatment plans developed by chiropractors
Medical doctors (M.D.s and D.O.s) may be asked to agree to and sign a physical medicine treatment plan developed by chiropractors. The physical medicine treatment plan must be kept on file by the chiropractor.
Blue Cross Blue Shield of Michigan will pay for the first physical medicine service per patient, not per visit. A prescription isn’t required for a member to receive covered physical medicine services from a chiropractor.
Also, as a reminder, we no longer use the term “physical therapy” when referring to certain types of treatment provided by chiropractors. We use the term “physical medicine.” We’re currently in the process of updating benefit information on Availity and Benefit Explainer, as well as our certificates and riders, to reflect this verbiage change.
Note: No physician agreement or signature is required on a treatment plan for MESSA members.
For more details on chiropractic services, see the “Chiropractic Services” chapter of the Blue Cross Commercial Provider Manual.
We’ve updated and posted our 2023 HEDIS tip sheets
Our 2023 HEDIS® tip sheets were recently posted in the Clinical Quality section of Secure Provider Resources on our provider portal.
Each year, we update and post our HEDIS and Star measure tip sheets. The Star Measure Tips were posted earlier this year. Note: We made a recent change to the Statin Use in Persons with Diabetes (SUPD) Star tip sheet. You may want to check out the updated list of exclusions in that tip sheet.
Accessing the tip sheets
To access our HEDIS and Star tip sheets, follow these steps:
- Log in to our provider portal (availity.com).**
- Under Payer Spaces, click on the BCBSM and BCN logo.
- Click on Secure Provider Resources (Blue Cross and BCN) under the Resources tab.
- Under the Member Care tab, click on Clinical Quality Tip Sheets.
About our tip sheets
- HEDIS tip sheets are developed to assist health care providers and their staff in efforts to improve overall health care quality and prevent or control diseases and chronic conditions. HEDIS® is one of the most widely used performance improvement tools in the U.S.
- Star tip sheets highlight select measures in the Medicare Star Ratings program. Most of the measures featured in our Star tip sheets are also HEDIS measures.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
HEDIS®, which stands for Healthcare Effectiveness Data and Information Set, is a registered trademark of the National Committee for Quality Assurance, or NCQA.
We’ve updated medical record documentation guidelines for musculoskeletal procedures
In February 2023, Blue Cross Blue Shield of Michigan, Blue Care Network and TurningPoint Healthcare Solutions LLC updated the guidelines for medical record documentation for musculoskeletal procedures as follows:
See the updated requirements document titled GN-1002 Medical Record Documentation.** It’s available on the Musculoskeletal Services pages of our ereferrals.bcbsm.com website.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own this document and aren’t responsible for its content.
TurningPoint Healthcare Solutions LLC is an independent company that manages authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
We’ve made updates to list of musculoskeletal procedure codes that require prior authorization
We recently updated the Musculoskeletal procedure codes that require authorization by TurningPoint document to reflect the following changes:
- For dates of service on or after March 19, 2023, procedure code *64625 is no longer payable for Medicare Plus Blue℠ or BCN Advantage℠ members.
Note: This procedure code continues to be payable for Blue Cross Blue Shield of Michigan and Blue Care Network commercial members. It requires prior authorization for BCN commercial members. It doesn’t require prior authorization for Blue Cross commercial members.
- For dates of service on or after March 25, 2023, procedure code C1767 doesn’t require prior authorization for Medicare Plus Blue, BCN commercial or BCN Advantage members.
Note: This procedure code has never required prior authorization for Blue Cross commercial members.
- For dates of service on or after July 1, 2023, procedure code *0775T will require authorization for Blue Cross commercial, Medicare Plus Blue, BCN commercial and BCN Advantage members.
For more information about TurningPoint’s musculoskeletal surgical quality and safety management program, see the following pages on the ereferrals.bcbsm.com website:
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.

We’ll use 2023 InterQual criteria, starting Aug. 1
Blue Cross Blue Shield of Michigan and Blue Care Network will start using 2023 InterQual® criteria to make determinations on prior authorization requests for the behavioral and nonbehavioral health services we manage, starting Aug. 1, 2023.
The information below applies to lines of business and members whose authorizations are managed by Blue Cross or BCN directly and not by independent companies that provide services to Blue Cross.
Nonbehavioral health services
We’ll use updated criteria for all levels of care to make determinations on prior authorization requests for nonbehavioral health services for the following members:
- Blue Cross commercial
- Medicare Plus Blue℠
- BCN commercial
- BCN Advantage℠
When clinical information is requested for a medical or surgical admission — or for other services — we require providers to submit specific components of the medical record that show that the request meets the criteria. We review this information when making determinations on prior authorization requests.
Blue Cross and BCN also use local rules, which are modifications of InterQual criteria, in making determinations. You can access these rules as follows:
Refer to the table below for more specific information about which criteria we use in making determinations for various types of nonbehavioral health prior authorization requests.
Starting Aug. 1, we’ll no longer use the condition-specific local rules for acute inpatient medical admissions.
|
Criteria |
Services |
InterQual acute — adult and pediatrics |
- Inpatient admissions
- Continued stay discharge readiness
|
InterQual level of care — subacute and skilled nursing facility |
- Subacute and skilled nursing facility admissions
- Continued stay discharge readiness
|
InterQual rehabilitation — adult and pediatrics |
- Inpatient admissions
- Continued stay and discharge readiness
|
InterQual level of care — long-term acute care |
- Long-term acute care facility admissions
- Continued stay discharge readiness
|
InterQual imaging |
- Imaging studies and X-rays
|
InterQual procedures — adult and pediatrics |
- Surgery and invasive procedures
|
Medicare coverage guidelines (as applicable) |
- Services that require clinical review for medical necessity and benefit determinations
|
Blue Cross and BCN medical policies |
- Services that require clinical review for medical necessity
|
Local rules for post-acute care (apply to inpatient rehabilitation, skilled nursing facility and long-term acute care admissions for Blue Cross commercial and BCN commercial) |
- Exceptions to the application of InterQual criteria that reflect the accepted practice standards for Blue Cross and BCN
|
Behavioral health services
On Aug. 1, 2023, we’ll begin using the 2023 InterQual criteria to make determinations on prior authorization requests for behavioral health services for these members:
- Medicare Plus Blue
- BCN commercial
- BCN Advantage
In addition, certain determinations will be based on modifications to InterQual criteria or on local rules or medical policies, as shown in the table below.
Products |
Modified InterQual criteria for: |
Local rules or medical policies for: |
BCN commercial and BCN Advantage |
- Mental health disorders: partial hospital program
- Residential mental health treatment (adult, geriatric, child and adolescent members)
Note: Neither BCN commercial members with BCN1, BCN5 and BCN10 plans nor BCN Advantage members have residential mental health treatment benefits. |
- Applied behavior analysis for autism spectrum disorder
- Neurofeedback for attention deficit disorder and attention deficit hyperactivity disorder
- Transcranial magnetic stimulation, or TMS
- Telemedicine (telepsychiatry and teletherapy)
|
Medicare Plus Blue |
- Mental health disorders: partial hospital program
|
- Telemedicine (telepsychiatry and teletherapy)
|
You can find links to the current modified behavioral health and autism local rules, as well as instructions for accessing the medical policies, on these webpages:
We’ll update these pages before Aug. 1 to reflect the criteria changes.
Note: Determinations on Blue Cross commercial behavioral health authorization requests are handled by New Directions Behavioral Health®. New Directions uses its own medical necessity criteria.
New Directions Behavioral Health is an independent company that manages authorizations for behavioral health and autism services for Blue Cross Blue Shield of Michigan members who have commercial plans.
What you need to know about the new prepayment DRG review process and how to provide input
Blue Cross Blue Shield of Michigan is proposing the implementation of a new prepayment DRG review process that will reduce the number of retrospective audit reviews. Program implementation is scheduled for Jan. 1, 2024, for Blue Cross commercial and will include in-state and host claims.
Both DRG coding and clinical validation will be included in this process. To ensure claims are being billed correctly and are supported by medical documentation, we’ll be looking for the following items:
- Reported discharge status
- Diagnosis
- Present on admission indicators
- Surgical procedure codes
- Clinically valid and properly documented diagnoses
- Coding guideline compliant
This isn’t a medical necessity review. To support payment accuracy and encourage correct coding, Blue Cross is working with Optum to identify claims that may require additional review. Optum is an independent company that contracts with Blue Cross to assist with claims processing.
What this means to facilities
Performance will be monitored and adjusted either up or down based on each facility’s results. For example, fewer claims will be reviewed for facilities with minimal findings.
This process is expected to lead to:
- More accurate initial payments; elimination of claim adjustments and reduction in refund requests
- Educational opportunities for billing and claims staff
- Elimination of the need to find old medical records documentation
- Ability to review the case more quickly
Current DRG review process |
Proposed pre-payment DRG review process |
- Retrospective audit takes place after a claim has been paid.
- Medical records are requested by mail, allowing a total of 90 days to submit.
- If there are findings, Blue Cross adjusts the claim.
- If there are no findings, the claim will remain as reimbursed.
- Two-step appeal process:
- Level 1: Appeal within 50 days with Change HealthCare EquiClaim
- Level 2: Appeal within 20 days with the Physicians Review Organization
|
- Pre-payment complex analytic review prior to claim payment.
- Claim would pend for review.
- Medical records would be requested by mail, allowing a total of 60 days to submit
- If not received within 60 days, the claim will deny.
- Records can be submitted within 180 days from the initial request for review.
- If there are no findings, the claim will be released for payment.
- If there are findings, the claim will be denied.
- Facility would rebill the claim with adjustments or appeal if they disagree with findings.
- Two-step appeal process:
- Level 1: Reconsideration within 180 days from the initial closure date with Optum
- Level 2: Appeal within 60 days from the reconsideration closure date with Optum
|
Input requested
As per the Contract Administration Process — part of the Participating Hospital Agreement that went into effect July 1, 2021 — we allow non-binding input from participating facilities about such proposals.
Input from facilities is requested by July 31, 2023. Send any input you may have to Erin Redman at ERedman@bcbsm.com.
After input is received, Blue Cross has 30 calendar days to respond to input.
Behavioral health providers: How to bill prolonged services
In January 2023, we posted a provider alert that asked behavioral health providers to hold claims for dates of service on or after Jan. 1, 2023, that contain procedure codes *99354 and *99355. These codes were for prolonged services and were terminated by the American Medical Association as of Jan. 1, 2023.
At that time, we indicated that we were working on identifying active codes to bill in place of the terminated codes.
What to do with claims you’ve been holding
- For Blue Cross Blue Shield of Michigan and Blue Care Network commercial members, use HCPCS code G2212 in place of procedure codes *99354 and *99355 for dates of service on or after Jan 1, 2023. The G2212 code can now be billed with procedure codes *90837 and *90847.
- For Medicare Plus Blue℠ and BCN Advantage℠ members, follow the Centers for Medicare & Medicaid Services billing guidelines.
Additional information and reminders
- HCPCS code G2212 is billed in increments of 15 minutes for each unit of prolonged service after the time of the base code is exhausted.
- You can submit claims with G2212 for dates of service as early as Jan. 1, 2023.
- Any claims for dates of service on or after Jan. 1, 2023, that contain codes *99354 and *99355 will be rejected, even if the claims also contain codes that are payable.
- Claims with dates of service prior to Jan. 1, 2023, can still be billed with procedure codes *99354 and *99355.
Reminder: Blue Cross now covers in-state mental health services provided by intensive outpatient programs
Effective July 1, 2023, Blue Cross Blue Shield of Michigan will cover in-state mental health services provided through an intensive outpatient program, or IOP, as announced in a May Record article. This coverage, an enhancement to Blue Cross’ behavioral health benefits, applies to our commercial members.
Coding
Outpatient psychiatric care providers should report intensive outpatient program services for mental health using an appropriate HCPCS procedure code:
- For IOP mental health services provided in an outpatient hospital setting: Revenue codes 0905 and 0906 must be reported with an appropriate mental health diagnosis and a valid CPT/HCPCS procedure code combination.
These revenue codes are being added to the “All-Other Remainder” category for fee-based reimbursement and will follow Participating Hospital Agreement guidelines.
- For IOP mental health services provided in an approved freestanding residential hospital or outpatient substance abuse facility: Revenue code 0905 (Psychiatric) should be billed with an appropriate mental health diagnosis.
Other information
- Reimbursement for these locations will be based on an established rate.
- Mental health services for IOP admissions don’t require preauthorization.
- Benefits may vary based on group specifics.
Reminder: Blue Cross now covers partial hospitalization program services for substance use disorders
Effective July 1, 2023, Blue Cross Blue Shield of Michigan will cover partial hospitalization program, or PHP, services for substance use disorders, as announced in a May Record article.
This is an enhancement to behavioral health benefits for our commercial members.
Coding
Outpatient psychiatric care providers should report partial hospitalization program services for substance use disorders using HCPCS code S0201.
A quantity of one unit per date of service will be allowed for members of Blue Cross fully insured and self-funded groups. Quantities greater than one will reject back to the psychiatric provider as “daily max met, provider liable.”
For PHP services for substance use disorders provided in an outpatient hospital setting, revenue code 0913 (partial hospitalization-intensive and more than four hours per day) should be reported with a substance use disorder diagnosis and a valid CPT/HCPCS procedure code combination.
About revenue code 0913
This code:
- Is considered fee-based reimbursement and processes under the “All-Other Remainder” category in the Participating Hospital Agreement.
- Is being added as payable when reported with a substance use disorder diagnosis in a freestanding residential substance abuse facility or outpatient substance abuse facility. Reimbursement in these locations will be based on an established rate.
Admission to a partial hospitalization program for substance use disorder will require preauthorization if the patient is admitted to a hospital or residential inpatient facility. Benefits may vary based on group specifics.
Starting Aug. 15, we’ll require prior authorization for some diabetes drugs
Beginning Aug. 15, 2023, health care providers for Blue Cross Blue Shield of Michigan and Blue Care Network commercial members will need to obtain prior authorization to show that the brand-name medications listed below are being used for Type 2 diabetes for us to pay for them. Medicare members are excluded from this change.
Brand-name medication |
FDA-approved indication |
Plan payment requirement |
Bydureon®
Byetta®
Mounjaro®
Ozempic®Rybelsus®
Trulicity®
Victoza® |
Type 2 diabetes |
Payment from Blue Cross or BCN will require one of the following:
- Being used for the treatment of Type 2 diabetes
- Trial of one generic or preferred medication for the treatment of Type 2 diabetes
|
Members should ask their prescribing doctor to contact us to request a prior authorization for the medications listed above. If the prescription isn’t authorized in advance, it may not be paid for.
We announced a similar change on Feb. 1, 2023, which didn’t apply to members who were already taking these medications. Effective Aug. 15, all members are required to have a prior authorization for these medications.
Providers can request prior authorization electronically. For information on how to submit the request:
- Go to ereferrals.bcbsm.com.
- Click on Blue Cross for commercial members or BCN for BCN members.
- Click on Pharmacy Benefit Drugs on the left.
For a complete list of drugs and associated requirements, go to bcbsm.com/druglists.
Elahere, Imjudo, Tecvayli and Lunsumio to require prior authorization for most members, starting Aug. 23
For dates of service on or after Aug. 23, 2023, the following drugs will require prior authorization through Carelon Medical Benefits Management (formerly known as AIM Specialty Health®) for most Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members:
- Elahere™ (mirvetuximab soravtansine-gynx), HCPCS code J9063
- Imjudo® (tremelimumab-actl), HCPCS code J9347
- Tecvayli™ (teclistamab-cqyv), HCPCS code J9380
- Lunsumio™ (mosunetuzumab-axgb), HCPCS code J9350
These drugs are covered under the members’ medical benefits, not their pharmacy benefits.
Prior authorization requirements apply when these drugs are administered in outpatient settings for:
- Blue Cross commercial
Note: This requirement doesn’t apply to members who have coverage through the Blue Cross and Blue Shield Federal Employee Program®.
- Medicare Plus Blue℠ members
- BCN commercial members
- BCN Advantage℠ members
How to submit authorization requests
Submit authorization requests to Carelon using one of the following methods:
- Through the Carelon ProviderPortal, which you can access by doing one of the following:
- Logging in to our provider portal at availity.com,** clicking on Payer Spaces and then clicking on the BCBSM and BCN logo. This takes you to the Blue Cross and BCN payer space where you’ll click on the Carelon ProviderPortal tile.
- Logging in directly to the Carelon ProviderPortal at providerportal.com.**
- Calling the Carelon Contact Center at 1-844-377-1278.
More about the authorization requirements
Authorization isn’t a guarantee of payment. As always, health care practitioners need to verify eligibility and benefits for members.
For additional information on requirements related to drugs covered under the medical benefit, refer to the following drug lists:
- Blue Cross commercial and BCN commercial:
- URMBT members with Blue Cross non-Medicare plans:
- Medicare Plus Blue and BCN Advantage members:
We’ll update the pertinent drug lists to reflect the information in this message prior to the effective date.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage authorizations for select services.
Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Clarification: Xgeva continues to require prior authorization through NovoLogix for most commercial members
Xgeva® (denosumab), HCPCS code J0897, continues to require prior authorization for most Blue Cross Blue Shield of Michigan and Blue Care Network group and individual commercial members. Providers should submit prior authorization requests for these members through the NovoLogix® online tool.
Note: On Dec. 6, 2022, we published a provider alert stating that Xgeva would no longer require prior authorization through Carelon Medical Benefits Management (formerly known as AIM Specialty Health®). That change applied only to Medicare Plus Blue℠ and BCN Advantage℠ members, starting Jan. 1, 2023.
How to submit prior authorization requests
Submit prior authorization requests through NovoLogix. It offers real-time status checks and immediate approvals for certain medications.
To access NovoLogix, log in to our provider portal at availity.com,** click on Payer Spaces in the menu bar and then click on the BCBSM and BCN logo. You’ll find links to the NovoLogix tools on the Applications tab.
Note: If you need to request access to our provider portal, see the Register for web tools webpage on bcbsm.com.
Some Blue Cross commercial groups aren’t subject to this requirement
For Blue Cross commercial groups, this prior authorization requirement applies only to groups that participate in the standard commercial Medical Drug Prior Authorization Program for drugs administered under the medical benefit. To determine whether a group participates in the prior authorization program, see the Specialty Pharmacy Prior Authorization Master Opt-in/out Group list.
Note: Blue Cross and Blue Shield Federal Employee Program® members and UAW Retiree Medical Benefits Trust (non-Medicare) members don’t participate in the standard prior authorization program.
List of requirements
For a full list of requirements related to drugs covered under the medical benefit, see the Blue Cross and BCN utilization management medical drug list for Blue Cross commercial and BCN commercial members.
You can access this list and other information about requesting prior authorization on the following pages of the ereferrals.bcbsm.com website:
Authorization isn't a guarantee of payment. Health care practitioners need to verify eligibility and benefits for members.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own or control this website.
Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services.
Availity® is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to offer provider portal and electronic data interchange services.
Carelon to expand existing prior authorization program, starting Sept. 1
For dates of service on or after Sept. 1, 2023, additional services will require prior authorization by Carelon Medical Benefits Management (formerly known as AIM Specialty Health®).
Carelon currently manages select services for Blue Cross Blue Shield of Michigan commercial, Blue Care Network commercial, Medical Plus Blue℠ and BCN Advantage℠ members.
Here’s a summary of the changes that will occur starting Sept. 1:
- For both Blue Cross and BCN commercial members, additional cardiology and advanced imaging services will require prior authorization.
- For Blue Cross commercial members, additional sleep study services will require prior authorization.
- For BCN commercial members, Carelon will start managing in-lab sleep studies.
By Aug. 14, the Carelon ProviderPortal® and the Carelon call center will be ready to accept prior authorization requests for these additional services.
These changes apply to:
- Most Blue Cross commercial members
- All BCN commercial members
For the services that Carelon already manages, you’ll continue to request prior authorization through the Carelon ProviderPortal.
Look for additional details about these changes in upcoming provider alerts and newsletter articles.
Carelon Medical Benefits Management is an independent company that contracts with Blue Cross Blue Shield of Michigan and Blue Care Network to manage prior authorizations for select services.
Lunch and learn webinars for physicians and coders focus on risk adjustment, coding
As a reminder, we’re offering live, 30-minute educational webinars that provide updated information on documentation and coding for common challenging diagnoses. Webinars include an opportunity to ask questions.
Here’s our upcoming schedule and tentative topics for the webinars. Each session starts at noon Eastern time. Log in to the provider training website to register for sessions that work with your schedule.
Session date |
Topic |
July 19 |
Coding heart disease and vascular |
Aug. 16 |
Medical record documentation and coding MEAT |
Sept. 20 |
Coding tips for COPD and asthma |
Oct. 18 |
ICD-10-CM updates and changes for 2024 |
Nov. 15 |
Coding chronic kidney disease and rheumatoid arthritis |
Dec. 13 |
CPT coding scenarios for 2024 |
If you haven’t already registered for the provider training website, follow these steps:
- Click here to register.
- Complete the registration. We recommend using the same email you use to communicate with Blue Cross Blue Shield of Michigan for other needs. This will become your login ID.
Locating a session
Click here if you are already registered for the provider training website. On the provider training website, look in the Event Calendar or use the search feature using the keyword “lunch” to quickly locate all 2023 sessions.
See the screenshots below for more details. 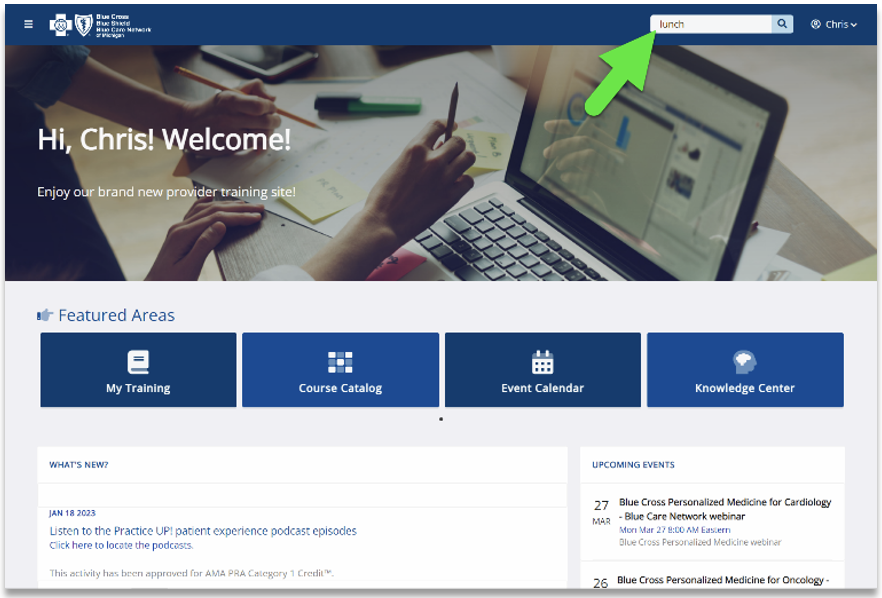
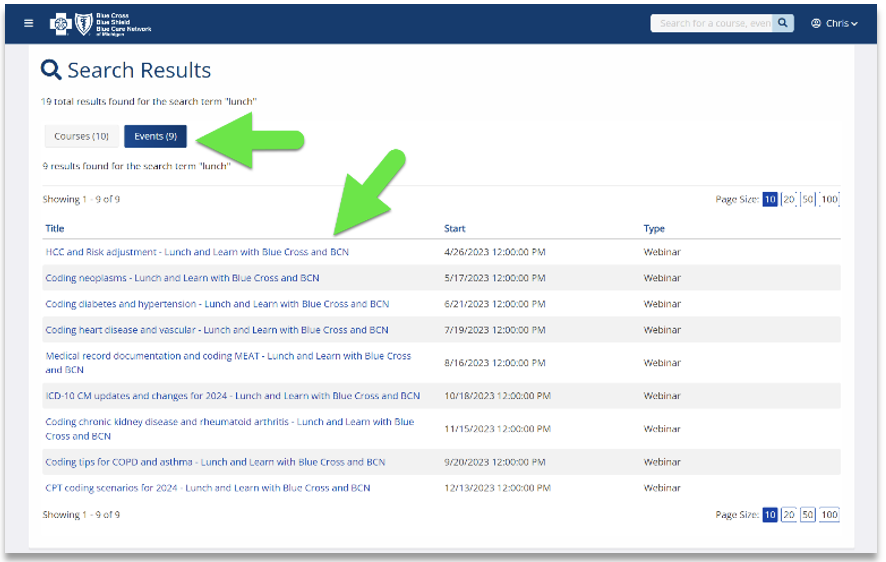
Previous sessions
You can also listen to previously recorded sessions. Check out the following:
Previous sessions
You can also listen to previously recorded sessions. Check out the following:
Date |
Topic |
April 26 |
HCC and risk adjustment coding scenarios |
May 17 |
Coding neoplasms |
June 21 |
Coding diabetes and hypertension |
For more information
If you have any questions about the sessions, contact April Boyce at aboyce@bcbsm.com. If you have questions regarding a session or website registration, email ProviderTraining@bcbsm.com.
Reminder: Physical medicine treatment plans developed by chiropractors
Medical doctors (M.D.s and D.O.s) may be asked to agree to and sign a physical medicine treatment plan developed by chiropractors. The physical medicine treatment plan must be kept on file by the chiropractor.
Blue Cross Blue Shield of Michigan will pay for the first physical medicine service per patient, not per visit. A prescription isn’t required for a member to receive covered physical medicine services from a chiropractor.
Also, as a reminder, we no longer use the term “physical therapy” when referring to certain types of treatment provided by chiropractors. We use the term “physical medicine.” We’re currently in the process of updating benefit information on Availity and Benefit Explainer, as well as our certificates and riders, to reflect this verbiage change.
Note: No physician agreement or signature is required on a treatment plan for MESSA members.
For more details on chiropractic services, see the “Chiropractic Services” chapter of the Blue Cross Commercial Provider Manual.
We’ve updated medical record documentation guidelines for musculoskeletal procedures
In February 2023, Blue Cross Blue Shield of Michigan, Blue Care Network and TurningPoint Healthcare Solutions LLC updated the guidelines for medical record documentation for musculoskeletal procedures as follows:
See the updated requirements document titled GN-1002 Medical Record Documentation.** It’s available on the Musculoskeletal Services pages of our ereferrals.bcbsm.com website.
**Blue Cross Blue Shield of Michigan and Blue Care Network don’t own this document and aren’t responsible for its content.
TurningPoint Healthcare Solutions LLC is an independent company that manages authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
We’ve made updates to list of musculoskeletal procedure codes that require prior authorization
We recently updated the Musculoskeletal procedure codes that require authorization by TurningPoint document to reflect the following changes:
- For dates of service on or after March 19, 2023, procedure code *64625 is no longer payable for Medicare Plus Blue℠ or BCN Advantage℠ members.
Note: This procedure code continues to be payable for Blue Cross Blue Shield of Michigan and Blue Care Network commercial members. It requires prior authorization for BCN commercial members. It doesn’t require prior authorization for Blue Cross commercial members.
- For dates of service on or after March 25, 2023, procedure code C1767 doesn’t require prior authorization for Medicare Plus Blue, BCN commercial or BCN Advantage members.
Note: This procedure code has never required prior authorization for Blue Cross commercial members.
- For dates of service on or after July 1, 2023, procedure code *0775T will require authorization for Blue Cross commercial, Medicare Plus Blue, BCN commercial and BCN Advantage members.
For more information about TurningPoint’s musculoskeletal surgical quality and safety management program, see the following pages on the ereferrals.bcbsm.com website:
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
TurningPoint Healthcare Solutions LLC is an independent company that manages prior authorizations for musculoskeletal surgical and related procedures for Blue Cross Blue Shield of Michigan and Blue Care Network.
HMS to decommission its provider portal
As reported in the November 2022 Record, Blue Cross Blue Shield of Michigan and Blue Care Network transitioned their audit services from HMS® to Cotiviti in December 2022 for Medicare Plus Blue℠ and BCN Advantage℠ claim reviews. HMS and Cotiviti are independent companies that provide auditing support services for Blue Cross and BCN.
HMS will decommission its provider portal on July 31, 2023. Starting Aug. 1, access to the portal will cease. Clients and health care providers attempting to log in to the portal on or after Aug. 1 will receive an error message stating the portal has been decommissioned.
Records uploaded into the portal prior to the decommission date will continue to be processed.
Call Cotiviti Provider Relations at 1-866-875-1749 to address:
- Questions or issues pertaining to records uploaded prior to Aug. 1, 2023
- Questions or instructions about submitting records or appeals on or after Aug. 1.
To submit records or appeals to Cotiviti on or after Aug. 1, fax them to 203-202-6511.
Reminder: IMRT delivery codes
Blue Cross Blue Shield of Michigan continues to expand its claim editing process to further promote correct coding and payment accuracy. As part of our efforts, we want to remind you that delivery codes for intensity-modulated radiation therapy, or IMRT, that are billed within a 14-day period before or after the IMRT planning code shouldn’t be billed separately.
CPT codes *77014, *77280, *77285, *77290, *77295, *77306 through *77321, *77331 and *77370 are considered as included in the payment for CPT code *77301 (IMRT planning) when performed as part of the development of the IMRT plan on the same or different dates of service for the same tumor. This is in alignment with guidelines from the American Medical Association, as well as the Centers for Medicare & Medicaid Service’s National Correct Coding Initiative Policy Manual.
Be sure to bill IMRT services according to the above guidelines. When the above-mentioned CPT codes are billed separately, they may be denied.
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
|