Forward to a friend |
Subscribe | The Record Archive | Contacts | bcbsm.com | Print this article
|
January 2023
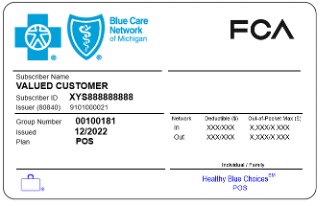
Members enrolled in Healthy Blue Choices POS don’t need referrals to specialistsWhat you need to know We want to let specialists who participate with Blue Cross Blue Shield of Michigan know that members enrolled in Healthy Blue Choices℠ POS don’t need a referral to see them for covered services. However, some services are covered only from in-network providers, including office visits. Healthy Blue Choices℠ POS is a new point-of-service plan, effective Jan. 1, 2023, for FCA non-bargaining employees and retirees** that allows the flexibility to receive covered health care services in or out of network without a referral. It’s administered by Blue Care Network and works similarly to our popular Blue Elect Plus℠ POS plan. Members enrolled in Healthy Blue Choices POS or Blue Elect Plus POS don't need a referral for any covered service. They can refer themselves to any provider — even to providers who are considered out of network for this product. The member ID card prefix for both plans is the same one that’s on the member ID card for HMO coverage. The difference is that the front of the ID card shows the name of the plan. (See image below.) In addition, there is wording on the back of the card noting that referrals aren’t required. Healthy Blue Choices POS for employees
Requirements for selecting a primary care provider Healthy Blue Choices POS members with a Michigan address must select a BCN primary care physician; however, they also have the option to receive covered health care services in or out of network without a referral. Members who live outside of Michigan, with a non-Michigan address, don’t need an assigned primary care physician. They also don’t need a referral — they just need to see a BlueCard-participating provider if they want to pay the lower in-network out-of-pocket costs. More key information
For more information Refer to the Healthy Blue Choices℠ POS webpage for more information. If you have questions about Healthy Blue Choices POS, call Provider Inquiry as follows:
**FCA bargaining employees are covered under a separate health plan administered by Blue Care Network. |
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|