
Forward to a friend |
Subscribe | The Record Archive | Contacts | bcbsm.com | Print this article
|
November 2020
How to use C3 to correctly bill multiple surgery outpatient facility claimsWhen two surgeries that have a mutually exclusive relationship or represent an overlap in services are billed on the same date, only one surgery is eligible for payment. To ensure proper reimbursement on outpatient claims, the charges for the claim should be billed on the line with the more extensive surgery. This can be determined by using the Clear Claim Connection™ tool, also known as C3. C3 enables you to view the Blue Cross Blue Shield of Michigan professional and outpatient facility claim combination rules and clinical rationale. Specifically, this web-based code-auditing reference tool does the following:
Obtaining access You can find the C3 web link on Provider Secured Services by following these steps:
If you don’t have access to web-DENIS, you can call our helpline toll-free at 1-877-258-3932, weekdays from 8 a.m. to 8 p.m. Or complete and return the Professional Secured Access and Use and Protection Agreement forms available on our website. From the Claim Entry screen, pictured below, follow these steps:
Note: Codes with letters must be keyed in upper case. 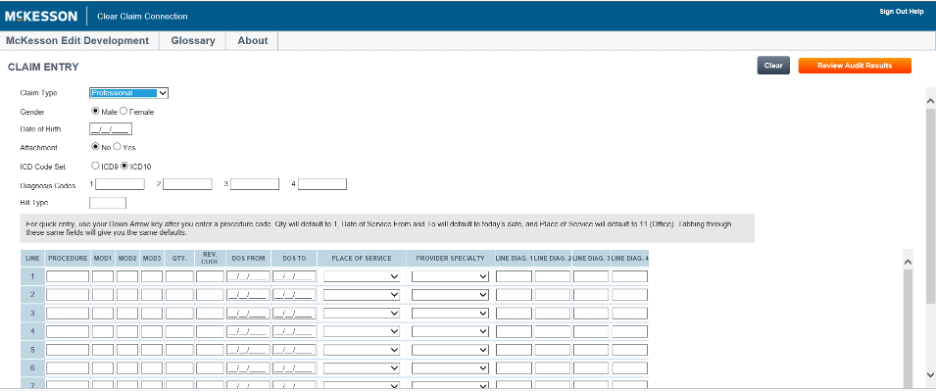 The C3 entry screen initially allows 10 rows for entering procedure codes. An additional 10 rows may be added by clicking the Add More Procedures line located directly under the procedure code entry field.
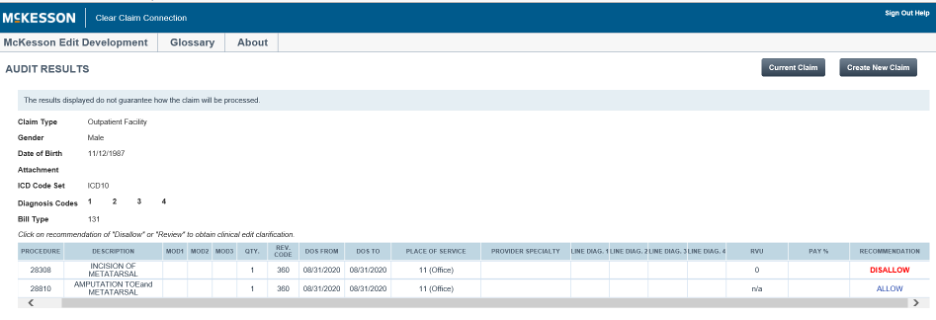 The results from entering the code combinations will be displayed in the Recommend column as Allow, Disallow or Review. A clinical edit clarification is provided for those claims with a recommendation of Disallow or Review. The above screen will help you identify primary surgery and secondary (or inclusive) surgeries so that you can roll up charges correctly on the primary surgery claim line. To view a clinical edit clarification, click on the procedure line that displays Disallow or Review. From this screen you can print the rationale (Printable Version), choose to enter a new claim (New Claim), go back to the original claim entry screen (Current Claim) or review the decision for the original claim (Review Claim Audit Results). 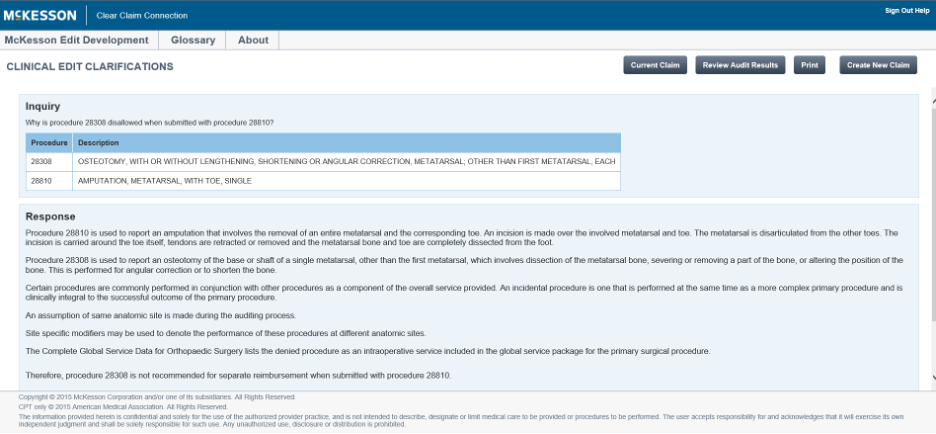 Please note that the clinical edits and rationale contained within C3 aren’t to be used as a guarantee of payment or a source for benefit policy information. Note: When all billed surgeries performed on the same day are payable, then repeat the following steps to identify most intensive surgery:
The claim scenario below shows that both procedures, 58140 and 29860, are payable when performed on the same date of service. However, the relative value unit, or RVU, of procedure 58140 is 26.92, and the relative value unit of procedure 29860 is 19.24. Therefore, procedure 58140 is more intensive, and the provider may roll up charges on the claim line reported with procedure 58140. 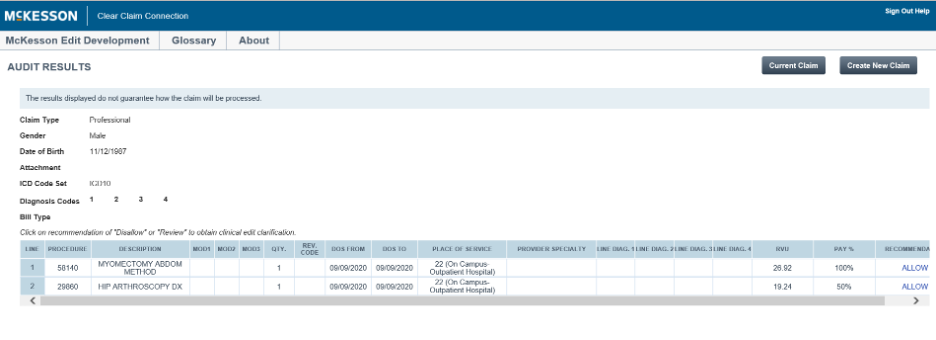 To end the session, click on Logoff. Note: The information contained in C3 is based on the date of service or the date the procedure code combination is entered for review. Exclusions C3 isn’t intended for use with combination rules that include the following:
C3 may occasionally be unavailable on Saturdays from 9 a.m. to 1 p.m. for maintenance. |
|
No portion of this publication may be copied without the express written permission of Blue Cross Blue Shield of Michigan, except that BCBSM participating health care providers may make copies for their personal use. In no event may any portion of this publication be copied or reprinted and used for commercial purposes by any party other than BCBSM.
|