|
January 2019

Blue Cross will start notifying providers on the CMS preclusion list in January
The Centers for Medicare & Medicaid Services adopted a rule in April 2018 that stipulates providers can’t be on a preclusion list and receive payment from a Medicare plan. CMS will make the preclusion list available to Part D sponsors and Medicare Advantage plans, beginning Jan. 1, 2019.
Once Blue Cross Blue Shield of Michigan receives the preclusion list on the first of each month, our Provider Enrollment and Data Management department will send a letter — within 30 days — to any contracted Medicare Plus BlueSM PPO provider who is on the list. The letter will include the effective date of the provider’s preclusion, which will be 90 days from the date of the published preclusion list.
We’re required to remove any contracted provider who is included on the preclusion list from our networks. We’re also required to notify enrollees who have received care in the last 12 months from a contracted provider or a prescription from a provider who is on the preclusion list.
In addition, effective April 1, 2019:
- Part D sponsors will be required to reject a pharmacy claim (or deny a beneficiary request for reimbursement) for a Part D drug that is prescribed by an individual on the preclusion list.
- Medicare Advantage plans will be required to deny payment for a health care item or service given by an individual or entity on the preclusion list.
What is the preclusion list?
The preclusion list is a list of providers and prescribers who are precluded from receiving payment for Medicare Advantage items and services or Part D drugs furnished or prescribed to Medicare beneficiaries. The list was created to replace the Medicare Advantage and prescriber enrollment requirements and to ensure patient protections and to protect the trust funds from prescribers and providers identified as bad actors.
More information is available at the CMS website.**
** Blue Cross Blue Shield of Michigan doesn’t own or control this website.
CMS releases 2019 opioid safety edits
In the final contract year 2019 Call Letter, the Centers for Medicare & Medicaid Services announced strategies to further help Medicare Part D plan sponsors prevent and combat prescription opioid overuse. CMS has tailored its approach to help Medicare Part D opioid users, including new or opioid naïve users, chronic opioid users and those with potentially problematic concurrent medication use.
CMS’ opioid safety edits are intended to encourage both prescribers and members to actively think about and discuss overdose risks and prevention. Residents of long-term care facilities, those in hospice care, patients receiving palliative or end-of-life care, and patients being treated for active cancer-related pain are exempt from these interventions. Buprenorphine for medication-assisted treatment isn’t included in the opioid safety edits.
CMS expects sponsors to implement the following edits beginning Jan. 1, 2019:
- Soft edit for concurrent opioid and benzodiazepine use
- Soft edit at the point of sale to prompt additional safety review when these agents are used concurrently.
- If the opioid or benzodiazepine is written by the same prescriber, this edit will not generate. If the prescriptions are written by different prescribers, the edit will generate.
- Soft edit for duplicative long-acting opioid therapy
- Soft edit at the point of sale to prompt additional safety review when a member is receiving multiple long-acting opioids.
- Any usage of multiple long-acting opioids, even if prescribed by the same provider, will generate this edit.
- Care coordination edit at 90 morphine milligram equivalents
- The care coordination edit will trigger when a member’s cumulative MME per day across their opioid prescriptions reaches or exceeds 90 MME, and there are at least two prescribers contributing to the edit.
- The pharmacist must consult the prescriber and document the discussion and, if the prescriber confirms medical necessity, use an override code that indicates the prescriber has been consulted.
- Buprenorphine for medication-assisted treatment will not trigger the edit.
- Hard edit at 200 morphine milligram equivalents
- Beginning Jan. 1, 2017, CMS required sponsors to implement a cumulative opioid edit.
- The edit will trigger when a member’s cumulative MME per day across their opioid prescriptions reaches or exceeds 200 MME.
- Claims that trigger the edit will be stopped at the point of sale and require prior authorization for processing.
- Hard edit seven-day supply limit for initial opioid fills
- Hard edit to limit initial opioid prescription fills for the treatment of acute pain to no more than a seven-day supply for opioid naïve members, who are members who haven’t filled an opioid prescription in the preceding 108 days.
- This includes short- and long-acting opioids, except buprenorphine for medication-assisted treatment, which won’t trigger the edit.
- CARA Drug Management Program
- CMS requires sponsors to establish drug management programs for members who are at-risk of overuse and allow sponsors to limit members’ coverage for frequently abused drugs to certain prescribers and pharmacies. This is known as a lock-in.
- A member specific point of sale claim edit may be implemented after case management with the prescribers and notice to the beneficiary.
- The member will have to meet clinical guidelines based on the level of opioids they are taking and the fact that they are obtaining them from multiple pharmacies and prescribers to be eligible.
- Monitoring for concurrent opioid and opioid-potentiator use
- CMS has requested increased vigilance and monitoring of members taking the combination of opioids and opioid-potentiator medications (gabapentin, pregabalin).
Providers can find out more about Part D coverage at the CMS website.** This website also includes educational materials about Medicare prescription coverage for doctors and other health care professionals.
** Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Certain infusion drugs won’t be covered in outpatient hospitals, starting Jan. 1
Here’s important information we communicated Nov. 1 in a web-DENIS message:
Beginning Jan. 1, 2019, Blue Cross Blue Shield of Michigan is adding three preauthorized medical drugs to the site of care requirement for members. Infusions for these drugs won’t be covered at hospital outpatient facilities without prior authorization for an approved location, starting Jan. 1.
The authorization requirement only applies to groups that are currently participating in the commercial Medical Drug Prior Authorization program for drugs administered under the medical benefit. These changes don’t apply to BCN AdvantageSM, Blue Cross Medicare Plus BlueSM PPO or Federal Employee Program® members.
All drugs included in this program already need prior authorization for payment. Approved authorizations will be payable for professional locations, with no further action required:
- Physician’s offices or other health care provider’s offices
- Ambulatory infusion centers
- The member’s home, from a home infusion therapy provider
Members must receive their infusions in a professional office setting, a professional infusion center or in the member’s home.
If your patient currently receives one of these infusions at a hospital outpatient facility:
- Submit a prior authorization request for your patient to Blue Cross for a hospital outpatient facility. If this request isn’t submitted and approved, the patient will be responsible for the full cost of the medicine.
- Find out where your patient can continue his or her infusion therapy. Check the directory of participating home infusion therapy providers and infusion centers. Please confirm network participation for your patient before his or her infusion.
- Tell your patient to contact any of the listed infusion therapy providers. If they’re able to accommodate your patient, they’ll work with you and your patient to make the change easy. We’re also sending this information to your patient.
- Help your patient switch his or her infusion therapy to your office, infusion center or home infusion therapy provider by Jan. 1.
For the ordering provider:
If a member must receive one of these infusions in a hospital outpatient facility, follow the normal steps for a prior authorization request and include:
- The authorization number previously approved
- Rationale that clearly describes the reason the infusion must be administered in a hospital setting
- Supporting chart notes
The medical drugs subject to this requirement include:
HCPCS |
Drug name |
J2786 |
Cinqair® |
J2182 |
Nucala® |
J2357 |
Xolair® |
For more information about hospital outpatient infusion therapy, view previous issues of The Record:
2017
October
December
2018
March
June
AMA updates applied behavior analysis codes for autism
If you currently use the following codes to bill applied behavior analysis for autism services to Blue Cross Blue Shield of Michigan, you need to change the codes you bill starting Jan. 1, 2019:
- *0359T-*0361T
- *0363T-*0372T
- *0374T
The above-listed T codes are ending Dec. 31, 2018, following the American Medical Association’s procedure code changes. On Jan. 1, 2019, the previous codes will be replaced with the following:
- *0362T
- *0373T
- *97151-*97158
Starting with dates of service in 2019, you should use one of the appropriate procedure codes only if you used the T codes in 2018.
Prior authorizations for applied behavior analysis that were requested and approved under the T codes will remain valid. You don’t need to request a new authorization to accommodate the change in procedure codes.
The code change doesn’t apply to any Blue Cross services that didn’t use these T codes for autism specific benefits in 2018. The change also doesn’t apply to Blue Care Network.
Coverage for some diabetes drugs changing, starting Jan. 1
Our goal at Blue Cross Blue Shield of Michigan and Blue Care Network is to provide our members with safe, high-quality prescription drugs while also controlling costs. To accomplish this, we’re making coverage changes to some diabetes drugs (see tables below).
To discuss treatment options with their doctors, we’ll let members fill their current prescriptions through Feb. 28, 2019. If members fill their prescriptions on or after March 1, 2019, it will cost more or will no longer be covered.
Members who have an approved prior authorization for any of the drugs listed below can continue to fill their prescriptions until the prior authorization end date, but may have a higher copayment.
Drug that will have a higher copayment, starting Jan. 1, 2019:
Drug class: Insulins |
Nonpreferred drug |
Member cost |
Preferred alternatives |
Basaglar® Kwikpen U-100 |
Nonpreferred brand copayment |
Lantus® (all forms)
Levemir® (all forms)
Toujeo® (all forms)
Tresiba® Flextouch® |
Drugs we won’t cover, starting Jan. 1, 2019:
Drug class: Glucagon-like peptide-1 (GLP-1) receptor agonists |
Excluded drugs |
Member cost starting March 1, 2019 |
Preferred alternatives |
Bydureon® (all forms)
Byetta® |
Full cost |
Ozempic®
Trulicity®
Victoza® |
Drug class: Dipeptidyl peptidase 4 (DPP-4) inhibitors |
Excluded drugs |
Member cost starting March 1, 2019 |
Preferred alternatives |
Alogliptin**
Onglyza®
Nesina® |
Full cost |
Januvia®
Tradjenta® |
Drug class: Dipeptidyl peptidase 4 (DPP-4) inhibitors combinations |
Excluded drugs |
Member cost starting March 1, 2019 |
Preferred alternatives |
Alogliptin/metformin**
Alogliptin/pioglitazone**
Kazano®
Kombiglyze®
Oseni®
Steglujan® |
Full cost |
Glyxambi®
Janumet®
Janumet® XR
Jentadueto®
Jentadueto® XR
Qtern® |
**These aren’t generic drugs. These are considered brand-name drugs and don’t have generic equivalents.
Medicare Part B medical specialty drug prior authorization lists changing in 2019
Some updates are coming for the Part B medical specialty medical prior authorization drug list for Blue Cross Medicare Plus BlueSM PPO and BCN AdvantageSM members. These changes include additions and removals from the prior authorization program as follows.
Medicare Plus Blue PPO
Removals — for dates of service starting Jan. 1, 2019:
- J0202 Lemtrada®
- J2323 Tysabri®
- J2350 Ocrevus®
Additions — for dates of service starting Feb. 1, 2019:
- C9036 Onpattro™
- J2840 Kanuma®
- J2860 Sylvant®
- J3357 Stelara® SQ
- J3358 Stelara® IV
- J1746 Trogarzo™
- J9022 Tecentriq®
- J9023 Bavencio®
- J9042 Adcetris®
- J9176 Empliciti®
- J9308 Cyramza®
- J9352 Yondelis®
For Medicare Plus Blue, we require prior authorization for these medications when you bill them on a professional CMS-1500 claim form or by electronic submission via an 837P transaction, for the following sites of care:
- Physician office (place of service code 11)
- Outpatient facility (place of service code 19, 22 or 24)
We don’t require authorization for these medications when you bill them on a facility claim form (such as a UB04) or electronically via an 837I transaction.
BCN Advantage
Removals — for dates of service starting Jan. 1, 2019:
- J9032 Beleodaq®
- J9310 Rituxan®
Additions — for dates of service starting Feb. 1, 2019:
- J2860 Sylvant®
- J3357 Stelara® SQ
- J3358 Stelara® IV
- J3490/C9399 Onpattro™
- J1746 Trogarzo™
- J9022 Tecentriq®
- J9023 Bavencio®
- J9042 Adcetris®
- J9176 Empliciti®
- J9352 Yondelis®
For BCN Advantage, we require prior authorization for these medications when you bill them on a professional CMS-1500 claim form (or submit them electronically via an 837P transaction) or on a facility claim form such as a UB04 (or submit them electronically via an 837I transaction), for the following sites of care:
- Physician office (place of service code 11)
- Outpatient facility (place of service code 19, 22 or 24)
- Home (place of service code 12)
Reminder: You must get authorization prior to administering these medications. Use the NovoLogix® online tool to quickly submit your requests.
Reminder: Update TPA, Provider Authorization Form when making changes to trading partner information
Blue Cross Blue Shield of Michigan is dedicated to safeguarding the protected health information of our members. These safeguards include completion of a Trading Partner Agreement and Provider Authorization Form as part of the electronic data interchange setup process. All EDI trading partners must complete both before they can exchange PHI with Blue Cross.
Terms of the TPA require you to notify Blue Cross of any changes in your trading partner information. You must update your Provider Authorization Form if you send claims using a different submitter ID or route your Electronic Remittance Advice, or 835s, to a different unique receiver or trading partner ID. Updating the form ensures information is routed to the appropriate destination.
Any time you switch vendors, billing services or clearinghouses, you need to update your Provider Authorization Form.
To make changes to your EDI setup:
- Go to bcbsm.com.
- On the homepage, select Providers.
- On the Providers page, select Quick Links under Welcome to Provider Services.
- Click on Electronic Connectivity (EDI) from the list of links and then select How to use EDI to exchange information with us electronically.
- Select Update your Provider Authorization Form in the middle of the page under EDI Agreements.
You should review your provider authorization information if you’ve:
- Joined a new group practice.
- Left a group practice and now bill using your own NPI.
- Hired a new billing service.
- Started submitting claims through a clearinghouse or you’ve changed clearinghouses.
- Decided you no longer want to receive 835 files.
- Selected a new destination for your 835s.
For questions about EDI enrollment, contact our help desk at 1-800-542-0945. For assistance with TPA and Provider Authorization forms, select the TPA option.
Here’s more information about professional claim editing enhancements, including DME/P&O services
On Dec. 21, 2018, Blue Cross Blue Shield of Michigan added advanced claim editing for select groups. This is an enhancement to our claim editing processes that encourage correct coding. The goal is to have claim payment policies that are national in scope, simple to understand and come from respectable sources. Given the widespread use of these policies, we believe this will help you and your billing staff to better understand our payment of your claims.
The enhancements are for the correct reporting of:
- Diagnosis codes
- Procedure age
- Modifier guidelines
- Global surgery
- Split surgical care
- Co-surgery
- Team surgery
- Once per lifetime services
- Place of service
- Anesthesia
We’ll administer nationally recognized clinical editing based on guidelines established by American Medical Association CPT guidelines, Centers for Medicare & Medicaid Services standards and general peer accepted standards.
Examples of some edits we’ll adopt:
- Use modifier 79 to report a service performed by the same provider only when the service is unrelated to the original procedure during the 0-day, 10-day or 90-day global period. Documentation must clearly indicate that the procedure is unrelated to the prior surgical procedure.
- Professional services billed by a durable medical equipment supplier, physical therapist or speech-language pathologist during the same time period as institutional hospice care is included in the institutional stay.
- Bill a finger extension or flexion device (procedure code E1825) with the proper finger modifier (FA-F9).
- Manual wheelchair accessories shouldn’t be billed with a power wheelchair.
- Capped rentals should be billed with no more than one capped rental modifier (KH, KI, KJ) on the same claim line.
You can review previous publications on our claim editing process enhancements in the September 2018 Record and the December 2018 Record.
Appeal process for clinical edits
In addition, we’re also streamlining the appeal process for clinical edits. The following changes will begin Jan. 1, 2019:
- Appeals must be submitted with a Clinical Editing Appeal form. All required fields must be completed or the appeal will be returned to you. This form can be found on the Blue Cross provider site. It will also be available in the online provider manual on web-DENIS.
- Submit the appeals form one of the following ways:
- Fax it to 1-866-392-7191
- Mail it to Clinical Editing Appeals
Mail Code G820
Blue Cross Blue Shield of Michigan PPO
611 Cascade West Parkway, SE
Grand Rapids, MI 49546-2143
- Appeals must be submitted within 180 days of the original clinical editing denial.
- Documentation supporting the appeal must be submitted with the appeal. What is required may vary on the service being appealed. For example, office services that have denied may require office notes, services denied as duplicates will require records for both the denied and paid service to show more than one was performed, surgical denials may require operative reports, and so on. It’s important to look at the denial reason and submit documentation appropriate to the procedure code that was denied and the denial reason.
This process is based on the BCN and Medicare Advantage clinical editing appeals processes. So, if you have submitted an appeal to BCN or MA PPO in the past for a clinical edit, then you have followed the process that will be in place for PPO. The only differences are the explanation (or message) codes and the fax number.
If you have questions about the changes in the appeal process, contact Provider Inquiry at 1-866-344-8525 or contact your provider representative.
Blue Cross qualification forms should be submitted electronically
This year, you’ll probably see patients with wellness plans who ask you to complete and return their 2019 Blue Cross Blue Shield of Michigan qualification forms. Here are some reminders about completing the forms:
- We didn’t make any changes to the qualification forms for 2019.
- Make sure all fields on the form are completed in their entirety before submitting for accurate processing.
- Perform the cotinine test only if the qualification form indicates it’s required, as it’s not a standard covered benefit.
- If you’re a Michigan health care provider, submit Blue Cross qualification forms electronically to improve form processing.
- Out-of-state providers can fax completed forms to 1-866-392-6496.
We’re instructing members to partner with their doctor to complete and submit the qualification form. We’re asking you to submit the qualification form electronically for your convenience and to help improve processing time.
The form and instructions for completing it electronically are online:
- Log in to the Provider Secured Services page at bcbsm.com.
- Scroll down to the BCBSM Qualification Form section.
- Click on the BCBSM Qualification Form link, which will send you to the online form.
- For instructions for completing the form, select BCBSM Qualification Form Instructions (located below the BCBSM Qualification Form link).
- After completing the electronic qualification form for your patient, print two copies of the form.
- Give one completed and signed copy to your patient and keep a copy of the form with the patient’s medical records.
If you’re an out-of-state provider you’ll need to fax completed forms to 1-866-392-6496. We gave your patients instructions on how to print out a form for you to complete.
Please continue using the Healthy Blue LivingSM qualification form for Blue Care Network members.
Value-based reimbursements will be applied to additional anesthesia time and base modifiers
The value-based reimbursement fee schedule sets fees at greater than 100 percent of the anesthesia maximum payment schedule.
Currently, if an anesthesiologist is eligible to be reimbursed in accordance with the VBR fee schedule, value-based reimbursements are applied to the time and base codes billed by the anesthesiologist with the AA and GC modifiers.
Effective March 1, 2019, value-based reimbursements will also be app
Starting Feb. 1, eviCore managing two radiopharmaceutical drugs
For dates of service on or after Feb. 1, 2019, the following radiopharmaceutical drugs need authorization through eviCore healthcare:
- Lutathera® (lutetium Lu 177 dotatate, HCPCS code A9513)
- Xofigo® (radium Ra 223 dichloride, HCPCS code A9606)
This applies to members covered by:
- Blue Cross Blue Shield of Michigan PPO (commercial) and Blue Cross Medicare Plus BlueSM PPO
Note: Currently, eviCore manages procedures associated with code A9606 for Blue Cross and Medicare Plus Blue members. On Feb. 1, eviCore will begin managing procedures associated with code A9513.
- BCN HMOSM commercial and BCN AdvantageSM
Note: Lutathera was managed for BCN HMO members under the prior authorization program for drugs covered under the medical benefit. Currently, eviCore manages procedures associated with code A9513 (currently C9031) for BCN Advantage members. For BCN HMO members, C codes aren’t payable. However, services associated with the administration of an approved treatment plan with Lutathera are payable for BCN HMO members. On Feb. 1, eviCore will begin managing procedures associated with code A9606 for both BCN HMO and BCN Advantage.
We’ll update the Procedures that require authorization by eviCore healthcare document before the effective date of the change.
Send authorization requests to eviCore online or by telephone at 1-855-774-1317.
Note: These changes don’t apply to MESSA members.
Helping patients with medication compliance
When patients adhere to their medication plan, it reduces the chance of adverse events and mortality — particularly for patients with diabetes, hypertension and coronary artery disease. But not all patients are taking their medication as prescribed.
For every 100 prescriptions written:
- 50 to 70 are filled by the pharmacy
- 48 to 66 are picked up from the pharmacy
- 25 to 30 are taken properly
- 15 to 20 are refilled as prescribed
There are many factors that affect patient adherence:
- A patient’s understanding of the disease
- A patient’s expectations of improvement from the medication
- Side effects the patient experiences
Some individuals are unintentionally noncompliant due to their mental health status or confusion, often complicated by a polypharmacy regimen. Polypharmacy relates to the simultaneous use of multiple drugs to treat a single ailment or condition.
As always, a patient’s best resource if they have questions about their condition and medication is their doctor.
How the Federal Employee Program® can help
Members who participate in the Federal Employee Program can take advantage of additional resources to help them adhere to their medication regimen. Services include chronic condition programs that enable a member to talk on the phone or communicate online with a health coach.
For more information, FEP members can go to fepblue.org or call the Customer Service number on the back of their member ID card.
Here are the FEP benefit updates for 2019
Following are the benefit changes for the 2019 Federal Employee Program Standard and Basic Options.
- Preventive care benefits
- No limitation for adult preventive booster of the tetanus, diphtheria, pertussis (Tdap) vaccine
- Pathology services associated with preventive colonoscopies or sigmoidoscopies
- Appropriate site of care
- Benefits for inpatient admissions to nonmember hospitals or other facilities for emergency (maternity) deliveries and base payment on the billed amount. Benefits for inpatient admissions to nonmember hospitals and other facilities for non-emergency (routine maternity) deliveries and base payment on the local plan allowance
- Blue Cross plan allowance used to reimburse outpatient nonmember facilities for non-emergency services
- Nonparticipating provider calculation process for emergency medical services performed in the emergency department of a nonmember facility will reference Blue Cross plan allowance instead of the usual, customary and reasonable, or UCR, amount
- Telehealth services for dermatology care – diagnosis, treatment and prevention of diseases of the skin, hair, nails and body
- Gender reassignment surgery
- Members are required to be under the care of a behavioral health professional for a minimum of 12 months prior to treatment
- Electrolysis added as part of the preparation for gender reassignment surgery
- Miscellaneous benefit changes
- Acupuncture facility-billed claims for services will accumulate toward the annual visit maximum, except when performed as an anesthesia service
- Limit dental diagnostic imaging benefit to intraoral complete series
- Medical benefits for the infusion medication Remicade and its two biosimilars, Renflexis and Inflectra.
- Bariatric surgery benefit for members who have a diagnosis of morbid obesity for a period of one year prior to surgery
- Air ambulance prior approval required for non-emergency transports
- Outpatient facility home-based sleep study claims will be assessed a $40 copayment
- Prior approval for gene therapy and cellular immunotherapy, e.g., CAR-T and T-cell receptor therapy
- For information regarding FEP pharmacy benefits, contact CVS Caremark at 1-800-624-5060 or go to fepblue.org/pharmacy. To view the pharmacy formulary, go to fepblue.org/formulary.
New for 2019: FEP Blue Focus
The Blue Cross and Blue Shield Federal Employee Program® has a new benefit option for 2019 — FEP Blue Focus. This is a fee-for-service plan that provides covered services through a Preferred Provider Organization. Members can choose their own health care providers without referrals but must use Preferred providers to receive benefits.
Benefits under FEP Blue Focus have been divided into three categories:
Core Benefits are those that have a low copayment or none at all and aren’t subject to a deductible or coinsurance. These are benefits commonly used for general care and to cover accidental injuries.
For example, each member’s first 10 health care visits with a primary care physician, specialist or other health care professional are subject to a $10 copayment per visit. Preventive care benefits for adults and children are covered at no cost to the member.
Non-Core Benefits are for unexpected medical costs incurred during the calendar year. They share the same annual deductible and coinsurance level. For example, after a member has 10 health care visits, he or she will pay a coinsurance for additional visits until the deductible is reached.
Wrap Benefits may or may not be used during the year. These benefits are subject to limitations and different copayments or coinsurance levels than the Core and Non-Core benefits.
For example, the calendar-year deductible doesn’t apply to the following:
- Occupational therapy
- Physical or speech therapy
- Maternity care benefits
Occupational, physical or speech therapy services have a $25 copayment per visit and are limited to 25 visits per person, per calendar year for the individual therapy or any combination of all three therapies.
Maternity facility care has a $1,500 copayment per pregnancy. Members who become pregnant during the benefit period are encouraged to contact Blue Cross Blue Shield of Michigan during the first trimester.
Prior approval required
Some services and procedures covered under FEP Blue Focus require prior approval, such as CT scans and MRIs, genetic testing and certain surgeries. Failure to obtain the prior approval may result in a $100 penalty to the member.
Inpatient admissions require precertification. Failure to obtain precertification, may result in a $500 penalty to the member.
For more information on prior approvals or precertification, download the FEP Blue Focus brochure at fepblue.org/brochure or contact Customer Service at 1-800-482-3600.
The FEP Blue Focus benefit plan uses a two-tiered closed formulary.
Preferred retail pharmacy – Tier 1: (Preferred generic drugs at a Preferred retail pharmacy) |
$5 for up to a 30-day supply
$15 for up to a 90-day supply |
Preferred retail pharmacy – Tier 2 (Preferred brand-name drugs) |
40% of the plan allowance (up to $350 maximum) for up to a 30-day supply
40% of the plan allowance (up to a $1,050 maximum) for up to a 90-day supply |
Specialty pharmacy – Tier 2 (Preferred generic specialty drugs and Preferred brand-name specialty drugs) |
40% of the Plan allowance (up to a $350 maximum) for up to a 30-day supply |
Members must obtain prior approval for certain drugs and supplies, and prior approval must be renewed periodically. Preferred retail pharmacies or the Specialty Drug Pharmacy Program must be used to receive benefits. To view the formulary, go to fepblue.org/formulary.
For information about FEP pharmacy benefits, contact CVS Caremark® at 1-800-624-5060 or go to fepblue.org/pharmacy.
Know what’s covered
FEP Blue Focus offers extensive benefits, but it doesn’t cover everything. It’s important to know what isn’t included.
Services FEP Blue Focus doesn’t cover include:
- Routine dental services
- Non-preferred drugs
- Hearing aids
- Skilled nursing facility
- Long-term care
To see a complete list of exclusions, see the FEP Blue Focus brochure at fepblue.org/brochure.
For an official statement of benefits, see the Blue Cross and Blue Shield Service Benefit Plan FEP Blue Focus brochure (RI 71-017). All benefits are subject to the definitions, limitations and exclusions set forth in the brochure.
For more information on FEP Blue Focus, go to fepblue.org or contact Customer Service at 1-800-482-3600.
CVS Caremark® is an independent company that provides pharmacy benefit management services.
Redesigned Blues Brief available electronically starting January
Our one-page provider and facility newsletter, Blues Brief, will have a new look starting in January. Blues Brief contains brief Blue Cross Blue Shield of Michigan and Blue Care Network articles and is distributed by provider consultants to doctors, specialists and their office staff. Provider offices receive it monthly and facilities quarterly.
The refreshed look will feature a new nameplate, color scheme and icons to identify which articles pertain to individual lines of business. Specialty-specific versions will be created periodically for chiropractic, behavioral health and physical, occupational and speech therapy offices.
We have another new feature — providers can now subscribe to receive Blues Brief electronically. Choose from the monthly physician office version, quarterly hospitals and facilities version and the specialty-specific versions.
To avoid possible subscription errors, add Blues Brief to your subscriptions by clicking the Manage Subscriptions link at the bottom of your BCN Provider News or Record newsletter emails. You can also visit the subscription page to choose your preferred Blues Brief versions.

Reminder: Changes to the PGIP allocation will support Organized Systems of Care efforts
As we announced in the April and September 2018 issues of The Record, the Physician Group Incentive Program allocation increased from 5 to 7 percent of the allowed amount in July 2018 to help fund new PGIP Organized Systems of Care initiatives.
Blue Cross Blue Shield of Michigan is now taking the next step in its journey by creating the 2019 PGIP Risk-Bearing OSC program. Starting Jan. 1, 2019, the 7 percent PGIP allocation will be directed as follows:
- Blue Cross will direct 2 percent to fund the 2019 PGIP Risk-Bearing OSC program. This new program rewards OSCs for managing the benefit cost trend of their attributed Blue Cross PPO patient population and is the first step in our pathway to risk strategy.
- The remaining 5 percent will continue to reward eligible physician organizations and OSCs for improving the quality of patient care, system and practice transformation, and reducing costs.
In addition, the PGIP allocation will apply to most professional procedure codes regardless of the billed provider charge, effective Jan. 1, 2019.
Also, as of April 1, 2019, providers will see a new voucher message that represents each of the allocations. There is no change in the overall percentage.
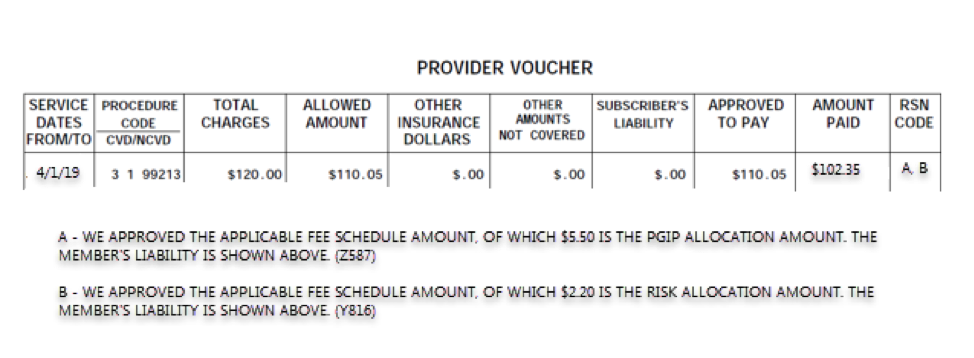
Providers contractually agree in their participation agreements to allocate a portion of their reimbursement to the PGIP fund. All funds allocated are distributed to physician organizations and OSCs that participate in PGIP to support physician practice and system transformation. No money is retained by Blue Cross for administrative costs.
For more information about PGIP, go to bcbsm.com/provider/value_partnerships/pgip.
Note: Claims for Federal Employee Program® members are excluded from the PGIP allocation.
Remember to check member benefits and eligibility
At Blue Cross Blue Shield of Michigan, we’re enhancing our systems to make sure you have consistent information about member benefits.
Be sure to check member eligibility and benefits through web-DENIS and Provider Automated Response System, or PARS, since they could change any time during the year or during open enrollment.
Use PARS when calling to receive general benefit information. Our provider inquiry representatives will be available to help you if you’re unfamiliar with using PARS or if the information you’re looking for is not on PARS.
You can also use web-DENIS to obtain benefit and eligibility information online.
Checking benefits and eligibility this way will help you be sure that you have the most up-to-date information about your patients. It will also help you save time since you don’t have to wait in call queues.
For more information about PARS, check out the September 2017 Record article “Here are some tips for navigating PARS.”
You don’t need to reset your password as often
We’ve changed our password reset requirements for the Blue Cross Blue Shield of Michigan secure provider website. In the past, you had to change your password every 30 days. Now you only need to change it every 60 days.
We made this change to make it easier for you to do business with us. We know it can be challenging to change your password so often, so we’ve reduced the number of times you need to do it. Resetting your password is still important because it’s a key step in securing patient information.
Tips for keeping your office’s information secure:
- Don’t share user IDs. Each employee who needs access should have an individual ID.
- Protect your passwords. The safest passwords are hard to guess, never shared and never posted where others can see them.
- Disable access when employees leave your company. When a user no longer needs access to our system, make sure you tell us right away so we can remove his or her access. Fax a request on your company’s letterhead to 1-800-495-0812. Include the name of the employee who no longer needs access, the person’s user ID and the signature of the current authorized employee.
- Secure your workstation. Before leaving your workstation, make sure your computer is secure and lock your screen.
If you need technical help to access our website, contact the Blue Cross Web Support Help Desk at 1-877-258-3932.
Watch for fraudulent prescription and durable medical equipment schemes
Blue Cross Blue Shield of Michigan and Blue Care Network want to make you aware of the escalating prescription schemes that solicit authorizations from prescribers for medications and durable medical equipment that may not be medically necessary for patients. We’ve received complaints from members who have received unwanted medication and supplies.
Some telemarketing companies solicit insurance information and primary care doctors’ contact information from patients through phone calls, emails, social media and online or mail surveys. These companies will then fax prescriptions to the prescriber’s office to obtain his or her authorization. Other times, pharmacies may call requesting authorization from the prescriber to change a medication to a different formulation (for example, extended release or controlled release versus immediate release).
Once the faxed authorization is received, the member begins receiving mailed deliveries of medications or durable medical equipment supplies. Typically, the members’ efforts to contact the pharmacy or DME company to end the shipments aren’t successful.
How to avoid the faxed prescription scheme
Blue Cross urges you to be vigilant about prescriptions received through fax from pharmacies indicating that the patient has requested the medication or needs an authorization for refill. Pay attention to fax or phone requests for the following types of prescriptions:
- Topical applications (lidocaine, doxepin, fluocinonide, calcipotriene, diclofenac, triamcinolone)
- Acid reflux or GERD medication (omeprazole-sodium bicarbonate)
- Diabetic supplies, blood glucose meters, alcohol pads, test strips, lancet devices, control solutions and lancets
- Nasal sprays (dihydroergotamine)
- Non-steroidal anti-inflammatory drugs (naproxen CR/ER, mefenamic acid, fenoprofen calcium)
Red flags
- The faxed prescription may already be completed or offer check boxes for the prescriber to fill out.
- Prescriptions will often request three to five medications, sometimes labeled as a “kit.”
- Beware of requesting pharmacies or DME suppliers that are located out of state. Many times, the prescription will be associated with a pharmacy or DME supplier that you and your patient haven’t had any previous interaction with.
- The prescription will usually request high quantities of medications. Requests for topical applications usually range between 180 to 1,000 grams. Requests for oral dosage forms will typically be enough for a 90-day supply.
Targeted medications frequently change. Carefully review any prescription that your office did not initiate. If you aren’t sure that the patient requested the medication, please do not approve the request. And be especially cautious about requests for topical applications and low- or moderate-intensity pain relievers.
Starting Feb. 1, prior authorization required for high opioid dosages
Blue Cross Blue Shield of Michigan and Blue Care Network remain committed to battling our country’s opioid crisis through various programs and initiatives. Starting Feb. 1, 2019, Blue Cross and BCN will require prior authorization the first time a member’s opioid dosage exceeds 90 morphine milligram equivalents per day. This change affects commercial members only and doesn’t apply to members with an oncology diagnosis or terminal illness, or those with Medicare plans.
The following are opioids commonly prescribed at 90 morphine milligram equivalents per day:
- 90 mg of hydrocodone (nine tablets of hydrocodone/acetaminophen 10/325 mg)
- 60 mg of oxycodone (two tablets of oxycodone extended-release 30 mg)
We’ll continue to ensure that our members receive high-quality care for pain, while reducing potential risks that come from such treatments. Higher opioid dosages haven’t been shown to reduce long-term pain and are associated with a higher risk of overdose and death. Dosages at or above 100 morphine milligram equivalents per day are associated with a nearly nine-fold increase in overdose risk compared to dosages of 20 morphine milligram equivalents per day or less.
To help reduce the risk of overdose, we encourage providers to review their patients’ total daily dose of opioids. This helps to identify patients who may benefit from closer monitoring, reduction or tapering of opioids, a naloxone prescription or other measures.
The Centers for Medicare & Medicaid Services and the Centers for Disease Control and Prevention offer some free resources:
- The CMS morphine equivalent chart is available here.**
- The CDC’s new Opioid Guideline app** includes its Guideline for Prescribing Opioids for Chronic Pain, tools and other resources, including a morphine milligram equivalent calculator.
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
2019 HCPCS Update: Coverage decisions on 2019 procedure codes now available
Information about new or deleted Healthcare Common Procedural Coding System codes, including CPT codes, has been released. You may begin using the new codes starting Jan. 1, 2019.
We’ve posted the 2019 coverage decisions as a PDF on web-DENIS. You can access our annual HCPCS Update document as follows:
- From the homepage of web-DENIS, click on BCBSM Provider Publications and Resources.
- Click on Newsletters & Resources.
- Look in the What’s New section of the page to find the 2019 HCPCS Update.
Our claims processing systems use HCPCS codes to allow health care providers to report services they performed. HCPCS is a two-level coding system. Providers should use the following resources to find the code that best describes the service provided:
- Level I codes are published in the Physicians' Current Procedural Terminology, CPT 2019, maintained by the American Medical Association. For a comprehensive list of 2018 changes, refer to Appendix B.
- Level II codes are the Centers for Medicare & Medicaid Services codes and apply to professional services, procedures, items and supplies. For a comprehensive list of CMS Level II code changes, refer to the HCPCS Level II Code Book.
The 2019 CPT and HCPCS manuals may be purchased from various sources, including the following:
American Medical Association
To order by mail:
Order Department
American Medical Association
P.O. Box 930876
Atlanta, GA 31193-0876
To order online: amabookstore.com
To order by phone: 1-800-621-8335
Practice Management Information Corporation
To order by mail:
PMIC
200 W. 22nd Street, Suite 253
Lombard, IL 60148
To order online: pmiconline.com
To order by phone: 1-800-633-7467, ext. 2713
For more information about the 2019 HCPCS Update, send an email to ProvComm@bcbsm.com.
Always report most current procedure codes so our ClaimsXten™ updates are accurate
As a reminder, we update ClaimsXten™ each quarter. ClaimsXten is clinical editing software that uses the most current Healthcare Common Procedure Coding System codes, including Common Procedural Terminology codes.
To ensure that we can process your claims and send accurate reimbursements to you as quickly and efficiently as possible, it’s important that you always report the most current HCPCS or CPT codes. You’ll want to check out the 2019 HCPCS Update, which has been posted on web-DENIS for the most recent list of new and deleted procedure codes for 2019. Check out the article in this month’s issue for more details about the 2019 HCPCS Update and how to easily locate it on web-DENIS.
Blue Cross Blue Shield of Michigan works to make sure that ClaimsXten is also aligned with any unique Blue Cross payment policy. Blue Cross reserves the right to make changes or corrections when additional changes are required or new information becomes available. In some instances, changes to ClaimsXten may be applied retroactively.
Battling the opioid epidemic: A roundup of recent news and information
 Suicide, overdose deaths continue to rise, USA Today reports Suicide, overdose deaths continue to rise, USA Today reports
Suicide and drug overdose rates continued to rise in 2017, driving the number of U.S. deaths to the highest total in more than 100 years, USA Today** reported on Nov. 29, 2018. The newspaper based it’s report on a series of reports from the Centers for Disease Control and Prevention. Here are some key statistics:
- Drug overdose deaths among U.S. residents exceeded 70,000 in 2017, nearly 6,600 more than in 2016, according to the CDC.
- In 2017, 47,000 people committed suicide, a rate of 14 per 100,000 people. That’s up from 10.5 in 1999. The total number of suicide deaths was the highest in a half century.
For more details on the CDC report, “Mortality in the United States, 2017,” click here.**
Pharmaceutical manufacturer exploiting opioid crisis, 60 Minutes reports
On Nov. 18, 60 Minutes** aired an investigative piece about the abusive pricing practices of pharmaceutical manufacturer kaléo Inc., which produces EVZIO®, an auto injector that administers naloxone during an opioid overdose. Kaléo has increased the price of the product by more than 600 percent since February 2016 amid the national opioid epidemic. America's Health Insurance Plans, a national association whose members provide coverage for health and health-related services, worked closely with the producers of 60 Minutes to provide extensive educational assistance about out-of-control drug prices, the role of insurance providers in making care and medications accessible, and insights into the relationship among pharmacy benefit managers, insurers and drug manufacturers.
Nearly 11 million pounds of pills collected during Drug Take Back Day
During the 16th National Prescription Drug Take Back Day on Oct. 27, the Drug Enforcement Administration and federal, state and local partners disposed of more than 900,000 pounds of potentially dangerous, unused prescription medications collected at nearly 6,000 sites across the country. These twice-yearly events play a key role in removing opioids and other medications from the country’s homes where they could be stolen or abused by family members and visitors.
As the state’s largest health insurers, Blue Cross Blue Shield of Michigan and Blue Care Network support these events in various ways: through blogs, Twitter chats and resources offered through its Opioids 101 site. Drug take-back events are part of a larger, corporatewide effort to battle the opioid epidemic.
The next Drug Take Back Day is April 27, 2019, so mark your calendar. But your patients don’t need to wait until then to dispose of unwanted prescription drugs. They can find a nearby drug disposal facility by using the DEA’s search tool** or Michigan OPEN’s Opioid Disposal Map.**
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Reminder: New MESSA product takes effect Jan. 1
In a November Record article, we told you that the Michigan Education Special Services Association would be launching a new product effective Jan. 1, 2019, called Essentials by MESSA. It offers premiums and deductibles that are lower than some other MESSA products, made possible by reducing and eliminating some benefits that members have said aren’t crucial to their health care needs.
Because the benefits available under Essentials by MESSA can be significantly different from other MESSA plans, we’d like to remind you to check web-DENIS for benefits before providing services to MESSA members.
Billing chart: Blues highlight medical, benefit policy changes
You’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart.
This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures.
You will also see that descriptions for the codes are no longer included. This is a result of recent negotiations with the AMA on use of the codes.
We will publish information about new BCBS groups or changes to group benefits under the Group Benefit Changes heading.
For more detailed descriptions of the BCBSM policies for these procedures, please check under the Medical/Payment Policy tab in Explainer on web-DENIS. To access this online information:
- Log in to web-DENIS.
- Click on BCBSM Provider Publications & Resources.
- Click on Benefit Policy for a Code.
- Click on Topic.
- Under Topic Criteria, click on the drop-down arrow next to Choose Identifier Type and then click on HCPCS Code.
- Enter the procedure code.
- Click on Finish.
- Click on Search.
| Code* |
BCBSM changes to:
Basic Benefit and Medical Policy, Group
Variations Payment Policy, Guidelines |
| POLICY CLARIFICATIONS |
J3490 |
Basic benefit and medical policy
Aristada Initio (aripiprazole lauroxil)
Effective June 25, 2018, Aristada Initio (aripiprazole lauroxil) is covered for the following FDA-approved indications:
Aristada Initio (aripiprazole lauroxil) is used for the initiation of Aristada (aripiprazole lauroxil), a long-acting injectable atypical antipsychotic for the treatment of schizophrenia in adults. Aristada Initio is only to be used as a single dose to re-initiate Aristada treatment following a missed dose of Aristada. Aristada Initio is administered as an extended-release injectable suspension, 675 mg is provided in a single dose pre-filled syringe.
NDC: 65757050003.
Preauthorization isn't required.
This drug isn’t a benefit for URMBT. |
J3590 |
Basic benefit and medical policy
Palynziq (pegvaliase-pqpz)
Effective May 24, 2018, Palynziq (pegvaliase-pqpz) was
covered for the following FDA-approved indications:
Palynziq (pegvaliase-pqpz) is a phenylalanine-metabolizing enzyme indicated to reduce blood phenylalanine concentrations in adult patients with phenylketonuria who have uncontrolled blood phenylalanine concentrations greater than 600 micromol/L on existing management. The recommended initial dosage is 2.5 mg subcutaneously once weekly for four weeks. Titrate the dosage in a step-wise manner over at least five weeks based on tolerability to achieve a dosage of 20 mg subcutaneously once daily.
NDCs: 68135075620, 68135005890, 68135067340.
Preauthorization isn't required.
This drug isn’t a benefit for URMBT. |
| GROUP BENEFIT CHANGES |
Metro Health Hospital |
Metro Health Hospital, group number 71719, is adding a vision option.
Group number: 71719
Alpha prefix: JXP
Platform: NASCO hybrid
Plans offered:
PPO triple tier medical/surgical (no drugs)
HDHP PPO triple tier medical/surgical (CDH HSA) with drugs
New vision option on MOS platform |

Certain infusion drugs won’t be covered in outpatient hospitals, starting Jan. 1
Here’s important information we communicated Nov. 1 in a web-DENIS message:
Beginning Jan. 1, 2019, Blue Cross Blue Shield of Michigan is adding three preauthorized medical drugs to the site of care requirement for members. Infusions for these drugs won’t be covered at hospital outpatient facilities without prior authorization for an approved location, starting Jan. 1.
The authorization requirement only applies to groups that are currently participating in the commercial Medical Drug Prior Authorization program for drugs administered under the medical benefit. These changes don’t apply to BCN AdvantageSM, Blue Cross Medicare Plus BlueSM PPO or Federal Employee Program® members.
All drugs included in this program already need prior authorization for payment. Approved authorizations will be payable for professional locations, with no further action required:
- Physician’s offices or other health care provider’s offices
- Ambulatory infusion centers
- The member’s home, from a home infusion therapy provider
Members must receive their infusions in a professional office setting, a professional infusion center or in the member’s home.
If your patient currently receives one of these infusions at a hospital outpatient facility:
- Submit a prior authorization request for your patient to Blue Cross for a hospital outpatient facility. If this request isn’t submitted and approved, the patient will be responsible for the full cost of the medicine.
- Find out where your patient can continue his or her infusion therapy. Check the directory of participating home infusion therapy providers and infusion centers. Please confirm network participation for your patient before his or her infusion.
- Tell your patient to contact any of the listed infusion therapy providers. If they’re able to accommodate your patient, they’ll work with you and your patient to make the change easy. We’re also sending this information to your patient.
- Help your patient switch his or her infusion therapy to your office, infusion center or home infusion therapy provider by Jan. 1.
For the ordering provider:
If a member must receive one of these infusions in a hospital outpatient facility, follow the normal steps for a prior authorization request and include:
- The authorization number previously approved
- Rationale that clearly describes the reason the infusion must be administered in a hospital setting
- Supporting chart notes
The medical drugs subject to this requirement include:
HCPCS |
Drug name |
J2786 |
Cinqair® |
J2182 |
Nucala® |
J2357 |
Xolair® |
For more information about hospital outpatient infusion therapy, view previous issues of The Record:
2017
October
December
2018
March
June
Medicare Part B medical specialty drug prior authorization lists changing in 2019
Some updates are coming for the Part B medical specialty medical prior authorization drug list for Blue Cross Medicare Plus BlueSM PPO and BCN AdvantageSM members. These changes include additions and removals from the prior authorization program as follows.
Medicare Plus Blue PPO
Removals — for dates of service starting Jan. 1, 2019:
- J0202 Lemtrada®
- J2323 Tysabri®
- J2350 Ocrevus®
Additions — for dates of service starting Feb. 1, 2019:
- C9036 Onpattro™
- J2840 Kanuma®
- J2860 Sylvant®
- J3357 Stelara® SQ
- J3358 Stelara® IV
- J1746 Trogarzo™
- J9022 Tecentriq®
- J9023 Bavencio®
- J9042 Adcetris®
- J9176 Empliciti®
- J9308 Cyramza®
- J9352 Yondelis®
For Medicare Plus Blue, we require prior authorization for these medications when you bill them on a professional CMS-1500 claim form or by electronic submission via an 837P transaction, for the following sites of care:
- Physician office (place of service code 11)
- Outpatient facility (place of service code 19, 22 or 24)
We don’t require authorization for these medications when you bill them on a facility claim form (such as a UB04) or electronically via an 837I transaction.
BCN Advantage
Removals — for dates of service starting Jan. 1, 2019:
- J9032 Beleodaq®
- J9310 Rituxan®
Additions — for dates of service starting Feb. 1, 2019:
- J2860 Sylvant®
- J3357 Stelara® SQ
- J3358 Stelara® IV
- J3490/C9399 Onpattro™
- J1746 Trogarzo™
- J9022 Tecentriq®
- J9023 Bavencio®
- J9042 Adcetris®
- J9176 Empliciti®
- J9352 Yondelis®
For BCN Advantage, we require prior authorization for these medications when you bill them on a professional CMS-1500 claim form (or submit them electronically via an 837P transaction) or on a facility claim form such as a UB04 (or submit them electronically via an 837I transaction), for the following sites of care:
- Physician office (place of service code 11)
- Outpatient facility (place of service code 19, 22 or 24)
- Home (place of service code 12)
Reminder: You must get authorization prior to administering these medications. Use the NovoLogix® online tool to quickly submit your requests.
Reminder: Update TPA, Provider Authorization Form when making changes to trading partner information
Blue Cross Blue Shield of Michigan is dedicated to safeguarding the protected health information of our members. These safeguards include completion of a Trading Partner Agreement and Provider Authorization Form as part of the electronic data interchange setup process. All EDI trading partners must complete both before they can exchange PHI with Blue Cross.
Terms of the TPA require you to notify Blue Cross of any changes in your trading partner information. You must update your Provider Authorization Form if you send claims using a different submitter ID or route your Electronic Remittance Advice, or 835s, to a different unique receiver or trading partner ID. Updating the form ensures information is routed to the appropriate destination.
Any time you switch vendors, billing services or clearinghouses, you need to update your Provider Authorization Form.
To make changes to your EDI setup:
- Go to bcbsm.com.
- On the homepage, select Providers.
- On the Providers page, select Quick Links under Welcome to Provider Services.
- Click on Electronic Connectivity (EDI) from the list of links and then select How to use EDI to exchange information with us electronically.
- Select Update your Provider Authorization Form in the middle of the page under EDI Agreements.
You should review your provider authorization information if you’ve:
- Joined a new group practice.
- Left a group practice and now bill using your own NPI.
- Hired a new billing service.
- Started submitting claims through a clearinghouse or you’ve changed clearinghouses.
- Decided you no longer want to receive 835 files.
- Selected a new destination for your 835s.
For questions about EDI enrollment, contact our help desk at 1-800-542-0945. For assistance with TPA and Provider Authorization forms, select the TPA option.
Value-based reimbursements will be applied to additional anesthesia time and base modifiers
The value-based reimbursement fee schedule sets fees at greater than 100 percent of the anesthesia maximum payment schedule.
Currently, if an anesthesiologist is eligible to be reimbursed in accordance with the VBR fee schedule, value-based reimbursements are applied to the time and base codes billed by the anesthesiologist with the AA and GC modifiers.
Effective March 1, 2019, value-based reimbursements will also be applied to the time and base codes billed by anesthesiologists with the QK and QY modifiers.
Starting Feb. 1, eviCore managing two radiopharmaceutical drugs
For dates of service on or after Feb. 1, 2019, the following radiopharmaceutical drugs need authorization through eviCore healthcare:
- Lutathera® (lutetium Lu 177 dotatate, HCPCS code A9513)
- Xofigo® (radium Ra 223 dichloride, HCPCS code A9606)
This applies to members covered by:
- Blue Cross Blue Shield of Michigan PPO (commercial) and Blue Cross Medicare Plus BlueSM PPO
Note: Currently, eviCore manages procedures associated with code A9606 for Blue Cross and Medicare Plus Blue members. On Feb. 1, eviCore will begin managing procedures associated with code A9513.
- BCN HMOSM commercial and BCN AdvantageSM
Note: Lutathera was managed for BCN HMO members under the prior authorization program for drugs covered under the medical benefit. Currently, eviCore manages procedures associated with code A9513 (currently C9031) for BCN Advantage members. For BCN HMO members, C codes aren’t payable. However, services associated with the administration of an approved treatment plan with Lutathera are payable for BCN HMO members. On Feb. 1, eviCore will begin managing procedures associated with code A9606 for both BCN HMO and BCN Advantage.
We’ll update the Procedures that require authorization by eviCore healthcare document before the effective date of the change.
Send authorization requests to eviCore online or by telephone at 1-855-774-1317.
Note: These changes don’t apply to MESSA members.
Redesigned Blues Brief available electronically starting January
Our one-page provider and facility newsletter, Blues Brief, will have a new look starting in January. Blues Brief contains brief Blue Cross Blue Shield of Michigan and Blue Care Network articles and is distributed by provider consultants to doctors, specialists and their office staff. Provider offices receive it monthly and facilities quarterly.
The refreshed look will feature a new nameplate, color scheme and icons to identify which articles pertain to individual lines of business. Specialty-specific versions will be created periodically for chiropractic, behavioral health and physical, occupational and speech therapy offices.
We have another new feature — providers can now subscribe to receive Blues Brief electronically. Choose from the monthly physician office version, quarterly hospitals and facilities version and the specialty-specific versions.
To avoid possible subscription errors, add Blues Brief to your subscriptions by clicking the Manage Subscriptions link at the bottom of your BCN Provider News or Record newsletter emails. You can also visit the subscription page to choose your preferred Blues Brief versions.

Blue Cross will start notifying providers on the CMS preclusion list in January
The Centers for Medicare & Medicaid Services adopted a rule in April 2018 that stipulates providers can’t be on a preclusion list and receive payment from a Medicare plan. CMS will make the preclusion list available to Part D sponsors and Medicare Advantage plans, beginning Jan. 1, 2019.
Once Blue Cross Blue Shield of Michigan receives the preclusion list on the first of each month, our Provider Enrollment and Data Management department will send a letter — within 30 days — to any contracted Medicare Plus BlueSM PPO provider who is on the list. The letter will include the effective date of the provider’s preclusion, which will be 90 days from the date of the published preclusion list.
We’re required to remove any contracted provider who is included on the preclusion list from our networks. We’re also required to notify enrollees who have received care in the last 12 months from a contracted provider or a prescription from a provider who is on the preclusion list.
In addition, effective April 1, 2019:
- Part D sponsors will be required to reject a pharmacy claim (or deny a beneficiary request for reimbursement) for a Part D drug that is prescribed by an individual on the preclusion list.
- Medicare Advantage plans will be required to deny payment for a health care item or service given by an individual or entity on the preclusion list.
What is the preclusion list?
The preclusion list is a list of providers and prescribers who are precluded from receiving payment for Medicare Advantage items and services or Part D drugs furnished or prescribed to Medicare beneficiaries. The list was created to replace the Medicare Advantage and prescriber enrollment requirements and to ensure patient protections and to protect the trust funds from prescribers and providers identified as bad actors.
More information is available at the CMS website.**
** Blue Cross Blue Shield of Michigan doesn’t own or control this website.
Coverage for some diabetes drugs changing, starting Jan. 1
Our goal at Blue Cross Blue Shield of Michigan and Blue Care Network is to provide our members with safe, high-quality prescription drugs while also controlling costs. To accomplish this, we’re making coverage changes to some diabetes drugs (see tables below).
To discuss treatment options with their doctors, we’ll let members fill their current prescriptions through Feb. 28, 2019. If members fill their prescriptions on or after March 1, 2019, it will cost more or will no longer be covered.
Members who have an approved prior authorization for any of the drugs listed below can continue to fill their prescriptions until the prior authorization end date, but may have a higher copayment.
Drug that will have a higher copayment, starting Jan. 1, 2019:
Drug class: Insulins |
Nonpreferred drug |
Member cost |
Preferred alternatives |
Basaglar® Kwikpen U-100 |
Nonpreferred brand copayment |
Lantus® (all forms)
Levemir® (all forms)
Toujeo® (all forms)
Tresiba® Flextouch® |
Drugs we won’t cover, starting Jan. 1, 2019:
Drug class: Glucagon-like peptide-1 (GLP-1) receptor agonists |
Excluded drugs |
Member cost starting March 1, 2019 |
Preferred alternatives |
Bydureon® (all forms)
Byetta® |
Full cost |
Ozempic®
Trulicity®
Victoza® |
Drug class: Dipeptidyl peptidase 4 (DPP-4) inhibitors |
Excluded drugs |
Member cost starting March 1, 2019 |
Preferred alternatives |
Alogliptin**
Onglyza®
Nesina® |
Full cost |
Januvia®
Tradjenta® |
Drug class: Dipeptidyl peptidase 4 (DPP-4) inhibitors combinations |
Excluded drugs |
Member cost starting March 1, 2019 |
Preferred alternatives |
Alogliptin/metformin**
Alogliptin/pioglitazone**
Kazano®
Kombiglyze®
Oseni®
Steglujan® |
Full cost |
Glyxambi®
Janumet®
Janumet® XR
Jentadueto®
Jentadueto® XR
Qtern® |
**These aren’t generic drugs. These are considered brand-name drugs and don’t have generic equivalents.
Medicare Part B medical specialty drug prior authorization lists changing in 2019
Some updates are coming for the Part B medical specialty medical prior authorization drug list for Blue Cross Medicare Plus BlueSM PPO and BCN AdvantageSM members. These changes include additions and removals from the prior authorization program as follows.
Medicare Plus Blue PPO
Removals — for dates of service starting Jan. 1, 2019:
- J0202 Lemtrada®
- J2323 Tysabri®
- J2350 Ocrevus®
Additions — for dates of service starting Feb. 1, 2019:
- C9036 Onpattro™
- J2840 Kanuma®
- J2860 Sylvant®
- J3357 Stelara® SQ
- J3358 Stelara® IV
- J1746 Trogarzo™
- J9022 Tecentriq®
- J9023 Bavencio®
- J9042 Adcetris®
- J9176 Empliciti®
- J9308 Cyramza®
- J9352 Yondelis®
For Medicare Plus Blue, we require prior authorization for these medications when you bill them on a professional CMS-1500 claim form or by electronic submission via an 837P transaction, for the following sites of care:
- Physician office (place of service code 11)
- Outpatient facility (place of service code 19, 22 or 24)
We don’t require authorization for these medications when you bill them on a facility claim form (such as a UB04) or electronically via an 837I transaction.
BCN Advantage
Removals — for dates of service starting Jan. 1, 2019:
- J9032 Beleodaq®
- J9310 Rituxan®
Additions — for dates of service starting Feb. 1, 2019:
- J2860 Sylvant®
- J3357 Stelara® SQ
- J3358 Stelara® IV
- J3490/C9399 Onpattro™
- J1746 Trogarzo™
- J9022 Tecentriq®
- J9023 Bavencio®
- J9042 Adcetris®
- J9176 Empliciti®
- J9352 Yondelis®
For BCN Advantage, we require prior authorization for these medications when you bill them on a professional CMS-1500 claim form (or submit them electronically via an 837P transaction) or on a facility claim form such as a UB04 (or submit them electronically via an 837I transaction), for the following sites of care:
- Physician office (place of service code 11)
- Outpatient facility (place of service code 19, 22 or 24)
- Home (place of service code 12)
Reminder: You must get authorization prior to administering these medications. Use the NovoLogix® online tool to quickly submit your requests.
| 
