|
December 2018

Blue Cross Rewards program will help members compare costs while earning e-gift cards
Our members and group customers alike are asking us to help them hold the line on health care costs. In response, we’ve developed the Blue Cross Rewards SM program, which will enable members to shop for care, compare costs and choose health care services to meet their needs. The program will also allow members to potentially reduce their out-of-pocket expenses. We’re providing you with information about the program in case your patients ask about it or you’d like to share this information with them.
Starting in January 2019, Blue Cross Rewards will give 600,000 fully insured commercial PPO group members the chance to earn e-gift cards ranging from $25 to $75 for visiting a cost-effective health care provider location for select, non-emergency procedures. More than 100 imaging and outpatient services will be available for price comparison and incentives, including mammograms, ultrasounds, colonoscopies and MRIs. Click here to see the list of rewardable services.
How do we determine if a service is cost effective? For purposes of this program, it’s considered cost effective if the cost falls within the lowest 30 percent cost range of all claims submitted for a service during the previous year.
How the program works
Once Blue Cross Rewards launches, eligible members can begin reaping its rewards by:
- Logging in to their account at bcbsm.com/get-rewards or through the BCBSM mobile app
- Searching for a reward-eligible procedure or service
- Signing up for the reward
- Choosing a cost-effective in-network provider location with a green trophy symbol
- Making an appointment with that location for the procedure needed
- Once the service is completed at a cost-effective location and the claim has been processed, the member will be notified by email to redeem their e-gift card.
Note: These features will only be viewable by members who are eligible for the program.
Online health services available to Medicare Plus Blue PPO members, starting Jan. 1
Beginning Jan. 1, 2019, our Medicare Plus BlueSM and BCN AdvantageSM plans will offer Blue Cross Online VisitsSM.
Commercial Blue Cross PPO and Blue Care Network HMO members already have this benefit, while the Michigan Public School Employees Retirement System group opted out of this benefit for 2019.
Members who use this benefit can virtually connect with a physician, therapist or other health care provider with a two-way, real-time communication, using a:
- Mobile phone
- Tablet
- Computer with a web camera
- Video conferencing device
This service provides our members with:
- A real-time, alternative way to get treatment for non-emergency care when their doctor is unavailable
- Medical and behavioral health services while traveling (available in all 50 states)
Primary physician or behavioral health copayments will apply.
We encourage members who take advantage of this service to inform their primary care physician of the online visit and share their visit summary with their doctor.
You can let your patients know they can access this benefit or get more information by:
Blue Cross Online Visits is powered by American Well®, an independent company that provides online visits for Blue Cross Blue Shield of Michigan and Blue Care Network members. They aren’t intended to replace a member’s relationship with his or her primary care physician. They’re an alternate way to seek treatment for acute illness when the member’s primary care physician isn’t available or when it isn’t convenient for the member to visit their primary care physician or an urgent care center.
Interested in offering online visits?
If you’re interested in offering online visits for our Medicare Plus Blue members and have the technology to do so, we’ll have the ability to support such visits next year. We’ll be publishing a policy paper in January, outlining our online visit policy and billing codes. The paper will be posted on this page of our website in January.
Survey results: Providers say printed materials are important resource
In July 2018, we requested input about training and education needs from our provider community. We received about 120 responses.
Our key takeaways include:
- Printed materials and publications continue to be an important resource. Basic training on how to find materials is helpful.
- Electronic resources (The Record, BCN Provider News and web-DENIS) are key ways providers and their staff get information. Continue using these methods to share changes and updates.
- Online learning and webinars are convenient ways for providers and their staff to learn. You want us to do more of these.
Following are some of the specific responses to questions.
Question: Which of the following topics would you like to learn more about?
Top answers:
- Patient benefits and eligibility
- Billing basics
- Trouble-shooting claim issues
- Navigating web-DENIS
- Provider manuals
- Medical authorizations
- BlueCard claims and appeals
Question: Which of the following methods of training do you prefer?
Top answers:
- Self-guided online e-learning
- Printed materials
- Live webinars
We appreciate your feedback and would like to thank the providers who took part in the survey.
Battling the opioid epidemic: A roundup of news and information
 Trump signs ‘opioid package’ into law Trump signs ‘opioid package’ into law
On Oct. 24, President Trump signed H.R. 6,** the “Support for Patients and Communities Act,” commonly known as “the opioid package,” into law. The bill contains more than 200 provisions, including those affecting Medicare, Medicaid, commercial health plans and law enforcement. It promises $8.5 billion this year for opioid-related programs. Blue Cross Blue Shield of Michigan and the Blue Cross and Blue Shield Association were very involved in advocacy on this issue.
Surgeon general publishes report on opioid addiction
The surgeon general recently published a report,** Facing Addiction in America: The Surgeon General’s Spotlight on Opioids. It calls for a cultural shift in the way Americans talk about the opioid crisis and recommended actions that can prevent and treat opioid misuse. The surgeon general urges people to:
- Talk about opioid misuse. Have a conversation about preventing drug misuse and overdose.
- Be safe. Only take opioid medications as prescribed, make sure to store medication in a secure place and dispose of unused medication properly.
- Understand pain and talk with your health care provider. Treatments other than opioids can be effective in managing pain.
- Understand that addiction is a chronic disease. With the right treatment and supports, people do recover.
- Be prepared. Get and learn how to use naloxone, an opioid overdose reversing drug.
The report draws upon data from the Centers for Disease Control and Prevention, which indicates that overdose deaths rose by almost 10 percent in 2017 to claim the lives of more than 70,000 Americans, 48,000 of which were attributable to opioids.
For more news and information about the opioid epidemic, see the following articles and columns in the November – December issue of Hospital and Physician Update:
**Blue Cross Blue Shield of Michigan doesn’t own or control this website.
We’re offering prizes to providers who submit feedback about our utilization management services
Your feedback is important to Blue Cross Blue Shield of Michigan and Blue Care Network. That’s why we want to know:
- How satisfied you are with our utilization management services
- How we can improve to better meet your needs
We’re encouraging you to complete the 2018 Utilization Management Survey, and please ask your office colleagues, including physicians, nurses and referral coordinators, to do so as well. Your input will help us evaluate our efforts and determine other improvements to enhance our care management processes.
The survey will be available online through Dec. 31, 2018.
As a token of our appreciation, those who respond and provide their contact information following the survey will be entered in to a drawing to win one of two $250 gift certificates.**
All survey responses must be submitted no later than Dec. 31, 2018, to be eligible for the random drawing.
This drawing is open to all participating Blue Cross and BCN providers. If you don’t wish to participate in the survey but want to be included in the drawing, you may enter by emailing BCNPhysicianSurvey@bcbsm.com with your entry request.
Please include your name, phone number, office name and address. All requests must be emailed no later than Dec. 31, 2018.
If you have any questions, please contact your provider consultant.
**Two winners will be selected in a random drawing at the end of the survey from among all eligible entries. Each of the winners will receive a $250 gift certificate. The drawing will take place approximately one month following the closure of the survey. Participating in the drawing won’t be necessary for providers. The winners will be notified by telephone or email following the drawing.
HCPCS update: Code added
The Centers for Medicare & Medicaid Services has added a HCPCS code. The code, effective date and Blue Cross Blue Shield of Michigan’s coverage decision are below.
Medicine supplementary — Injections
Code |
Change |
Coverage comments |
Effective date |
Q5108 |
Added |
Revision to change effective date of the code from Oct. 1, 2018, to July 12, 2018. |
July 12, 2018 |
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Billing chart: Blues highlight medical, benefit policy changes
You’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart.
This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures.
You will also see that descriptions for the codes are no longer included. This is a result of recent negotiations with the AMA on use of the codes.
We will publish information about new BCBS groups or changes to group benefits under the Group Benefit Changes heading.
For more detailed descriptions of the BCBSM policies for these procedures, please check under the Medical/Payment Policy tab in Explainer on web-DENIS. To access this online information:
- Log in to web-DENIS.
- Click on BCBSM Provider Publications & Resources.
- Click on Benefit Policy for a Code.
- Click on Topic.
- Under Topic Criteria, click on the drop-down arrow next to Choose Identifier Type and then click on HCPCS Code.
- Enter the procedure code.
- Click on Finish.
- Click on Search.
| Code* |
BCBSM changes to:
Basic Benefit and Medical Policy, Group
Variations Payment Policy, Guidelines |
| UPDATES TO PAYABLE PROCEDURES |
81445, 0018U, 0026U (effective Sept. 1, 2018)
81545 (effective March 1, 2017)
81479**
**When reported for an Afirma® test
Not covered:
81479***
***When reported for RosettaGX Reveal® test |
Basic benefit and medical policy
Genetic testing: Molecular markers in fine needles aspirates of the thyroid
The use of either Afirma gene expression classifier or ThyroSeq v3 in fine needle aspirates of thyroid nodules with indeterminate cytologic findings (i.e., Bethesda diagnostic Category III [atypia/follicular lesion of undetermined significance] or Bethesda diagnostic Category IV [follicular neoplasm/suspicion for a follicular neoplasm]) established in patients who have the following characteristics:
- Thyroid nodules without strong clinical or radiologic findings suggestive of malignancy.
- In whom surgical decision-making would be affected by test results.
The use of any of the following types of molecular marker testing or gene variant analysis in fine needle aspirates of thyroid nodules with indeterminate findings (Bethesda diagnostic Category III [atypia/follicular lesion of undetermined significance] or Bethesda diagnostic Category IV [follicular neoplasm/suspicion for a follicular neoplasm]) or suspicious findings (Bethesda diagnostic Category V [suspicious for malignancy]) to rule in malignancy to guide surgical planning for initial resection rather than a two-stage surgical biopsy followed by definitive surgery may be considered established:
- ThyroSeq v3
- ThyraMIR microRNA/ThyGenX
- Afirma BRAF after Afirma gene expression classifier
- Afirma MTC after Afirma gene expression classifier
Gene expression classifiers, genetic variant analysis and molecular marker testing in fine needle aspirates of the thyroid not meeting criteria outlined above, including but not limited to use of RosettaGX Reveal, are considered experimental.
The policy updates are effective Sept. 1, 2018.
Payment policy
It isn’t payable in an office location. Modifiers 26 and TC don’t apply. |
J9039 |
Basic benefit and medical policy
Blincyto (blinatumomab)
Effective March 29, 2018, Blincyto (blinatumomab) is covered for the following FDA-approved indications:
Blincyto is a bispecific CD19-directed CD3 T-cell engager indicated for the treatment of adults and children with:
- B-cell precursor acute lymphoblastic leukemia in first or second complete remission with minimal residual disease greater than or equal to 0.1 percent. This indication is approved under accelerated approval based on MRD response rate and hematological relapse-free survival. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials.
- Relapsed or refractory B-cell precursor acute lymphoblastic leukemia.
The NDC is 55513-160-01. |
| POLICY CLARIFICATIONS |
90672 |
Basic benefit and medical policy
FluMist
FluMist®, procedure code 90672, is payable, effective Sept. 1, 2018.
This change is being implemented to accommodate the Advisory Committee on Immunization Practices’ decision to recommend use of this vaccine for the 2018-19 season. Following are the payable professional providers:
- M.D. and D.O.
- Certified nurse practitioner
- Physician assistant
- Certified nurse midwife
- Urgent care center
- Specialty pharmacy
- Retail health centers
- Retail based pharmacy
- All other retail pharmacies
It’s also payable in a hospice facility setting. |
J0887, J0888 |
Basic benefit and medical policy
Micera
Effective June 7, 2018, Micera is approved for the treatment of anemia associated with chronic kidney disease in adult patients who are currently on dialysis or aren’t on dialysis. It’s also approved for pediatric patients, ages 5 to 17, on hemodialysis who are converting from another erythropoiesis-stimulating agent after their hemoglobin level was stabilized with an ESA. |
J3490, J8499, C9399 |
Basic benefit and medical policy
Macrilen (macimorelin)
Effective July 23, 2018, Macrilen™ (macimorelin) is
covered for the following FDA-approved indications:
Macrilen (macimorelin) for oral solution is a growth hormone secretagogue receptor agonist indicated for the diagnosis of adult growth hormone deficiency.
Recommended dose is 0.5 mg/kg as a single oral dose, after fasting for at least eight hours.
Discontinue therapy with strong CYP3A4 inducers, growth hormones and drugs that affect GH release for an adequate length of time before administering Macrilen (macimorelin).
Adequately replace other hormone deficiencies before administering Macrilen (macimorelin).
Limitations of use:
The safety and diagnostic performance hasn’t been established for subjects with body mass index >40kg/m2.
Pharmacy doesn’t require preauthorization of this drug.
Macrilen (macimorelin) isn’t a benefit for URMBT. |
| GROUP BENEFIT CHANGES |
Android Industries |
Android Industries, group number 71778, is joining Blue Cross Blue Shield of Michigan, effective Jan. 1, 2019.
Group number: 71778
Alpha prefix: PPO (VWV)
Platform: NASCO Flexlink
Plans offered:
PPO, medical/surgical
Prescription drugs |
Avancez LLC |
Avancez LLC, group number 71779, is joining Blue Cross Blue Shield of Michigan, effective Jan. 1, 2019.
Group number: 71779
Alpha prefix: PPO (VWZ)
Platform: NASCO Flexlink
Plans offered:
PPO, medical/surgical
Prescription drugs |
Edw. C. Levy |
Edw. C. Levy, group number 71777, is joining Blue Cross Blue Shield of Michigan, effective Jan. 1, 2019.
Group number: 71777
Alpha prefix: PPO (VWU)
Platform: NASCO Flexlink
Plans offered:
PPO, medical/surgical
Prescription drugs |
McNaughton McKay Electric Company |
McNaughton McKay Electric Company, group number 71380, is joining Blue Cross Blue Shield of Michigan, effective Jan. 1, 2019.
Group number: 71380
Alpha prefixes: PPO (KYA), CMM (KYK)
Platform: NASCO hybrid
Plans offered:
PPO, medical/surgical
Prescription drugs
CDH — HSA |
MidMichigan Health |
MidMichigan Health, group number 71776, is joining Blue Cross Blue Shield of Michigan, effective Jan. 1, 2019.
Group number: 71776
Alpha prefix: PPO (VYJ)
Platform: NASCO Flexlink
Plans offered:
PPO, medical/surgical
CDH — HSA
Note: All provider requests for prior authorizations should be directed to ConnectCare at 989-839-1629 or 1-888-646-2429. |
Tower International Inc. |
Effective Jan. 1, 2019, Tower International Inc., group number 71379, is adding new PPO plans with an HSA. Reference Based Benefits (called the Fair Price Program) will be applied to the following package codes:
Tower International is also removing imaging services from its Reference Based Benefits program, effective Jan. 1, 2019. |
Trinity Health |
Trinity Health, group number 71349, BCN (Grand Rapids) membership is moving to Blue Cross Blue Shield of Michigan PPO, effective Jan. 1, 2019.
Group number: 71349
Alpha prefix: TIY (Michigan members)
Platform: NASCO
Plans offered:
Triple-tier PPO |
TI Group Automotive LLC |
TI Group Automotive LLC, group number 71780, is joining Blue Cross Blue Shield of Michigan, effective Jan. 1, 2019.
Group number: 71780
Alpha prefixes: PPO (ZIO), CMM (ZOO)
Platform: NASCO hybrid
Plans offered:
PPO, medical/surgical
Dental
CDH — HSA |
Veoneer US Inc. |
Veoneer US Inc., group number 71781, is joining Blue Cross Blue Shield of Michigan, effective Jan. 1, 2019.
Group number: 71781
Alpha prefix: PPO (ZRR)
Platform: NASCO hybrid
Plans offered:
PPO, medical/surgical
Prescription drug
Vision
CDH — HSA |

Changes for UAW Retiree Medical Benefits Trust non-Medicare members
Beginning Jan. 1, 2019, the UAW Retiree Medical Benefits Trust Traditional Care Network and PPO plans will transition to the Enhanced Care Plan for non-Medicare UAW hourly auto retirees. This plan offers the same quality with enhanced benefits and services, which will address gaps in coverage for non-Medicare members.
The Enhanced Care Plan, or ECP, features:
- Unlimited office and outpatient visit coverage with a participating primary care physician and a $25 copay
- Unlimited office and outpatient visit coverage with participating specialists and a $35 copay
- Facility clinic fee coverage for office visits
- New health management programs
- Personalized member servicing by HealthGuide
Members will receive new ID cards, which will indicate they are in the Enhanced Care Plan and will feature HealthGuide’s phone number.
The new health management programs include prior authorization for medical oncology and radiation oncology (in addition to the current prior authorization requirement for high-tech radiology through AIM Specialty Health as mentioned in the October Record article). They’ll also feature the new diabetes management program (Fit4D), in-home assessments and a shopper program for MRIs and CT scans. More information on the shopper program can be found in the November Record article.
Specialty drugs will also require prior authorization, which will be administered by Blue Cross Blue Shield of Michigan.
UAW Retiree Medical Benefits Trust members with Medicare will continue with their current TCN plan.
Always be sure to check benefit and eligibility information on web-DENIS. You can also continue to call our provider service phone numbers for assistance. Visit our Contact Us page for more details.
New approach aims to educate and promote appropriate use of evaluation and management codes
Selecting the CPT code that best reflects the complexity of an evaluation and management service is a big challenge for coders. Perhaps that’s why there are more mistakes made with E/M coding than with coding for other services.
To help health care providers and their office staff determine which E/M code appropriately reflects the complexity of a visit, Blue Cross Blue Shield of Michigan has contracted with Change Healthcare to implement its Coding Advisor solution. Change Healthcare reviews the E/M codes billed and other scenarios, such as modifier 25, observation care and nursing facility care, on claims submitted to Blue Cross. The program provides useful data insights to the provider community and works to maximize coding efficiency and accuracy through up-front education, rather than a traditional post-claim review process.
Beginning in the first quarter of 2019, Change Healthcare will reach out by phone or letter to a subset of providers who submit claims to Blue Cross with E/M codes. Coding Advisor will compare the billing of those codes across provider types with their peers through a physician profile. See example of a physician profile below.
Throughout the course of this program, Coding Advisor will continue to monitor billing practices and send updated reports periodically. They may contact your practice to discuss coding variances and to offer one-on-one coding education. All correspondence will be sent to you from Change Healthcare.
If you have any questions, call Change Healthcare Customer Support at 1-844-592-7009, Option 3.
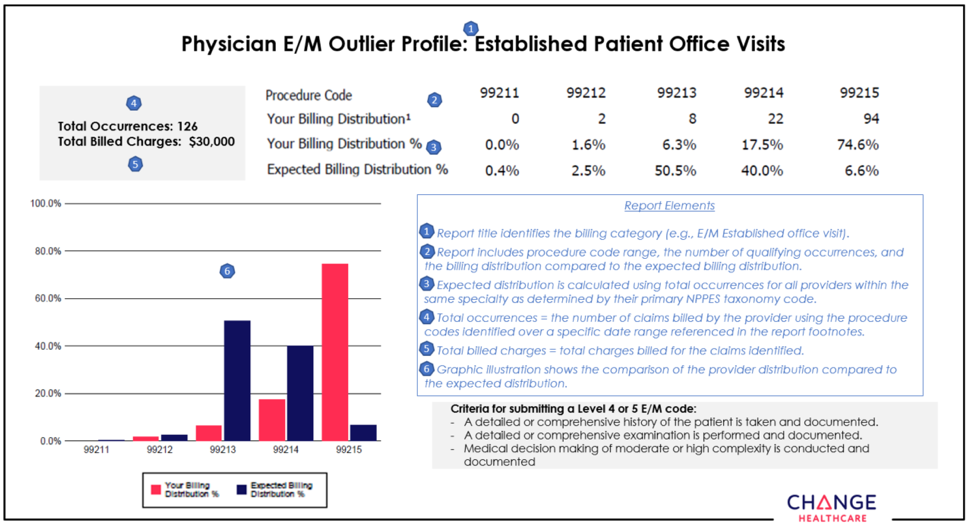
None of the information included in this article is intended to be legal advice and, as such, it remains the health care provider’s responsibility to ensure that all coding and documentation are done in accordance with all applicable state and federal laws and regulations.
Here’s what you need to know about administering the Shingrix® shingles vaccine
Blue Cross Blue Shield of Michigan and Blue Care Network cover Shingrix at zero cost share for most commercial (non-Medicare) members age 50 and older.
Shingrix prevents shingles and its complications and is administered as two injections. The second injection should be administered at least 60 days up to six months after the first injection.
The Centers for Disease Control and Prevention released a monitoring report** in May 2018 indicating that providers may be confusing Shingrix with Zostavax®. The CDC found that from October 2017 to February 2018, the Vaccine Adverse Events Reporting System received 155 reports regarding Shingrix. Of these, 13, or 8 percent, were attributed to administration error.
These errors include:
- Subcutaneous administration rather than intramuscular administration
- Inappropriate age
- Wrong vaccine information statement
- No instructions to return for the second dose
- Administering the wrong vaccine
- Administering without reconstitution of the vaccine
The CDC recommends that healthy adults age 50 and older get Shingrix, even if in the past they:
- Had shingles
- Received Zostavax
- Are not sure if they had chickenpox
Blue Cross and BCN also cover the shingles vaccine Zostavax at zero cost share for most commercial (non-Medicare) members age 60 and older. Shingrix should not be administered less than two months after Zostavax was administered.
Shingrix versus Zostavax
|
Shingrix® |
Zostavax® |
Manufacturer |
GSK |
Merck |
Type |
Recombinant adjuvanted |
Live-attenuated virus |
Storage |
Refrigerator (do not freeze) |
Freezer |
Dosage |
0.5 mL IM x 2 doses
(2-6 months apart) |
0.65 mL SC x 1 dose |
Supply and administration |
Two components:
- Vial one: Single-dose vial of adjuvant suspension component (blue-green cap)
- Vial two: Single-dose vial of lyophilized gE antigen component (brown cap)
Contents in vial one (adjuvant) should be withdrawn and transferred in entirety to vial two (antigen).
Gently shake until powder is completely dissolved. Withdraw 0.5 mL from vial two and administer intramuscularly. |
Single-dose vial of lyophilized vaccine and a vial of sterile water diluent |
ACIP recommendation |
Immunocompetent adults 50 years and older, including those who previously received Zostavax. Shingrix is preferred over Zostavax. |
Immunocompetent adults aged 60 years and older |
Read the Shingrix prescribing information here.
**Blue Cross Blue Shield of Michigan doesn't own or control this website.
We’re excluding some Custom Select drugs, effective Jan. 1, 2019
Our goal at Blue Cross Blue Shield of Michigan and Blue Care Network is to provide our members with safe, high-quality prescription drug therapies. We continually review prescription drugs to provide the best value for our members, control costs and make sure our members are using the right medication for the right situation.
Because there are safe, effective and less-costly alternatives available, we’ll no longer cover some brand-name and generic drugs on the Custom Select Drug List, starting Jan. 1, 2019.
A member whose prescription drug plan uses the Custom Select Drug List will be responsible for the full cost if he or she fills a prescription for one of these drugs on or after Jan. 1, 2019.
For a complete list of covered drugs go to bcbsm.com/pharmacy and click on Drug lists.
Common use |
Drugs to be excluded
Jan. 1, 2019 |
Average cost per unit or package |
Covered generic alternatives |
Average cost
per unit or package |
Allergies |
Xyzal® |
$1 |
These drugs are available over the counter without a prescription. |
Zyrtec®solution |
$3 |
Diabetes |
Actoplus Met® XR |
$13 to $25 |
Actoplus Met® |
$2 |
Fortamet® |
$6 to $11 |
Glucophage®, Glucophage® XR |
<$1 |
Heart conditions |
Lanoxin® 62.5 and 187.5mcg |
$15 |
Lanoxin® 125 mcg, 250 mcg |
<$1 |
HIV |
Crixivan® |
$3 |
Go to bcbsm.com/pharmacy and click on Drug lists for a complete list of covered alternatives.
Members should discuss their treatment options with their doctor. |
Rescriptor® |
$3 |
Trizivir® |
$20 |
Videx® |
$27 |
Videx® EC |
$9 |
Viracept® |
$5 to $12 |
Migraines |
Migranal® nasal spray |
$551 |
Cafergot® |
$15 |
D.H.E. 45® |
$179 |
Generic triptans
(such as Imitrex®, Maxalt®, Zomig®) |
$10 to $20 |
Mood disorders |
Aplenzin® |
$52 to $156 |
Wellbutrin®, Wellbutrin® SR, Wellbutrin® XL |
<$1 |
Muscle relaxants |
Lorzone® |
$9 to $10 |
Flexeril® |
<$1 |
Norflex® |
Parafon Forte DSC® 500 mg |
Robaxin® |
Zanaflex® |
Overactive bladder |
Toviaz® |
$13 |
Detrol®, Detrol® LA |
$2 to $5 |
Ditropan®, Ditropan® XL |
Sanctura®, Sanctura® XR |
Skin conditions
|
Bactroban® cream |
$222 |
Bactroban® ointment |
$6 |
gentamicin cream, ointment |
$50 |
Denavir® |
$975 |
Zovirax® ointment |
$297 |
Desonate® |
$660 |
Dermacort®, Hytone® 2.5% |
$7 to $150 |
Desowen® |
Kenalog® 0.025% cream, lotion |
Valisone® lotion |
Florone®
Psorcon® |
$210 to $932 |
Aristocort®, Kenalog® 0.5% |
$5 to $80 |
Diprolene® cream, lotion |
Diprosone® cream, ointment |
Elocon® ointment |
Valisone® ointment |
Pandel® |
$1,287 |
Diprosone® lotion |
$8 to $100 |
Elocon® cream, lotion, solution |
Kenalog® ointment, spray |
Synalar® ointment |
Westcort® ointment |
Zyclara® |
$1,485 |
Efudex® |
$165 |
Protopic® |
$336 |
We’re changing coverage for some vitamin supplements, effective Jan. 1
Blue Cross and Blue Care Network will no longer cover certain vitamins or nutritional supplements starting Jan. 1, 2019. The vitamins and nutritional supplements listed below will no longer be covered because these products are not approved by the FDA.
Many of these vitamins and nutritional supplements have over-the-counter alternatives that are available without a prescription.
A |
|
H |
|
R |
ACTIVE FE |
|
HEMATINIC PLUS |
|
RENAL CAPS |
ANIMI-3 |
|
HEMATINIC WITH FOLIC ACID |
|
RENA-VITE RX |
AV-PHOS 250 NEUTRAL |
|
HEMATOGEN |
|
RENO CAPS |
B |
|
HEMATOGEN FORTE |
|
S |
BIFERA RX |
|
HEMATRON-AF |
|
SE-TAN PLUS |
C |
|
HEMAX |
|
STROVITE FORTE |
CALCIUM-FOLIC ACID PLUS D |
|
HEMETAB |
|
STROVITE ONE |
CENTRATEX |
|
HEMOCYTE PLUS |
|
T |
CORVITA |
|
HEMOCYTE-F |
|
TANDEM PLUS |
CORVITE FE |
|
I |
|
TARON FORTE |
D |
|
INTEGRA F |
|
THRIVITE-19 |
DIALYVITE |
|
INTEGRA PLUS |
|
TL GARD RX |
DIALYVITE 3000 |
|
IROSPAN |
|
TL-HEM 150 |
DIALYVITE 5000 |
|
K |
|
TL ICON |
DIALYVITE SUPREME D |
|
K-PHOS NEUTRAL |
|
TRICON |
E |
|
M |
|
TRIGELS-F FORTE |
ESCAVITE |
|
MAGNEBIND 400 RX |
|
TRIPHROCAPS |
ESCAVITE D |
|
MULTIGEN FOLIC |
|
TRI-VITAMIN WITH FLUORIDE |
ESCAVITE LQ |
|
MULTIGEN PLUS |
|
V |
F |
|
MULTIVITAMINES-A,B,C,D,E |
|
V-C FORTE |
FEROCON |
|
MULTIVITAMIN W/FLUORIDE & IRON |
|
VI-C FORTE |
FERRALET 90 |
|
MULTIVITAMIN WITH FLUORIDE |
|
VIRT-GARD |
FERRAPLUS 90 |
|
MVC-FLUORIDE |
|
VOL-CARE RX |
FERREX 150 FORTE |
|
MYNEPHROCAPS |
|
VOL-NATE |
FERREX 28 |
|
MYNEPHRON |
|
VOL-TAB RX |
FERROCITE PLUS |
|
N |
|
VIRT-PHOS 250 NEUTRAL |
FLUORABON |
|
NEPHPLEX RX |
|
VIRT-VITE |
FOLBEE |
|
NEPHROCAPS |
|
VIRT-VITE PLUS |
FOCALGIN DSS |
|
NEPHROCAPS QT |
|
VIT 3 |
FOLGARD OS |
|
NEPHRON FA |
|
VITAFOL |
FOLGARD RX |
|
NEPHRO-VITE RX |
|
VITAL-D RX |
FOLIC ACID-CYANCOBAL-PYRIDOXIN |
|
NIVA-PLUS |
|
VITAMINS A,C,D & FLUORIDE |
FOLIVANE-F |
|
P |
|
VOL-PLUS |
FOLIVANE-PLUS |
|
PHOSPHA 250 NEUTRAL |
|
VP-VITE RX |
FOLPLEX 2.2 |
|
PHOSPHOROUS |
|
|
FOLTRATE |
|
POLY-IRON 150 FORTE |
|
|
FORTAVIT |
|
POLY-VI-FLOR |
|
|
FUSION PLUS |
|
POLY-VI-FLOR W/IRON |
|
|
|
|
POLY-VITAMIN WITH FLUORIDE |
|
|
|
|
PUREVIT DUALFE PLUS |
|
|
It's important to understand the difference between ‘home health’ and ‘home infusion’
In practice, you may use the terms “home health” and “home infusion” synonymously. However, when it comes to your patients’ benefits with Blue Cross Blue Shield of Michigan and Blue Care Network, these terms have very different meanings and coverage requirements.
Home health care is a benefit for members who have it as part of their plan and meet specific criteria, including being certified by a doctor as non-ambulatory or homebound. This allows them to receive certain services at home as an alternative to long-term hospital care. These services include skilled nursing, physical therapy, speech therapy, nutritional therapy, occupational therapy and social service guidance.
Some services, including the following, aren’t covered under the home health care benefit.
- Custodial care: This service is for patients in nursing homes, hospice or other facility settings who don’t need skilled medical or nursing care. It’s provided by individuals who aren’t required to have special training. Services include assistance with daily living activities, such as bathing, dressing, shopping, cleaning, cooking and laundry.
- Personal care: This is care given by certified home health aides. Services include bathing, dressing or using the bathroom.
Home infusion, a service that our Site of Care Optimization policy refers to, is an alternative to traveling to a hospital outpatient infusion center or physician’s office to receive certain medications from a health care professional. Home infusion services are included under the Blue Cross and BCN medical benefit. There’s no requirement for your patient to be deemed non-ambulatory or homebound to use a contracted home infusion provider.
Home infusion providers use specially trained nurses that travel to your patients’ homes to administer the medications you’ve prescribed. They’ll also monitor patients throughout the infusion process and for an appropriate amount of time after the infusion has been completed. Home infusion is a safe and convenient way to administer prescription medications.
For more information
- Use web-DENIS to determine whether a member has the home health benefit.
- To learn more about the home health benefit or the Site of Care Optimization policy, review our medical policies by using the Medical Policy & Pre-Cert/Pre-Auth Router.
- For information relating to medical drugs included in the Site of Care Program, follow these steps:
For Blue Cross
- From the web-DENIS homepage, click on BCBSM Provider Publications and Resources.
- Click on Newsletters and Resources.
- Click on Forms.
- Click on Physician administered medications
For BCN
Register for Medicare Advantage webinar: Avastin use for patients with retinal disorders
Learn about the safe and effective use of Avastin® for retinal disorders and how to correctly bill Medicare Plus BlueSM PPO and BCN AdvantageSM for maximum reimbursement.
Register for one of the following webinars now:
Thursday, Dec. 6, 2018, 1 to 1:30 p.m.
Friday, Dec. 7, 2018, 10 to 10:30 a.m.
Once the host approves your registration, you’ll receive a confirmation email with instructions for joining the session.
E-referral system now includes updated authorization criteria and questionnaires
We’ve made updates to the authorization criteria and questionnaires in the e-referral system for the following services:
- Hip replacement surgery procedure, initial
- Hyperbaric oxygen therapy,** outpatient
- Knee replacement surgery, nonunicondylar, initial
- Knee replacement surgery, unicondylar, initial
- Lumbar spine surgery** for adults
- Transcatheter arterial chemoembolization of hepatic tumors, or TACE
- Endometrial ablation**
- Cervical spine surgery with artificial disc replacement**
- Shoulder joint replacement surgery
- Deep brain stimulation
The updated questionnaires are in the e-referral system. We use these criteria and questionnaires when making utilization management determinations for the following members:
- BCN HMOSM
- BCN AdvantageSM
- Blue Cross Medicare Plus BlueSM PPO
**Only applies to BCN HMO and BCN Advantage members.
The updated authorization criteria and preview questionnaires are available at ereferrals.bcbsm.com. Here’s where to find them:
- For BCN documents — From ereferrals.bcbsm.com, click on BCN, then click Authorization Requirements & Criteria. Next, look in the Authorization criteria and preview questionnaires section.
- For Medicare Plus Blue documents — From ereferrals.bcbsm.com, click on Blue Cross, then click Authorization Requirements & Criteria. Next, look in the For Blue Cross Medicare Plus Blue PPO members section.
You can look over the preview questionnaires to see what questions you’ll need to answer in the e-referral system for each service, and then prepare your answers ahead of time. This can cut down on the time it takes to submit the authorization request.
We’re making a change to prior authorization requirement for PPO members
In an October Record article, we told you that you’d need to obtain prior authorization for high-tech radiology, in-lab sleep management and echocardiogram services for all Blue Cross Blue Shield of Michigan PPO members, regardless of where they lived. We’ve subsequently changed our approach and will only require prior authorization for those services for patients who live in Michigan.
The challenge of keeping provider data correct drives improvement initiatives
In 2016, a research group at West Virginia University had a team of secret shoppers pose as patients. They tried to make appointments with 743 primary care physicians listed in the company’s provider directory. They were successful only 30 percent of the time.
Keeping provider data consistently accurate is a challenge for everyone. Demographics, affiliations, locations and specialties change continually. Studies have shown that:
- 2.4 percent of provider demographics change each month
- 30 percent of doctors change their affiliations each year
- 5 percent of doctors change their status each year
In a review of Blue Cross Blue Shield of Michigan’s provider data, we found that many provider groups have more than three locations for a single provider.
As part of our data model, we require one primary location for each group that a provider is affiliated with, regardless of how many addresses there are for that group. Non-primary locations should only be added if patients can make an appointment at that location.
About our data quality improvement initiatives
Over the past two years, Blue Cross Blue Shield of Michigan and its Physician Group Incentive Program’s physician organizations have partnered on programs that improve provider data quality and, subsequently, patient satisfaction when using Find a Doctor.
Our Provider Data Directory Quality program rewards physician organizations for keeping up-to-date provider data. Accuracy results have increased 14 percent overall to an average 68 percent since data quality was assessed in 2017.
Other quality initiatives include the recent pilot of CAQH Direct Assure 2.0, a tool to reconcile CAQH provider data with data in the Blue Cross system. Preliminary results show that alignment has improved by more than 30 percent.
Blue Cross also routinely performs internal analyses on provider data to identify non-essential or non-appointing address data that displays in Find a Doctor.
Room for improvement
While we have many data quality improvement initiatives, we still have a long way to go. We’ve discovered that our non-primary provider location data is out of date and only about 40 to 50 percent accurate.
Over the next few months, we’ll be reviewing data and cleansing non-primary locations. Once complete, you’ll be able to:
- Focus on your primary provider locations.
- Start with a clean slate for non-primary locations.
Rest assured, removal of locations because of this cleanse won’t affect any claims payments.
Playing your part
To improve our data, please continue working with us to keep your demographic information up to date. Use the Provider Enrollment and Self-service tool to make any necessary changes and use CAQH ProView to verify that CAQH has correct location information for you.
While making updates, keep these pointers in mind:
- Minimize the number of locations added for each provider so they’re easier to manage.
- If primary locations for providers don’t take appointments, don’t display them in the directory.
- Additional locations shouldn’t be added to the provider’s profile unless they’re appointment addresses.
- When making CAQH location updates, don’t forget to add the Type 2 National Provider Identifier (NPI 2) and Taxpayer Identification Number.
If you have any questions about the information in this article, reach out to Sarah Aly, Team Leader II, Provider Ops & Innovation, at saly@bcbsm.com.
We’ll grant board certification exceptions for certain PCMH providers
Blue Cross Blue Shield of Michigan will continue to verify board certification statuses of practitioners in our Blue Cross and Blue Care Network managed care networks.
Effective Jan. 1, 2019, Blue Cross will annually review the board certification status of family medicine, internal medicine and pediatric practitioners. If their board certification status has lapsed and they are a designated Patient-Centered Medical Home physician, we’ll grant an exception and allow the practitioner to remain in our Blue Cross and BCN managed care networks.
This exception doesn’t apply to new practitioner enrollments. Blue Cross and BCN will continue to require all practitioners to have board certification upon initial enrollment for affiliation with us.
Non-board-certified family and internal medicine and pediatric practitioners who don’t have PCMH designation will be required to complete their applicable specialty’s Maintenance of Certification requirements within a two-year time frame. Failure to meet these requirements will result in termination from our managed care networks.
GM to offer new PPO plan option — ConnectedCare: Henry Ford Health System — in January
Effective Jan. 1, 2019, General Motors will offer a new PPO medical plan option for select salaried employees and eligible dependents in the Detroit area. Called ConnectedCare: Henry Ford Health System, it includes medical, surgical and hearing services. As reported in the billing chart in the September Record, it’s not affiliated with BCN AdvantageSM ConnectedCare.
Members’ ID cards will indicate they’re with General Motors and in the PPO plan called ConnectedCare: Henry Ford Health System. The group number is 83640.
The plan option features two benefit levels.
- Level 1 — Providers in the Henry Ford Health System
- Level 2 — All other providers
Blue Cross Blue Shield of Michigan will serve as the third-party administrator of benefits for this plan option. As always, you can check web-DENIS for information about benefits and eligibility for your patients.
Blue Cross Blue Shield of Michigan to cover mental health and substance abuse benefits for some GM members as of Jan. 1
Starting Jan. 1, 2019, Blue Cross and New Directions will manage the behavioral health and substance abuse benefits for General Motors enrollees who have a Health Savings Account. (These are members in group number 83640 or 83650.)
New Directions will be responsible for prior authorizations, as well as approvals and denials of all behavioral health and substance abuse admissions and select outpatient services. GM enrollees who are affected by this change will receive new ID cards with the appropriate phone numbers.
As always, be sure to check your patients’ ID cards and web-DENIS for eligibility and prior authorization information.
Clarification: Telephone sessions as part of telemedicine for behavioral health providers
Some of our participating psychologists and other psychotherapy practitioners have asked whether they can bill Blue Cross Blue Shield of Michigan for audio-only encounters. We want to let you know that an audio-only encounter is payable. Blue Cross medical policy does not require a visual component to telemedicine provided by psychotherapy practitioners.
These encounters are payable if they comply with CPT rules and Blue Cross medical policy. Psychologists and other psychotherapy practitioners may use the CPT codes that are within their scope of practice once the service has been delivered and they’re able to satisfy the documentation requirements of those codes.
Keep in mind that sessions involving a Blue Cross member must:
- Be synchronous — conducted in real time
- Utilize procedures that are within your scope of practice
- Meet documentation requirements for procedure codes reported
When submitting a claim for a telemedicine session, report the appropriate procedure code and place-of-service code 02. Code 02 identifies the service as telemedicine. You should also use modifier 95 or GT to indicate a real-time audiovisual encounter. (Modifiers 95 and GT should not be used for audio-only telemedicine encounters.)
The following codes don’t require a modifier as they’re specific to a telephone (audio only) evaluation and management or assessment and management service: *99441, *99442, *99443, *98966, *98967 and *98968.
- Codes *99441, *99442 and *99443 are used by M.D.s, D.O.s, nurse practitioners and physician assistants who deliver evaluation and management services.
- Codes *98966, *98967 and *98968 are used by qualified non-physician health care professionals, including psychologists and clinical social workers and other psychotherapy practitioners who deliver assessment and management services.
These codes have specific inclusions and exclusions in their nomenclature so be sure to check your CPT code book for details.
Notes:
- Even though this article is targeted to behavioral health specialists, the information is applicable to all providers within their scope of practice.
- Blue Care Network doesn’t reimburse health care providers for telephone-only sessions.
For more details, see the Blue Cross telemedicine policy and the BCN telemedicine policy.
Here are guidelines for billing medical drugs correctly
About National Drug Code quantities and conversions
See the June 2016 Record for information on calculating and billing National Drug Code quantities and tips on billing electronically. For information on a tool you can use to quickly and easily convert HCPCS or CPT units to NDC units, see the September 2017 Record.
Here are some general guidelines for billing injectable drugs:
- Use the appropriate HCPCS code based on code descriptor.
- Not-otherwise-classified codes should only be reported for drugs that don’t have a valid HCPCS code, which describes the drug being administered.
- Units of drugs must be accurately reported in terms of dosage specified in the HCPCS descriptor and the NDC descriptor.
- Hemophilia factor is an exception; follow current guidelines.
- If there’s no expense to the physician for the drug, don’t bill for it.
- Don’t bill units based on the way the drug is packaged, stored or stocked.
- Don’t bill for the full amount of a drug when it’s been split between two or more patients. Only bill for the amount given to each patient.
- Documentation in the patient’s medical record must indicate the drug and dosage.
Before you fill out the claim form to bill for a medical drug, you need the following:
- Amount of drug administered
- Procedure code
- Number of CPT or HCPCS units
- NDC number
- Number of NDC units
- NDC unit of measure
Here are some reporting examples:
Example 1: HCPCS description or billable units of drug is 6 mg.
6 mg. are administered = 1 unit is billed
Example 2: HCPCS description or billable units of drug is 50 mg.
200 mg. are administered = 4 units are billed
Example 3: HCPCS description or billable units of drug is 1 mg.
10 mg. vial of drug is administered = 10 units are billed
Procedure |
Procedure code billable units** |
Dose example |
HCPCS quantity (for dose example |
NDC code |
NDC billable units** |
NDC quantity (for dose example) |
90670 |
0.5 ML |
0.5 ML |
1 |
00005197101 |
ML |
ML0.5 |
90715 |
0.5 ML |
0.5 ML |
1 |
49281040010 |
ML |
ML0.5 |
J0129 |
10 mg |
250 mg |
25 |
00003218710 |
UN |
UN1 |
J0585 |
1 UN |
200 |
200 |
00023114501 |
UN |
UN2 |
J0696 |
250 mg |
250 mg |
1 |
00143985701 |
Determine by product used: If a powder needs to be reconstituted, then use UN; if an oral tablet, then use UN; if liquid in vial, then use ML. |
UN0.25 |
J0897 |
1 mg |
120 mg |
120 |
55513073001 |
ML |
ML1.7 |
J1569 |
500mg |
10,000 mg |
20 |
00944270002 |
Determine by product used: If a powder that needs to be reconstituted, then use UN; if an oral tablet, then use UN: if liquid in vial, then use ML. |
ML100 |
J1572 |
500 mg |
10,000 mg |
20 |
61953000400 |
ML |
ML200 |
J1745 |
10 mg |
1,100 mg |
110 |
57894003001 |
UN |
UN11 |
J1885 |
15 mg |
30 mg |
2 |
00409379301 |
ML |
ML2 |
J2357 |
5 mg |
150 mg |
30 |
50242004062 |
UN |
UN1 |
J3262 |
1 mg |
200 mg |
200 |
50242013501 |
ML |
ML10 |
J3301 |
10 mg |
20 mg |
2 |
00003029320 |
ML |
ML0.5 |
J3380 |
1 mg |
300 mg |
300 |
64764030020 |
UN |
UN1 |
J3420 |
1000 mcg |
2000 mcg |
2 |
00143961901 |
ML |
ML2 |
**Billable units can be found on the Injections Minimum Fee Schedule on web-DENIS.
Some medical benefit drugs for Medicare Advantage members need step therapy, starting Jan. 1
In the new year, according to Centers for Medicare & Medicaid Services’ guidance, certain Medicare Part B specialty drugs will have additional step therapy authorization requirements. This will apply to Medicare Plus BlueSM PPO and BCN AdvantageSM members for dates of service on or after Jan. 1, 2019.
Step therapy is treatment for a medical condition that starts with the most preferred drug therapy and progresses to other drug therapies only if necessary. The goal of step therapy is to encourage better clinical decision-making.
Some examples of drugs that require step therapy are:
- Botox® for migraines and over active bladder
- Eylea®, Lucentis® and Macugen® for neovascular age-related macular edema
- Prolia® for osteoporosis
What’s changing?
For drugs requiring step therapy, authorization request questions will be different from the ones you currently answer.
Use NovoLogix® to submit authorization requests
We encourage you to send prior authorization requests for Medicare Part B specialty drugs through the NovoLogix web tool via Provider Secured Services. It’s the most efficient way to get a determination.
FEP provides support for pregnant mothers and families through wellness programs
The Blue Cross and Blue Shield Federal Employee Program® offers support and rewards to pregnant members and those with young children through two programs: the Pregnancy Care Incentive Program and Health Families.
The Pregnancy Care Incentive Program encourages pregnant mothers to receive timely prenatal care throughout their pregnancy and make healthy choices to keep themselves and their babies well. The program offers support and incentives during each stage of pregnancy. Eligible members can earn rewards toward a health account to be used for qualified expenses.
As soon as a child is born, FEP members can take advantage of the Healthy Families programs. These programs support healthy lifestyle habits and address such topics as:
- Vaccination schedules
- Well-child visits
- Weight management strategies
For more information, direct members to fepblue.org. The website offers details on both the Pregnancy Care Incentive Program and the Healthy Families programs under the Wellness Resources & Tools tab. Members can also call Customer Service at 1-800-482-3600.
Reminder: Updates to PPO professional claims editing process coming in December
In the September 2018 Record, we let you know that Blue Cross Blue Shield of Michigan will update its claims editing processes for select groups in December 2018. The initial implementation will apply to professional claims, including durable medical equipment, prosthetics and orthotics, and medical supplies. The outpatient facility implementation will take place in the second quarter in 2019.
These updates will make our claims payment system easier for you and your billing staff to navigate. Unique clinical editing reason codes will appear on the 835 response files or provider vouchers.
As a reminder, when billing PPO claims, you should follow guidelines from:
- The American Medical Association’s Current Procedural Terminology code set regarding:
- Correct modifier usage
- Evaluation and management reporting guidelines
- National bundling edits
- National specialty societies, such as:
- American College of Surgeons
- American College of Radiology
- American Association of Neuromuscular and Electrodiagnostic Medicine
- American Cancer Society
As part of your contract with us, health care providers affiliated with the PPO network agree to supply services to Blue Cross members and bill according to guidelines and requirements set by the American Medical Association and select specialty societies.

Changes for UAW Retiree Medical Benefits Trust non-Medicare members
Beginning Jan. 1, 2019, the UAW Retiree Medical Benefits Trust Traditional Care Network and PPO plans will transition to the Enhanced Care Plan for non-Medicare UAW hourly auto retirees. This plan offers the same quality with enhanced benefits and services, which will address gaps in coverage for non-Medicare members.
The Enhanced Care Plan, or ECP, features:
- Unlimited office and outpatient visit coverage with a participating primary care physician and a $25 copay
- Unlimited office and outpatient visit coverage with participating specialists and a $35 copay
- Facility clinic fee coverage for office visits
- New health management programs
- Personalized member servicing by HealthGuide
Members will receive new ID cards, which will indicate they are in the Enhanced Care Plan and will feature HealthGuide’s phone number.
The new health management programs include prior authorization for medical oncology and radiation oncology (in addition to the current prior authorization requirement for high-tech radiology through AIM Specialty Health as mentioned in the October Record article). They’ll also feature the new diabetes management program (Fit4D), in-home assessments and a shopper program for MRIs and CT scans. More information on the shopper program can be found in the November Record article.
Specialty drugs will also require prior authorization, which will be administered by Blue Cross Blue Shield of Michigan.
UAW Retiree Medical Benefits Trust members with Medicare will continue with their current TCN plan.
Always be sure to check benefit and eligibility information on web-DENIS. You can also continue to call our provider service phone numbers for assistance. Visit our Contact Us page for more details.
URMBT members with Medicare Plus Blue to receive fifth-level hospice services
Beginning Jan. 1, 2019, UAW Retiree Medical Benefits Trust, or URMBT, members with Medicare Plus BlueSM will be eligible to receive fifth-level hospice benefits. These benefits are currently offered under the Traditional Care Network (TCN) plan, which provides supplemental coverage for Medicare-eligible URMBT members.
Fifth-level hospice care benefits cover inpatient room and board in a skilled nursing facility. Members would be responsible for any deductibles or coinsurance. There’s a lifetime maximum of 210 days of coverage for fifth-level care.
The hospice agency, not the skilled nursing facility, should bill Blue Cross Blue Shield of Michigan for room and board, using revenue code 0658. Only hospice providers are eligible for payment from Blue Cross. Hospice providers should remember to bill original Medicare for all other hospice services.
Members shouldn’t be billed directly. If you have any questions about submitting claims, see your Medicare Plus Blue PPO Manual.
For more details on fifth-level hospice services, see the hospice section of the Medicare Plus Blue PPO Manual.
Register for Medicare Advantage webinar: Avastin use for patients with retinal disorders
Learn about the safe and effective use of Avastin® for retinal disorders and how to correctly bill Medicare Plus BlueSM PPO and BCN AdvantageSM for maximum reimbursement.
Register for one of the following webinars now:
Thursday, Dec. 6, 2018, 1 to 1:30 p.m.
Friday, Dec. 7, 2018, 10 to 10:30 a.m.
Once the host approves your registration, you’ll receive a confirmation email with instructions for joining the session.
E-referral system now includes updated authorization criteria and questionnaires
We’ve made updates to the authorization criteria and questionnaires in the e-referral system for the following services:
- Hip replacement surgery procedure, initial
- Hyperbaric oxygen therapy,** outpatient
- Knee replacement surgery, nonunicondylar, initial
- Knee replacement surgery, unicondylar, initial
- Lumbar spine surgery** for adults
- Transcatheter arterial chemoembolization of hepatic tumors, or TACE
- Endometrial ablation**
- Cervical spine surgery with artificial disc replacement**
- Shoulder joint replacement surgery
- Deep brain stimulation
The updated questionnaires are in the e-referral system. We use these criteria and questionnaires when making utilization management determinations for the following members:
- BCN HMOSM
- BCN AdvantageSM
- Blue Cross Medicare Plus BlueSM PPO
**Only applies to BCN HMO and BCN Advantage members.
The updated authorization criteria and preview questionnaires are available at ereferrals.bcbsm.com. Here’s where to find them:
- For BCN documents — From ereferrals.bcbsm.com, click on BCN, then click Authorization Requirements & Criteria. Next, look in the Authorization criteria and preview questionnaires section.
- For Medicare Plus Blue documents — From ereferrals.bcbsm.com, click on Blue Cross, then click Authorization Requirements & Criteria. Next, look in the For Blue Cross Medicare Plus Blue PPO members section.
You can look over the preview questionnaires to see what questions you’ll need to answer in the e-referral system for each service, and then prepare your answers ahead of time. This can cut down on the time it takes to submit the authorization request.
GM to offer new PPO plan option — ConnectedCare: Henry Ford Health System — in January
Effective Jan. 1, 2019, General Motors will offer a new PPO medical plan option for select salaried employees and eligible dependents in the Detroit area. Called ConnectedCare: Henry Ford Health System, it includes medical, surgical and hearing services. As reported in the billing chart in the September Record, it’s not affiliated with BCN AdvantageSM ConnectedCare.
Members’ ID cards will indicate they’re with General Motors and in the PPO plan called ConnectedCare: Henry Ford Health System. The group number is 83640.
The plan option features two benefit levels.
- Level 1 — Providers in the Henry Ford Health System
- Level 2 — All other providers
Blue Cross Blue Shield of Michigan will serve as the third-party administrator of benefits for this plan option. As always, you can check web-DENIS for information about benefits and eligibility for your patients.
Some medical benefit drugs for Medicare Advantage members need step therapy, starting Jan. 1
In the new year, according to Centers for Medicare & Medicaid Services’ guidance, certain Medicare Part B specialty drugs will have additional step therapy authorization requirements. This will apply to Medicare Plus BlueSM PPO and BCN AdvantageSM members for dates of service on or after Jan. 1, 2019.
Step therapy is treatment for a medical condition that starts with the most preferred drug therapy and progresses to other drug therapies only if necessary. The goal of step therapy is to encourage better clinical decision-making.
Some examples of drugs that require step therapy are:
- Botox® for migraines and over active bladder
- Eylea®, Lucentis® and Macugen® for neovascular age-related macular edema
- Prolia® for osteoporosis
What’s changing?
For drugs requiring step therapy, authorization request questions will be different from the ones you currently answer.
Use NovoLogix® to submit authorization requests
We encourage you to send prior authorization requests for Medicare Part B specialty drugs through the NovoLogix web tool via Provider Secured Services. It’s the most efficient way to get a determination.
Reminder: Updates to PPO professional claims editing process coming in December
In the September 2018 Record, we let you know that Blue Cross Blue Shield of Michigan will update its claims editing processes for select groups in December 2018. The initial implementation will apply to professional claims, including durable medical equipment, prosthetics and orthotics, and medical supplies. The outpatient facility implementation will take place in the second quarter in 2019.
These updates will make our claims payment system easier for you and your billing staff to navigate. Unique clinical editing reason codes will appear on the 835 response files or provider vouchers.
As a reminder, when billing PPO claims, you should follow guidelines from:
- The American Medical Association’s Current Procedural Terminology code set regarding:
- Correct modifier usage
- Evaluation and management reporting guidelines
- National bundling edits
- National specialty societies, such as:
- American College of Surgeons
- American College of Radiology
- American Association of Neuromuscular and Electrodiagnostic Medicine
- American Cancer Society
As part of your contract with us, health care providers affiliated with the PPO network agree to supply services to Blue Cross members and bill according to guidelines and requirements set by the American Medical Association and select specialty societies.

ESI to be Michigan retail pharmacy network manager for our commercial business, starting Jan. 1, 2019
Blue Cross Blue Shield of Michigan and Blue Care Network are launching a new relationship with Express Scripts, or ESI, as our Michigan retail pharmacy network manager for our commercial business, starting Jan. 1, 2019. We’re making the change to remain as competitive as possible and to help make our integrated pharmacy benefit more affordable for customers. This change does not affect your patients’ pharmacy benefits.
Blue Cross already contracts with ESI for our out-of-state and Medicare Advantage pharmacy network management. ESI contracts with other Michigan health plans as well.
ESI manages a broad network in Michigan that’s nearly identical to Blue Cross’ existing network. Here are some key details:
- More than 99.9 percent of Michigan pharmacies already belong to an ESI network arrangement for other Michigan health plans and accept ESI’s reimbursement arrangement for other Michigan health plans.
- There are 2,400 pharmacies in the Blue Cross and BCN pharmacy network and all but approximately 30 belong to the National Plus pharmacy network managed by ESI. We will ensure that they’re offered an opportunity to join the ESI National Plus network.
- ESI pharmacy network management does not affect our members’ prescription drug benefit design. As they do today, prescription benefits will continue to depend on a group’s benefit design selection.
This change is in direct response to customer needs and designed to deliver significant savings to our customers while maintaining access to a large network of pharmacies. Our customers and members have expressed concerns about the ever-increasing costs of prescription drugs. Helping to lower these costs through effective pharmacy benefit management is key to keeping employer-sponsored and individual health coverage affordable.
Here’s what you need to know about administering the Shingrix® shingles vaccine
Blue Cross Blue Shield of Michigan and Blue Care Network cover Shingrix at zero cost share for most commercial (non-Medicare) members age 50 and older.
Shingrix prevents shingles and its complications and is administered as two injections. The second injection should be administered at least 60 days up to six months after the first injection.
The Centers for Disease Control and Prevention released a monitoring report** in May 2018 indicating that providers may be confusing Shingrix with Zostavax®. The CDC found that from October 2017 to February 2018, the Vaccine Adverse Events Reporting System received 155 reports regarding Shingrix. Of these, 13, or 8 percent, were attributed to administration error.
These errors include:
- Subcutaneous administration rather than intramuscular administration
- Inappropriate age
- Wrong vaccine information statement
- No instructions to return for the second dose
- Administering the wrong vaccine
- Administering without reconstitution of the vaccine
The CDC recommends that healthy adults age 50 and older get Shingrix, even if in the past they:
- Had shingles
- Received Zostavax
- Are not sure if they had chickenpox
Blue Cross and BCN also cover the shingles vaccine Zostavax at zero cost share for most commercial (non-Medicare) members age 60 and older. Shingrix should not be administered less than two months after Zostavax was administered.
Shingrix versus Zostavax
|
Shingrix® |
Zostavax® |
Manufacturer |
GSK |
Merck |
Type |
Recombinant adjuvanted |
Live-attenuated virus |
Storage |
Refrigerator (do not freeze) |
Freezer |
Dosage |
0.5 mL IM x 2 doses
(2-6 months apart) |
0.65 mL SC x 1 dose |
Supply and administration |
Two components:
- Vial one: Single-dose vial of adjuvant suspension component (blue-green cap)
- Vial two: Single-dose vial of lyophilized gE antigen component (brown cap)
Contents in vial one (adjuvant) should be withdrawn and transferred in entirety to vial two (antigen).
Gently shake until powder is completely dissolved. Withdraw 0.5 mL from vial two and administer intramuscularly. |
Single-dose vial of lyophilized vaccine and a vial of sterile water diluent |
ACIP recommendation |
Immunocompetent adults 50 years and older, including those who previously received Zostavax. Shingrix is preferred over Zostavax. |
Immunocompetent adults aged 60 years and older |
Read the Shingrix prescribing information here.
**Blue Cross Blue Shield of Michigan doesn't own or control this website.
We’re excluding some Custom Select drugs, effective Jan. 1, 2019
Our goal at Blue Cross Blue Shield of Michigan and Blue Care Network is to provide our members with safe, high-quality prescription drug therapies. We continually review prescription drugs to provide the best value for our members, control costs and make sure our members are using the right medication for the right situation.
Because there are safe, effective and less-costly alternatives available, we’ll no longer cover some brand-name and generic drugs on the Custom Select Drug List, starting Jan. 1, 2019.
A member whose prescription drug plan uses the Custom Select Drug List will be responsible for the full cost if he or she fills a prescription for one of these drugs on or after Jan. 1, 2019.
For a complete list of covered drugs go to bcbsm.com/pharmacy and click on Drug lists.
Common use |
Drugs to be excluded
Jan. 1, 2019 |
Average cost per unit or package |
Covered generic alternatives |
Average cost
per unit or package |
Allergies |
Xyzal® |
$1 |
These drugs are available over the counter without a prescription. |
Zyrtec®solution |
$3 |
Diabetes |
Actoplus Met® XR |
$13 to $25 |
Actoplus Met® |
$2 |
Fortamet® |
$6 to $11 |
Glucophage®, Glucophage® XR |
<$1 |
Heart conditions |
Lanoxin® 62.5 and 187.5mcg |
$15 |
Lanoxin® 125 mcg, 250 mcg |
<$1 |
HIV |
Crixivan® |
$3 |
Go to bcbsm.com/pharmacy and click on Drug lists for a complete list of covered alternatives.
Members should discuss their treatment options with their doctor. |
Rescriptor® |
$3 |
Trizivir® |
$20 |
Videx® |
$27 |
Videx® EC |
$9 |
Viracept® |
$5 to $12 |
Migraines |
Migranal® nasal spray |
$551 |
Cafergot® |
$15 |
D.H.E. 45® |
$179 |
Generic triptans
(such as Imitrex®, Maxalt®, Zomig®) |
$10 to $20 |
Mood disorders |
Aplenzin® |
$52 to $156 |
Wellbutrin®, Wellbutrin® SR, Wellbutrin® XL |
<$1 |
Muscle relaxants |
Lorzone® |
$9 to $10 |
Flexeril® |
<$1 |
Norflex® |
Parafon Forte DSC® 500 mg |
Robaxin® |
Zanaflex® |
Overactive bladder |
Toviaz® |
$13 |
Detrol®, Detrol® LA |
$2 to $5 |
Ditropan®, Ditropan® XL |
Sanctura®, Sanctura® XR |
Skin conditions
|
Bactroban® cream |
$222 |
Bactroban® ointment |
$6 |
gentamicin cream, ointment |
$50 |
Denavir® |
$975 |
Zovirax® ointment |
$297 |
Desonate® |
$660 |
Dermacort®, Hytone® 2.5% |
$7 to $150 |
Desowen® |
Kenalog® 0.025% cream, lotion |
Valisone® lotion |
Florone®
Psorcon® |
$210 to $932 |
Aristocort®, Kenalog® 0.5% |
$5 to $80 |
Diprolene® cream, lotion |
Diprosone® cream, ointment |
Elocon® ointment |
Valisone® ointment |
Pandel® |
$1,287 |
Diprosone® lotion |
$8 to $100 |
Elocon® cream, lotion, solution |
Kenalog® ointment, spray |
Synalar® ointment |
Westcort® ointment |
Zyclara® |
$1,485 |
Efudex® |
$165 |
Protopic® |
$336 |
We’re changing coverage for some vitamin supplements, effective Jan. 1
Blue Cross and Blue Care Network will no longer cover certain vitamins or nutritional supplements starting Jan. 1, 2019. The vitamins and nutritional supplements listed below will no longer be covered because these products are not approved by the FDA.
Many of these vitamins and nutritional supplements have over-the-counter alternatives that are available without a prescription.
A |
|
H |
|
R |
ACTIVE FE |
|
HEMATINIC PLUS |
|
RENAL CAPS |
ANIMI-3 |
|
HEMATINIC WITH FOLIC ACID |
|
RENA-VITE RX |
AV-PHOS 250 NEUTRAL |
|
HEMATOGEN |
|
RENO CAPS |
B |
|
HEMATOGEN FORTE |
|
S |
BIFERA RX |
|
HEMATRON-AF |
|
SE-TAN PLUS |
C |
|
HEMAX |
|
STROVITE FORTE |
CALCIUM-FOLIC ACID PLUS D |
|
HEMETAB |
|
STROVITE ONE |
CENTRATEX |
|
HEMOCYTE PLUS |
|
T |
CORVITA |
|
HEMOCYTE-F |
|
TANDEM PLUS |
CORVITE FE |
|
I |
|
TARON FORTE |
D |
|
INTEGRA F |
|
THRIVITE-19 |
DIALYVITE |
|
INTEGRA PLUS |
|
TL GARD RX |
DIALYVITE 3000 |
|
IROSPAN |
|
TL-HEM 150 |
DIALYVITE 5000 |
|
K |
|
TL ICON |
DIALYVITE SUPREME D |
|
K-PHOS NEUTRAL |
|
TRICON |
E |
|
M |
|
TRIGELS-F FORTE |
ESCAVITE |
|
MAGNEBIND 400 RX |
|
TRIPHROCAPS |
ESCAVITE D |
|
MULTIGEN FOLIC |
|
TRI-VITAMIN WITH FLUORIDE |
ESCAVITE LQ |
|
MULTIGEN PLUS |
|
V |
F |
|
MULTIVITAMINES-A,B,C,D,E |
|
V-C FORTE |
FEROCON |
|
MULTIVITAMIN W/FLUORIDE & IRON |
|
VI-C FORTE |
FERRALET 90 |
|
MULTIVITAMIN WITH FLUORIDE |
|
VIRT-GARD |
FERRAPLUS 90 |
|
MVC-FLUORIDE |
|
VOL-CARE RX |
FERREX 150 FORTE |
|
MYNEPHROCAPS |
|
VOL-NATE |
FERREX 28 |
|
MYNEPHRON |
|
VOL-TAB RX |
FERROCITE PLUS |
|
N |
|
VIRT-PHOS 250 NEUTRAL |
FLUORABON |
|
NEPHPLEX RX |
|
VIRT-VITE |
FOLBEE |
|
NEPHROCAPS |
|
VIRT-VITE PLUS |
FOCALGIN DSS |
|
NEPHROCAPS QT |
|
VIT 3 |
FOLGARD OS |
|
NEPHRON FA |
|
VITAFOL |
FOLGARD RX |
|
NEPHRO-VITE RX |
|
VITAL-D RX |
FOLIC ACID-CYANCOBAL-PYRIDOXIN |
|
NIVA-PLUS |
|
VITAMINS A,C,D & FLUORIDE |
FOLIVANE-F |
|
P |
|
VOL-PLUS |
FOLIVANE-PLUS |
|
PHOSPHA 250 NEUTRAL |
|
VP-VITE RX |
FOLPLEX 2.2 |
|
PHOSPHOROUS |
|
|
FOLTRATE |
|
POLY-IRON 150 FORTE |
|
|
FORTAVIT |
|
POLY-VI-FLOR |
|
|
FUSION PLUS |
|
POLY-VI-FLOR W/IRON |
|
|
|
|
POLY-VITAMIN WITH FLUORIDE |
|
|
|
|
PUREVIT DUALFE PLUS |
|
|
Register for Medicare Advantage webinar: Avastin use for patients with retinal disorders
Learn about the safe and effective use of Avastin® for retinal disorders and how to correctly bill Medicare Plus BlueSM PPO and BCN AdvantageSM for maximum reimbursement.
Register for one of the following webinars now:
Thursday, Dec. 6, 2018, 1 to 1:30 p.m.
Friday, Dec. 7, 2018, 10 to 10:30 a.m.
Once the host approves your registration, you’ll receive a confirmation email with instructions for joining the session.
Some medical benefit drugs for Medicare Advantage members need step therapy, starting Jan. 1
In the new year, according to Centers for Medicare & Medicaid Services’ guidance, certain Medicare Part B specialty drugs will have additional step therapy authorization requirements. This will apply to Medicare Plus BlueSM PPO and BCN AdvantageSM members for dates of service on or after Jan. 1, 2019.
Step therapy is treatment for a medical condition that starts with the most preferred drug therapy and progresses to other drug therapies only if necessary. The goal of step therapy is to encourage better clinical decision-making.
Some examples of drugs that require step therapy are:
- Botox® for migraines and over active bladder
- Eylea®, Lucentis® and Macugen® for neovascular age-related macular edema
- Prolia® for osteoporosis
What’s changing?
For drugs requiring step therapy, authorization request questions will be different from the ones you currently answer.
Use NovoLogix® to submit authorization requests
We encourage you to send prior authorization requests for Medicare Part B specialty drugs through the NovoLogix web tool via Provider Secured Services. It’s the most efficient way to get a determination.
| 
