|
August 2015

Are you ready for ICD-10?
A federal mandate requires all HIPAA-covered entities adopt ICD-10 by Oct. 1, 2015. If you don’t know where to start, here are some helpful resources:
Resources and websites (click on links below)
- For a general overview on ICD-10, watch this Blue Cross Blue Shield of Michigan webinar by clicking here: ICD-10 Overview webinar. Also, check web-DENIS to register for upcoming ICD-10 webinars
- Centers for Medicare and Medicaid Services (CMS.gov**) provider resources include a Quick Start Guide: www.cms.gov/icd10/**
- CMS sponsored "Road to ICD-10" website for small-medium physician practices: Build your action plan and jump start your transition to ICD-10. It’s simple and free. Visit the CMS tool at: www.roadto10.org/**
- American Academy of Professional Coders (AAPC.com**) has resources, coding cross walks and an online ICD-10 code conversion tool:
- Specialized training resources for an extra cost: American Association Professional Coders – (AAPC.com**) and the American Health Information Management Association (AHIMA.org**):
- Coding and documentation tips (AHIMA.org** and Californiahia.org**):
- American Medical Association (AMA.org**):
- American Hospital Association (AHA.org**):
- Blue Cross — bcbsm.com/ICD-10, provider readiness and testing mailboxes:
- CMS MLN Matters #SE1325 – Institutional services split claims billing instructions for Medicare fee-for-service claims that span the ICD-10 implementation date:
- CMS MLN ICD-10-CM/PCS myths and facts:
- Michigan Department Community Health - ICD 10 awareness and training
- American Academy of Family Physicians (AAFP.org**):
- American Academy of Pediatrics (AAP.org**):
- Check with your societies and associations
- If you’d like to view prior Precyse University webinars conducted on behalf of Blue Cross, download the presentation by visiting: precyseuniversity.com/bcbsmi/webinars/, then click on the picture to listen to the webinar.
Professional testing
Testing ICD-10 knowledge is one of the more important success factors for managing the potential risk of business disruptions and achieving ICD-10 compliance. Blue Cross is offering a medical scenario-based, professional testing tool for providers or for facilities that are billing for professionals. This testing will provide hands-on ICD-10 coding practice that represents high-volume claims by specialty that professionals are most likely to encounter:
- The testing tool will be available through the ICD-10 implementation on Oct. 1, 2015.
- Testing is done through the Web; no special software or lengthy test requirements are needed.
- It is “content based” and “specialty specific,” which means that providers for 40 different specialties will be represented with several medical scenarios to code in ICD-10. Providers can register for more than one specialty.
- Blue Cross will provide a peer group report of the participant responses for the same scenario.
- Click on this registration link to the Blue Cross professional testing tool: http://bcbsmicd10providerregistry.highpoint-solutions.com/Registration.aspx?Test=y
We recommend that the people completing the tests are familiar with the ICD-10 code set and that they either have a code book or other references or tools to complete the testing.
Professional specialty scenarios available for testing with Blue Cross
Allergy/immunology
Audiologist
Cardiovascular disease
Certified nurse midwife
Chiropractic
Clinical psychologist
Dermatology
Emergency medicine
Endocrinology
Family practice
Gastroenterology
General practice
General surgeon
Group practice
Hematology
Hematology/oncology
Infectious disease
Internal medicine
Nephrology
Neurology |
Nurse practitioner
Obstetrics and gynecology
Occupational therapist
Ophthalmology
Optometry
Orthopedic surgery
Otolaryngology
Pediatric medicine
Physical medicine and rehabilitation
Physical therapist
Plastic and reconstructive surgery
Podiatry
Psychiatry
Psychologist
Pulmonary disease
Radiation oncology
Rheumatology
Thoracic surgery
Urology
Vascular surgery |
For transactional and end-to-end testing for facilities with Blue Cross, contact us at icd-10providertesting@bcbsm.com. For other ICD-10 questions, contact us at ICD-10projectinquiries@bcbsm.com or icd-10providerreadiness@bcbsm.com.
**BCBSM does not own or control this website.
Blue Cross promotes clinical effectiveness for mental health treatment
Blue Cross Blue Shield of Michigan is committed to improving the quality of mental health treatment delivered to our members. As a result, we’re taking the following actions:
- Encouraging all health care professionals to follow treatment guidelines developed by the Michigan Quality Improvement Consortium in connection with Blue Cross
- Tracking certain aspects of quality using measures in the Healthcare Effectiveness Data and Information Set, also known as HEDIS®
MQIC guidelines
MQIC now has three guidelines focused on common conditions in mental health. These conditions include attention deficit hyperactivity disorder, depression and substance abuse.
- Diagnosis and management of ADHD (new)
- Symptom assessment leading to detection and diagnosis
- Elements of non-pharmacological management and proper initiation of pharmacotherapy
- Common co-morbid conditions frequently seen with ADHD
- Follow-up during the 30 days following initiation of pharmacotherapy and twice during the following nine months, the continuation and maintenance phase
- Primary care diagnosis and management of adults with depression
- This guideline addresses key components of detection and diagnosis using validated screening tools (PHQ-2 and PHQ-9) and criteria from the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, 4th edition, or DSM-IV.
- The guideline includes recommendations for screening for suicidal risk and management of patients on antidepressant medication. This includes conditions and circumstances in which referral to a behavioral health specialist is advised.
- Guideline for titration of medications and routine follow-up, typically at least monthly.
- Guideline advises that patients should remain on medication at least nine to 12 months until symptoms completely resolve. May require longer treatment, particularly for recurrent major depression, which often requires lifelong treatment.
- Screening, diagnosis and referral for substance use disorders
- This guideline should be followed at every health maintenance exam or first pregnancy visit.
- The guideline includes the HEDIS standard of treatment initiation and follow-up within 14 and 30 days, respectively.
You can find all of the MQIC guidelines at MQIC.org.**
HEDIS measures
Four HEDIS measures are related to behavioral health services, including:
- Antidepressant medication management
- Follow-up care for children prescribed ADHD medication
- Follow-up after hospitalization for mental illness
- Initiation and engagement of alcohol and other drug dependence treatment
Blue Cross’ Physician Group Incentive Program endorses all of the behavioral health measures in its tracking initiative (evidence-based care reporting).
**Blue Cross Blue Shield of Michigan does not own or control this website.
Online training tool explains best practices for risk adjustment, documentation and diagnosis coding
Managing patient care begins with accurate documentation and coding. You can now watch a 15-minute, informational Brainshark presentation to learn more about risk adjustment and how accurate documentation benefits both doctors and patients at brainshark.com/bcbsm/riskadjustment.
This new online training tool also provides helpful information about:
- Risk adjustment for Medicare Advantage, individual and small group health plans
- The Medicare Advantage Diagnosis Closure Incentive Program
- Useful tools and resources available to you
We strive to ensure that all patients with chronic conditions are seen at least once a year and that they receive appropriate care. Your detailed documentation and coding of diagnoses, along with any treatment or care each year, are key to managing patient care.
To properly document and code, doctors must manage, evaluate, assess or treat every patient and every condition every year.
This fall, watch for an interactive, computer-based training module that provides more important information and helpful tips about documenting and coding your patient’s conditions.
Visit the link above to learn more about best practices in documentation and coding and the advantages they provide to you and your patients. We look forward to partnering with you to provide affordable, high-quality care to our members.
Want to learn more?
Visit brainshark.com/bcbsm/riskadjustment to view a Brainshark presentation titled Risk Adjustment, Best Practices for Documentation and Diagnosis Coding.
Blue Cross reinstates reimbursements for medical record requests related to diagnoses submission
We recently told you about a policy change, effective May 1, 2015, related to reimbursement for Blue Cross Blue Shield of Michigan risk adjustment medical records. This change indicated we would no longer reimburse in-network physicians for the administrative costs associated with medical record retrieval.
We’ve decided to suspend that policy retroactive to May 1, 2015. The previous risk adjustment policy, which reimbursed in-network, Medicare Advantage physicians for medical records, will remain in effect. You may resume submitting reimbursement requests under that policy. We apologize for any inconvenience this shift may have caused.
As you know, the Centers for Medicare & Medicaid Services expects health plans and providers to conduct accurate documentation and complete medical record coding. Performing well in this regard is in our collective best interest. We appreciate your continued partnership in meeting these compliance expectations.
As we look to the future, we believe electronic medical record connectivity between Blue Cross, Blue Care Network and the provider community will reduce costs and administrative challenges.
We’ll continue striving to use information technology, wherever possible, to reduce the need for providers and Blue Cross to manually collect medical records. To that end, we’re working to identify additional connectivity options to support our provider community in the use of electronic medical records and retrieval.
Contact your provider consultant if you have any questions or concerns related to medical record requests.
There’s a change in Deductible Maximums screen for chiropractors and skilled nursing facilities
As you read in a web-DENIS message in June, there’s been a change in the Deductible Maximums screens on web-DENIS for services provided by chiropractors and skilled nursing facilities. You’re now able to see if the benefit has been used, as well as how many visits remain for chiropractic services and the number of days remaining for the skilled nursing benefit.
This feature applies to members on the NASCO and MOS platforms who have migrated to the Accumulator Solution. We hope to have all NASCO and MOS groups migrated by the end of this year.
If you have any questions, contact your provider consultant.
New Medicare Part D prescriber prerequisite enrollment deadline extended
As an update to the new Centers for Medicare and Medicaid mandate, providers and other health care professionals who write prescriptions for Medicare Part D members must enroll in Medicare for an approved prescriber status or submit a valid opt-out affidavit before Jan. 1, 2016. Providers and other eligible health professionals need to enroll to ensure continued prescription coverage under Medicare Part D.
Those who’ve previously applied to meet this requirement and have received registration confirmation from CMS aren’t required to do anything else to fulfill this requirement.
CMS has also issued an interim final rule that excuses pharmacists from the enrollment requirement. However, other prescribers remain subject to this final rule and these new requirements will be enforced beginning June 1, 2016.
Providers should have their completed Medicare enrollment applications or opt-out affidavits submitted to their Medicare administrative contractors no later than Jan. 1, 2016, to prevent their patients’ prescription drug claims from being denied by their Part D plans, beginning June 1, 2016. For more information, click here.**
If you have any questions, contact your Medicare administrative contractor at their toll-free number, which can be found by accessing the Review Contractor Directory Interactive Map** on the CMS website.
Enrolling in Medicare Part D
You may submit your enrollment application electronically using the Internet-based Provider Enrollment, Chain, and Ownership System located at pecos.cms.hhs.gov/pecos/login.do** or by completing the paper CMS-855I or CMS-855O application, which is available at http://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/CMS-Forms-List.html.** Note that an application fee isn’t needed as part of your application submission.
**Blue Cross Blue Shield of Michigan does not own or control this website.
CMS adds 10 new CPT codes
The Centers for Medicare & Medicaid Services has added 10 new Common Procedure Terminology codes, commonly known as CPT codes, in the category of “Pathology and Laboratory Multianalyte Assays with Algorithmic Analyses.”
The new codes are listed below, and none are covered by Blue Cross Blue Shield at this time:
Code |
Change |
Coverage comments |
Effective date |
81490 |
Added |
Not covered by Blue Cross Blue Shield of Michigan |
Jan. 1, 2016 |
81493 |
Added |
Not covered by Blue Cross Blue Shield of Michigan |
Jan. 1, 2016 |
81525 |
Added |
Not covered by Blue Cross Blue Shield of Michigan |
Jan. 1, 2016 |
81528 |
Added |
Not covered by Blue Cross Blue Shield of Michigan |
Jan. 1, 2016 |
81535 |
Added |
Not covered by Blue Cross Blue Shield of Michigan |
Jan. 1, 2016 |
81536 |
Added |
Not covered by Blue Cross Blue Shield of Michigan |
Jan. 1, 2016 |
81538 |
Added |
Not covered by Blue Cross Blue Shield of Michigan |
Jan. 1, 2016 |
81540 |
Added |
Not covered by Blue Cross Blue Shield of Michigan |
Jan. 1, 2016 |
81545 |
Added |
Not covered by Blue Cross Blue Shield of Michigan |
Jan. 1, 2016 |
81595 |
Added |
Not covered by Blue Cross Blue Shield of Michigan |
Jan. 1, 2016 |
As part of our ongoing series on the BlueCard program, here’s the answer to a question we recently received.
I need to request required authorizations for services rendered to BlueCard members. Can I submit those requests electronically?
Yes, a Michigan provider can request a required authorization electronically as long as member’s home plan has electronic capability for its local providers. The Electronic Provider Authorization tool allows a Michigan provider to access an out-of-state plan’s website through Provider Secured Services at bcbsm.com.
The member’s three-letter alpha prefix will route you to his or her home plan’s Web page. Each home plan’s Web page will look different, and every plan will not offer the same electronic capabilities. If an electronic option is not available for the authorization you require, the plan’s website should direct you to contact the plan using the BlueCard toll free number: 1-800-676-2583.
For more information on the EPA and BlueCard programs, including links to articles about the EPA program, please reference the BlueCard chapter of the online provider manuals.
If you’re experiencing issues with the information provided in the BlueCard chapter or any of the online tools — or if you’d like more information on a particular topic — contact your provider consultant. If you’d like to suggest a topic to be covered in a future issue of The Record, send an email to ProvComm@bcbsm.com and put “BlueCard series” in the subject line.
Coding corner: Improve medical record documentation for alcohol abuse and alcohol dependence
Blue Cross Blue Shield of Michigan follows the Centers for Medicare & Medicaid Services’ ICD-9-CM coding guidelines and American Hospital Association coding clinics to identify supporting documentation for alcohol use. The medical record documentation for alcohol-related conditions isn’t always clear to the reader.
Complete documentation is crucial to accurately report the medical condition, status, severity, and any other conditions that affect or are affected by the abuse or dependence. Medical conditions submitted to CMS are based solely on provider documentation.
It’s important to be specific, too. Complete documentation is essential to determine whether the condition is alcohol abuse or alcohol dependence, known as alcoholism. The following are examples from progress notes that don’t include the diagnosis:
- Patient is aware his drinking is causing problems with family relationships.
- Patient needs a drink to get going in the morning or to unwind after a long day.
- Patient admits to drinking every Friday to get drunk with friends.
- Patient drinks a beer but is finding it difficult to stop at one.
It’s critical that providers take it onestep further and identify the status of alcohol use in their documentation. For example, providers should note if it’s continuous, episodic or in remission. Here are sample situations where additional documentation is needed to identify the status of the condition:
- Patient needs a drink every day to unwind.
- Patient only drinks on Friday to get a high.
- Patient hasn’t had a drink in a week, two weeks, a month or two months.
A review of the past medical history is a critical part of the patient encounter. It’s important to remember the following:
- The progress note must be current and updated with each office visit.
- Actively treating conditions recorded in past medical history must be addressed and documented in the face-to-face encounter.
- When both “abuse” and “dependence” have been recorded, the notes should clearly describe which one is actively being treated. Without this clarification, neither diagnosis can be reported. Note: This differs from the ICD-10-CM coding guidelines. See details below under ICD-10.
“History of” means the condition no longer exists and the patient is no longer receiving any treatment. Providers often use “history of” to signify “ongoing” or “continual” conditions. Without supporting documentation, the status of the condition is unclear and may default to a personal history. The following are examples of the two scenarios:
- Patient has a history of consuming a minimum of six cans of beer daily since age 18. Patient has been sober now for five years and continues with Alcoholics Anonymous program.
- Patient has a history of consuming a minimum of six cans of beer daily since age 18. We discussed in today’s visit how the patient’s drinking continues to affect his overall health.
It’s equally important to review associated medical conditions in the face-to-face encounter. For example:
- Patient is present for annual visit. He’s alcohol dependent and drinks a minimum six cans of beer daily and has done so continuously over the past five years. In today’s visit, it was stressed that his liver damage will worsen if he doesn’t stop drinking.
- Patient is an alcoholic who quit drinking three days ago. He’s complaining of shakiness and anxiety. It was explained that his body has developed a physical dependence and he’s experiencing withdrawal symptoms.
ICD-10
As we anticipate the conversion to ICD-10-CM coding guidelines on Oct. 1, 2015, it’s important to remember that ICD-10-CM includes a more comprehensive index to capture a complete diagnosis, such as alcohol, delirium, with intoxication, in abuse.
Both ICD-10-CM and ICD-9-CM coding guidelines allow onlyone code to be assigned when referring to alcohol use, abuse and dependence. However, with ICD-10-CM, a hierarchy is followed. For example:
- When both “use”and “abuse” are documented, only a code for “abuse” can be reported.
- When both “abuse” and “dependence” are documented, only a code for “dependence” can be reported.
Alcohol documentation should read as “use,” “abuse” or “dependence.” It’s equally important to identify the pattern of use. For example, “uncomplicated,” “intoxication” or “remission.”
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with applicable state and federal laws and regulations.
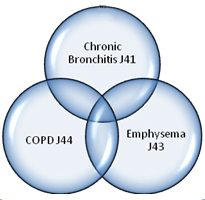
Coding corner update: Improve medical record documentation for airway-related conditions
Beginning Oct. 1, 2015, the transition to ICD-10-CM will affect every area of health care. Many codes contain much greater specificity. This article includes updated codes to align with the transition to ICD-10-CM.
The overlap in terminology used to define airway-related conditions, such as chronic obstructive pulmonary disease, asthma, emphysema and chronic bronchitis, can often be confusing. The appropriate terminology for these conditions can best be determined through careful use of the ICD-10-CM Alphabetic Index.
Two particularly challenging conditions for coders are COPD and asthma. Although both share airway obstruction as a common feature, they’re at different ends of the clinical spectrum. However, the two conditions may overlap in many patients later in life.
Asthma often develops during childhood and can cause temporary airway obstruction. It’s often caused by allergies, too. In contrast, COPD usually develops later in life, is often related to smoking, and causes permanent airway obstruction. The two main forms of COPD are emphysema and chronic bronchitis. Asthma and COPD can often overlap, especially in elderly patients who might be affected by both diseases.
In ICD-10-CM, chronic obstructive asthma and asthma with COPD are reported with codes from the J44 category, other chronic obstructive pulmonary disease. Coding notes for this category state to code also the type of asthma, if applicable (J45.-). Use an additional code to identify exposure to tobacco smoke and tobacco use or dependence, if applicable.
Careful attention should be paid to documentation for a patient with a form of COPD and asthma. Here’s an example of how to assign diagnosis codes for a patient who’s affected by both conditions:
Assessment
- Acute exacerbation of COPD
- Acute bronchitis
- Acute exacerbation of asthma
Report diagnosis code J44.0, chronic obstructive pulmonary disease with acute lower respiratory infection for the COPD with acute lower respiratory infection (use additional code for the infection, bronchitis). Assign code J44.1, Chronic obstructive pulmonary disease with (acute) exacerbation, for the acute exacerbation of COPD; and code J45.901, unspecified asthma with (acute) exacerbation, for the acute exacerbation of asthma.
There’s an exclusion note under code J44.1 (COPD with acute exacerbation) that means multiple codes are required to code COPD with both an acute exacerbation as well as an acute respiratory infection.
The asthma category of codes has changed significantly in ICD-10-CM to reflect the current clinical classification of asthma. The following terms have been added to describe asthma: mild intermittent, mild persistent, moderate persistent and severe persistent. In addition, the ICD-10-CM codes also have the ability to identify with or without exacerbation and status asthmaticus. The classifications are determined by the frequency of the symptoms, exacerbation and status asthmaticus. Here are examples of the codes:
ICD-10-CM code |
Description |
J45.20 |
Mild intermittent asthma, uncomplicated |
J45.31 |
Mild persistent asthma with (acute) exacerbation |
J45.42 |
Moderate persistent asthma with status asthmaticus |
J45.51 |
Severe persistent asthma with (acute) exacerbation |
J45.902 |
Unspecified asthma with status asthmaticus |
J45.990 |
Exercise induced bronchospasm |
According to the ICD-10-CM guidelines, acute exacerbation is a worsening or a decompensation of a chronic condition. An acute exacerbation is not equivalent to an infection superimposed on a chronic condition, though an exacerbation may be triggered by an infection.Status asthmaticus is defined as a patient’s failure to respond to therapy administered during an asthmatic episode and is a life-threatening complication that requires emergency care.
ICD-10-CM coding for all conditions should follow coding conventions, chapter specific guidelines and general coding guidelines.
If you have any questions, contact your provider consultant.
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with applicable state and federal laws and regulations.
Coding corner update: Improve medical record documentation for angina
Beginning Oct. 1, 2015, the transition to ICD-10-CM will affect every area of health care. Many codes contain much greater specificity. This article includes updated codes to align with the transition to ICD-10-CM.
Angina is pain or discomfort that occurs when your heart doesn’t get enough oxygen due to reduced blood flow. Over time, the coronary arteries that supply blood to your heart can become clogged with plaque. When plaque builds up in the heart’s arteries, the condition is called atherosclerosis. If one or more arteries are partly clogged, not enough blood flows through and can cause chest pain.
Angina is usually an early manifestation of ischemic heart disease known as coronary heart disease, also called coronary artery disease. According to the American Heart Association, heart disease is the number one killer of men and women, affecting one out of three in the U.S. Women sometimes don’t understand the risks, putting them more at risk for a heart attack.
Documentation in the medical record must be specific and clear to properly code the condition. Chest or abdominal pain is classified as a symptom and is only acceptable for reporting purposes when the provider has not established a confirmed diagnosis.
In ICD-10-CM, a causal relationship can be assumed in a patient with both atherosclerosis and angina pectoris, unless the documentation indicates the angina is due to something other than the atherosclerosis. (Coding guideline I.C.9.b). If a patient is diagnosed with angina, you should document the specific type of angina.
Types of angina
- Stable angina (ICD-10-CM code I20.9, angina pectoris, unspecified)
- Can occur during physical activity or emotional stress
- Unstable angina (ICD-10-CM code I20.0, unstable angina)
- Can occur with or without physical activity, even while at rest or sleeping
- Occurs when plaque in one or more coronary artery ruptures and if the buildup happens rapidly, there’s risk for a heart attack
- Variant angina (Prinzmetal’s angina) (ICD-10-CM code I20.1, angina pectoris with documented spasm)
- A rare type of angina that happens without warning
- Caused by a spasm in a coronary artery in which the artery narrows, reducing blood flow to the heart and causing chest pain
- Microvascular angina (ICD-10-CM code I20.8, other forms of angina pectoris)
- Can be a more severe type of angina that lasts longer, and the pain is caused by spasms within the walls of small arterial blood vessels
Men and women may experience different symptoms that can vary depending on the type of angina.
Elderly people may experience different symptoms of angina, and these can be easily overlooked. For example:
- Indigestion after meals may be blamed on a stomach ulcer or reflux.
- Pain in the back and shoulders may be interpreted by the patient or diagnosed as arthritis.
Keep in mind that dementia can play a role in a person’s ability to communicate the pain they’re experiencing.
It’s important to include specific documentation that angina exists at the time of the patient encounter, and that this diagnosis requires or affects care, treatment and management.
ICD-10-CM coding for all conditions should follow coding conventions, chapter specific guidelines and general coding guidelines.
For more information about this coding process, contact your provider consultant.
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with applicable state and federal laws and regulations.
Coding corner update: Improve medical record documentation for heart failure
Beginning Oct. 1, 2015, the transition to ICD-10-CM will affect every area of health care. Many codes contain much greater specificity. This article includes updated codes to align with the transition to ICD-10-CM.
Heart failure is a challenge for all providers and affects all different specialties. Heart failure occurs when the heart muscle doesn’t pump blood to the body as effectively as it should. It can be an acute condition, but most of the time it occurs slowly and becomes a chronic condition. Heart failure often develops after other conditions have damaged or weakened the heart.
Congestive heart failure is a specific type of heart failure that occurs when blood backs up — and becomes congested — into other locations such as the liver, abdomen, lower extremities and lungs. It’s often mistakenly used interchangeably with heart failure. Congestion is one feature of heart failure, but it doesn’t occur in all patients.
Causes of heart failure include coronary artery disease, cardiomyopathy, arrhythmias, hypertension, myocarditis and faulty heart valves. In turn, heart failure may contribute to the severity of other conditions such as kidney disease, diabetes, pulmonary embolism, endocarditis, anemia and other conditions.
Heart failure can involve the left, right or both sides of the heart, but usually begins on the left side.
Type of heart failure |
Description |
Right-sided
(right ventricular) |
Secondary to left-sided heart failure. Fluid may back up into abdomen, legs and feet, causing swelling (edema). |
Left-sided |
This is the most common type of heart failure. Fluid may back up in lungs, causing shortness of breath. There are two types of left-sided heart failure: |
|
- Systolic — Occurs when the ability of the heart to contract decreases and the result is blood coming from the lungs into the heart may back up.
- Diastolic — Occurs when the left ventricle can’t relax fully between contractions. The heart can’t properly fill with blood, which may lead to fluid accumulation in the legs, ankles and feet.
|
Symptoms of heart failure include:
- Shortness of breath
- Dizziness, fatigue and weakness
- Fluid and water retention
- Rapid or irregular heartbeats
- Cough or wheezing with white or pink blood-tinged phlegm
- Chest pain
Coding for heart failure
Coding and documentation of heart failure and congestive heart failure has its own challenges. The types of heart failure referenced above should be documented in order to correctly assign ICD-10 codes. Systolic heart failure uses codes in the I50.2 category, while diastolic heart failure uses codes in the I50.3 category. There’s also a category for combined systolic and diastolic heart failure: I50.4. A fifth character can be used to further specify whether the heart failure is unspecified, acute, chronic or acute on chronic.
When documenting only “congestive heart failure,” use ICD-10 code I50.9: heart failure, unspecified.
If a patient has hypertensive heart disease with congestive heart failure, report a code for the hypertensive heart disease with heart failure (I11.0). Use an additional code for heart failure (I50 category) to identify the type of heart failure. However, a causal relationship between the two conditions must be documented by the practitioner in order to be coded as such.
A coder can’t assume a cause-and-effect relationship, and the correct way to document a causal relationship is by stating “congestive heart failure due to hypertension.” A patient with congestive heart failure and hypertension without a documented causal relationship is assigned separate ICD-10 codes for congestive heart failure (I50.9) and hypertension (I10). Documentation simply stating “heart failure” codes to I50.9.
Documentation of diastolic or systolic dysfunction without mention of heart failure codes to I51.9: heart disease, unspecified. Don’t assume that a patient is in heart failure if only “diastolic dysfunction” or “systolic dysfunction” is documented. Other terms for this code include “Heart disease, unspecified” and “Organic heart disease NOS.”
ICD-10-CM coding for all conditions should follow coding conventions, chapter specific guidelines and general coding guidelines.
If you have questions or need more information, contact your provider consultant.
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with applicable state and federal laws and regulations.
Coding corner update: Improve medical record documentation for chronic obstructive pulmonary disease and other associated respiratory conditions
Beginning Oct. 1, 2015, the transition to ICD-10-CM will affect every area of health care. Many codes contain much greater specificity. This article includes updated codes to align with the transition to ICD-10-CM.
In order to support the ICD-10-CM diagnosis code selected, chronic obstructive pulmonary disease and other associated respiratory conditions need to be properly documented in the medical record.
What’s COPD?
Chronic obstructive pulmonary disease is a common and progressive disease that makes it difficult to breathe. Common symptoms include coughing that produces large amounts of mucus, wheezing, shortness of breath and chest tightness. The two main forms of COPD are emphysema and chronic bronchitis. However, many patients with COPD have both emphysema and chronic bronchitis.
What causes COPD?
Smoking cigarettes is the leading cause of COPD. Most people who have COPD are either current smokers or have a history of tobacco use. Other causes include long- term exposure to lung irritants such as air pollution, chemical fumes and dust, all of which can contribute to COPD.
Tips to remember when coding COPD
When coding for COPD, bronchitis (acute, chronic), asthmatic bronchitis (acute, chronic), emphysema and other associated respiratory conditions, it’s important to properly code whether or not the condition is acute, chronic or in acute exacerbation.
- Due to the overlapping nature of the conditions that comprise COPD, code selection must be based on terms documented by the provider.
- ICD-10-CM code J44.9, chronic obstructive pulmonary disease, unspecified, should only be used if the type of COPD being treated is not specified in the medical record.
- It’s imperative to always document and code to the highest specificity. For example, if the provider states “acute bronchitis” or “chronic bronchitis,” (both unspecified) then report ICD-10-CM codes J20.9 and J42.0, respectively. However if the provider does not indicate whether the bronchitis was either acute or chronic, then the appropriate ICD-10-CM code would be J40: Bronchitis not specified as acute or chronic.
- When COPD with an acute exacerbation is documented without acute bronchitis, then report ICD-10-CM code J44.1: Chronic obstructive pulmonary disease with (acute) exacerbation.
- Code J44.0 (Chronic obstructive pulmonary disease with acute lower respiratory infection) when the medical record supports acute bronchitis and COPD. Use an additional code to identify the infection.
ICD-10-CM code |
Description of respiratory condition |
J41.0 |
Simple chronic bronchitis |
J41.1 |
Mucopurulent chronic bronchitis |
J44.– |
Other Obstructive pulmonary disease
J44.0 COPD with acute lower respiratory infection
J44.1 COPD with (acute) exacerbation
J44.9 COPD, unspecified |
J41.8 |
Mixed simple and mucopurulent chronic bronchitis |
J42 |
Unspecified chronic bronchitis |
J43.9 |
Emphysema, unspecified |
J45.– |
Asthma
J45.2- Mild Intermittent asthma
J45.3- Mild persistent asthma
J45.4- Moderate persistent asthma
J45.5- Severe persistent asthma
J45.9- Other and unspecified asthma |
R09.02 and J44.9 |
Hypoxemia and COPD
Please note that hypoxemia is not an inherent component of COPD (AHA, Coding Clinic, 2009, issue 3). |
Z93.0 |
Tracheostomy status |
Z99.11 |
Dependence on respirator; ventilator status |
J95.850 |
Mechanical complication of respirator |
Z99.81 |
Dependence on supplemental oxygen (You should code the underlying condition first.) |
Z43.0 |
Encounter for attention to tracheostomy |
It’s important to review the ICD-10-CM Coding Guidelines (Chapter 10: “Diseases of Respiratory System J00-J99”), as well as any instructional notes under the various COPD subcategories and codes in the tabular list of the ICD-10-CM manual, in order to select the correct code. In addition to the codes listed above it is important to include codes related to tobacco usage, dependence or other exposure.
ICD-10-CM coding for all conditions should follow coding conventions, chapter specific guidelines and general coding guidelines.
If you have questions or need more information, contact your provider consultant.
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with applicable state and federal laws and regulations.
Coding corner update: Improve medical record documentation for hypertension
Beginning Oct. 1, 2015, the transition to ICD-10-CM will affect every area of health care. Many codes contain much greater specificity. This article includes updated codes to align with the transition to ICD-10-CM.
According to the Centers for Disease Control and Prevention, one in every three adults has hypertension and only half of those adults have it under control. If left uncontrolled for too long, hypertension can damage the heart, kidneys and other organs.
Coding of hypertension was simplified in ICD-10-CM as it is no longer classified by malignant, benign or unspecified. There is only one code, I10 Essential (primary) hypertension. Therefore there is no longer a table in the alphabetic index in the code book.
There are ICD-10-CM codes which are used for reporting hypertension in its simple vascular state, without manifestations, and combination codes that illustrate the affect of hypertension on other organs. This allows providers to communicate the complexity of their patient’s condition to the greatest specificity — whether the condition exists alone or with other diseases.
Coding tips for hypertension
Here are common codes for hypertension:
- Primary or essential hypertension is considered idiopathic — occurring without apparent cause. Code categories I10 to I13 are used for primary hypertension.
- Secondary hypertension is due to an underlying cause and is reported with codes from category I15. Code also the underlying condition.
- Although ICD-10-CM classifies benign or malignant hypertension to one code, I10- Essential (primary) hypertension, the documentation in the medical record should be specific.
- According to the National Institutes of Health, malignant hypertension is defined as high blood pressure that comes on suddenly and quickly. Malignant hypertension often causes organ damage. Other terms for malignant hypertension include accelerating or necrotizing.
- Benign hypertension is mild to moderate elevation in blood pressure of prolonged or chronic duration without target organ damage.
- Hypertension is benign or malignant and it must be documented in the progress note by the provider.
- Documentation should indicate hypertension, benign, or hypertension, malignant. Documentation that states only elevated or high blood pressure could be misinterpreted as transient or incidental hypertension.
- Documentation that indicates elevated or high blood pressure, or borderline hypertension, but doesn’t state a diagnosis of hypertension, is reported with R03.0 (elevated blood pressure reading without diagnosis of hypertension).
Hypertension and correct coding
ICD-10-CM classifies hypertension by type as essential or primary (code I10, essential (primary) hypertension and secondary (category I15). An additional code to identify tobacco use or exposure should be listed if applicable.
Hypertensive heart disease
Hypertension may increase the workload of the left ventricle of the heart due to the higher systemic vascular resistance. This can result in hypertrophy of the heart or combined hypertrophy and dilation, also known as heart disease.
Heart conditions classified to I50.– or I51.4-I51.9, are assigned to a code from category I11, Hypertensive heart disease, when a causal relationship is stated (due to hypertension) or implied (hypertensive). Providers must establish causality in the documentation in order for the combination code to be assigned since causality can’t be assumed. When using codes from category I11, use an additional code from category I50 heart failure to identify the type of heart failure when present. The same heart conditions (I50.–, I51.4-I51.9) with hypertension, but without a stated causal relationship, are coded separately. Make sure to sequence according to the circumstances of the encounter.
Code |
Title |
I11.9 |
Hypertensive heart disease, without heart failure |
I11.0 |
Hypertensive heart disease, with heart failure |
Hypertensive chronic kidney disease
According to the National Kidney Foundation, hypertension is the leading cause of chronic kidney disease. It can also be a complication of chronic kidney disease, and the association between hypertension and chronic kidney disease is so strong that ICD-10-CM presumes a cause and effect relationship between the two conditions.
Code |
Title |
I12.0 |
Hypertensive chronic kidney disease with stage 5 chronic kidney disease or end stage renal disease |
I12.9 |
Hypertensive chronic kidney disease with stage 1-4 chronic kidney disease or unspecified chronic kidney disease |
A code from category N18 should also be used to document the stage of chronic kidney disease.
Only chronic kidney conditions classified to category N18 can be reported with the hypertensive chronic kidney disease codes. There isn’t an assumed causal relationship between hypertension and acute renal failure, which usually develops as the result of an event such as dehydration, major blood loss or the side effect of medication, and it’s often reversible. In contrast, chronic kidney disease is caused by the effects of hypertension or other diseases over a long period of time.
Hypertensive heart and chronic kidney disease
The kidneys play an important role in regulating blood pressure. But when they develop disease, blood pressure can increase and the likelihood of heart problems can increase as well. Due to their interactive nature, category I13 combines three conditions: heart disease, hypertension and chronic kidney disease. As previously indicated, a relationship between chronic kidney disease and hypertension can be assumed, but documentation must indicate a causal relationship between hypertension and heart disease.
Code |
Title |
I13.0 |
Hypertensive heart and chronic kidney disease with heart failure and stage 1-4 chronic kidney disease or unspecified chronic kidney disease |
I13.10 |
Hypertensive heart and chronic kidney disease without heart failure with stage 1-4 chronic kidney disease or unspecified chronic kidney disease. |
I13.11 |
Hypertensive heart and chronic kidney disease without heart failure with stage 5 chronic kidney disease or end stage renal disease. |
I13.2 |
Hypertensive heart and chronic kidney disease with heart failure and with stage 5 chronic kidney disease or end stage renal disease. |
Additional codes should be added to indicate the type of heart failure and stage of chronic kidney disease.
Secondary hypertension
Secondary hypertension is coded using category I15. It’s defined as high arterial blood pressure due to another underlying cause or primary disease, such as a renal disorder, central nervous system disorders, endocrine or vascular diseases. A code should be reported for the type of secondary hypertension and also a code for the underlying etiology.
Hypertension may contribute or accelerate the development of many other conditions. Because ICD-10-CM doesn’t provide combination codes for every condition, assign a code for each individual condition to communicate the complexity of a patient’s condition.
ICD-10 coding for all conditions should follow coding conventions, chapter specific guidelines and general coding guidelines.
If you have questions or need more information, contact your provider consultant.
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with applicable state and federal laws and regulations.
Reminder: Auto insurance is primary when treating FEP® members for auto accident-related injuries
When you’re treating Federal Employee Program members for injuries and conditions sustained in a car accident, bill the member’s no-fault auto insurer as the primary payer.
In these circumstances, regardless of any state law, FEP requires the member’s no-fault auto insurance to be the primary payer. FEP has rights of recovery and subrogation under certain situations including when members are injured in a car accident, despite the member’s coverage under any no-fault auto insurance and associated Personal Injury Protection.
This holds true even if the FEP member has elected to designate their auto insurance coverage as secondary to their FEP health benefits coverage.
Blues highlight medical, benefit policy changes
You’ll find the latest information about procedure codes and Blue Cross Blue Shield of Michigan billing guidelines in the following chart.
This billing chart is organized numerically by procedure code. Newly approved procedures will appear under the New Payable Procedures heading. Procedures for which we have changed a billing guideline or added a new payable group will appear under Updates to Payable Procedures. Procedures for which we are clarifying our guidelines will appear under Policy Clarifications. New procedures that are not covered will appear under Experimental Procedures.
You will also see that descriptions for the codes are no longer included. This is a result of recent negotiations with the AMA on use of the codes.
We will publish information about new BCBS groups or changes to group benefits under the Group Benefit Changes heading.
For more detailed descriptions of the BCBSM policies for these procedures, please check under the Medical/Payment Policy tab in Explainer on web-DENIS. To access this online information:
- Log in to web-DENIS.
- Click on BCBSM Provider Publications & Resources.
- Click on Benefit Policy for a Code.
- Click on Topic.
- Under Topic Criteria, click on the drop-down arrow next to Choose Identifier Type and then click on HCPCS Code.
- Enter the procedure code.
- Click on Finish.
- Click on Search.
| Code* |
BCBSM changes to:
Basic Benefit and Medical Policy, Group
Variations Payment Policy, Guidelines |
| NEW PAYABLE PROCEDURES |
33270, 33271, 33272 **, 33273
** Payable effective 1/1/2015 |
Basic benefit and medical policy
The safety and effectiveness of an automatic implantable cardioverter defibrillator and electronic surveillance of the AICD have been established. It may be considered a useful therapeutic option for patients who meet selection criteria.
The safety and effectiveness of a subcutaneous automatic implantable cardioverter defibrillator and electronic surveillance of the AICD have been established. It may be considered a useful therapeutic option for patients who meet selection criteria, effective March 1, 2015.
Inclusionary guidelines
FDA-approved subcutaneous cardioverter-defibrillators are established for adult or pediatric persons who meet patient selection criteria for an implanted cardioverter-defibrillator and do not need pacing and the placement of a conventional AICD is precluded due to any of the following conditions:
- Poor vascular access secondary to dialysis or
- other vascular conditions
- A high risk for infection, e.g., immune-
- compromised patients or those with a history
- of a previous transvenous infection
- History of congenital heart disease with
- anatomic limitations for transvenous
- placement of the AICD
- Pediatric patients with primary cardiac diseases that display electrical conductivity problems, such as those with Brugada syndrome, LQTS disease or hypertrophic cardiomyopathy
Note: The criteria for standard automatic implantable cardioverter defibrillators was published in the December 2013 edition of The Record, and is available in the medical policy. |
90620 |
Basic benefit and medical policy
The safety and effectiveness of Bexsero®, a two-dose schedule intramuscular Serogroup B meningococcal recombinant protein and outer membrane vesicle vaccine, is established, effective Feb. 1, 2015. It is recommended by the Advisory Committee on Immunization Practices for persons meeting select criteria.
Basic benefit policy group variations
Refer to member’s policy for coverage status.
Inclusionary guidelines
Children age 10 through 18 at increased risk for meningococcal disease, attributable to serogroup B, including:
- Children who have persistent complement component deficiencies (including inherited or chronic deficiencies in C3, C5-C9, properdin, factor H or factor D, or taking eculizumab [Soliris®])
- Children who have anatomic or functional asplenia, including sickle cell disease
- Children identified to be at increased risk because of a meningococcal disease outbreak attributable to serogroup B
|
90630 |
Basic benefit and medical policy
The safety and effectiveness of Fluzone® QIV ID, a quadrivalent inactivated influenza vaccine designed for intradermal administration have been established. It may be considered a useful therapeutic option when administered according to U.S. FDA-approved guidelines. This policy is effective Jan. 1, 2015. |
90651 |
Basic benefit and medical policy
The safety and effectiveness of Gardasil®9 have been established, effective Jan. 1, 2015.
Basic benefit policy group variations
Refer to member’s policy for coverage status.
Inclusionary guidelines
The Advisory Committee on Immunization Practices recommends that routine HPV vaccination be initiated at age 11 or 12. The vaccination series can be started beginning at age 9. Vaccination is also recommended for females ages 13 through 26 and for males ages 13 through 21 who have not been vaccinated previously or who have not completed the three-dose series. Males ages 22 through 26 years may be vaccinated. Vaccination of females is recommended with 2vHPV, 4vHPV (as long as this formulation is available), or 9vHPV. Vaccination of males is recommended with 4vHPV (as long as this formulation is available) or 9vHPV.
2vHPV, 4vHPV and 9vHPV all protect against HPV 16 and 18, types that cause about 66 percent of cervical cancers and the majority of other HPV-attributable cancers in the United States. 9vHPV targets five additional cancer causing types, which account for about 15 percent of cervical cancers. 4vHPV and 9vHPV also protect against HPV 6 and 11, types that cause anogenital warts.
Administration: 2vHPV, 4vHPV, and 9vHPV are each administered in a 3-dose schedule. The second dose is administered at least 1 to 2 months after the first dose and the third dose at least 6 months after the first dose. If the vaccine schedule is interrupted, the vaccination series does not need to be restarted.
If vaccination providers do not know or do not have available the HPV vaccine product previously administered, or are in settings transitioning to 9vHPV, any available HPV vaccine product may be used to continue or complete the series for females for protection against HPV 16 and 18; 9vHPV or 4vHPV may be used to continue or complete the series for males. There are no data on efficacy of fewer than 3 doses of 9vHPV.
Special populations: HPV vaccination is recommended through age 26 years for men who have sex with men and for immunocompromised persons (including those with HIV infection) who have not been vaccinated previously or have not completed the three-dose series. |
Condition codes:
R1, R2, R3, R4, R5, R6, R7, R8, and R9 |
Payment policy
The National Uniform Billing Committee approved these condition codes, effective April 1, 2015. BCBSM also accepts these codes, effective April 1, 2015. |
| UPDATES TO PAYABLE PROCEDURES |
33228 |
Payment policy
Revenue codes:
0450 - Emergency Room-General
0480 - Cardiology-General
0510 - Clinic-General classification
0514 - Clinic-OB/GYN Clinic
0515 - Clinic-Pediatric Clinic
0516 - Clinic-Urgent Care Clinic
0517 - Clinic-Family Practice Clinic
0519 - Clinic-Other Clinic
0761 - Specialty Services-Treatment Room has been added to fee-based reimbursement, effective Oct. 1, 2013.This process is in alignment with hospital outpatient pricing.
The revenue codes listed above requires the reporting of a valid CPT or HCPCS code when services are performed in Location 22 (outpatient hospital). |
73020, 73030, 73050, 73060, 73070, 73080, 73090, 73100, 73110, 73120, 73130, 73140, 73500, 73550, 73560, 73565, 73590, 73600, 73620, 73630 |
Basic benefit and medical policy
Chiropractors are now payable providers for these procedure codes as part of the Radiology Management Program. The Federal Employee Program® is not included in this change. |
99204, 99211, 99212, 99213, 99214, 8943, 97014, 97018, 97022, 97024, 97026, 97028, 97032, 97034, 97035, 97110, 97112, 97113, 97116, 97124,
97140, G0283 |
Basic benefit and medical policy
Chiropractors are now payable providers for these procedure codes in an office setting. |
A4639, A7025, E0984, E0986, E1002, E1003, E1004, E1005, E1006, E1007, E1008, E1010, E1014, E1029, E2227, E2310, E2311, E2321, E2322, E2325,
E2326, E2327, E2328, E2329, E2330, E2351, E2373, E2374, E2375, E2376, E2377, K0607, K0730 |
Basic benefit and medical policy
Effective Sept. 1, 2015, Blue Cross will allow HCPCS codes listed to pay as a capped rental, allowing one monthly rental for up to 10 months. Then the item is considered purchased and you cannot balance-bill the member for further rental payments.
Items are also available as a purchase.
This change does not apply to groups that have DME/P&O benefits carved out to a vendor. |
J0178 |
Basic benefit and medical policy
J0178 is now payable for the following additional diagnosis of 362.36, effective Oct. 6, 2014. |
J7182 |
Basic benefit and medical policy
Novoeight (turoctocog alfa) received approval from the FDA on Oct. 16, 2013, and is covered under this procedure code, effective Jan. 1, 2015.
Novoeight (turoctocog alfa), a parenterally-administered drug, for adults, adolescents and children with Hemophilia A for:
- Control and prevention of bleeding episodes
- Perioperative management of patients with hemophilia A
- Routine prophylaxis to prevent or reduce the frequency of bleeding in adults, adolescents and children
This drug will not require prior authorization through the Specialty Pharmacy Program. |
J3490, Q9976 |
Basic benefit and medical policy
Effective Jan. 23, 2015, Triferic™ is covered under J3490 for the replacement of iron to maintain hemoglobin in adult patients with hemodialysis-dependent chronic kidney disease. Beginning July 1, 2015, report Triferic™ with HCPCS code Q9976. |
| GROUP BENEFIT CHANGES |
City of Brighton |
Effective Aug. 1, 2015, Medicare-eligible retirees of the City of Brighton will have Blue Cross Blue Shield of Michigan’s Medicare Advantage PPO plan, Medicare Plus BlueSM Group PPO for their medical, surgical and prescription drug benefits. The group number is 67371 with suffix 600. You can identify members by the XYL prefix on their ID cards, like those of other Medicare Plus Blue Group PPO plans.
For information about our Medicare Advantage PPO plan, go to bcbsm.com/provider/ma. |
City of Jackson |
Effective Aug. 1, 2015, Medicare-eligible retirees of the City of Jackson will have Blue Cross Blue Shield of Michigan’s Medicare Advantage PPO plan, Medicare Plus BlueSM Group PPO for their medical, surgical and prescription drug benefits. The group number is 67373 with suffix 600. You can identify members by the XYL prefix on their ID cards, like those of other Medicare Plus Blue Group PPO plans.
For information about our Medicare Advantage PPO plan, go to bcbsm.com/provider/ma. |
Halla Visteon Climate Control USA LLC |
Halla Visteon Climate Control USA LLC, group number 007041050, joins Blue Cross Blue Shield of Michigan, effective Aug. 1, 2015. The members in this group were previously in a Visteon Salaried group.
The group is offering one PPO, one HSA plan and one HMO, consisting of a medical and prescription drug plan.
Member ID cards will show the following alpha prefixes:
- XYQ for PPO plans
- XYY for Traditional plans
- XYR for Complementary plans
- XYH for HMO plans
|
National Heritage Academies |
Effective Sept. 1, 2015, National Heritage Academies joins Blue Cross Blue Shield of Michigan.
Group number: 71440
Alpha prefix: NHT
Plan offered:
One health savings account plan |

Do you know about GeoBlue®? It offers Blue Cross coverage for some GM members

As you read in a recent web-DENIS message, GeoBlue, in partnership with Blue Cross Blue Shield of Michigan, began serving more than 3,000 internationally based General Motors members Jan. 1, 2015. Many of these members seek care in the U.S. and present the GeoBlue identification card. See example at right.
We’ve received some inquiries from members regarding GeoBlue coverage so wanted to ensure that health care providers understand it fully. GeoBlue is a Blue Cross Blue Shield product and members have full access to the BlueCard provider network. Their ID card contains all BlueCard specifications and all BlueCard processes apply for coverage and claims.
If a member calls for an appointment and states that they have GeoBlue insurance, you can verify eligibility and benefits by calling GeoBlue Customer Service at 1-855-282-3517. After following the prompts (press 1 for services inside the U.S.), you’ll hear a recording that you cannot bypass. You need to wait until a customer service representative answers your call. Or you can go online and verify benefits through the Blue Exchange BlueCard system.
The GeoBlue ID card shows the member contract number, including the three-letter alpha prefix, and has the Blue Cross and Blue Shield symbols prominently displayed on the front.
Members with a GeoBlue ID card also have BlueDental® coverage. These members have access to dental providers who participate with the Blue Cross dental network or on a per claim basis. To verify dental benefits, log into web-DENIS or call PARS. Submit claims through the regular dental claims process.
Additional procedure codes payable to chiropractors for physical therapy services
Additional procedure codes** are payable to chiropractors for physical therapy services, effective Aug. 1, 2015. This change applies to groups with standard chiropractic benefits.
Due to this change, starting Aug. 1, physicians may be asked to agree to and sign a physical therapy treatment plans developed by chiropractors. A prescription is not required for a member to receive covered physical therapy benefits from a chiropractor.
This provision means only that Blue Cross Blue Shield of Michigan will pay for the first physical therapy service per patient and not per visit. After the first physical therapy service is provided, Blue Cross will not pay for additional physical therapy services to the patient without the development of a PT plan that is agreed to and signed by the M.D. or D.O. The only exception to this requirement is for mechanical traction (physical therapy code *97012), which may be performed at subsequent visits without a PT plan.
Regarding mechanical traction, Blue Cross will maintain the current payment structure. A physical therapy treatment plan is not required for this code. Providers are asked to document the use of the code in the PT plan if it is performed in addition to other physical therapy services. This will allow the M.D. or D.O. to be aware of all of the treatment the patient is receiving and ensure coordination and quality of care.
Note: No physician agreement or signature is required on a treatment plan for MESSA members.
**Check the billing chart in this issue of The Record for the specific codes now payable to a chiropractor.
Blue Cross Blue Shield of Michigan contracts with psychiatric residential treatment facilities in Michigan
Most Blue Cross members with mental health coverage now have coverage for psychiatric residential treatment.
Psychiatric residential treatment allows people who are suffering from a psychiatric illness to receive around-the-clock care on a short-term basis.
This level of care can allow patients with illnesses such as anorexia nervosa, schizophrenia or bipolar disorder to spend less time in a psychiatric hospital or avoid hospitalization. The treatment takes place in a state-licensed facility, for example, in an adult or child foster care facility with a multidisciplinary treatment team.
Psychiatric residential treatment is not meant to be used on an emergency basis, and admission must be coordinated by a mental health professional as part of an overall treatment plan.
Always make sure to check the member’s benefit coverage to determine eligibility. The facility must obtain preauthorization for the treatment to be covered.
To find an approved facility in Michigan, see our complete listing here.
Or you can go to bcbsm.com.
- Click Find a Doctor.
- Under “More Information,” click on Dental, Vision and Other Directories.
- Click on Approved Psychiatric Residential Treatment Facility List (PDF).
For more information on qualifying as a psychiatric residential treatment facility, read the January Record article on this topic.
Resolving your issues: Do I call or do I write?
Did you know?
- Last year, Provider Relations and Servicing processed more than 1.3 million phone inquiries and more than 100,000 written inquiries.
- On average, we answered each phone call within 90 seconds.
- On average, each phone call lasts 11 minutes.
- On average, our response time for written inquiries is more than 21 days.
First article in a series providing guidance on the best way to get your questions answered.
We’re committed to resolving your inquiries as soon as possible and making it easier for you to do business with us. That’s why we want to let you know that many of your inquiries can be handled more quickly and efficiently by calling Provider Inquiry rather than by writing to us.
When you need to write
To improve your service experience, beginning Sept. 1, 2015, we’ll only process written inquiries for the following reasons:
- Preauthorization for Blue Cross Blue Shield of Michigan-enrolled members. (For more details, see the June 2012 article on requesting medical reviews.)
- Ten or more claims regarding the same issue, including refund requests
When you can call
Below is a list of inquiries that will be handled by phone (list is not all-inclusive):
- Benefit and eligibility questions
- Duplicate rejections
- Benefit rejections
- Incorrect claim rejections
- Precertification rejections
- BlueCard rejections that don’t require medical documentation
- Provider affiliation rejections
- Claims processed after Medicare has paid or rejected
- Issues related to quantities billed (e.g., number of procedures, amount of drugs)
- In or out-of-network payments
- Refund requests
- Requests for additional payment
- Payment discrepancies
- Questions regarding patient benefits and claims
- COB claim inquiries
A provider service representative will review your claim and determine how to best resolve the issue. If the issue requires further investigation, the representative will document your concerns and forward your inquiry for review and resolution.
In the next article in this series, we’ll take a look at the many self-service tools and resources that can help answer your questions.
Reporting claims correctly and obtaining required prior authorizations reduces claim rejections and member appeals
Over the past several months, we’ve noticed an increased number of member appeals. Verifying member benefits and eligibility, reporting your claims accurately and obtaining required prior authorizations reduces your claim rejections and the number of member appeals.
Most claims are rejected because a claim submission contained incomplete documentation or incorrect coding for a service. Once the missing required information is submitted, the claim may be approved, avoiding an appeal.
Here are four common examples of incomplete or incorrect documentation:
- A laboratory submits a claim using a medical diagnosis code when it should be using a routine diagnosis code. This happens most frequently when lab tests are submitted by a primary care doctor as part of an annual health maintenance exam that is covered under the Affordable Care Act. In these cases, the lab services are considered routine, not medical, and the services should be coded as such.**
- There are laboratory tests (e.g., thyroid tests) that are considered diagnostic and are only covered with a medical diagnosis. These lab services should only be coded as medical, not routine.
- Infusion providers request prior authorization without supporting information. The authorization should be from the prescribing physician.
- A doctor’s office requests prior authorization for a drug but neglects to:
- Submit the correct prior authorization form for the drug.
- Include clinical information and member information.
- Complete the diagnosis field.
- Include chart notes or lab work that confirms the need for the drug, which supports the coverage requirements.
- Sign the prior authorization form.***
As a reminder, be sure to code services correctly and submit the appropriate documentation.
**You can access a list of Blues preventive services codes with no member cost sharing on web-DENIS.
- From the homepage of web-DENIS, click on BCBSM Provider Publications and Resources.
- Click on Newsletters and Resources.
- Under Health Reform, click on Information, and then on Blues preventive services codes with no cost sharing.
***For more information about drug prior authorizations, see this month’s installment of “Training Tips and Opportunities” by clicking here.
Training tips and opportunities: drug prior authorization
This is the fourth article in a series designed to educate health care providers and their staff about key aspects of the business and to let them know about the resources available to help them.
Prior authorization record reviews from across the country reveal some common trends in practice efficiency — and inefficiency — regarding prior authorization requests.
A practice’s prior authorizations requests for medications usually involve brand-name drugs for which there may or may not be a generic equivalent — or a drug that a patient has taken for years but that now requires reauthorization.
Tip: Practices should access the provider section of our website at bcbsm.com/providers to obtain prior authorizations whenever possible. Going online usually results in a faster response and helps you avoid wasting time while on hold with the telephone.
Most common errors
The most common errors when requesting a prior authorization and step therapy review are:
- Not using the prior authorization form that is specific to the requested drug
- Missing required clinical information or not completely filling out the prior authorization form
- Missing member information; e.g., contract number
- Not completing the diagnosis field
- Not sending “chart notes” or “lab reports” that support use of the medication
- Incorrectly marking a drug request as urgent when it is not
- Not signing drug prior authorization forms
Guidelines to follow
Keep the following in mind:
- Get prior authorization for specific drugs. Prior authorization is very important for all drugs ordered for patient use. For example, if you choose to administer a drug in the office that requires a prior authorization and it is later denied, your office may be charged for the cost of the drug. Some specialty drugs may cost $10,000 or more for one treatment. Denials can add up quickly, potentially creating time-consuming rework.
- Keep urgent drug requests reserved for life-threatening situations or if it is the opinion of a physician with knowledge of the patient’s medical condition that a standard processing time may seriously jeopardize the health or the patient’s ability to regain maximum function. If the urgent request is incorrectly prioritized, short time frames apply and incomplete forms may render a denial due to lack of information.
- Know what types of denials your practice typically receives. The errors listed above are just a few common causes of denials. These errors may cost your practice time and money filling in the missing information and resubmitting the request as an appeal. The more clearly you can identify any barriers that may cause your office to submit incomplete prior authorization requests, the better equipped you’ll be in addressing — and avoiding — them.
- Create an appeals process or review the one you already have. When denials are caused by inadequate documentation, it’s recommended to appeal the claim and supply the documentation that was originally missing from the initial prior authorization request to support the medical necessity. Also, file the appeal within the required timeframe.
Provider forums coming to a town near you
Blue Cross Blue Shield of Michigan and Blue Care Network are coming to you this summer. We’ve scheduled a series of forums focusing on our professional providers across the state. The classes will cover such key topics as:
- ICD-10 (professional)
- Medicare Advantage
- Provider Inquiry
- BlueCard
- Evicare
- Transparency
- Provider enrollment
Here’s a schedule of events:
- Half-day classes start at 9 a.m. and end at noon, with registration at 8:30 a.m.
- To accommodate driving schedules to the Upper Peninsula, classes will begin one hour later than usual. Registration for the Marquette and Sault Ste. Marie classes will be at 9:30 a.m., with the class starting at 10 a.m. (These times are for Upper Peninsula classes only.)
- Continental breakfast will be served.
To register, click on the link next to the event you’d like to attend. If you have questions, contact your provider consultant.
Class location |
Date |
Registration |
Sault Ste. Marie
Ramada Plaza Ojibway
240 W Portage Ave. 49783 |
Tuesday, Aug. 18, 2015 |
Click here. |
Marquette
Holiday Inn Marquette
1951 U.S. 41 West 49855 |
Wednesday, Aug. 19, 2015 |
Click here. |
Kalamazoo
Radisson Kalamazoo
100 West Michigan Ave. 49007 |
Tuesday, Sept. 15, 2015 |
Click here. |
Grand Rapids
Crowne Plaza
5700 28th St SE, Grand Rapids 49546 |
Thursday, Sept. 17, 2015 |
Click here. |
Novi
Sheraton Novi
21111 Haggerty Road 48375 |
Tuesday, Sept. 22, 2015 |
Click here. |
Frankenmuth
Bavarian Inn Lodge
One Covered Bridge Lane 48734 |
Tuesday, Oct, 6. 2015 |
Click here. |
Traverse City
Holiday Inn West Bay
615 E Front St, Traverse City 49686 |
Wednesday, Oct. 7, 2015 |
Click here. |
Sterling Heights
Best Western Sterling Inn
34911 Van Dyke Ave. 48312 |
Tuesday, Oct. 13, 2015 |
Click here. |
Okemos
Okemos Conference Center
2187 University Park Dr, Okemos 48864 |
Tuesday, Oct. 20, 2015 |
Click here. |
Southgate
Holiday Inn Southgate - Banquet & Conference Center
17201 Northline Road 48195 |
Wednesday, Oct. 21, 2015 |
Click here. |
Muskegon
Holiday Inn Muskegon - Harbor
939 3rd St, Muskegon 49440 |
Tuesday, Oct. 27, 2015 |
Click here. |
St. Joseph
Holiday Inn Express and Suites
3019 Lakeshore Dr., St. Joseph 49085 |
Wednesday, Oct. 28, 2015 |
Click here. |
Reminder: Training classes set for Upper Peninsula
As you read in the July Record, we’ve scheduled facility and professional training classes in Marquette and Sault Ste. Marie this August.
The facility class will feature billing tips, web-DENIS information and a question-and-answer session.
The professional class will cover such topics as coding and documentation, risk adjustment, the diagnostic closure incentive program, the performance recognition program, Health e-BlueSM and ICD-10.
U.P. training classes will begin one hour later than classes are usually scheduled:
- Full-day classes start at 10 a.m. and end at 4 p.m., with registration at 9:30 a.m.
- A lunch break will be provided between noon and 1 p.m., with lunch served at all locations.
- Classes might extend later or end earlier, depending on participant questions.
Following are the dates of the sessions and the class location:
Location |
Class |
Date |
Ramada Plaza Ojibway
240 W. Portage Ave.
Sault Ste. Marie, MI 49783 |
Professional |
Tuesday, Aug. 4 |
Facility |
Tuesday, Aug. 4 |
Holiday Inn Marquette
1951 U.S. 41 West
Marquette, MI 49855 |
Professional |
Thursday, Aug. 6 |
Facility |
Wednesday, Aug. 5 |
To register, email jholzhausen@bcbsm.com. For the facility class, type “Facility Marquette” or “Facility Sault Ste. Marie” in the subject line. For the professional class, type “HEDIS/RMRA Marquette” or “HEDIS/RMRA Sault Ste. Marie.” In the body of the email, include the date of the class and the number and names of attendees expected from your facility.
You’ll receive a confirmation within 72 hours of registering. It’s important that you register so we have an accurate headcount for lunch.
For more information, contact your provider consultant.
Reminder: Register today for summer educational sessions
We’ve scheduled a series of professional training opportunities this summer, with classes to be held at 14 locations across the state. The classes will cover such key topics as:
- HEDIS** and Medicare star ratings
- ICD-10 (professional)
- Performance recognition program
- Improving patient satisfaction
- Coding and documentation
- Diagnostic evaluation incentive program
- Health eBlueSM
- Member care alerts
To register, send an email to Jeff Holzhausen at JHolzhausen@bcbsm.com. In the subject line, write “HEDIS/RMRA” and the city where you wish to attend the class. Include the class date and the names and number of attendees expected from your facility. You will receive a confirmation within 72 hours of registering. It’s important that you register so we can have an accurate headcount for lunch.
For more information, contact your provider consultant.
**HEDIS is a registered trademark of the National Committee for Quality Assurance.
Documentation guidelines updated for physical therapy services
Effective July 15, 2015, we updated the medical record documentation requirements for physical therapy services.
For detailed information, see the “Documentation Guidelines for Physicians and Other Professional Providers” chapter of your online provider manual. Follow these steps to view the provider manual:
- From web-DENIS, click on BCBSM Provider Publications and Resources.
- Click on Provider Manual.
- Click on Provider Type and select yours from the “Make a Selection” box.
- Click on the Search button and then on the Documentation Guidelines for Physicians and Other Professional Providers chapter.
Magellan will stop servicing Blue Cross behavioral health authorization requests Oct. 1
Providers are strongly encouraged to finish all activities they have with Magellan Behavioral of Michigan Inc. as soon as possible. This includes incomplete authorizations and continued stay reviews, as well as initiating denial appeals or inquiries for dates of service prior to April 1, 2015.
New Directions LLC began managing Blue Cross Blue Shield of Michigan’s behavioral health services on April 1, replacing Magellan. Magellan discontinued the fax and e-mail process and contacts for obtaining authorizations on April 22. It will discontinue servicing of Blue Cross authorizations and related appeals effective Oct. 1.
Group accounts that have behavioral health services currently managed by another vendor arrangement are not affected by this reminder. This includes the State of Michigan, autos customers, UAW retirees and DENSO. The transition to New Directions does not affect these customer groups or network providers.
Here’s how to report charges for CPT II codes for lab services performed in office setting
When a physician performs laboratory tests *80061, *83036 or *83721 in the office, they are required to report the corresponding CPT II code (*3044F, *3045F, *3046F, *3048F, *3049F or *3050F). (Refer to the September 2013 Record article for more information.)
Providers should report a penny ($0.01) on the *3044F, *3045F, *3046F, *3048F, *3049F and *3050F claim lines as the charge billed. Providers will not receive reimbursement of the penny, as these codes are only for documentation purposes. Blue Cross Blue Shield of Michigan began paying health care providers an additional $5 per billing for LDL-C and HbA1c screeninglab services, as of July 15, 2013, and it’s included in the reimbursed fee.
This reporting information is for services performed in a physician office setting for members with PPO, Traditional and Medicare Advantage PPO plans when billed with the correct CPT Category II codes. These CPT Category II codes represent results of the tests in the form of a range of values.
Submitting a corrected claim
In April 2014, we began using the revised CMS-1500 form, version 02/12. This form replaced both the old CMS-1500 (version 08/05) and the Status Claim Review Form.
The new CMS-1500 form changed the process for submitting corrections for claims billed incorrectly. The Status Claim Review Form is no longer needed; the original claim can easily be corrected following the steps in your provider manual, which you can find on web-DENIS.
Following are the steps for correcting claims using web-DENIS.
- From web-DENIS, click on BCBSM Provider Publications and Resources.
- Click on Provider Manual.
- Click on Provider Type and select yours from the “Make Selection” box.
- Click on the Search button.
- Click on the Claims chapter.
- Click on Correcting Billing Errors.
Please follow these steps to submit corrected claims for billing errors and to add documentation when needed. Provider Inquiry service representatives will help you with the process if you are not yet familiar with it; however they cannot make the corrections.
Reporting global maternity services under ICD-10-CM
Beginning with dates of service on or after Oct. 1, 2015, ICD-10 codes will be used in place of ICD-9 codes. A claim can’t contain both ICD-9 and ICD-10 codes.
Some of the CPT codes for maternity services are global codes that may cover dates of service that span across the ICD-10 implementation date. When these instances occur, follow these guidelines when reporting a global maternity care code for services that span over the ICD-10 effective date. Current guidelines for reporting the dates of service in the “from” and “to” fields remain the same.
The following guidelines apply only when the “from” and “to” dates span across the ICD-10 implementation date of Oct. 1, 2015, and global maternity service procedure codes are used.
- Prenatal care only with a global CPT code: (*59425 and *59426)
- Enter the date of the first prenatal visit in the “from” field and last prenatal visit in the “to” field on the 1500 form. Note: This is the current guideline.
- Report the diagnosis using the ICD code set that is in effect for the date of service in the “from” field. For example, if the date in the “from” field is on or before Sept. 30, 2015, use the ICD-9 code. If the date in the “from” field is on or after Oct. 1, 2015, use the ICD-10 code.
- Global maternity care with a global CPT code: (*59400, *59410, *59510, *59515, *59610, *59614, *59618 or *59622)
- Enter the date of the first prenatal visit in the “from” field and the date of delivery in the “to” field. Note: This is the current guideline.
- Report the diagnosis using the ICD code set that’s in effect for the date of service in the “from” field. If the date in the “from” field is on or before Sept. 30, 2015, use the ICD-9 code. If the date in the “from” field is on or after Oct. 1, 2015, use the ICD-10 code.
- When the “from” date is on or before Sept. 30, 2015, and the postpartum care code of *0503F is for date of service on or after Oct. 1, 2015, submit this code on a separate claim and use that date of service in the “from” field and report the diagnosis using the ICD-10 code. Follow current billing guidelines and report a penny ($0.01) as the charge billed in field 24F. Or, if billing electronically, refer to the electronic billing manual for the correct procedure to follow. The three components of global maternity care include antepartum care, delivery and postpartum care.
As noted above, these guidelines apply only when the dates of service span across the ICD-10 implementation date and the service is covered under a global maternity code where the service cannot be split billed.
Reporting follow-up office visits for chemotherapy treatment with ICD-10-CM
The International Classification of Diseases, 10th revision, Clinical Modification, medical code set will become effective with dates of service on or after Oct. 1, 2015. As a result, some changes in reporting diagnosis codes will be needed due to differences between the ICD-9-CM and ICD-10-CM code set.
These code set differences will also affect reporting follow-up visits for monitoring a course of chemotherapy. Currently, there isn’t a unique code in ICD-10-CM to report a follow-up visit during a course of chemotherapy. In these instances, follow the ICD-10-CM Official Guidelines for Coding and Reporting. You can access the document by clicking here.
Here are two examples that may apply:
- Official coding guidelines state when the patient admission or encounter is only for administration of chemotherapy (immunotherapy or radiation therapy), assign the applicable code from category Z51 for other aftercare as the first listed or principal diagnosis. The malignancy that the therapy is being administered for should be assigned as a secondary diagnosis. When a follow-up visit is performed on the same day that the next course of chemotherapy is administered, these guidelines will apply. The code Z51.11 represents encounter for antineoplastic chemotherapy. Use of this code will establish that the patient is receiving a course of chemotherapy.
Example:
- Code: Z51.11 – Encounter for antineoplastic chemotherapy
- Code: For malignancy
- Official coding guidelines state that when the patient admission or encounter is for the management of anemia associated with an adverse effect of the administration of chemotherapy (or immunotherapy), and the treatment is only for the anemia, the anemia code is listed first, followed by the appropriate codes for the neoplasm and the adverse effect. Other blood disorders, such as pancytopenia or agranulocytosis, which are due antineoplastic chemotherapy, also apply to this guideline.
Example:
- Code: D64.81 – Anemia due to antineoplastic chemotherapy
- Code: For malignancy
- Code: For adverse effect of antineoplastic and immunosuppressive drugs
CPT and HCPCS Level II codes are not changing. You can continue to report the applicable procedure codes and continue to follow guidelines for those code sets.
If you have any questions, email ICD-10providerreadiness@bcbsm.com.
Clarification: transitional care management
In the May and August 2014 editions of The Record, we reported that procedure code 99495 is not payable for Blue Cross Blue Shield of Michigan contracts. The Federal Employees Program® is the only exception.
Procedure code 99496 remains payable for all cases of transitional care management.
The provider must communicate directly, electronically or by telephone with the patient or caregiver within two days of discharge from an inpatient hospital, skilled nursing facility or community mental health center stay, outpatient observation or partial hospitalization. A face-to-face visit must occur within seven business days of the patient’s discharge.
Services performed during the face-to-face visit must take place in conjunction with the appropriate non-face-to-face TCM services outlined within the “Transitional Care Management Services” section of the CPT manual.
Do you know about Blues Brief?
Blues Brief, a one-page newsletter designed for our participating health care providers, gives you a look at some of the top articles in two of our provider newsletters: The Record and BCN Provider News. It’s published monthly for professional providers and quarterly for facility providers.
Consultants share the document with providers during in-person visits. The newsletter also can be found on web-DENIS. Go to BCBSM Provider Publications and Resources, and then select Newsletters and Resources. Or you can subscribe to Blues Brief via email. Simply email your provider consultant and ask to be added to the email distribution list. Don’t know who your provider consultant is? Follow the instructions below.
How to find your provider consultant
- Go to bcbsm.com/providers.
- Click on Contact Us in the upper right corner of the page.
- Under “Physicians and professionals” or “Hospitals and facilities,” click on Blue Cross Blue Shield of Michigan provider contacts.
- Click on Provider consultants.
- Find your provider consultant on the applicable regional list.
Or simply click here.
Blues Brief survey
We recently conducted a survey to find out how satisfied health care providers and office staff are with the monthly newsletter. More than 180 providers responded to our survey. Here’s what you told us:
- Fifty-seven percent receive Blues Brief regularly.
- Seventy percent read Blues Brief often/sometimes.
- Eighty percent strongly agree or agree that the one-page format is easy to read.
- Seventy-five percent strongly agree or agree that Blues Brief includes useful information relevant to work you do with BCBSM and BCN.
- Eighty-six percent strongly agree or agree they are glad Blues Brief is available for both BCBSM and BCN.
Some providers asked how they could get other provider-related news. You can find out more about all of our provider e-newsletters and subscribe to them clicking here.
Congratulations, survey winner
In February, we invited readers of Blues Brief to take a brief survey and be entered into a drawing to win a $25 gift card. Jo Lunt of the Center for Pulmonary and Sleep Medicine in Petoskey was the winner.
Reminder: NPI to replace Blue Cross PIN on AIM Specialty Health’s provider portal
Effective June 23, 2015, AIM Specialty Health’s provider portal has implemented the use of each physician’s national provider identifier instead of the Blue Cross PIN for linking M.D.s or D.O.s to user accounts.
For active physicians already on the portal, you don’t need to make any changes. Their PINs will be migrated to NPIs; therefore, users will not need to re-add providers to their accounts.
When adding new physicians, please use the NPI, not the Blue Cross PIN. If you have any technical issues, please contact AIM’s technical support team at 1-800-252-2025 for assistance.
Please note that this does not affect hospitals as they are recognized and linked by their tax ID.

Do you know about GeoBlue®? It offers Blue Cross coverage for some GM members

As you read in a recent web-DENIS message, GeoBlue, in partnership with Blue Cross Blue Shield of Michigan, began serving more than 3,000 internationally based General Motors members Jan. 1, 2015. Many of these members seek care in the U.S. and present the GeoBlue identification card. See example at right.
We’ve received some inquiries from members regarding GeoBlue coverage so wanted to ensure that health care providers understand it fully. GeoBlue is a Blue Cross Blue Shield product and members have full access to the BlueCard provider network. Their ID card contains all BlueCard specifications and all BlueCard processes apply for coverage and claims.
If a member calls for an appointment and states that they have GeoBlue insurance, you can verify eligibility and benefits by calling GeoBlue Customer Service at 1-855-282-3517. After following the prompts (press 1 for services inside the U.S.), you’ll hear a recording that you cannot bypass. You need to wait until a customer service representative answers your call. Or you can go online and verify benefits through the Blue Exchange BlueCard system.
The GeoBlue ID card shows the member contract number, including the three-letter alpha prefix, and has the Blue Cross and Blue Shield symbols prominently displayed on the front.
Members with a GeoBlue ID card also have BlueDental® coverage. These members have access to dental providers who participate with the Blue Cross dental network or on a per claim basis. To verify dental benefits, log into web-DENIS or call PARS. Submit claims through the regular dental claims process.
Blue Cross Blue Shield of Michigan contracts with psychiatric residential treatment facilities in Michigan
Most Blue Cross members with mental health coverage now have coverage for psychiatric residential treatment.
Psychiatric residential treatment allows people who are suffering from a psychiatric illness to receive around-the-clock care on a short-term basis.
This level of care can allow patients with illnesses such as anorexia nervosa, schizophrenia or bipolar disorder to spend less time in a psychiatric hospital or avoid hospitalization. The treatment takes place in a state-licensed facility, for example, in an adult or child foster care facility with a multidisciplinary treatment team.
Psychiatric residential treatment is not meant to be used on an emergency basis, and admission must be coordinated by a mental health professional as part of an overall treatment plan.
Always make sure to check the member’s benefit coverage to determine eligibility. The facility must obtain preauthorization for the treatment to be covered.
To find an approved facility in Michigan, see our complete listing here.
Or you can go to bcbsm.com.
- Click Find a Doctor.
- Under “More Information,” click on Dental, Vision and Other Directories.
- Click on Approved Psychiatric Residential Treatment Facility List (PDF).
For more information on qualifying as a psychiatric residential treatment facility, read the January Record article on this topic.
Reporting claims correctly and obtaining required prior authorizations reduces claim rejections and member appeals
Over the past several months, we’ve noticed an increased number of member appeals. Verifying member benefits and eligibility, reporting your claims accurately and obtaining required prior authorizations reduces your claim rejections and the number of member appeals.
Most claims are rejected because a claim submission contained incomplete documentation or incorrect coding for a service. Once the missing required information is submitted, the claim may be approved, avoiding an appeal.
Here are four common examples of incomplete or incorrect documentation:
- A laboratory submits a claim using a medical diagnosis code when it should be using a routine diagnosis code. This happens most frequently when lab tests are submitted by a primary care doctor as part of an annual health maintenance exam that is covered under the Affordable Care Act. In these cases, the lab services are considered routine, not medical, and the services should be coded as such.**
- There are laboratory tests (e.g., thyroid tests) that are considered diagnostic and are only covered with a medical diagnosis. These lab services should only be coded as medical, not routine.
- Infusion providers request prior authorization without supporting information. The authorization should be from the prescribing physician.
- A doctor’s office requests prior authorization for a drug but neglects to:
- Submit the correct prior authorization form for the drug.
- Include clinical information and member information.
- Complete the diagnosis field.
- Include chart notes or lab work that confirms the need for the drug, which supports the coverage requirements.
- Sign the prior authorization form.***
As a reminder, be sure to code services correctly and submit the appropriate documentation.
**You can access a list of Blues preventive services codes with no member cost sharing on web-DENIS.
- From the homepage of web-DENIS, click on BCBSM Provider Publications and Resources.
- Click on Newsletters and Resources.
- Under Health Reform, click on Information, and then on Blues preventive services codes with no cost sharing.
***For more information about drug prior authorizations, see this month’s installment of “Training Tips and Opportunities” by clicking here.
Training tips and opportunities: drug prior authorization
This is the fourth article in a series designed to educate health care providers and their staff about key aspects of the business and to let them know about the resources available to help them.
Prior authorization record reviews from across the country reveal some common trends in practice efficiency — and inefficiency — regarding prior authorization requests.
A practice’s prior authorizations requests for medications usually involve brand-name drugs for which there may or may not be a generic equivalent — or a drug that a patient has taken for years but that now requires reauthorization.
Tip: Practices should access the provider section of our website at bcbsm.com/providers to obtain prior authorizations whenever possible. Going online usually results in a faster response and helps you avoid wasting time while on hold with the telephone.
Most common errors
The most common errors when requesting a prior authorization and step therapy review are:
- Not using the prior authorization form that is specific to the requested drug
- Missing required clinical information or not completely filling out the prior authorization form
- Missing member information; e.g., contract number
- Not completing the diagnosis field
- Not sending “chart notes” or “lab reports” that support use of the medication
- Incorrectly marking a drug request as urgent when it is not
- Not signing drug prior authorization forms
Guidelines to follow
Keep the following in mind:
- Get prior authorization for specific drugs. Prior authorization is very important for all drugs ordered for patient use. For example, if you choose to administer a drug in the office that requires a prior authorization and it is later denied, your office may be charged for the cost of the drug. Some specialty drugs may cost $10,000 or more for one treatment. Denials can add up quickly, potentially creating time-consuming rework.
- Keep urgent drug requests reserved for life-threatening situations or if it is the opinion of a physician with knowledge of the patient’s medical condition that a standard processing time may seriously jeopardize the health or the patient’s ability to regain maximum function. If the urgent request is incorrectly prioritized, short time frames apply and incomplete forms may render a denial due to lack of information.
- Know what types of denials your practice typically receives. The errors listed above are just a few common causes of denials. These errors may cost your practice time and money filling in the missing information and resubmitting the request as an appeal. The more clearly you can identify any barriers that may cause your office to submit incomplete prior authorization requests, the better equipped you’ll be in addressing — and avoiding — them.
- Create an appeals process or review the one you already have. When denials are caused by inadequate documentation, it’s recommended to appeal the claim and supply the documentation that was originally missing from the initial prior authorization request to support the medical necessity. Also, file the appeal within the required timeframe.
Reminder: Training classes set for Upper Peninsula
As you read in the July Record, we’ve scheduled facility and professional training classes in Marquette and Sault Ste. Marie this August.
The facility class will feature billing tips, web-DENIS information and a question-and-answer session.
The professional class will cover such topics as coding and documentation, risk adjustment, the diagnostic closure incentive program, the performance recognition program, Health e-BlueSM and ICD-10.
U.P. training classes will begin one hour later than classes are usually scheduled:
- Full-day classes start at 10 a.m. and end at 4 p.m., with registration at 9:30 a.m.
- A lunch break will be provided between noon and 1 p.m., with lunch served at all locations.
- Classes might extend later or end earlier, depending on participant questions.
Following are the dates of the sessions and the class location:
Location |
Class |
Date |
Ramada Plaza Ojibway
240 W. Portage Ave.
Sault Ste. Marie, MI 49783 |
Professional |
Tuesday, Aug. 4 |
Facility |
Tuesday, Aug. 4 |
Holiday Inn Marquette
1951 U.S. 41 West
Marquette, MI 49855 |
Professional |
Thursday, Aug. 6 |
Facility |
Wednesday, Aug. 5 |
To register, email jholzhausen@bcbsm.com. For the facility class, type “Facility Marquette” or “Facility Sault Ste. Marie” in the subject line. For the professional class, type “HEDIS/RMRA Marquette” or “HEDIS/RMRA Sault Ste. Marie.” In the body of the email, include the date of the class and the number and names of attendees expected from your facility.
You’ll receive a confirmation within 72 hours of registering. It’s important that you register so we have an accurate headcount for lunch.
For more information, contact your provider consultant.
Documentation guidelines updated for physical therapy services
Effective July 15, 2015, we updated the medical record documentation requirements for physical therapy services.
For detailed information, see the “Documentation Guidelines for Physicians and Other Professional Providers” chapter of your online provider manual. Follow these steps to view the provider manual:
- From web-DENIS, click on BCBSM Provider Publications and Resources.
- Click on Provider Manual.
- Click on Provider Type and select yours from the “Make a Selection” box.
- Click on the Search button and then on the Documentation Guidelines for Physicians and Other Professional Providers chapter.
Magellan will stop servicing Blue Cross behavioral health authorization requests Oct. 1
Providers are strongly encouraged to finish all activities they have with Magellan Behavioral of Michigan Inc. as soon as possible. This includes incomplete authorizations and continued stay reviews, as well as initiating denial appeals or inquiries for dates of service prior to April 1, 2015.
New Directions LLC began managing Blue Cross Blue Shield of Michigan’s behavioral health services on April 1, replacing Magellan. Magellan discontinued the fax and e-mail process and contacts for obtaining authorizations on April 22. It will discontinue servicing of Blue Cross authorizations and related appeals effective Oct. 1.
Group accounts that have behavioral health services currently managed by another vendor arrangement are not affected by this reminder. This includes the State of Michigan, autos customers, UAW retirees and DENSO. The transition to New Directions does not affect these customer groups or network providers.
Do you know about Blues Brief?
Blues Brief, a one-page newsletter designed for our participating health care providers, gives you a look at some of the top articles in two of our provider newsletters: The Record and BCN Provider News. It’s published monthly for professional providers and quarterly for facility providers.
Consultants share the document with providers during in-person visits. The newsletter also can be found on web-DENIS. Go to BCBSM Provider Publications and Resources, and then select Newsletters and Resources. Or you can subscribe to Blues Brief via email. Simply email your provider consultant and ask to be added to the email distribution list. Don’t know who your provider consultant is? Follow the instructions below.
How to find your provider consultant
- Go to bcbsm.com/providers.
- Click on Contact Us in the upper right corner of the page.
- Under “Physicians and professionals” or “Hospitals and facilities,” click on Blue Cross Blue Shield of Michigan provider contacts.
- Click on Provider consultants.
- Find your provider consultant on the applicable regional list.
Or simply click here.
Blues Brief survey
We recently conducted a survey to find out how satisfied health care providers and office staff are with the monthly newsletter. More than 180 providers responded to our survey. Here’s what you told us:
- Fifty-seven percent receive Blues Brief regularly.
- Seventy percent read Blues Brief often/sometimes.
- Eighty percent strongly agree or agree that the one-page format is easy to read.
- Seventy-five percent strongly agree or agree that Blues Brief includes useful information relevant to work you do with BCBSM and BCN.
- Eighty-six percent strongly agree or agree they are glad Blues Brief is available for both BCBSM and BCN.
Some providers asked how they could get other provider-related news. You can find out more about all of our provider e-newsletters and subscribe to them clicking here.
Congratulations, survey winner
In February, we invited readers of Blues Brief to take a brief survey and be entered into a drawing to win a $25 gift card. Jo Lunt of the Center for Pulmonary and Sleep Medicine in Petoskey was the winner.
Coding corner update: Improve medical record documentation for airway-related conditions
Beginning Oct. 1, 2015, the transition to ICD-10-CM will affect every area of health care. Many codes contain much greater specificity. This article includes updated codes to align with the transition to ICD-10-CM.
The overlap in terminology used to define airway-related conditions, such as chronic obstructive pulmonary disease, asthma, emphysema and chronic bronchitis, can often be confusing. The appropriate terminology for these conditions can best be determined through careful use of the ICD-10-CM Alphabetic Index.
Two particularly challenging conditions for coders are COPD and asthma. Although both share airway obstruction as a common feature, they’re at different ends of the clinical spectrum. However, the two conditions may overlap in many patients later in life.
Asthma often develops during childhood and can cause temporary airway obstruction. It’s often caused by allergies, too. In contrast, COPD usually develops later in life, is often related to smoking, and causes permanent airway obstruction. The two main forms of COPD are emphysema and chronic bronchitis. Asthma and COPD can often overlap, especially in elderly patients who might be affected by both diseases.
In ICD-10-CM, chronic obstructive asthma and asthma with COPD are reported with codes from the J44 category, other chronic obstructive pulmonary disease. Coding notes for this category state to code also the type of asthma, if applicable (J45.-). Use an additional code to identify exposure to tobacco smoke and tobacco use or dependence, if applicable.
Careful attention should be paid to documentation for a patient with a form of COPD and asthma. Here’s an example of how to assign diagnosis codes for a patient who’s affected by both conditions:
Assessment
- Acute exacerbation of COPD
- Acute bronchitis
- Acute exacerbation of asthma
Report diagnosis code J44.0, chronic obstructive pulmonary disease with acute lower respiratory infection for the COPD with acute lower respiratory infection (use additional code for the infection, bronchitis). Assign code J44.1, Chronic obstructive pulmonary disease with (acute) exacerbation, for the acute exacerbation of COPD; and code J45.901, unspecified asthma with (acute) exacerbation, for the acute exacerbation of asthma.
There’s an exclusion note under code J44.1 (COPD with acute exacerbation) that means multiple codes are required to code COPD with both an acute exacerbation as well as an acute respiratory infection.
The asthma category of codes has changed significantly in ICD-10-CM to reflect the current clinical classification of asthma. The following terms have been added to describe asthma: mild intermittent, mild persistent, moderate persistent and severe persistent. In addition, the ICD-10-CM codes also have the ability to identify with or without exacerbation and status asthmaticus. The classifications are determined by the frequency of the symptoms, exacerbation and status asthmaticus. Here are examples of the codes:
ICD-10-CM code |
Description |
J45.20 |
Mild intermittent asthma, uncomplicated |
J45.31 |
Mild persistent asthma with (acute) exacerbation |
J45.42 |
Moderate persistent asthma with status asthmaticus |
J45.51 |
Severe persistent asthma with (acute) exacerbation |
J45.902 |
Unspecified asthma with status asthmaticus |
J45.990 |
Exercise induced bronchospasm |
According to the ICD-10-CM guidelines, acute exacerbation is a worsening or a decompensation of a chronic condition. An acute exacerbation is not equivalent to an infection superimposed on a chronic condition, though an exacerbation may be triggered by an infection.Status asthmaticus is defined as a patient’s failure to respond to therapy administered during an asthmatic episode and is a life-threatening complication that requires emergency care.
ICD-10-CM coding for all conditions should follow coding conventions, chapter specific guidelines and general coding guidelines.
If you have any questions, contact your provider consultant.
None of the information included in this article is intended to be legal advice and, as such, it remains the provider’s responsibility to ensure that all coding and documentation are done in accordance with applicable state and federal laws and regulations.
Reminder: Register for Inpatient Clinical Document Improvement Forum
Facilities are invited to participate in a live informational forum on clinical documentation improvement on Thursday, Sept. 10, 2015, from 10 a.m. to 11:30 a.m., presented via WebEx. The program is for physicians and coders, and will be presented by Dr. Andrew Rothschild of the Berkeley Research Group. Dr. Rothschild will focus on documentation for complex inpatient coding issues such as blood loss anemia, acute renal failure and acute respiratory failure.
To register for the WebEx, email jvanbuitenen@bcbsm.com by Friday, Sept. 4, 2015. In the subject line, indicate “CDI Forum” and in the body of the email, list your name, facility, and the names of people participating who are not registering separately.
You’ll receive a confirmation within 72 hours of registering. Confirmation will include the WebEx information.
Reminder: Billing changes for inpatient and outpatient services
Outpatient services that occur 24 hours before, during or after an inpatient admission should be billed with the inpatient stay. Please combine the outpatient and inpatient services and submit one bill; the admission date should be the same as the date for the inpatient stay.
Outpatient services will only be considered part of the inpatient admission if there is a similar diagnosis/condition for each. Otherwise, the outpatient service is paid separately.
Reminder: Billing for physical, occupational and speech therapy
Blue Cross Blue Shield of Michigan has been receiving calls from hospitals that some PT, OT and ST claims are rejecting due to benefit maximum limits being reached. These claims may reach benefit maximum limits too early because of incorrect billing. If a date span is billed, rather than the individual dates of service, visit counts will be higher than they should be. Date spans should not be billed for PT, OT or ST claims.
For dates of service of Oct. 1, 2013, and later, hospital outpatient departments and freestanding OPTs were instructed to bill a separate revenue line reporting the revenue code and corresponding HCPCS code for each date of service a patient received a PT, OT or ST service. Billing instructions and examples were provided in the July 2013 issue of The Record. These instructions and claim examples are also in the “Claims” chapter of the hospital outpatient and freestanding OPT provider manuals.

Reporting claims correctly and obtaining required prior authorizations reduces claim rejections and member appeals
Over the past several months, we’ve noticed an increased number of member appeals. Verifying member benefits and eligibility, reporting your claims accurately and obtaining required prior authorizations reduces your claim rejections and the number of member appeals.
Most claims are rejected because a claim submission contained incomplete documentation or incorrect coding for a service. Once the missing required information is submitted, the claim may be approved, avoiding an appeal.
Here are four common examples of incomplete or incorrect documentation:
- A laboratory submits a claim using a medical diagnosis code when it should be using a routine diagnosis code. This happens most frequently when lab tests are submitted by a primary care doctor as part of an annual health maintenance exam that is covered under the Affordable Care Act. In these cases, the lab services are considered routine, not medical, and the services should be coded as such.**
- There are laboratory tests (e.g., thyroid tests) that are considered diagnostic and are only covered with a medical diagnosis. These lab services should only be coded as medical, not routine.
- Infusion providers request prior authorization without supporting information. The authorization should be from the prescribing physician.
- A doctor’s office requests prior authorization for a drug but neglects to:
- Submit the correct prior authorization form for the drug.
- Include clinical information and member information.
- Complete the diagnosis field.
- Include chart notes or lab work that confirms the need for the drug, which supports the coverage requirements.
- Sign the prior authorization form.***
As a reminder, be sure to code services correctly and submit the appropriate documentation.
**You can access a list of Blues preventive services codes with no member cost sharing on web-DENIS.
- From the homepage of web-DENIS, click on BCBSM Provider Publications and Resources.
- Click on Newsletters and Resources.
- Under Health Reform, click on Information, and then on Blues preventive services codes with no cost sharing.
***For more information about drug prior authorizations, see this month’s installment of “Training Tips and Opportunities” by clicking here.
Training tips and opportunities: drug prior authorization
This is the fourth article in a series designed to educate health care providers and their staff about key aspects of the business and to let them know about the resources available to help them.
Prior authorization record reviews from across the country reveal some common trends in practice efficiency — and inefficiency — regarding prior authorization requests.
A practice’s prior authorizations requests for medications usually involve brand-name drugs for which there may or may not be a generic equivalent — or a drug that a patient has taken for years but that now requires reauthorization.
Tip: Practices should access the provider section of our website at bcbsm.com/providers to obtain prior authorizations whenever possible. Going online usually results in a faster response and helps you avoid wasting time while on hold with the telephone.
Most common errors
The most common errors when requesting a prior authorization and step therapy review are:
- Not using the prior authorization form that is specific to the requested drug
- Missing required clinical information or not completely filling out the prior authorization form
- Missing member information; e.g., contract number
- Not completing the diagnosis field
- Not sending “chart notes” or “lab reports” that support use of the medication
- Incorrectly marking a drug request as urgent when it is not
- Not signing drug prior authorization forms
Guidelines to follow
Keep the following in mind:
- Get prior authorization for specific drugs. Prior authorization is very important for all drugs ordered for patient use. For example, if you choose to administer a drug in the office that requires a prior authorization and it is later denied, your office may be charged for the cost of the drug. Some specialty drugs may cost $10,000 or more for one treatment. Denials can add up quickly, potentially creating time-consuming rework.
- Keep urgent drug requests reserved for life-threatening situations or if it is the opinion of a physician with knowledge of the patient’s medical condition that a standard processing time may seriously jeopardize the health or the patient’s ability to regain maximum function. If the urgent request is incorrectly prioritized, short time frames apply and incomplete forms may render a denial due to lack of information.
- Know what types of denials your practice typically receives. The errors listed above are just a few common causes of denials. These errors may cost your practice time and money filling in the missing information and resubmitting the request as an appeal. The more clearly you can identify any barriers that may cause your office to submit incomplete prior authorization requests, the better equipped you’ll be in addressing — and avoiding — them.
- Create an appeals process or review the one you already have. When denials are caused by inadequate documentation, it’s recommended to appeal the claim and supply the documentation that was originally missing from the initial prior authorization request to support the medical necessity. Also, file the appeal within the required timeframe.

Do you know about GeoBlue®? It offers Blue Cross coverage for some GM members

As you read in a recent web-DENIS message, GeoBlue, in partnership with Blue Cross Blue Shield of Michigan, began serving more than 3,000 internationally based General Motors members Jan. 1, 2015. Many of these members seek care in the U.S. and present the GeoBlue identification card. See example at right.
We’ve received some inquiries from members regarding GeoBlue coverage so wanted to ensure that health care providers understand it fully. GeoBlue is a Blue Cross Blue Shield product and members have full access to the BlueCard provider network. Their ID card contains all BlueCard specifications and all BlueCard processes apply for coverage and claims.
If a member calls for an appointment and states that they have GeoBlue insurance, you can verify eligibility and benefits by calling GeoBlue Customer Service at 1-855-282-3517. After following the prompts (press 1 for services inside the U.S.), you’ll hear a recording that you cannot bypass. You need to wait until a customer service representative answers your call. Or you can go online and verify benefits through the Blue Exchange BlueCard system.
The GeoBlue ID card shows the member contract number, including the three-letter alpha prefix, and has the Blue Cross and Blue Shield symbols prominently displayed on the front.
Members with a GeoBlue ID card also have BlueDental® coverage. These members have access to dental providers who participate with the Blue Cross dental network or on a per claim basis. To verify dental benefits, log into web-DENIS or call PARS. Submit claims through the regular dental claims process. |