|
March 2014
We’ll no longer accept old version of CMS-1500 claim form beginning April 1
As you’ve read in previous issues of The Record, Blue Cross Blue Shield of Michigan will no longer accept the 08/05 version of the CMS-1500 claim form or the Status Claim Review Form, starting April 1, 2014.
You’ll need to use the revised CMS-1500 form, version 02/12. This form replaces both the old CMS-1500 (version 08/05) and the Status Claim Review Form.
If you submit an old CMS-1500 form (version 08/05) or Status Claim Review Form after March 31, 2014, it will be returned.
You can order the revised CMS-1500 claim form (version 02/12) by completing the Facility and Professional Supply Requisition form. There are two ways to access the form.
1) Through your provider manual:
- From web-DENIS, click on BCBSM Provider Publications and Resources.
- Click on Provider Manual.
- Click on Provider Type and select yours from the “Make Selection” box.
- Click on the Search button and then on the Blue Pages Directory chapter.
- Click on Forms and supplies and then on Facility and Professional Supply Requisition.
- Print and complete the form and mail it, along with a check for the total amount of your order, to the address provided on the form.
2) Through the Newsletters & Resources page:
- From web-DENIS, click on BCBSM Provider Publications and Resources.
- Click on Newsletters & Resources.
- Click on Facility and Professional Supply Requisition form, which you can access from the list of frequently used forms on the right side of the screen.
- Print and complete the form and mail it, along with a check for the total amount of your order, to the address provided on the form.
Differences in revised form
There are several key differences in the revised CMS-1500 form (version 02/12), including:
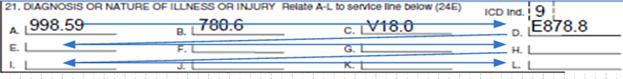
- The placement of the diagnosis codes in Field 21, “Diagnosis or Nature of Illness or Injury," has changed. You can now add additional diagnosis codes in this field. See screen shot below.
- Diagnosis pointers are now alphabetic characters in Field 24E, “Diagnosis Pointer”.
- Field 22, “Code And Original Ref. No.,” is now used to bill status inquiry claims.
- Field 19, “Additional Claim Information,” is the place to provide additional information, such as reasons for resubmission.
Correct billing format for revised form
Following is a closer look at the correct billing format for several key fields.
21. Diagnosis or Nature of Illness or Injury
- In the upper right-hand portion of Field 21, enter the applicable ICD indicator to identify which version of ICD codes is being reported. Enter “9” for ICD-9-CM or “0” for ICD-10-CM.
- Place the ICD indicator between the two vertical dotted lines in the upper right-hand portion of the field.
- Enter the appropriate codes to identify the patient’s diagnosis or condition. List no more than 12 diagnosis codes. Relate lines A-L to the lines of service in Field 24E by entering the corresponding reference letter (pointer) in Field 24E. (See screen shot under “24E., Diagnosis Pointer.”)
- Use the highest level of specificity possible. Do not provide a narrative description in this field.
- Diagnosis code placement is left to right (follow alpha characters).
24E. Diagnosis Pointer
- In Field 24E, enter the diagnosis code reference letter (pointer) as described above to relate the date of service and the procedures performed to the primary diagnosis. When multiple services are performed, the primary reference letter for each service should be listed first; other applicable services should follow.
- The reference letters should be A-L, as applicable. ICD-9-CM or ICD-10-CM diagnosis codes must be entered in Field 21 only. Do not enter them in Field 24E.
22. Resubmission Code and Original Ref. No.
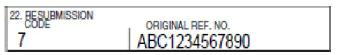
- This field takes the place of the Status Claim Review Form. If this is an original claim submission, leave this field blank.
- List the original reference number for resubmitted claims. When resubmitting a claim, enter the appropriate bill frequency code left-justified in the left-hand side of the field. Use “7” for a replacement of a prior claim or “8” to void or cancel a previous claim.
- If you complete Field 22 to indicate that this is a resubmitted claim, you must complete Field 19 as well, and provide additional information, such as the reason for resubmission.
19. Additional Claim Information
Keep in mind that this article only provides an overview of some of the key changes to the CMS-1500 claim. For more information about the form and how to complete it correctly, refer to your BCBSM provider manual. You may also check out the article in the January Record or contact your provider consultant. |