
|
|---|
|
|
| This newsletter includes short summaries, reminders and updates for Blue Cross and BCN providers. Please visit The Record or BCN Provider News for complete newsletter editions. New oncology management program for BCN starting Aug. 1 The Oncology Management Program promotes optimal cancer care and allows providers to compare planned cancer treatment against evidence-based regimens. The program will require providers to obtain authorizations from AIM Specialty Health® for medical oncology and supportive chemotherapy drugs, as well as immunotherapy. AIM applies Blue Cross Blue Shield of Michigan and Blue Care Network medical policies and identifies a subset of regimens as a Cancer Treatment Pathway. Blue Cross and BCN medical policies support Food and Drug Administration labeled indications and/or the National Comprehensive Cancer Network guidelines. Pathway regimens Cancer Treatment Pathways support high-quality, high-value cancer treatment. A rigorous process is applied to evaluate regimens supported by national guidelines, such as NCCN, oncology professional society practice guidelines, and by peer-reviewed published data. Factors considered include:
Enhanced reimbursement for providers By choosing a Pathway regimen, when clinically appropriate, the ordering provider may be eligible for enhanced reimbursement. The AIM ProviderPortalSM will display S-codes for the provider to bill BCN:
How to identify members in the program This program has already been implemented for Blue Cross URMBT PPO non-Medicare. To easily identify members included in the program refer to membership ID cards as shown at the top right. 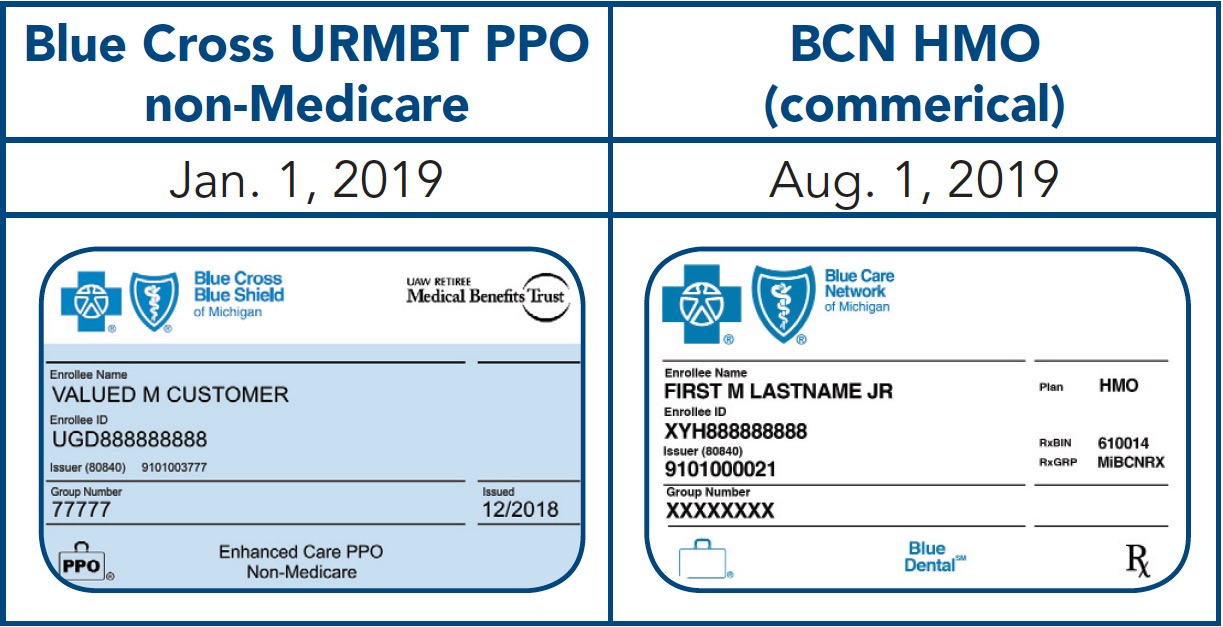
To learn more:
Reminder: Prior authorization changes for Blue Cross URMBT non-Medicare members, effective Jan. 1, 2019 Effective Jan. 1, 2019, Blue Cross began two new utilization management programs for medical and radiation oncology services delivered to UAW Retiree Medical Benefi ts Trust non-Medicare members. The programs require prior authorization for some outpatient through AIM Specialty Health. URMBT non-Medicare members who were in a treatment course prior to Jan. 1, 2019 were included in the continuity of care process. Read more in the November 2018 issue of The Record. Sign up to receive Blues Brief electronically As announced previously, Blues Brief is now available via email subscription. To sign up and avoid possible subscription errors, add Blues Brief to your subscriptions by clicking the Manage Subscriptions link at the bottom of your BCN Provider News or The Record newsletter emails. You can also visit the subscription page on bcbsm.com/providers to choose your preferred Blues Brief versions. Read more on Page 6 of the March–April 2019 BCN Provider News or the March 2019 issue of The Record. RC Claim Assist helps you bill for drugs under the medical benefit RC Claim Assist is available to Blue Cross and BCN contracted providers, and it’s a free resource for you to use. The benefi ts of using this tool are that it gives you an overview of HCPCS and CPT* drug codes, product names and national drug codes. In addition, it offers complete drug information on package-size billable units and reference pricing. To learn more, please see these resources on ereferrals.bcbsm.com. Click BCN or Blue Cross, then click the Medical Benefit Drugs – Pharmacy page:
*CPT codes, descriptions and two-digit numeric modifiers only are copyright 2018 American Medical Association. All rights reserved. Holiday office closings Blue Cross and BCN offi ces will be closed May 27 (Memorial Day) and July 4-5 (Independence Day). Utilization management programs summary document updated The Summary of utilization management programs for Michigan providers (PDF) has been updated with the changes listed below and is now available on ereferrals.bcbsm.com. Click BCN or Blue Cross, then the Authorization Requirements & Criteria page (formerly Clinical Review & Criteria Charts): Medical oncology drugs –
Radiation oncology –
CAQH Direct Assure 2.0 phases III and IV continue to roll out CAQH Direct Assure allows you to see specific group affiliation information that’s in our system so you can make updates and add group information to an individual provider’s CAQH record. Direct Assure also allows certain group changes made in CAQH to update the Blue Cross system so you no longer have to make updates in both areas — the CAQH and Blue Cross systems. Phase IV is scheduled to roll out at the end of June to specialists who are likely to be audited by the Centers for Medicare & Medicaid Services, including primary care physicians, cardiologists, oncologists and ophthalmologists. For more information, see the May 2019 issue of The Record. |
Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. |